Abstract
Objective
The purpose of this study is to measure the prevalence of graded disc degeneration, spondylolisthesis, transitional segmentation and the distribution of sacral slope in patients 21 to 65 years of age with chronic low back pain (CLBP).
Methods
This retrospective study analyzed 247 digital lumbar radiographic series obtained during a randomized controlled trial of chiropractic patients with CLBP. CLBP was defined as pain in the low back lasting 12 weeks or longer. Radiographic findings of disc degeneration, spondylolisthesis, and lumbosacral transitional segmentation were graded by 2 authors using established classification criteria. Sacral slope was measured with a digital tool contained within imaging software.
Results
Lumbosacral transitional segments graded I – IV (Castellvi classification) were present in 14% of cases. Lumbar disc degeneration was most prevalent at L3-4 (49%) followed by L4-5 (42%), L2-3 (41%), L5-S1 (37%), and L1-2 (29%). Isthmic spondylolisthesis was present in 5% of cases with L5 the most common location. Degenerative spondylolisthesis demonstrated a prevalence rate of 18%, most commonly occurring at L4. The prevalence of degenerative spondylolisthesis was 51% for females aged 50–59 and 24% for males in the same age range.
Conclusions
Moderate-severe disc degeneration, multi-level disc narrowing, and degenerative spondylolisthesis were common in individuals with CLBP over age 40. Isthmic spondylolisthesis was not more prevalent than what has been reported in other populations. Transitional segmentation was identified in a minority of participants with some of these exhibiting accessory joints or fusion. Mean sacral slope in individuals with CLBP was not substantially different from mean slopes reported in other populations.
Keywords: Low Back Pain, Prevalence, Intervertebral Disc Degeneration, Spondylolisthesis, Radiography, Lumbosacral Region, Chiropractic
INTRODUCTION
Radiographic examination is commonly utilized in the clinical evaluation of low back pain, despite some guideline recommendations to the contrary.(1;2) Guidelines recommend against radiography for uncomplicated acute and subacute low back pain in part to reduce cost, decrease risk from ionizing radiation exposure, and to avoid labeling patients with a condition which may not be the cause of pain.(1;3–5) However, for patients with uncomplicated chronic low back pain (CLBP), definitive radiographic recommendations are less certain.(1;5) One reason why radiography is often employed for low back pain evaluation may be because some findings provide information considered important to manual therapy providers because they potentially alter management strategy.(2;6–8)
There is mixed evidence surrounding the relationship between lumbar disc degeneration (LDD) and low back pain.(9–14) However, regardless of the presence or absence of a relationship with pain, there is evidence suggesting clinical diagnosis and management may benefit from consideration of LDD grading because of the following relationships LDD has with other conditions. Lumbar disc narrowing escalates the risk of stenosis and/or radicular compression,(15) zygapophyseal degeneration,(15–17) leads to motion segment laxity,(15) (18–20) and is thought to contribute to facetogenic pain.(21) LDD is also associated with multifidus atrophy.(22–28) Evidence suggests that weight training may be a viable treatment option for patients with mild LDD though this may not be true in the presence of moderate-severe LDD due to factors such as internal disc matrix disorganization, reduced diffusion rates, and annular weakening.(8;29–31)
The Grade of LDD in CLBP patients may influence practitioners as they consider treatment strategies such as multifidus stabilization and strength training, which have been shown to reduce the recurrence of low back pain,(32) improve motor control, and stimulate regrowth in CLBP patients.(33–35) An evidenced-based, quantitative understanding of graded LDD prevalence data in CLBP patients may help practitioners rely less on imaging.
Though lumbosacral transitional segments are not strongly associated with low back pain, high-velocity low-amplitude manipulative forces (36;37) could still affect accessory joints. Some providers who employ spinal manipulation may modify high-velocity thrusting as a precaution.(6;7) Likewise, spondylolisthesis (isthmic or degenerative) can be a clinically important finding though the condition may not be a source of pain. Degenerative spondylolisthesis can contribute to lumbar stenosis, while the isthmic type does not.(15;38;39) Evidence shows specific stabilizing exercises and spinal manipulation may be treatment options for patients with spondylolisthesis.(40;41) Some authors have suggested that high velocity thrusting directly over these segments may not be beneficial(6;41;42) though clinical studies are needed to confirm or refute this concept.
The sacral slope, defined as the angle formed between a horizontal line and the superior endplate of S1, is a key component in determining sagittal spinal curves. Changes seen in patients with low back pain are hypothesized to be due to variations in postural compensation in the presence of pain.(43) Sacral slope is associated with distinct lumbar lordosis patterns(44) and high slope angles increase the likelihood of spondylolysis and isthmic spondylolisthesis.(43;45–48) Due to a complex relationship between the pelvis and lumbar spine, lower sacral slope angles are reportedly associated with degenerative spondylolisthesis.(49)
The purpose of this study was to report prevalence rates for LDD, lumbosacral transitional segments, spondylolisthesis, and the sacral slope distribution in adults aged 21–65 years with CLBP (duration > 12 weeks) because the prevalence is largely unknown in a CLBP population and these findings can alter management strategy.
METHODS
Radiographic data for this secondary analysis came from a randomized controlled trial studying low back pain conducted between January 2009 and May 2011.(50) The current study was approved by the Palmer College of Chiropractic institutional review board. All participants provided consent. Chronic low back pain was defined as pain in the low back lasting 12 weeks or longer.
Subjects
Participants 21–65 years of age with low back pain greater than or equal to 4/10 on a numerical rating scale at phone screen or a baseline visit were recruited from the general population of the Quad Cities area of Iowa and Illinois via press release and direct mailers. Pain duration information was collected on study questionnaires from each of the 428 volunteers. Baseline visits were conducted at the Palmer Center for Chiropractic Research where participants also completed a Roland Morris Disability Questionnaire(51) and received clinical evaluation by a doctor of chiropractic. Radiography was utilized when considered clinically necessary based on imaging guidelines(4) and to render appropriate eligibility decisions for the clinical trial. Participants were ineligible if they reported neurological symptoms and demonstrated corresponding neurological signs (myotome weakness and absent lower extremity reflex[s]). Participants were also ineligible when the following were identified at examination: contraindication(s) to spinal manipulation, bone or joint abnormality indicating intolerance to treatment or biomechanical testing protocols, inflammatory or destructive tissue changes to the spine, severe osteoporosis, history of spinal surgery, vascular claudication, extreme obesity, sensitivity to tape adhesive, suspicion of drug or alcohol abuse, uncontrolled hypertension, Quebec Task Force classification 4, 5, 6, 8, 9, 10, 11,(52) and the need for referral or advanced diagnostic testing (e.g., blood, other imaging). Other exclusion criteria included: bleeding disorders, pregnancy, pacemaker or defibrillator, joint replacement history, severe depression, ongoing treatment by other healthcare providers, an open/pending legal case related to low back pain, and any other intolerance to treatment and/or biomechanical testing procedures. Only participants with CLBP were included for this secondary analysis (N=415).
Radiographs and Identification of Findings
Radiographs were obtained when the history demonstrated unresponsiveness to prior care and/or when, after clinical evaluation, images were thought to provide valuable information to make informed eligibility decisions regarding the safety of strenuous biomechanical testing and treatment group allocation. Digital lumbar anterior to posterior (A-P) and lateral radiographs were obtained on 248 of 415 participants with CLBP who received baseline clinical evaluation. A-P images were obtained in a neutral upright position with arms resting normally along the sides of the body. Lateral radiographs were also obtained in a neutral upright position with shoulders and elbows flexed to near 90 degrees or with arms folded against the chest while the hands rested on the shoulders.
One licensed chiropractic radiologist and 1 licensed doctor of chiropractic, each with research experience and each with greater than 20 years of clinical experience in their field, independently reviewed all de-identified radiographs, recording measurements and findings for each of the 4 categories (LDD, spondylolisthesis, lumbosacral transitional segmentation, and sacral slope). The 2 reviewers met to review, discuss, and determine final disposition of any discordant findings. Individual findings were not graded or measured if image quality prevented adequate visualization of structures. One set of images was not viewable on the imaging software during data collection, reducing the analysis to 247 series.
LDD
Graded disc degeneration was conducted according to a classification system developed by Lane.(53) Lane’s classification system is a reliable grading method for LDD, recommended by Kettler in a review of classification methods.(54) Images were viewed using Catella radiographic imaging software (Catella 5.0 PACS, AMD Technologies Inc., Los Angeles, CA).
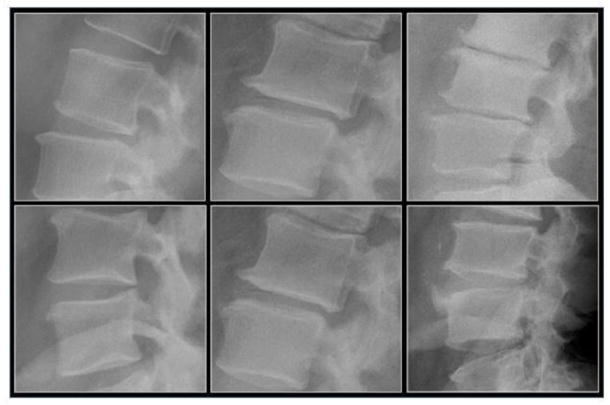
LDD was graded at each lumbar disc level based on 2 radiographic characteristics, disc narrowing and osteophytosis found on the lateral image. In some cases, the A-P image or other signs of degeneration, such as a vacuum phenomenon, were used to confirm an unclear finding on the lateral view. Scoring ranged from 0–3 for height loss and osteophytosis. A score of 0 represented no observable height loss or osteophytosis; a score of 1 represented mild height loss or mild osteophytosis; a score of 2 represented moderate height loss or moderate osteophytosis; and a score of 3 represented severe height loss or severe osteophytosis. When the disc level scored 0 for both height loss and osteophytosis, the grade was normal (no degeneration). A disc level scoring 1 (mild) for either height loss and/or osteophytosis was graded as mild degeneration. Scoring 2–3 for either disc height loss and/or osteophytosis was graded as moderate-severe degeneration. Wedge–shaped discs were not considered reduced in height unless other degenerative changes (e.g., osteophytosis, zygapophyseal hypertrophy, vacuum phenomenon, degenerative spondylolisthesis, or IVF narrowing) were present at that level. Lumbar discs below lumbosacral transitional segments were graded when fusion to the segment above or below was absent or the disc was not considered hypoplastic. Representative radiographs providing guideline examples of graded osteophytes and disc height loss were available to the reviewers throughout data collection. Images were agreed upon by all study team members prior to data collection and were consistent with examples described by Lane.(53) Figure 1 presents examples of radiographic features graded as mild, moderate and severe.
Figure 1.
Top row: Examples of disc narrowing graded as mild (with normal disc above), moderate, and severe from left to right. Bottom row: Examples of osteophytes graded as mild, moderate, and severe from left to right.
Spondylolisthesis
Isthmic spondylolisthesis was identified by forward translation of a vertebral body accompanied by an osseous defect or disruption in the pars interarticularis. Degenerative spondylolisthesis was identified by anterior vertebral body positioning with intact pars interarticularis. Both forms were graded by type and amount of anterior translation using the Meyerding grading system.(55) Grade 1 represents anterior translation of up to 25% of the posterior to anterior distance of the inferior vertebral body or sacrum as measured on the lateral image (grade 2 = 26–50%, grade 3 = 51–74%, grade IV = 75–100%).(55) Figure 2 presents examples of isthmic and degenerative spondylolisthesis.
Figure 2.
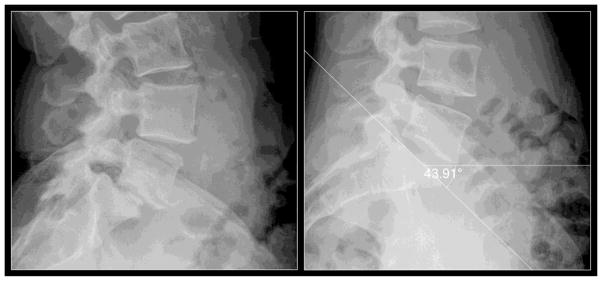
Left: illustrates an isthmic spondylolisthesis at L5 (Meyerding grade 2, i.e. between 25% and 50% anterior translation across the sacral plateau) and a degenerative spondylolisthesis at L4 (Meyerding grade 1, i.e. less than 25% anterior translation across the body of L5). Right: demonstrates sacral slope measurement using Catella 5.0 PACS digital software.
Lumbosacral transitional segmentation
Lumbosacral transitional segments were graded using a classification system developed by Castellvi.(56) This system graded the presence of unilateral or bilateral enlarged transverse processes, accessory joints or fusion in the lumbosacral area. Figure 3 shows examples of lumbosacral transitional segments graded with the Castellvi classification system.
Figure 3.

Lumbosacral transitional vertebrae (Castellvi Classification)
Left: Type IA, circle showing unilateral dysplastic (enlarged) transverse process. Center: Type IIA, arrow showing unilateral dysplastic transverse process with accessory joint. Right: Type III a, arrows showing unilateral dysplastic transverse process with bony union. Type IV or mixed (not shown) is classified as type II and type III on opposite sides. (Bilateral presentations of types I–III are designated with the letter b)
Sacral slope
Sacral slope was determined by forming an angle between a line drawn along the sacral base (sagittal view) and the horizontal plane using an angle measurement tool contained within the Catella imaging software. Figure 2 demonstrates a sacral slope measurement. Consensus measurements with both reviewers present occurred when individual measurements differed by more than 3 degrees. Three degrees was chosen as the maximum allowable variability because inter-observer variability measurements for sacral slope have been previously reported at 3 degrees.(57)
RESULTS
The sample includes 247 adults with 111 females and 136 males (Table 1). The mean (SD) age was 44.8 (10.9). All participants in this sample reported CLBP duration greater than 12 weeks. CLBP duration between 6 months and 1 year is represented by 7% of our sample. Ninety-one percent of participants in our sample reported symptoms lasting greater than 1 year. Mean (SD) pain as measured by the numerical rating scale was 5.7 (1.6) and mean Roland Morris disability score was 6.3 (4.2).
Table 1.
Number (percent) or mean (SD) of demographic and other characteristics of study participants with chronic low back pain.
| Female (n=111) | Male (n=136) | Total (n=247) | |
|---|---|---|---|
|
|
|||
| Age [mean (SD)] | 44.6 (11.2) | 45.1 (10.8) | 44.8 (10.9) |
| Age category | |||
| <40 | 33 (30) | 44 (32) | 77 (31) |
| 40 to 49 | 28 (25) | 40 (29) | 68 (28) |
| 50 to 59 | 43 (39) | 37 (27) | 80 (32) |
| 60 to 65 | 7 (6) | 15 (11) | 22 (9) |
| BMI1 [mean (SD)] | 30.3 (7.4) | 30.2 (5.4) | 30.2 (6.4) |
| NRS2 [mean (SD)] | 5.8 (1.8) | 5.6 (1.5) | 5.7 (1.6) |
| Beck Index3 [mean (SD)] | 9.5 (6.2) | 7.2 (5.9) | 8.3 (6.1) |
| Roland Morris4 [mean (SD)] | 6.8 (4.5) | 5.8 (4.0) | 6.3 (4.2) |
| Onset of pain (weeks) | |||
| >12 weeks and <6 months | 4 (4) | 0 (0) | 4 (2) |
| ≥6 months and <1 year | 10 (9) | 7 (5) | 17 (7) |
| ≥1 year | 97 (87) | 129 (95) | 226 (91) |
| Activity level5 | |||
| No physical activity | 2 (2) | 1 (1) | 3 (1) |
| Very light physical activity | 26 (23) | 19 (14) | 45 (18) |
| Light physical activity | 25 (23) | 16 (12) | 41 (17) |
| Moderate physical activity | 44 (40) | 69 (51) | 113 (46) |
| Heavy physical activity | 12 (11) | 27 (20) | 39 (16) |
| Very heavy physical activity | 2 (2) | 4 (3) | 6 (2) |
| Pain Frequency | |||
| Intermittent (0 to <25% of the time) | 6 (5) | 10 (7) | 16 (6) |
| Occasional (25 to <50% of the time) | 16 (14) | 22 (16) | 38 (15) |
| Frequent (50 to <75% of the time) | 23 (21) | 26 (19) | 49 (20) |
| Constant (75 to 100% of the time) | 66 (59) | 78 (57) | 144 (58) |
BMI= Body Mass Index
NRS= Numerical Rating Scale from 0–10; 0= no pain, 10= worst pain.
Beck Depression Inventory range 0–100; 0=no depression, 100= severe depression with <29 for eligibility.
Roland Morris range 0–24; 0= no disability, 24= severe disability.
Activity level was self-graded.
LDD occurred most often at L3-4 (49%). Table 2 presents information on LDD by disc level, age group and grade. Both multi-level disc narrowing and the prevalence of moderate to severe lumbar disc degeneration increased with age (Table 3.)
Table 2.
Number (percent) of graded disc degeneration1 by age group and disc level of study participants with chronic low back pain (n=247).
| Age group Graded disc |
L1-2 | L2-3 | L3-4 | L4-5 | L5-S1 |
|---|---|---|---|---|---|
| < 402 | (n=77) | (n=77) | (n=77) | (n=77) | (n=72) |
| None | 71 (92) | 66 (86) | 64 (83) | 69 (90) | 55 (76) |
| Mild | 5 (6) | 10 (13) | 13 (17) | 7 (9) | 14 (19) |
| Mod-severe | 1 (1) | 1 (1) | 0 (0.0) | 1 (1) | 3 (4) |
| 40–492 | (n=68) | (n=68) | (n=68) | (n=67) | (n=64) |
| None | 50 (74) | 40 (59) | 34 (50) | 35 (52) | 44 (69) |
| Mild | 15 (22) | 27 (40) | 30 (44) | 26 (39) | 7 (11) |
| Mod-severe | 3 (4) | 1 (1) | 4 (6) | 6 (9) | 13 (20) |
| 50–592 | (n=78) | (n=78) | (n=79) | (n=79) | (n=72) |
| None | 45 (58) | 36 (46) | 25 (32) | 33 (42) | 38 (53) |
| Mild | 32 (41) | 34 (44) | 43 (54) | 40 (51) | 21 (29) |
| Mod-severe | 1 (1) | 8 (10) | 11 (14) | 6 (8) | 13 (18) |
| 60–652 | (n=22) | (n=22) | (n=22) | (n=22) | (n=22) |
| None | 8 (36) | 2 (9) | 2 (9) | 5 (23) | 7 (32) |
| Mild | 9 (41) | 11 (50) | 11 (50) | 10 (45) | 9 (41) |
| Mod-severe | 5 (23) | 9 (41) | 9 (41) | 7 (32) | 6 (27) |
Disc degeneration graded according to Lane. None = no observable height loss or osteophytosis at disc level. Mild = mild height loss or mild osteophytosis. Mod-severe = moderate to severe height loss or moderate to severe osteophytosis.
Total numbers are due to gradable discs. Hypoplastic/rudimentary discs were not graded.
Table 3.
Number (percent within age group)1 of no disc narrowing, disc narrowing at 1 level, and multi-level disc narrowing with 1 or more levels of moderate to severe disc degeneration of study participants with chronic low back pain (n=247).
| Age | No narrowing | Single-level narrowing | Multi-level narrowing | Moderate to severe LDD2 |
|---|---|---|---|---|
| <40 (n=77) | 50 (65) | 20 (26) | 7 (9) | 6 (8) |
| 40–49 (n=68) | 33 (49) | 19 (28) | 16 (24) | 22 (32) |
| 50–59 (n=81) | 17 (21) | 28 (35) | 35 (43) | 26 (32) |
| 60–65 (n=22) | 2 (9) | 4 (18) | 16 (73) | 14 (64) |
| Total (n=248) | 102 (41) | 71 (29) | 74 (30) | 68 (27) |
Numbers (percent) reflect gradable discs. Hypolastic/rudimentary discs were not graded.
LDD- Lumbar disc degeneration which includes moderate to severe disc narrowing and/or moderate to severe osteophytes.
Isthmic spondylolisthesis was present in 12 cases representing a prevalence of 5%. L5 was the most common location (9) followed by L4 (2) and L3 (1). Meyerding grade 2 was present in 2 cases at L5 and 1 case at L4, while Grade 3 was present in a single case at L3. Degenerative spondylolisthesis was present in 45 cases representing a prevalence of 18%. The most common location for degenerative spondylolisthesis was L4 (26) followed by L5 (17) and L3 (2). Degenerative spondylolisthesis occurred once (1%) in the group below age 40. Other within-age-group comparisons revealed 5 cases (7%) of degenerative spondylolisthesis in the 40–49 yr age group, 31 cases (39%) within the 50 – 59 yr age group, and 8 cases (36%) above age 60. Degenerative spondylolisthesis by gender and age group is presented in Table 4.
Table 4.
Degenerative spondylolisthesis by gender and age in study participants with chronic low back pain (n=247).
| Age | Female | Male | Total | |||
|---|---|---|---|---|---|---|
| Sample size | n (%) | Sample size | n (%) | Sample size | n (%) | |
| <40 | 33 | 0 (0) | 44 | 1 (2) | 77 | 1 (1) |
| 40–49 | 28 | 4 (14) | 40 | 1 (3) | 68 | 5 (7) |
| 50–59 | 43 | 22 (51) | 37 | 9 (24) | 80 | 31 (39) |
| 60–65 | 7 | 2 (29) | 15 | 6 (40) | 22 | 8 (36) |
| Total | 111 | 28 (25) | 136 | 17 (13) | 247 | 45 (18) |
Thirty-five lumbosacral transitional segments were identified using the Castellvi classification system from 245 gradable cases (3 were not gradable), indicating a prevalence of 14%. There were 19 (8%) exhibiting accessory joints or fusion (Castellvi type II–IV). The mean (SD) sacral slope was 40.5 (7.8) degrees ranging from 20.4 to 61.5. The mean (SD) sacral slope for females was 41.3 (8.5) and for males was 39.9 (7.2).
DISCUSSION
Prevalence data for radiographically identifiable and graded LDD, spondylolisthesis, transitional segmentation, and sacral slope have not been widely reported in individuals specifically classified with CLBP. This study was conducted to help fill this evidence void. Knowledge of the likely presence or absence of these 4 radiographic findings is potentially important to clinicians evaluating patients with CLBP independent of whether or not findings are the source of or contribute to pain. Each of the findings studied represent physiological states that may not only influence imaging decisions and diagnosis, but also clinical treatment and management, especially for manual therapy providers.
Lumbar Disc Degeneration
Studies investigating prevalence of LDD use different imaging modalities and assessment methods unique to the procedure. Our findings were consistent with studies reporting that LDD is a common condition exhibiting an increasing prevalence with age.(9;10;12) In the current study, L3-4 was the most common level demonstrating any grade of LDD while L5-S1 showed the greatest frequency of moderate to severe grading. De Schepper reported L5-S1 as the most common level exhibiting radiographic narrowing in a sample aged 55 and higher using the same grading system.(53) In the current study, multi-level disc narrowing and moderate-severe LDD under age 40 was present in 9% and 8% of cases respectively, rising to 43% and 32% in the 50–59 age range.(Table 3). De Schepper reported narrowing and osteophytes occurred 50% and 55% respectively in the 55–59 age range.(9)
Using MRI, Vredeveld investigated Modic changes in patients scheduled for surgery and found far higher prevalence (80%) of LDD at non-disc herniation levels in patients over age 30 compared to those aged 29 and below (20%). (58) However, a pre-surgical study population is likely different from the sample evaluated in this study. Cheung, also using MRI, found higher rates of LDD with age in a general population sample, though L5-1 was again the most common level to show degeneration.(11)
Spondylolisthesis
Degenerative spondylolisthesis results from a combination of zygapophyseal (facet joint) deterioration and disc narrowing.(15) Our results are consistent with others reporting this finding more commonly in females 28 (25%) than males 17 (13%), most prevalent at L4 (26), and with increasing age.(38;59) Reduced prevalence in the over-60 age range is likely a factor of the very small sample in that group. Our results showed degenerative spondylolisthesis changed from 14% in females aged 40–49 to 51% of females aged 50–59 years, while males aged 40–49 demonstrated 3% prevalence increasing to 24% in the 50–59 group. Given the increasing prevalence trend in men aged 50–59 compared with earlier age groups, the results from this study are consistent with a 31% prevalence reported by Denard in men over age 64.(59)
Isthmic spondylolisthesis exhibits an anatomic defect located in the pars interarticularis and most commonly occurs at L5.(42) The prevalence of isthmic spondylolisthesis was 5%, approximately half the 8% reported elsewhere in a community sample.(60) Meyerding grade 1 was the most common presentation.
Lumbosacral Transitional Segments
Lumbosacral transitional segments are congenital anomalies of the lowest spinal segment, demonstrating anomalous formation of L5 or the superior sacral segment.(61) Though the relationship between lumbosacral transitional segments and low back pain is neither fully understood nor widely agreed upon,(13;61–64) recent evidence shows an association with types II and IV, characterized by accessory joints.(65) In this study, 19 (8%) were classified with accessory joints or fusion (Types II–IV).
The prevalence of all types of lumbosacral transitional segments categorized under the Castellvi classification system was 14%, similar to the 12% reported by Bron.(66) The prevalence of lumbosacral transitional segments has been reported as low as 2.3% and as high as 30% in symptomatic populations.(67;68) The large variation is likely the result of differences in classification criteria and populations studied.
Sacral Slope
The mean (SD) of 40.5 (7.8) degrees found in this study was similar to what has been reported in asymptomatic individuals (44;47;69;70) and slightly higher than the mean of 36.7 (9.0) reported by Chaléat-Valayer measured in CLBP patients.(71) The results of the current study suggest that sacral slope is not substantially different in patients with CLBP compared with other populations.
Limitations and future studies
Sixty percent of study participants with CLBP received radiographic examination based on the criteria described above. Because only a portion of individuals presenting for examination were imaged, results may not generalize to all CLBP patients. Secondly, systematic radiographic interpretation and inter-examiner reliability was not assessed and some findings may have been missed or made in error. To mitigate this limitation, the team chose reviewers with extensive clinical and research experience, used reliable and widely accepted grading/measuring methods, and included a consensus process to resolve discordant interpretation. The study had a small sample size of subjects in the 60–65 age range. Therefore, caution is warranted when interpreting results from this group. Spinal curvature and body size prevented adequate visualization, and therefore grading, of some intervertebral discs, potentially resulting in LDD underreporting.
Conclusions
This retrospective study provides prevalence data for radiographic findings of lumbosacral transitional segments, spondylolisthesis, LDD, and the distribution of sacral slope in adults age 21–65 with CLBP. The mean sacral slope and the prevalence of isthmic spondylolisthesis were similar to what has been reported in other populations. Moderate-severe disc degeneration and multi-level disc narrowing were common in individuals with CLBP over age 40.
Degenerative spondylolisthesis was common over age 39 in females and over age 49 in males. Knowledge of the high frequency of this condition in certain patient groups may assist clinicians with diagnostic and clinical management strategies.
Practical Applications.
The prevalence of transitional segmentation was 14% and 5% for isthmic spondylolisthesis.
Moderate to severe lumbar disc degeneration ranged from 8% under age 40 to 32% in participants age 50–59. Multi-level lumbar disc narrowing was evident in 9% of cases under age 40, increasing to 43% in the 50–59 age group.
The prevalence of degenerative spondylolisthesis was 0% in females under age 40, 14% in the 40–49 age group, and 51% in those aged 50–59.
In males, degenerative spondylolistheses was identified in 2% of those under age 40, 3% in those aged 40–49, and 24% in the 50–59 age group.
Mean (SD) sacral slope was 40.5 degrees (7.8).
Acknowledgments
FUNDING SOURCES
This work was partially funded through a grant from the National Institute of Health’s National Center for Complementary and Alternative Medicine (NCCAM) (1U19AT004137). This project was conducted in a facility constructed with support from Research Facilities Improvement Grant Number C06 RR15433 from the National Center for Research Resources, National Institutes of Health.
Footnotes
| Contributorship | For each author, list initials for how the author contributed to this manuscript. List author initials for each relevant category |
|---|---|
| Concept development (provided idea for the research) | RDV, EP, IM, MS, APM, JB, CG |
| Design (planned the methods to generate the results) | RDV, EP, IM, MS, APM, JB, CG |
| Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript) | RDV, EP, IM, MS, APM, JB, CG |
| Data collection/processing (responsible for experiments, patient management, organization, or reporting data) | RDV, EP, IM, MS, APM, JB, CG |
| Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results) | RDV, EP, IM, MS, APM, JB, CG |
| Literature search (performed the literature search) | RDV, EP, IM, MS, APM, JB, CG |
| Writing (responsible for writing a substantive part of the manuscript) | RDV, EP, IM, MS, APM, JB, CG |
| Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking) | RDV, EP, IM, MS, APM, JB, CG |
CONFLICTS OF INTEREST
No conflicts of interest were reported for this study.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Robert D. Vining, Associate Professor, Senior Research Clinician, Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
Eric Potocki, Research Clinician, Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
Ian McLean, Professor, Director of Clinical Radiology, Palmer College of Chiropractic.
Michael Seidman, Research Clinician, Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
A. Paige Morgenthal, Research Clinician, Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
James Boysen, Study Coordinator, Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
Christine Goertz, Vice Chancellor for Research and Health, Policy, Palmer Center for Chiropractic Research, Palmer College of Chiropractic.
Reference List
- 1.Chou R, Fu R, Carrino JA, Deyo RA. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. 2009 Feb 7;373(9662):463–72. doi: 10.1016/S0140-6736(09)60172-0. [DOI] [PubMed] [Google Scholar]
- 2.Ammendolia C, Bombardier C, Hogg-Johnson S, Glazier R. Views on radiography use for patients with acute low back pain among chiropractors in an Ontario community. J Manipulative Physiol Ther. 2002 Oct;25(8):511–20. doi: 10.1067/mmt.2002.127075. [DOI] [PubMed] [Google Scholar]
- 3.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007 Oct 2;147(7):478–91. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 4.Bussieres AE, Taylor JA, Peterson C. Diagnostic imaging practice guidelines for musculoskeletal complaints in adults-an evidence-based approach-part 3: spinal disorders. J Manipulative Physiol Ther. 2008 Jan;31(1):33–88. doi: 10.1016/j.jmpt.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Taylor JA, Bussieres A. Diagnostic imaging for spinal disorders in the elderly: a narrative review. Chiropr Man Therap. 2012;20(1):16. doi: 10.1186/2045-709X-20-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beck RW, Holt KR, Fox MA, Hurtgen-Grace KL. Radiographic anomalies that may alter chiropractic intervention strategies found in a New Zealand population. J Manipulative Physiol Ther. 2004 Nov;27(9):554–9. doi: 10.1016/j.jmpt.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 7.Bussieres AE, Patey AM, Francis JJ, Sales AE, Grimshaw JM, Brouwers M, et al. Identifying factors likely to influence compliance with diagnostic imaging guideline recommendations for spine disorders among chiropractors in North America: a focus group study using the Theoretical Domains Framework. Implement Sci. 2012;7:82. doi: 10.1186/1748-5908-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beattie PF. Current understanding of lumbar intervertebral disc degeneration: a review with emphasis upon etiology, pathophysiology, and lumbar magnetic resonance imaging findings. J Orthop Sports Phys Ther. 2008 Jun;38(6):329–40. doi: 10.2519/jospt.2008.2768. [DOI] [PubMed] [Google Scholar]
- 9.de Schepper EI, Damen J, van Meurs JB, Ginai AZ, Popham M, Hofman A, et al. The association between lumbar disc degeneration and low back pain: the influence of age, gender, and individual radiographic features. Spine (Phila Pa 1976) 2010 Mar 1;35(5):531–6. doi: 10.1097/BRS.0b013e3181aa5b33. [DOI] [PubMed] [Google Scholar]
- 10.Hicks GE, Morone N, Weiner DK. Degenerative lumbar disc and facet disease in older adults: prevalence and clinical correlates. Spine. 2009 May 20;34(12):1301–6. doi: 10.1097/BRS.0b013e3181a18263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheung KM, Karppinen J, Chan D, Ho DW, Song YQ, Sham P, et al. Prevalence and pattern of lumbar magnetic resonance imaging changes in a population study of one thousand forty-three individuals. Spine. 2009 Apr 20;34(9):934–40. doi: 10.1097/BRS.0b013e3181a01b3f. [DOI] [PubMed] [Google Scholar]
- 12.Kalichman L, Kim DH, Li L, Guermazi A, Hunter DJ. Computed tomography-evaluated features of spinal degeneration: prevalence, intercorrelation, and association with self-reported low back pain. Spine J. 2010 Mar;10(3):200–8. doi: 10.1016/j.spinee.2009.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine. 1997 Feb 15;22(4):427–34. doi: 10.1097/00007632-199702150-00015. [DOI] [PubMed] [Google Scholar]
- 14.Videman T, Battie MC, Gibbons LE, Maravilla K, Manninen H, Kaprio J. Associations between back pain history and lumbar MRI findings. Spine (Phila Pa 1976) 2003 Mar 15;28(6):582–8. doi: 10.1097/01.BRS.0000049905.44466.73. [DOI] [PubMed] [Google Scholar]
- 15.Modic MT, Ross JS. Lumbar degenerative disk disease. Radiology. 2007 Oct;245(1):43–61. doi: 10.1148/radiol.2451051706. [DOI] [PubMed] [Google Scholar]
- 16.Eubanks JD, Lee MJ, Cassinelli E, Ahn NU. Prevalence of lumbar facet arthrosis and its relationship to age, sex, and race: an anatomic study of cadaveric specimens. Spine (Phila Pa 1976) 2007 Sep 1;32(19):2058–62. doi: 10.1097/BRS.0b013e318145a3a9. [DOI] [PubMed] [Google Scholar]
- 17.Fujiwara A, Tamai K, Yamato M, An HS, Yoshida H, Saotome K, et al. The relationship between facet joint osteoarthritis and disc degeneration of the lumbar spine: an MRI study. Eur Spine J. 1999;8(5):396–401. doi: 10.1007/s005860050193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao F, Pollintine P, Hole BD, Dolan P, Adams MA. Discogenic origins of spinal instability. Spine. 2005 Dec 1;30(23):2621–30. doi: 10.1097/01.brs.0000188203.71182.c0. [DOI] [PubMed] [Google Scholar]
- 19.Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, et al. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine (Phila Pa 1976) 2000 Dec 1;25(23):3036–44. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 20.Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila Pa 1976) 1994 Jun 15;19(12):1371–80. doi: 10.1097/00007632-199406000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Hassett G, Hart DJ, Manek NJ, Doyle DV, Spector TD. Risk factors for progression of lumbar spine disc degeneration: the Chingford Study. Arthritis Rheum. 2003 Nov;48(11):3112–7. doi: 10.1002/art.11321. [DOI] [PubMed] [Google Scholar]
- 22.Kalichman L, Hodges P, Li L, Guermazi A, Hunter DJ. Changes in paraspinal muscles and their association with low back pain and spinal degeneration: CT study. Eur Spine J. 2010 Jul;19(7):1136–44. doi: 10.1007/s00586-009-1257-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hodges P, Holm AK, Hansson T, Holm S. Rapid atrophy of the lumbar multifidus follows experimental disc or nerve root injury. Spine (Phila Pa 1976) 2006 Dec 1;31(25):2926–33. doi: 10.1097/01.brs.0000248453.51165.0b. [DOI] [PubMed] [Google Scholar]
- 24.Hides JA, Stokes MJ, Saide M, Jull GA, Cooper DH. Evidence of lumbar multifidus muscle wasting ipsilateral to symptoms in patients with acute/subacute low back pain. Spine (Phila Pa 1976) 1994 Jan 15;19(2):165–72. doi: 10.1097/00007632-199401001-00009. [DOI] [PubMed] [Google Scholar]
- 25.Cooper RG, St Clair FW, Jayson MI. Radiographic demonstration of paraspinal muscle wasting in patients with chronic low back pain. Br J Rheumatol. 1992 Jun;31(6):389–94. doi: 10.1093/rheumatology/31.6.389. [DOI] [PubMed] [Google Scholar]
- 26.Danneels LA, Coorevits PL, Cools AM, Vanderstraeten GG, Cambier DC, Witvrouw EE, et al. Differences in electromyographic activity in the multifidus muscle and the iliocostalis lumborum between healthy subjects and patients with sub-acute and chronic low back pain. Eur Spine J. 2002 Feb;11(1):13–9. doi: 10.1007/s005860100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yoshihara K, Shirai Y, Nakayama Y, Uesaka S. Histochemical changes in the multifidus muscle in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 2001 Mar 15;26(6):622–6. doi: 10.1097/00007632-200103150-00012. [DOI] [PubMed] [Google Scholar]
- 28.Danneels LA, Vanderstraeten GG, Cambier DC, Witvrouw EE, De Cuyper HJ. CT imaging of trunk muscles in chronic low back pain patients and healthy control subjects. Eur Spine J. 2000 Aug;9(4):266–72. doi: 10.1007/s005860000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Niosi CA, Oxland TR. Degenerative mechanics of the lumbar spine. Spine J. 2004 Nov;4(6 Suppl):202S–8S. doi: 10.1016/j.spinee.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 30.Nguyen-minh C, Riley L, III, Ho KC, Xu R, An H, Haughton VM. Effect of degeneration of the intervertebral disk on the process of diffusion. AJNR Am J Neuroradiol. 1997 Mar;18(3):435–42. [PMC free article] [PubMed] [Google Scholar]
- 31.Lotz JC, Chin JR. Intervertebral disc cell death is dependent on the magnitude and duration of spinal loading. Spine (Phila Pa 1976) 2000 Jun 15;25(12):1477–83. doi: 10.1097/00007632-200006150-00005. [DOI] [PubMed] [Google Scholar]
- 32.Suni J, Rinne M, Natri A, Statistisian MP, Parkkari J, Alaranta H. Control of the lumbar neutral zone decreases low back pain and improves self-evaluated work ability: a 12-month randomized controlled study. Spine (Phila Pa 1976) 2006 Aug 15;31(18):E611–E620. doi: 10.1097/01.brs.0000231701.76452.05. [DOI] [PubMed] [Google Scholar]
- 33.Danneels LA, Cools AM, Vanderstraeten GG, Cambier DC, Witvrouw EE, Bourgois J, et al. The effects of three different training modalities on the cross-sectional area of the paravertebral muscles. Scand J Med Sci Sports. 2001 Dec;11(6):335–41. doi: 10.1034/j.1600-0838.2001.110604.x. [DOI] [PubMed] [Google Scholar]
- 34.Hides JA, Stanton WR, McMahon S, Sims K, Richardson CA. Effect of stabilization training on multifidus muscle cross-sectional area among young elite cricketers with low back pain. J Orthop Sports Phys Ther. 2008 Mar;38(3):101–8. doi: 10.2519/jospt.2008.2658. [DOI] [PubMed] [Google Scholar]
- 35.Van K, Hides JA, Richardson CA. The use of real-time ultrasound imaging for biofeedback of lumbar multifidus muscle contraction in healthy subjects. J Orthop Sports Phys Ther. 2006 Dec;36(12):920–5. doi: 10.2519/jospt.2006.2304. [DOI] [PubMed] [Google Scholar]
- 36.Triano J, Schultz AB. Loads transmitted during lumbosacral spinal manipulative therapy. Spine (Phila Pa 1976) 1997 Sep 1;22(17):1955–64. doi: 10.1097/00007632-199709010-00003. [DOI] [PubMed] [Google Scholar]
- 37.Van Zoest GG, Gosselin G. Three-dimensionality of direct contact forces in chiropractic spinal manipulative therapy. J Manipulative Physiol Ther. 2003 Nov;26(9):549–56. doi: 10.1016/j.jmpt.2003.08.001. [DOI] [PubMed] [Google Scholar]
- 38.Jacobsen S, Sonne-Holm S, Rovsing H, Monrad H, Gebuhr P. Degenerative lumbar spondylolisthesis: an epidemiological perspective: the Copenhagen Osteoarthritis Study. Spine (Phila Pa 1976) 2007 Jan 1;32(1):120–5. doi: 10.1097/01.brs.0000250979.12398.96. [DOI] [PubMed] [Google Scholar]
- 39.Jayakumar P, Nnadi C, Saifuddin A, Macsweeney E, Casey A. Dynamic degenerative lumbar spondylolisthesis: diagnosis with axial loaded magnetic resonance imaging. Spine (Phila Pa 1976) 2006 May 1;31(10):E298–E301. doi: 10.1097/01.brs.0000216602.98524.07. [DOI] [PubMed] [Google Scholar]
- 40.O’Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976) 1997 Dec 15;22(24):2959–67. doi: 10.1097/00007632-199712150-00020. [DOI] [PubMed] [Google Scholar]
- 41.Mierau D, Cassidy JD, McGregor M, Kirkaldy-Willis WH. A comparison of the effectiveness of spinal manipulative therapy for low back pain patients with and without spondylolisthesis. J Manipulative Physiol Ther. 1987 Apr;10(2):49–55. [PubMed] [Google Scholar]
- 42.Haun DW, Kettner NW. Spondylolysis and spondylolisthesis: a narrative review of etiology, diagnosis, and conservative management. J Chiropr Med. 2005;4(4):206–17. doi: 10.1016/S0899-3467(07)60153-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 2007 Sep;16(9):1459–67. doi: 10.1007/s00586-006-0294-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005 Feb 1;30(3):346–53. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 45.Antoniades SB, Hammerberg KW, DeWald RL. Sagittal plane configuration of the sacrum in spondylolisthesis. Spine. 2000 May 1;25(9):1085–91. doi: 10.1097/00007632-200005010-00008. [DOI] [PubMed] [Google Scholar]
- 46.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5-s1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine. 2005 Mar 15;30(6 Suppl):S27–S34. doi: 10.1097/01.brs.0000155560.92580.90. [DOI] [PubMed] [Google Scholar]
- 47.Rosok G, Peterson CK. Comparison of the sacral base angle in females with and without spondylolysis. J Manipulative Physiol Ther. 1993 Sep;16(7):447–52. [PubMed] [Google Scholar]
- 48.Wang Z, Parent S, Mac-Thiong JM, Petit Y, Labelle H. Influence of sacral morphology in developmental spondylolisthesis. Spine. 2008 Sep 15;33(20):2185–91. doi: 10.1097/BRS.0b013e3181857f70. [DOI] [PubMed] [Google Scholar]
- 49.Barrey C, Jund J, Perrin G, Roussouly P. Spinopelvic alignment of patients with degenerative spondylolisthesis. Neurosurgery. 2007 Nov;61(5):981–6. doi: 10.1227/01.neu.0000303194.02921.30. [DOI] [PubMed] [Google Scholar]
- 50.Wilder DG, Vining RD, Pohlman KA, Meeker WC, Xia T, DeVocht JW, et al. Effect of spinal manipulation on sensorimotor functions in back pain patients: study protocol for a randomised controlled trial. Trials. 2011;12:161. doi: 10.1186/1745-6215-12-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Deyo RA, Battie M, Beurskens AJ, Bombardier C, Croft P, Koes B, et al. Outcome measures for low back pain research. A proposal for standardized use. Spine (Phila Pa 1976) 1998 Sep 15;23(18):2003–13. doi: 10.1097/00007632-199809150-00018. [DOI] [PubMed] [Google Scholar]
- 52.Spitzer WO, LeBlanc FE, Dupuis M. Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine. 1987 Sep;12(7 Suppl):S1–S59. [PubMed] [Google Scholar]
- 53.Lane NE, Nevitt MC, Genant HK, Hochberg MC. Reliability of new indices of radiographic osteoarthritis of the hand and hip and lumbar disc degeneration. J Rheumatol. 1993 Nov;20(11):1911–8. [PubMed] [Google Scholar]
- 54.Kettler A, Wilke HJ. Review of existing grading systems for cervical or lumbar disc and facet joint degeneration. Eur Spine J. 2006 Jun;15(6):705–18. doi: 10.1007/s00586-005-0954-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet. 1932;54(2A):371–7. [Google Scholar]
- 56.Castellvi AE, Goldstein LA, Chan DP. Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine (Phila Pa 1976) 1984 Jul;9(5):493–5. doi: 10.1097/00007632-198407000-00014. [DOI] [PubMed] [Google Scholar]
- 57.Berthonnaud E, Labelle H, Roussouly P, Grimard G, Vaz G, Dimnet J. A variability study of computerized sagittal spinopelvic radiologic measurements of trunk balance. J Spinal Disord Tech. 2005 Feb;18(1):66–71. doi: 10.1097/01.bsd.0000128345.32521.43. [DOI] [PubMed] [Google Scholar]
- 58.Vredeveld T, Teitsma XM, Mert A, van der Wurff P. Prevalence of modic changes in active duty military men with lumbar disk herniation who were scheduled for surgery. J Manipulative Physiol Ther. 2012 Oct;35(8):622–8. doi: 10.1016/j.jmpt.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 59.Denard PJ, Holton KF, Miller J, Fink HA, Kado DM, Yoo JU, et al. Lumbar spondylolisthesis among elderly men: prevalence, correlates, and progression. Spine (Phila Pa 1976) 2010 May 1;35(10):1072–8. doi: 10.1097/BRS.0b013e3181bd9e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kalichman L, Kim DH, Li L, Guermazi A, Berkin V, Hunter DJ. Spondylolysis and spondylolisthesis: prevalence and association with low back pain in the adult community-based population. Spine (Phila Pa 1976) 2009 Jan 15;34(2):199–205. doi: 10.1097/BRS.0b013e31818edcfd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010 Nov;31(10):1778–86. doi: 10.3174/ajnr.A2036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Apazidis A, Ricart PA, Diefenbach CM, Spivak JM. The prevalence of transitional vertebrae in the lumbar spine. Spine J. 2011 Sep;11(9):858–62. doi: 10.1016/j.spinee.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 63.Luoma K, Vehmas T, Raininko R, Luukkonen R, Riihimaki H. Lumbosacral transitional vertebra: relation to disc degeneration and low back pain. Spine (Phila Pa 1976) 2004 Jan 15;29(2):200–5. doi: 10.1097/01.BRS.0000107223.02346.A8. [DOI] [PubMed] [Google Scholar]
- 64.Peterson CK, Bolton J, Hsu W, Wood A. A cross-sectional study comparing pain and disability levels in patients with low back pain with and without transitional lumbosacral vertebrae. J Manipulative Physiol Ther. 2005 Oct;28(8):570–4. doi: 10.1016/j.jmpt.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 65.Nardo L, Alizai H, Virayavanich W, Liu F, Hernandez A, Lynch JA, et al. Lumbosacral transitional vertebrae: association with low back pain. Radiology. 2012 Nov;265(2):497–503. doi: 10.1148/radiol.12112747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bron JL, van Royen BJ, Wuisman PI. The clinical significance of lumbosacral transitional anomalies. Acta Orthop Belg. 2007 Dec;73(6):687–95. [PubMed] [Google Scholar]
- 67.Delport EG, Cucuzzella TR, Kim N, Marley J, Pruitt C, Delport AG. Lumbosacral transitional vertebrae: incidence in a consecutive patient series. Pain Physician. 2006 Jan;9(1):53–6. [PubMed] [Google Scholar]
- 68.Hsieh CY, Vanderford JD, Moreau SR, Prong T. Lumbosacral transitional segments: classification, prevalence, and effect on disk height. J Manipulative Physiol Ther. 2000 Sep;23(7):483–9. doi: 10.1067/mmt.2000.108817. [DOI] [PubMed] [Google Scholar]
- 69.Marty C, Boisaubert B, Descamps H, Montigny JP, Hecquet J, Legaye J, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002 Apr;11(2):119–25. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hellems HK, Jr, Keats TE. Measurement of the normal lumbosacral angle. Am J Roentgenol Radium Ther Nucl Med. 1971 Dec;113(4):642–5. doi: 10.2214/ajr.113.4.642. [DOI] [PubMed] [Google Scholar]
- 71.Chaleat-Valayer E, Mac-Thiong JM, Paquet J, Berthonnaud E, Siani F, Roussouly P. Sagittal spino-pelvic alignment in chronic low back pain. Eur Spine J. 2011 Sep;20(Suppl 5):634–40. doi: 10.1007/s00586-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]