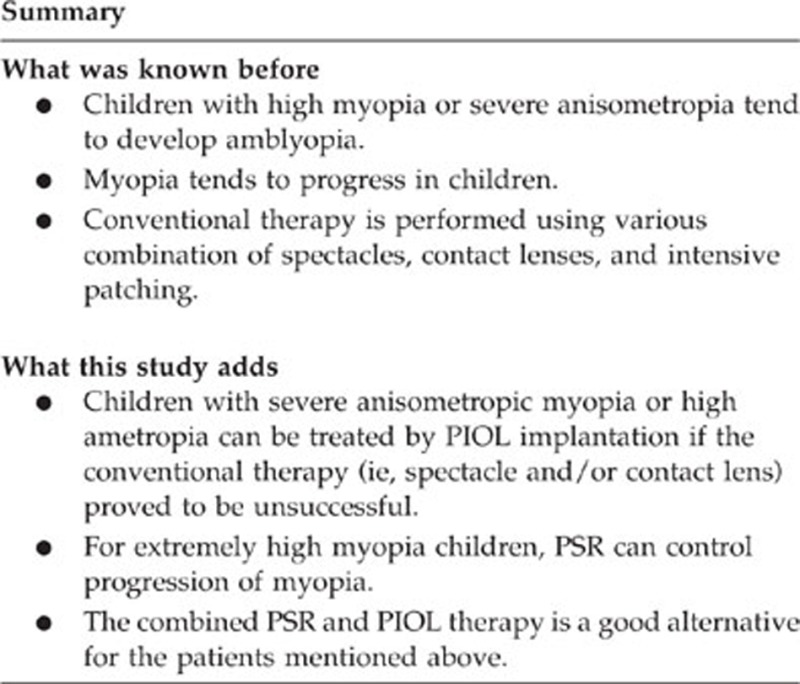
Abstract
Purpose
To study the safety and efficacy of posterior scleral reinforcement (PSR) combined with phakic intraocular lens (PIOLs) implantation for highly myopic amblyopia in children.
Methods
This study included eight highly myopic children (11 eyes) who failed in conventional therapy for amblyopia using various combination of spectacles, contact lenses, and intensive patching before enrollment into this study. They were treated sequentially with PSR and PIOL implantation, and were followed up for 3 years after surgery. Uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) in LogMAR, spherical equivalent power (SE), and complications were evaluated.
Results
Before surgery, the mean UCVA was 1.59±0.33, BCVA, 0.74±0.37, SE, −17.57±5.56D, the axial length (AL), 30.09±2.18 mm. After PSR, BCVA improved one line in three patients, the rest were unchanged, and AL was unchanged among all cases. Six eyes of three patients were implanted with an iris-claw PIOL and five eyes of five patients were implanted with a posterior PIOL. After completion of treatment, the mean UCVA was 0.44±0.21, BCVA 0.38±0.24, SE −0.54±0.74 D, and AL 30.35±2.29 mm. No patient experienced complications.
Conclusion
Combined PSR and PIOL implantation treatment for highly myopic amblyopia in children is safe and effective.
Introduction
Children with high myopia or severe anisometropia tend to develop amblyopia. Myopia is prone to progression, and its elongation of axial length (AL) may result into lesions in the fundus, eventually causing visual impairment. In children, high myopia or anisometropia is often difficult to correct because of noncompliance with spectacle or contact lens. Corneal refractive surgery is limited to patients with myopia of 10 D or less owing to the concern of ectasia secondary to a reduction in the residual stromal bed.1, 2 Reinforcement of the posterior sclera can control the progression of myopia. Phakic intraocular lens (PIOLs) implantation for children has been reported in the literature.3, 4, 5, 6, 7 In the current study, posterior scleral reinforcement surgery (PSR) and PIOL implantation were performed in highly myopic amblyopic children. The safety and efficacy for 3 years of follow-up were analyzed.
Materials and methods
This study enrolled highly myopic amblyopic children. All patients underwent conventional therapy for amblyopia using various combination of spectacles, contact lenses and intensive patching, and proved to be no improvement in their condition before enrollment into this study. Before PSR and PIOL implantation, the nature of both procedures and the expected results were explained to the parents and the children. Written informed consent was obtained from each patient.
Examinations
Patients were followed up at 1 day, 1 week, 1 month, 3 months, 6 months, and every 6 months after each of the intervention (ie, PSR, PIOL impantation, and patching therapy). Preoperative and postoperative examinations included manifest and cycloplegic refraction, uncorrected visual acuity (UCVA) and best corrected visual acuity (BCVA) in LogMAR, biomicroscopy, intraocular pressure, and dilated funduscopy. Eye position was measured by cover test. Postoperative stereopsis was measured by Randot Stereotest (Stereo Optical, Chicago, IL, USA) with refractive correction. Corneal curvature, anterior chamber depth and AL (IOLMaster, Zeiss, Jena, Germany), and corneal endotheliam density (SP-8000, Konan, Nishinomiya, Japan) were also measured.
Surgery procedure
Our surgical technique of PSR was published previously.8 PSR was performed under general anesthesia. Human sclera was obtained from a local eye bank after the cornea had been removed for transplantation. The donors of the sclera all had negative serology for HIV and hepatitis B. A 210° peritotomy of the conjunctiva was performed along the inferior–temporal axis of the limbus. A radial cut was made at each end of the peritotomy to expose the inferior and external rectus muscles and traction sutures prepared for these muscles. With the assistance of the traction sutures and a muscle hook that lifted up the complete inferior oblique, the scleral flap that was to be used for reinforcement was sequentially passed underneath the inferior oblique, external rectus, and inferior rectus muscles. During this process, efforts were made to protect the orbital septum and vortex veins. One end of the reinforcing flap was fixed to the sclera 2 mm behind the insertion point of the inferior rectus muscle, and the other end was stretched around the posterior pole and fixed to the sclera 2 mm temporal to the insertion point of the superior oblique muscle by using 5-0 nylon sutures. The reinforcement flap was stretched into a U-shape to surround the posterior pole. Before the end of procedure, the flap was checked to assure that it was correctly positioned and oriented. Finally, the conjunctival incision was closed using 8-0 absorbable sutures. Postoperatively, dexamethasone (0.1%) and antibiotic eye drops were recommended for use 4 times daily for 3 weeks.
After PSR, if the follow-up results revealed that manifest refraction, BCVA, and AL were stable, the PIOL would be implanted. Our surgical technique of PIOL implantation was published previously9 An iris-fixated PIOL (Artisan, Ophtec, Groningen, The Netherlands) was implanted in six eyes, and a posterior chamber PIOL (Visian ICL, STAAR Surgical, Nidau, Switzerland) was implanted in five eyes. One week after PIOL implantation, patients began patching therapy for 4 h per day, and continued for 3 months.
Results
Eight highly myopic pediatric patients (11 eyes) were recruited at the Eye Hospital of Wenzhou Medical University from February 2007 to July 2009. The patient demographics are as described in Table 1. Among them, four were female (seven eyes) and four were male (four eyes). The mean age was13.25±3.69 years (range: 9–17 years). The preoperative spherical equivalent power ranged from −11.5 D to −26.5 D. Three patients had bilateral high myopia and amblyopia, while 5 had severe anisometropia.
Table 1. Outcomes of posterior sclera reinforcement in eight children with high myopia.
| Patient no. | Sex | Age (years) | Eye | Operated | Preoperation | Postoperation | Follow-up (months) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
|
|
|
|
SE (D) |
BCVA |
AL (mm) |
SE (D) |
BCVA |
Line change in BCVA |
AL (mm) |
|
| 1 | M | 10 | OD | Y | −11.5 | 0.82 | 27.52 | −11.5 | 0.7 | 1 | 27.51 | 3 |
| OS | N | −2 | 0 | 23.62 | −2 | 0 | 23.63 | |||||
| 2 | M | 8 | OD | Y | −12 | 0.15 | 27.91 | −12 | 0.15 | 0 | 27.91 | 3 |
| OS | N | −2.25 | 0 | 24.4 | −2.25 | 0 | 24.4 | |||||
| 3 | F | 17 | OD | Y | −13 | 0.82 | 26.99 | −13 | 0.82 | 0 | 27.00 | 3 |
| OS | N | 0 | 0 | 22.36 | 0 | 0 | 22.36 | |||||
| 4 | M | 15 | OD | Y | −13.25 | 0.82 | 29.05 | −13.25 | 0.82 | 0 | 29.05 | 6 |
| OS | N | −3.25 | 0 | 25.09 | −3.25 | 0 | 25.09 | |||||
| 5 | F | 16 | OD | Y | −17 | 0.52 | 32.41 | −17 | 0.52 | 0 | 32.42 | 3 |
| OS | Y | −17.5 | 0.40 | 32.46 | −17.5 | 0.40 | 0 | 32.46 | ||||
| 6 | F | 9 | OD | Y | −26.25 | 1.30 | 31.38 | −26.25 | 1.30 | 1 | 31.38 | 3 |
| OS | Y | −26.5 | 1.00 | 30.87 | −26.5 | 1.00 | 1 | 30.88 | ||||
| 7 | F | 17 | OD | Y | −23.75 | 0.80 | 33.1 | −23.75 | 0.80 | 0 | 33.12 | 4 |
| OS | Y | −17.75 | 0.30 | 30.9 | −17.75 | 0.30 | 0 | 30.88 | ||||
| 8 | M | 14 | OD | N | −1.75 | 0 | 23.93 | −1.75 | 0 | 23.93 | ||
| OS | Y | −14.75 | 1.30 | 28.42 | −14.75 | 1.00 | 1 | 28.41 | 3 | |||
Abbreviations: AL, axis length; BCVA, best corrected visual acuity in LogMAR; SE, spherical equivalent power.
PSR and PIOL implantations were uneventful in all patients. The mean follow-up time was 38.25 months, and no postoperative complications occurred during whole follow-up period. Postoperative outcomes are presented in Tables 1, 2, 3. The mean spherical equivalent power improved from −17.57±5.56 D preoperatively to −0.54±0.74 D postoperatively (t=−10.33, P<0.01). BCVA improved from 0.74±0.37 preoperatively to 0.38±0.24 postoperatively (t=5.16, P<0.01). The mean postoperative UCVA was 0.44±0.21. The preoperative and postoperative AL were 30.09±2.18 and 30.35±2.29 mm, respectively (t=−3.19, P=0.01).
Table 2. Outcomes of PIOL implantation in eight children with high myopia.
| Patient no. | Eye |
Preoperation |
Postoperation |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SE (D) | UCVA | BCVA | ACD (mm) | AL (mm) | CED | PIOL | SE (D) | UCVA | BCVA | Line change in BCVA | AL (mm) | CED | Follow-up (months) | ||
| 1 | OD | −11.5 | 1.3 | 0.7 | 3.2 | 27.51 | 3205 | ICL-15.5 | 0 | 0.52 | 0.52 | 2 | 27.47 | 3121 | 46 |
| OS | −2 | 0.7 | 0 | 23.63 | −6.75 | 1.30 | 0 | 26.53 | |||||||
| 2 | OD | −12 | 1.5 | 0.15 | 3.02 | 27.91 | 2923 | ICL-17 | −0.75 | 0.22 | 0.10 | 1 | 28.56 | 2860 | 42 |
| OS | −2.25 | 0.52 | 0 | 24.4 | −6.75 | 1.00 | 0 | 26.49 | |||||||
| 3 | OD | −13 | 1.3 | 0.82 | 2.87 | 27.00 | 3076 | ICL-19 | 0.5 | 0.30 | 0.22 | 5 | 26.92 | 2993 | 42 |
| OS | 0 | 0 | 0 | 22.36 | −1.25 | 0.30 | 0 | 22.93 | |||||||
| 4 | OD | −13.25 | 1.5 | 0.82 | 3.06 | 29.05 | 3158 | ICL-19 | −1.5 | 0.40 | 0.30 | 4 | 29.56 | 3058 | 39 |
| OS | −3.25 | 0.7 | 0 | 25.09 | −6.25 | 1.00 | 0 | 26.49 | |||||||
| 5 | OD | −17 | 1.3 | 0.52 | 2.94 | 32.42 | 3401 | Artisan-17 | −0.5 | 0.22 | 0.15 | 3 | 32.77 | 2988 | 39 |
| OS | −17.5 | 1.3 | 0.40 | 2.96 | 32.46 | 3400 | Artisan-17 | −1 | 0.30 | 0.22 | 2 | 32.88 | 2933 | ||
| 6 | OD | −26.25 | 2 | 1.30 | 2.93 | 31.38 | 3058 | Artisan-23.5 | −0.5 | 0.70 | 0.70 | 3 | 31.48 | 2678 | 39 |
| OS | −26.5 | 2 | 1.00 | 2.97 | 30.88 | 2906 | Artisan-23.5 | 0 | 0.70 | 0.70 | 2 | 30.91 | 2896 | ||
| 7 | OD | −23.75 | 2 | 0.80 | 3.20 | 33.12 | 3003 | Artisan-23 | −1.75 | 0.80 | 0.70 | 1 | 33.46 | 2604 | 31 |
| OS | −17.75 | 2 | 0.30 | 3.3 | 30.88 | 2801 | Artisan-18.5 | −1 | 0.22 | 0.10 | 2 | 31.46 | 2755 | ||
| 8 | OD | −1.75 | 0.7 | 0 | 23.93 | −2.25 | 0.30 | 0 | 24.08 | 39 | |||||
| OS | −14.75 | 1.3 | 1.00 | 2.94 | 28.41 | 3169 | ICL-20 | 0.5 | 0.52 | 0.52 | 3 | 28.38 | 3108 | ||
Abbreviations: ACD, anterior chamber depth; AL, axis length; BCVA, best corrected visual acuity in LogMAR; CED, corneal endotheliam density (cells/mm2); PIOL, phakic intraocular lens; SE, spherical equivalent power; UCVA, uncorrected visual acuity in LogMAR.
Table 3. Functional results after combined therapy in eight children with high myopia during a 3-year follow-up.
| Patient no. | Eye |
Preoperation |
Postoperation |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Orthophoria | Stereopsis | Orthophoria | Stereopsis | BCVA | BCVA | BCVA | BCVA | BCVA | ||
| 1 week | 3 months | 1 year | 2 years | 3 years | ||||||
| 1 | OD | Y | N | Y | N | 0.52 | 0.52 | 0.52 | 0.52 | 0.52 |
| OS | ||||||||||
| 2 | OD | Y | N | Y | N | 0.1 | 0.1 | 0.1 | 0.1 | 0.10 |
| OS | ||||||||||
| 3 | OD | Y | N | Y | N | 0.52 | 0.4 | 0.22 | 0.22 | 0.22 |
| OS | ||||||||||
| 4 | OD | Y | N | Y | N | 0.52 | 0.4 | 0.3 | 0.3 | 0.30 |
| OS | ||||||||||
| 5 | OD | Y | — | Y | — | 0.22 | 0.22 | 0.22 | 0.15 | 0.15 |
| OS | 0.22 | 0.22 | 0.22 | 0.22 | 0.22 | |||||
| 6 | OD | Y | — | Y | — | 0.7 | 0.7 | 0.7 | 0.7 | 0.70 |
| OS | 0.7 | 0.7 | 0.7 | 0.7 | 0.70 | |||||
| 7 | OD | Y | — | Y | — | 0.7 | 0.7 | 0.7 | 0.7 | 0.70 |
| OS | 0.1 | 0.1 | 0.1 | 0.1 | 0.10 | |||||
| 8 | OD | |||||||||
| OS | Y | N | Y | N | 0.7 | 0.52 | 0.52 | 0.52 | 0.52 | |
Abbreviation: BCVA, best corrected visual acuity in LogMAR.
All patients were orthophoria before and after the combined treatment. Patients with unilateral high myopia (patients 1, 2, 3, 4, and 8) did not undergo stereopsis test after surgery. Patients 3, 4, and 8 gained one line of BCVA after intensive patching.
Discussion
After PSR, BCVA improved one line in three patients, the rest were unchanged, and AL was unchanged among all cases. The AL after PSR remained clinically stable during the 3 years of follow-up. In contrast, the AL increased significantly in eyes that did not receive PSR. High myopia occurs in children during a period of growth and development, and axial elongation occurs frequently, probably resulting to a series of fundus lesions such as choroidal atrophy, macular hemorrhage, choroidal neovascularization, and retinal holes. These lesions may ultimately lead to a serious decline in visual acuity. Many researches8, 10, 11 indicate that reinforcement of the posterior sclera can allow the allogeneic scleral material place around the macular area to adhere to the host sclera, and promote the entry of new vessels, thicken the new sclera, and mechanical reinforcement of the wall of eyeball. These changes can alleviate the pressure that extends back into the eye and maintain a stable refractive statue. At the same time, the biological effect of stimulating local allogeneic tissue leads to the dilation of the retinal vasculature and increased blood flow. The complications of PSR, particularly including optic nerve damage, muscle injury, retinal hemorrhage or ischemia, vortex vein damage, and globe distortion, has been reported in the literature. In the current study, PSR was performed under microscope, all patients had regular postoperative follow-up, and no complication occurred during the whole follow-up period.
Although PIOL implantation for myopia correction in adults proved to be safe and effective,1, 9, 12 performing surgery in pediatric patients may be somewhat controversial. People are concerned that PIOL implantation in children may cause complications such as acute or chronic inflammation, glaucoma, cataract, or a sustained loss of corneal endothelial cells. Patients were encouraged to maintain intensive patching therapy before they were enrolled into this study. However, visual acuity was not improved, and they were having difficulty in maintaining a normal daily life and learning due to poor vision during patching therapy. So PIOL implantation was considered as an alternative correction for high myopia in these children after fully communicating with patients' family members to ensure their understanding of the treatment. In this study, patients were followed up for 3 years after PIOL implantation, and no glaucoma, cataract, chronic inflammation, or other complications occurred. The rate of endothelial cell loss ranged from 1 to 13%. Our results are similar to previous studies13 that revealed implantation with an iris-claw or posterior chamber intraocular PIOL in highly myopic children significantly improved visual acuity. For safety reasons, doctors must carefully weigh the risks and benefits of PIOL implantation in children, and patients must be followed up regularly for long periods of time.
After combined PSR and PIOL implantation, the spherical equivalent power and visual acuity improved significantly and remained stable for 3-year follow-up. The stable refractive statue may be because of the enhanced mechanical resistance to axial growth after PSR. Visual acuity improvement after treatment is mainly due to the improvement of retinal image quality as a result of PIOL implantation. In addition, for highly anisometropic children, the refractive errors of the weak eye can be corrected after unilateral surgery. As visual stimulation improves, the pronounced inhibition can be significantly reduced. In this way, visual acuity can be significantly improved in these anisometropic cases. After intensive patching, BCVA improved one line in three patients. All patients expressed satisfaction with the results of their treatment. However, patients had no stereopsis after surgery even though they were orthophoria and the visual acuity was improved.
In conclusion, combined PSR and PIOL implantation treatment for highly myopic amblyopia in children is safe and effective. It is a good alternative to treat highly myopic amblyopia in children who have failed in conventional therapy (ie, spectacle and/or contact lens, and intensive patching).
The authors declare no conflict of interest.
References
- Chang DH, Davis EA. Phakic intraocular lenses. Curr Opin Ophthalmol. 2006;17:99–104. doi: 10.1097/01.cco.0000188624.54743.c7. [DOI] [PubMed] [Google Scholar]
- Tsiklis NS, Kymionis GD, Karp CL, Naoumidi T, Pallikaris AI. Nine-year follow-up a posterior chamber phakic IOL in one eye and LASIK in the fellow eye of the same patient. J Refract Surg. 2007;23 (9:935–937. doi: 10.3928/1081-597X-20071101-12. [DOI] [PubMed] [Google Scholar]
- BenEzra D, Cohen E, Karshai I. Phakic posterior chamber intraocular lens for the correction of anisometropia and treatment of amblyopia. Am J Ophthalmol. 2000;130:292–296. doi: 10.1016/s0002-9394(00)00492-x. [DOI] [PubMed] [Google Scholar]
- Lesueur LC, Arne JL. Phakic intraocular lens to correct high myopic amblyopia in children. J Refract Surg. 2002;18:519–523. doi: 10.3928/1081-597X-20020901-05. [DOI] [PubMed] [Google Scholar]
- Alió JL, Toffaha BT, Laria C, Piñero DP. Phakic intraocular lens implantation for treatment of anisometropia and amblyopia in children:5-year follow-up. J Refract Surg. 2011;27 (7:494–501. doi: 10.3928/1081597X-20110120-01. [DOI] [PubMed] [Google Scholar]
- Assil KK, Sturm JM, Chang SH. Verisyse intraocular lens implantation in a child with anisometropic amblyopia: four-year follow-up. J Cataract Refract Surg. 2007;33:1985–1986. doi: 10.1016/j.jcrs.2007.06.038. [DOI] [PubMed] [Google Scholar]
- Pirouzian A, Ip KC. Anterior chamber phakic intraocular lens implantation in children to treat severe anisometropic myopia and amblyopia: 3-year clinical results. J Cataract Refract Surg. 2010;36:1486–1493. doi: 10.1016/j.jcrs.2010.03.041. [DOI] [PubMed] [Google Scholar]
- Xue A, Bao F, Zheng L, Wang Q, Cheng L, Qu J. Posterior scleral reinforcement on progressive of high myopic young patients. Optom Vis Sci. 2014;91:412–418. doi: 10.1097/OPX.0000000000000201. [DOI] [PubMed] [Google Scholar]
- Ayong Y, Qinmei W, Anquan X, Zhu S, Wang S, Chen Y, et al. Comparison of contrast sensitivity after angle-supported, iris-fixated and posterior chamber phakic intraocular lenses implantation for high myopia. Ophthalmologica. 2008;222 (1:53–57. doi: 10.1159/000109280. [DOI] [PubMed] [Google Scholar]
- Ward B, Tarutta EP, Mayer MJ. The efficacy and safety of posterior pole buckles in the control of progressive high myopia. Eye (Lond) 2009;23:2169–2174. doi: 10.1038/eye.2008.433. [DOI] [PubMed] [Google Scholar]
- Zhu Z, Ji X, Zhang J, Ke G. Posterior scleral reinforcement in the treatment of macular retinoschisis in highly myopic patients. Clin Experiment Ophthalmol. 2009;37:660–663. doi: 10.1111/j.1442-9071.2009.02111.x. [DOI] [PubMed] [Google Scholar]
- Pirouzian A. Pediatric phakic intraocular lens surgery: review of clinical studies. Curr Opin Ophthalmol. 2010;21:249–254. doi: 10.1097/ICU.0b013e32833a9a9f. [DOI] [PubMed] [Google Scholar]
- Daoud YJ, Hutchinson A, Wallace DK, Song J, Kim T. Refractive surgery in children: treatment options, outcomes, and controversies. Am J Ophthalmol. 2009;147:573–582. doi: 10.1016/j.ajo.2008.12.028. [DOI] [PubMed] [Google Scholar]


