Abstract
Objective
To develop a tool for assessing amblyopic risk and monitoring the treatment effect of propranolol in periocular haemangioma management.
Methods
We present a study of nine children with periocular haemangioma who underwent propranolol treatment at York Hospital between 2009 and 2013.
A proposed measure of amblyogenic risk based on the induced anisometropia resulting from a periocular haemangioma was calculated in the form of a single quantitative value, measured in dioptres. This calculation used published work and developed it to produce a new function, termed the delta defocus equivalent (DFE-∂).
Refraction measurements were retrospectively collected from patients' notes in order to measure the trend of DFE-∂ over the treatment period with propranolol.
Results
The average DFE-∂ at commencement of propranolol was 1.54 (±0.62) D. The average at the end of treatment was 0.39 (±0.38) D.
Conclusion
This work presents a possible tool for assessing amblyopic risk in cases of periocular infantile haemangioma. The DFE-∂ gives a measure in dioptres, which may represent the true amblyopic risk, and so be useful in supporting treatment decisions in paediatric ophthalmology.
Introduction
Haemangiomata of infancy are common benign lesions occurring in up to 10% of children in their first year.1 When occurring periocularly, and left untreated, their visual sequelae are common.1 Amblyopia is the primary concern because of stimulus deprivation, induced anisometropia (mainly oblique astigmatism), secondary strabismus, or globe displacement.2
In 2008, Léauté-Labrèze et al3 reported a serendipitous discovery in the treatment of capillary haemangioma with propranolol. Propranolol has since been increasingly adopted as a first-line treatment for haemangioma4 and, while uncertainty of ideal dosage and treatment regimens still remains, 2 mg/kg/day split in three daily doses, is a frequently used regime.4 There is no consensus in the literature on the optimum time to start or stop propranolol therapy.
In this paper, we develop an approach using two formulae to calculate the amblyogenic risk.
Materials and methods
This is a retrospective clinical study of the first nine children who underwent propranolol treatment in our institution between 2009 and 2013 for periocular haemangioma.
Patients were started on 2 mg/kg/day propranolol by the paediatric team as per a local protocol. The cycloplegic refraction of both eyes was measured periodically. The initiation of treatment is based on the perceived risk of amblyopia from anisometropia, rather than observed difference in visual acuity.
To calculate an amblyogenic risk, the difference between the two refractions (from each eye) is calculated and expressed as a third theoretical refraction, using the Retzlaff formula.5 This is done by taking vector components of the cylinders in both the horizontal and vertical planes and comparing them. The formula accounts for the spherical equivalent, astigmatic power, and axis. It therefore will account for hypermetopic and myopic refractions, as well as positive and negative cylinder format. A calculation is then applied to this product, as described by Holladay et al6 to produce a single dioptre value, which Holladay termed the delta defocus equivalent (DFE), which might represent the amblyopic risk (as the DFE is proportional to the reduced visual acuity induced by that refraction6). Where the normal eye had an oblique refraction opposite to the affected eye, this was reflected about the 90° axis before being incorporated in the equation. As this is applied to the difference between the two refractions, we have termed this DFE-∂. A Microsoft Excel (Microsoft, Redmond, WA, USA) spreadsheet was used to implement DFE-∂ calculation.7
The following information was subsequently extracted from the patient files: lesion location, lesion type—superficial (lid) or deep (orbit), visual axis occlusion, age at initiation and termination of treatment, refractions, and visual acuity measured when treatment was discontinued (termed end visual acuity).
Results
Nine cases of periocular capillary haemangioma were treated in this study. None of the children had occlusion of the visual axis. The average DFE-∂ at commencement of propranolol was 1.54 (±0.62) D. The average at the end of treatment was 0.39 (±0.38) D (Table 1).
Table 1. Table showing data extracted from patient files. Patients ordered based on the age they started propranolol treatment from youngest to oldest.
| Patient | Sex | Lesion Location | Start age (weeks) | End age (weeks) | Total weeks treatment | Start refractions — Right eye — Left eye | End refractions — Right eye — Left eye | Cylinder power difference at start | Start DFE-∂ (dioptres) | End DFE-∂ (dioptres) | End Visual Acuity | Method for acuity measurement at end |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | M | Right orbit | 8 | 36 | 28 | +1.25/+2.00 × 45 +1.25/+1.00 × 85 | +1.00 DS +1.25 DS | 1.00 | 1.54 | 0.25 | 6/6 6/6 | Kay's |
| B | M | Left orbit | 9 | 47 | 38 | +1.25/+2.25 × 90 +1.25/+2.50 × 105 | +0.50/+0.75 × 90 +0.50/+1.00 × 90 | 0.25 | 0.75 | 0.25 | 6/6 BEO | CC |
| C | F | Left lid | 11 | 43 | 32 | +025/+3.00 × 90 +0.25/+4.00 × 100 | +1.50 +0.75/+1.00 × 90 | 1.00 | 1.28 | 0.75 | NR 6/9.5 | CC |
| D | F | Right orbit | 12 | 66 | 54 | −0.75/+4.00 × 70 +0.25/+2.00 × 90 | +1.00/+0.75 × 100 +1.25 | 2.00 | 1.39 | 0.50 | 6/9.5 6/9.5 | CC |
| Ea | M | Right orbit | 15 | 69 | 54 | −1.25/+4.00 × 105 +1.25/+1.00 × 95 | +0.50/+1.50 × 120 +0.75/+0.25 × 180 | 3.00 | 2.54 | 1.20 | 6/12 6/12 | CC |
| F | F | Right orbit+Lid | 22 | 70 | 48 | −2.00/+3.00 × 120 −2.00/+2.50 × 90 | +0.75/+1.25 × 180 +0.75/+1.00 × 180 | 0.50 | 1.64 | 0.25 | 6/12 6/12 | CC |
| G | F | Cheek lesion encroaching right orbit | 30 | 74 | 44 | pl/+2.50 × 110 +0.50/+1.00 × 90 | +1.75 DS +1.75 DS | 1.50 | 1.18 | 0 | 6/6 6/5 | SSG |
| H | F | Left lid | 34 | 83 | 49 | +0.25 DS +0.25/+1.00 × 80 | −0.25/+0.25 × 90 0/+0.25 × 75 | 1.00 | 1.00 | 0.32 | 6/6 6/6 | CC |
| I | M | Right orbit | 50 | 73 | 23 | +2.00/+1.75 × 60 +1.25 DS | +1.00 +1.00 | 1.75 | 2.50 | 0 | 6/6 6/6 | SSG |
| Mean (SD) | 21.2±14.2 | 62.3±16.2 | 41.1±11.4 | 1.54±0.62 | 0.39±0.38 |
Abbreviations: BEO, both eyes open; CC, Cardiff cards; Kay, Kay pictures; NR, not recorded; SSG, Sheridan Gardner Singles.
Propranolol treatment stopped and re-started (see results).
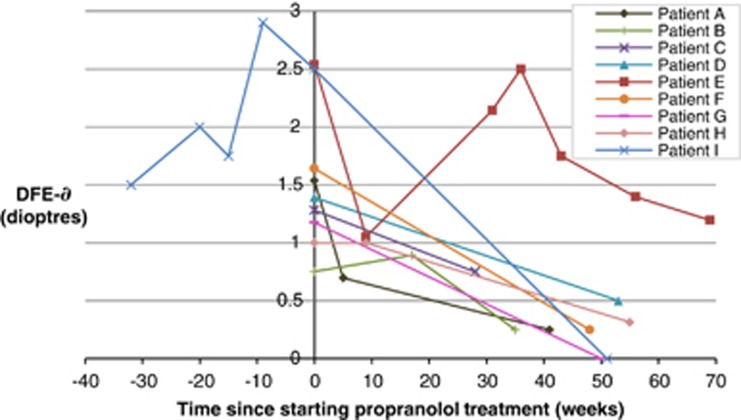
Figure 1 shows the DFE-∂ over the period of treatment for all the nine participants. It also demonstrates the DFE-∂ trend in patient I prior to initiating propranolol treatment.
Figure 1.
Change in DFE-∂ with respect to time for all the nine patients.
Of note is the DFE-∂ rise corresponding to rebound haemangioma growth in patient E whose propranolol treatment was stopped prematurely. Patient E's initial response to propranolol is represented by a drop from 2.54 to 1.06 after 9 weeks of treatment. After 20 weeks, the propranolol was tapered down as his mother had concerns that the treatment was contributing to breath-holding attacks. Refraction measurements were not taken at 20 weeks; however, the DFE-∂ calculations at 31 weeks (2.14 D) and 36 weeks (2.5 D) correlate to the clinically observed re-bound growth. At 36 weeks, 2 mg/kg/day propranolol was re-started and the DFE-∂ began to fall once more ending at 1.20 D.
Discussion
This work demonstrates a useful application of the Retzlaff formula and DFE as a tool for assessing amblyopic risk and monitoring treatment effect in infantile haemangioma management.
Measurement of the treatment effect from propranolol varies widely in the literature. Qualitative approaches have included the use of visual analogue scales to assess the lesion with respect to its colour, size and growth.8 Imaging with ultrasound, MRI9, and photographic surface area measurement10 have also been used. Ophthalmic quantitative measurements have mainly focused on calculating an amblyogenic astigmatic error from the difference in cylinder power between the affected and unaffected eyes.10, 11, 12Where cylinder axis and spherical equivalent are similar, the proposed formula for calculating the amblyogenic risk will have little advantage. However, this will ignore oblique axes induced by the haemangioma (eg patients A, B, and F) as well as over playing the cylinder power significance if the spherical equivalent is similar (eg patient D). We suggest a DFE-∂ calculation ultimately will be more accurate as all components of the refraction are included; however, we accept cylinder power alone will act as a guide. Larger studies will be needed to compare the two.
The decision to begin propranolol treatment was always made clinically; however, our results suggest a DFE-∂ of 1.5 D could be an appropriate guide, particularly if it is increasing over time, in support of the treatment decision.
This clinical study also adds to the increasing body of evidence4 in support of propranolol as a first-line treatment for periocular haemangioma.
The authors declare no conflict of interest.
Footnotes
An abstract has been submitted for consideration by the British Isles Paediatric, Ophthalmology & Strabismus Association (BIOPSA) as a 7 min ‘free paper presentation' at their annual conference in Birmingham in September 2014
References
- Wahrman J, Honig P. Haemangiomas. Paediatr Rev. 1994;15:266–271. doi: 10.1542/pir.15-7-266. [DOI] [PubMed] [Google Scholar]
- Stigmar G, Crawford JS, Ward CM, Thompson HG. Ophthalmic sequelae of infantile hemangiomas of the eyelids and orbit. Am J Ophthalmol. 1978;85 (6:806–813. doi: 10.1016/s0002-9394(14)78109-7. [DOI] [PubMed] [Google Scholar]
- Léauté-Labrèze C, Dumas de la Roque E, Hubiche T, Boralevi F. Propranolol for severe hemangiomas of infancy. N Engl J Med. 2008;358 (24:2649–2651. doi: 10.1056/NEJMc0708819. [DOI] [PubMed] [Google Scholar]
- Drolet BA, Frommelt PC, Chamlin SL, Haggstrom A, Bauman NM, Chiu YE, et al. Initiation and use of propranolol for infantile hemangioma: report of a consensus conference. Pediatrics. 2013;131 (1:128–140. doi: 10.1542/peds.2012-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retzlaff J, Paden PY, Ferrell L. Vector analysis of astigmatism. J Cat Ref Surg. 1993;19:393–398. doi: 10.1016/s0886-3350(13)80312-4. [DOI] [PubMed] [Google Scholar]
- Holladay JT, Lynn MJ, Waring GO, III, Gemmil M, Keehn G, Fielding B. The relationship of visual acuity, refractive error and pupil size after radial keratotamy. Arch Ophthalmol. 1991;109:70–77. doi: 10.1001/archopht.1991.01080010072036. [DOI] [PubMed] [Google Scholar]
- Taylor RH, Ellingham RB, Subramaniam S, Weakly LA. Calculating the error in refractive error. Eye. 2012;26 (4:622. doi: 10.1038/eye.2011.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassallo P, Forte R, Di Mezza A, Magli A. Treatment of infantile capillary hemangioma of the eyelid with systemic propranolol. Am J Ophthalmol. 2013;155 (1:165–170. doi: 10.1016/j.ajo.2012.06.021. [DOI] [PubMed] [Google Scholar]
- Thourmazet F, Léauté-Labrèze C, Colin J, Mortemousque B. Efficacy of systemic propranolol for severe infantile haemangioma of the orbit and eyelid: a case study of eight patients. Br J Ophthalmol. 2012;96 (3:370–374. doi: 10.1136/bjophthalmol-2011-300047. [DOI] [PubMed] [Google Scholar]
- Missoi TG, Lueder GT, Gilbertson K, Bayliss SJ. Oral propranolol for treatment of periocular infantile hemangiomas. Arch Ophthalmol. 2011;129 (7:899–903. doi: 10.1001/archophthalmol.2011.40. [DOI] [PubMed] [Google Scholar]
- Fabian ID, Ben-Zion I, Samuel C, Spierer A. Reduction in astigmatism using propranolol as first-line therapy for periocular capillary hemangioma. Am J Ophthalmol. 2011;151 (1:53–58. doi: 10.1016/j.ajo.2010.07.022. [DOI] [PubMed] [Google Scholar]
- Snir M, Reich U, Siegel R, Zvulunov A, Friling R, Goldenberg-Cohen N, et al. Refractive and structural changes in infantile periocular capillary haemangioma treated with propranolol. Eye. 2011;25:1627–1634. doi: 10.1038/eye.2011.233. [DOI] [PMC free article] [PubMed] [Google Scholar]