ABSTRACT
Purpose
Uncorrected refractive error remains a leading cause of visual impairment (VI) across the globe with Mozambique being no exception. The establishment of an optometry profession in Mozambique that is integrated into the public health system denotes significant progress with refractive services becoming available to the population. As the foundations of a comprehensive refractive service have now been established, this article seeks to understand what barriers may limit their uptake by the general population and inform decision making on improved service delivery.
Methods
A community-based cross-sectional study using two-stage cluster sampling was conducted. Participants with VI were asked to identify barriers that were reflective of their experiences and perceptions of accessing refractive services. A total of 4601 participants were enumerated from 76 clusters in Nampula, Mozambique.
Results
A total of 1087 visually impaired participants were identified (884 with near and 203 with distance impairment). Cost was the most frequently cited barrier, identified by more than one in every two participants (53%). Other barriers identified included lack of felt need (20%), distance to travel (15%), and lack of awareness (13%). In general, no significant influence of sex or type of VI on barrier selection was found. Location had a significant impact on the selection of several barriers. Pearson χ2 analysis indicated that participants from rural areas were found to feel disadvantaged regarding the distance to services (p ≤ 0.001) and adequacy of hospital services (p = 0.001).
Conclusions
For a comprehensive public sector refractive service to be successful in Mozambique, those planning its implementation must consider cost and affordability. A clear strategy for overcoming lack of felt need will also be needed, possibly in the form of improved advocacy and health promotion. The delivery of refractive services in more remote rural areas merits careful and comprehensive consideration.
Key Words: uncorrected refractive error, barriers, service uptake, eye health services, Mozambique
Mozambique has a population of more than 25 million people.1 Nampula Province has just fewer than 4 million people.2 Although Mozambique is currently experiencing unprecedented economic growth rates, buoyed by the discovery of natural resources, significant challenges remain for the population, such as adequate health care, including eye health services.
VISION 2020 is a global initiative to eliminate avoidable blindness by the year 2020. Its core strategies are focused on human resource development, infrastructure development, and disease control.3 The Mozambique Eyecare Project delivered a regional optometry model for Lusophone Africa, based on the VISION 2020 core strategies. A key output was a higher education program for optometry. Mozambique’s first professional optometrists graduated from Universidade de Lúrio in Nampula in 2013. To achieve the VISION 2020 goals, the services the optometrists are trained to provide must be fully implemented. To realize this potential, the use of refraction services by the general public must be fully understood.4
The body of evidence that exists in relation to the uptake of eye health services is limited. Research suggests that cost is the most significant barrier to eye health services.4–6 Indirect costs, such as transport, food, and lodgings, may also limit uptake.7 However, if cost as a barrier is removed, service uptake is not guaranteed.8 Even when eye health services are provided at no cost, not all patients choose to access them.9,10 In some instances, people with eye health needs may be unaware of free or subsidized services. A lack of information about the service may be as much of a barrier as cost.11 The significance of cost as a barrier may change with time. With ready-made spectacles, which provide a suitable correction for a significant proportion of refractive errors, now costing as little as $1 per pair to source, cost may no longer be a substantial barrier to usage for many subjects.12
Eye health services tend to be focused on urban areas of high population density, yet many people live in rural areas. Distance to services may therefore be a barrier.13 The journey to access services may be particularly difficult for those with visual impairment (VI). Gender must also be considered in this context. Unaccompanied travel for long distances may present different barriers for men and women in different societies.14 Entrenched cultural and religious beliefs may also present barriers.15 Whether these beliefs involve religion, ideas of destiny, or societal attitudes toward sex and gender, disability, or ethnicity, they may limit service uptake.13,16,17 The perception that vision loss is an untreatable and irreversible consequence of aging may also need to be countered.10
People may be unaware that they even have an eye health problem. A lack of awareness of general eye health and the interventions available may limit uptake. Those needing treatment may not understand the time needed for the intervention, the costs involved, whether it will hurt or not, and the chances of achieving a successful outcome.13 Eye health education and the provision of information may be key to overcoming these barriers.18 Quality of services will influence future uptake. Adequate health infrastructure and the suitability/quality of staff training are important determinants of the influence of such experience/outcome-related barriers.19 Bullying, ridicule, and peer victimization potentially may also limit service uptake or reduce compliance, particularly with regard to children with eye health problems.20 Strategies to improve the compliance of spectacle wear may be needed.21
Understanding the barriers to a refractive service will be central to the ultimate success of the intervention.22 This study has been designed to gain an understanding of the barriers to accessing refractive services perceived by the general population in Mozambique.
METHODS
A population-based cross-sectional study was conducted using two-stage cluster sampling in Nampula Province, Mozambique, between 2012 and 2013. This was completed alongside a Rapid Assessment of Refractive Error (RARE) study, designed to determine the prevalence of refractive error and presbyopia, assess spectacle coverage, and evaluate eye health–related quality of life perspectives among persons in Nampula, Mozambique.23 Rapid Assessment of Refractive Error studies are community-based cross-sectional studies that followed a standardized methodology, including the completion of a demographic questionnaire, a standardized ophthalmic assessment to determine refractive status and spectacle coverage, and a modified vision-related quality of life questionnaire to assess the impact of uncorrected refractive error (URE) on participant’s eye health status. Rapid Assessment of Refractive Error studies have been successfully used in other countries in the region, including Eritrea.24
For the current study, clusters were defined by the administrative level of “Bairro,” meaning neighborhood.2 There are 395 Bairros in Nampula province. As many as 76 Bairros were randomly selected for enumeration using a systematic random sampling method with probability proportional to size. A minimum of 60 participants were included per cluster. The calculation of sample size was based on several aspects including the required precision of the estimate, confidence levels, and the expected prevalence of refractive error, which was set at 5% of the population, as there was no formal estimate available. As the exact prevalence of refractive error was not known and statistical data for the population of Nampula province are limited, the sample of this study was set at a level to far exceed the necessary sample size required for the validation of the methodology. Cluster random sampling allowed 4601 subjects to be enumerated from the selected 76 clusters. The sampling was conducted in a manner that each subject participating has the same participation weight and an equal probability of selection; therefore, it is a self-weighting sample.
There is no single definition of urban or rural habitation.25 As such, an assessment was made for each cluster as to whether it was rural or urban based on a brief assessment of household access to treated water and electricity supply, population density, and the presence of surfaced roads.
To be included in the study, participants needed to be at least 15 years old, residing permanently at the address, and actively involved in making financial decisions in the household. Those people found to not meet these criteria were excluded.
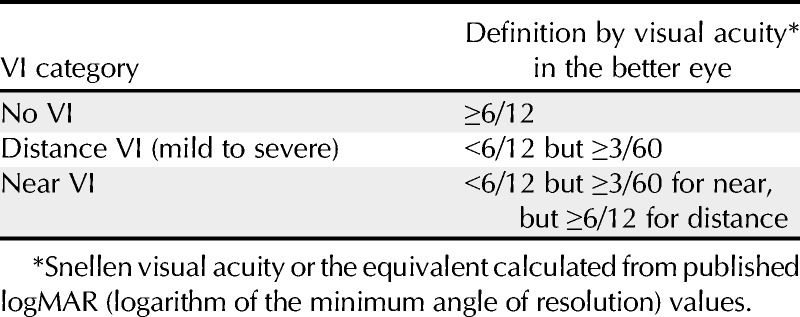
Participants were interviewed to establish barriers to the uptake of refractive services, using a precoded questionnaire. Visual acuity was assessed either by a qualified optometrist or by an optometry student enrolled at Universidade de Lúrio, Nampula, who had completed at least 2 years of study, under the supervision of a qualified optometrist. Visual impairment was defined using four categories as illustrated in Table 1.
TABLE 1.
Visual impairment category definition by visual acuity in the better eye26
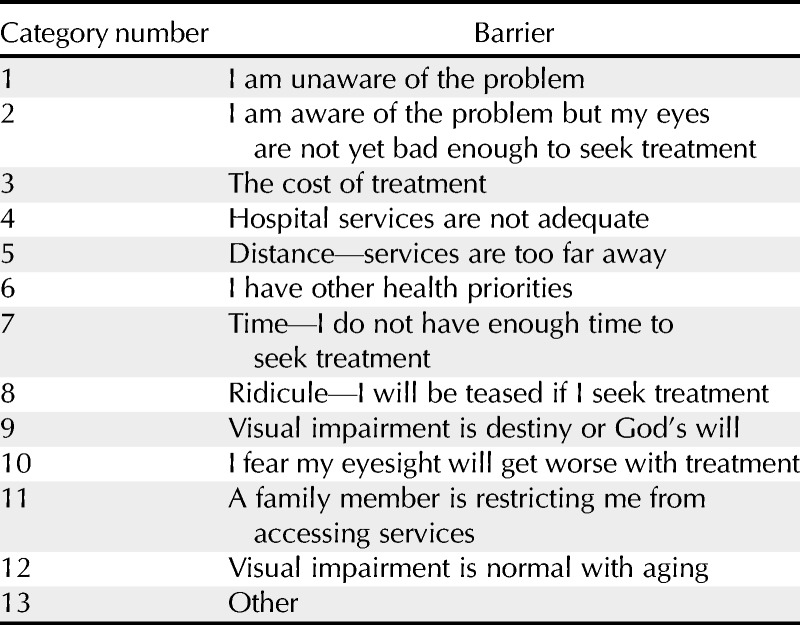
For each participant with confirmed VI, the barriers listed in Table 2 were presented in a randomized order. The barrier options presented were informed by existing relevant literature and stakeholder meetings involving social scientists, eye health professionals, students, and members of the public. The objective of the meetings was to ensure that the barriers were appropriate for the Mozambican context and that no other barriers needed to be included. A pilot study was conducted, which allowed for the protocol on enumeration, face-to-face interviews, clinical assessments, and data recording to be refined. It also allowed the suitability of the methodology to be verified and informed planning for the logistical requirements of the data collection. With the finalized questionnaire, participants were asked to select up to three barriers that represented their experience of accessing eye health services for refractive error. Participants were informed that if they felt strongly that they needed to select more barriers to reflect their experiences, they could do so. A subset of participants (25% of the total interviewed) were selected at random to answer questions on salaries and family finances.
TABLE 2.
Barriers
Ethics committee approval was granted for the study by the National Ethics Committee of Mozambique and under the Mozambique Eyecare Project (a joint initiative of the Dublin Institute of Technology, the University of Ulster, Universidade Lúrio, and the Brien Holden Vision Institute) by the Dublin Institute of Technology, Republic of Ireland. The research followed the tenets of the Declaration of Helsinki and informed consent was obtained from the subjects after an explanation of the study. Data were coded for anonymity. All data recorded were kept locked away. During the data collection phase, data were checked twice for consistency, once by an optometrist and once by a social scientist. An error log sheet was developed. Where possible, discrepancies were addressed in the field. The data were recorded in a custom database designed in Microsoft Excel. Data were analyzed using SPSS (version 21).
RESULTS
From the 4601 subjects enumerated, 1817 (39%) were from rural areas and 2784 (61%) were from urban areas. A total of 1087 (24%) people were found to have VI and were willing to participate by stating which barriers they perceived were restricting their access to refractive services. From the 3514 responses excluded, 3377 (96%) had no VI and 137 (4%) had VI but did not want to state barriers experienced. From those excluded, 1621 (46%) were male and 1893 (54%) were female. As many as 2050 (58%) were from urban areas as opposed to 1464 (42%) from rural areas.
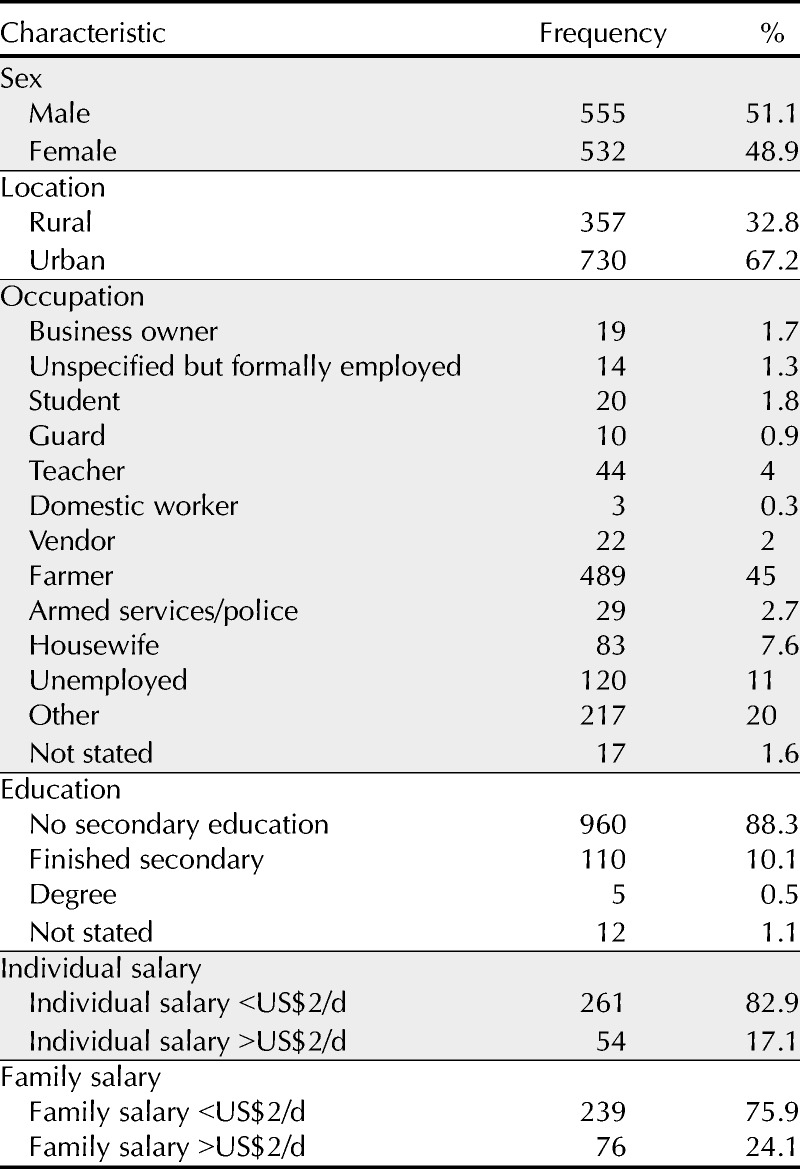
From the 4601 subjects enumerated, a subset of 1144 were asked about their financial situation. From that subset, only 315 participants who had given information on their financial situation were found to have VI and were willing to participate by stating which barriers they perceived were restricting their access to refractive services. The subset of participants that provided information on their financial situation was made up of 315 participants, equating to 29% of all the participants found to have VI and were willing to participate by stating which barriers. From the subset, as many as 192 (61%) participants in the subset came from rural areas, whereas 123 (39%) participants came from urban areas. As many as 176 (56%) participants from the subset were male, whereas 139 (44%) were female. Further details of participant characteristics are shown in Table 3.
TABLE 3.
Participant characteristics
The average (±SD) number of barriers cited per participant was 1.5 (±0.65), with a total of 1630 barriers cited in total. Only four participants selected more than three barriers, each citing four barriers.
Cost was the most frequently stated barrier, identified by 579 out of 1087 participants, equating to a positive response from 53% of the participants interviewed, and comprising 36% of the total barriers selected. A total of 304 participants (28%) stated that although they were aware of a problem, they felt it was not bad enough to seek treatment, equating to 19% of all responses. The distance to services was identified by 161 participants (15%) as a barrier, equating to 10% of all responses. Fig. 1 indicates the frequency that each barrier was stated. The response to two of the barrier options—fear of eyesight getting worse with treatment and a family member restricting access—equated to less than 1% of the responses for each. No solid conclusions could be drawn from such low frequency of responses; hence, these barrier options were not included in the statistical analysis.
FIGURE 1.
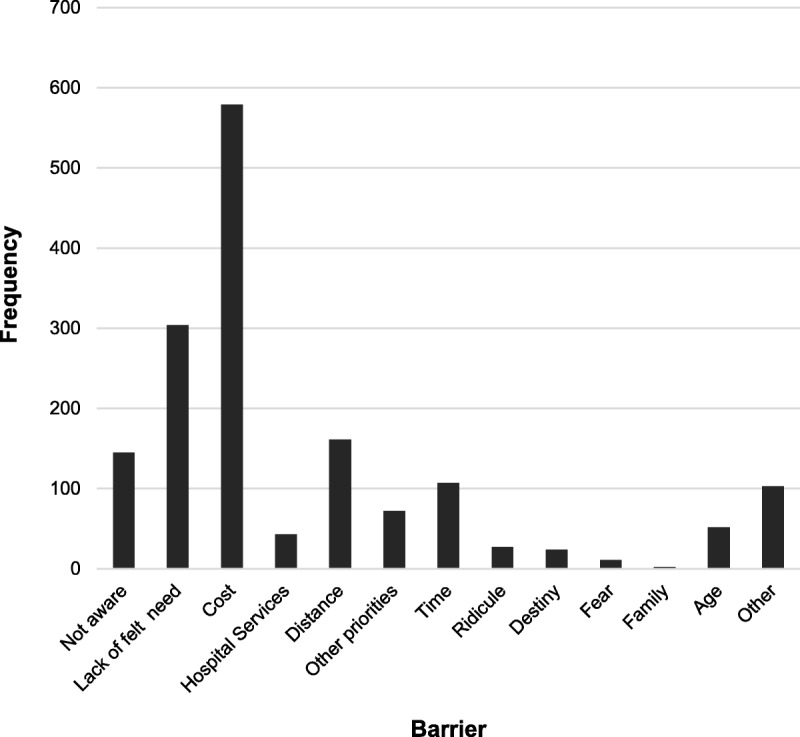
The figure demonstrates the frequency that each barrier to accessing refractive services in Mozambique was stated.
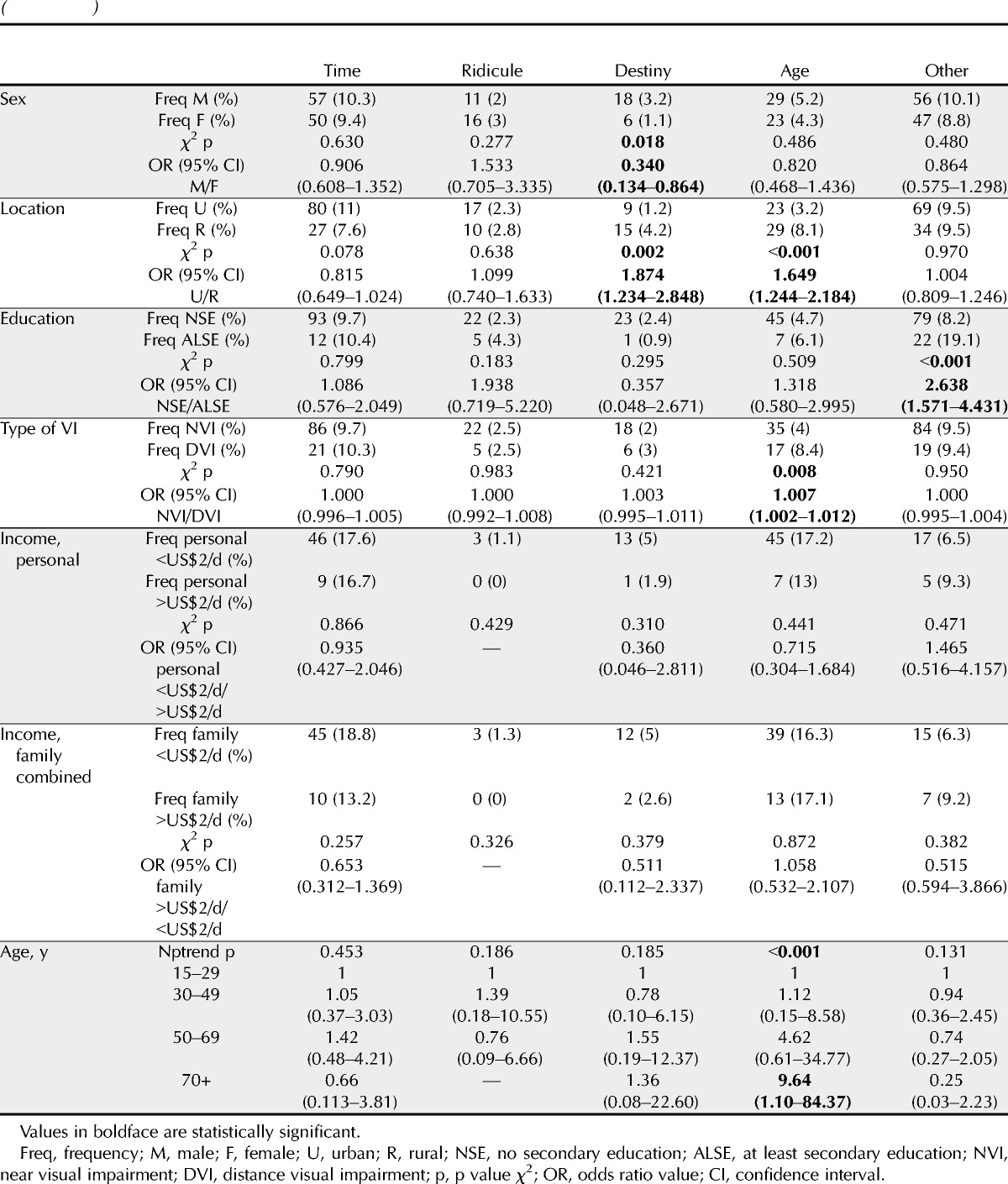
Pearson χ2 analysis indicated that sex did not have a significant association with the selection of barriers, other than the response that VI is destiny or God’s will (p = 0.018), with female subjects 0.34 (0.134 to 0.864) times less likely to report destiny or God’s will as a barrier compared with male subjects. However, the proportions of positive responses were relatively low; only 6 (1%) female subjects stated destiny/God’s will as a barrier, as opposed to 18 (3%) male subjects.
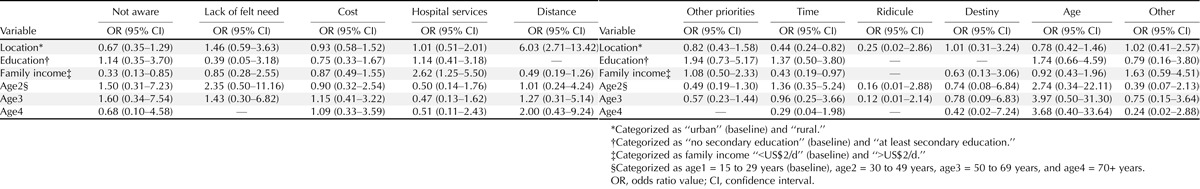
The location of the participant’s dwelling was found to have a significant association with six of the barriers selected. Participants from rural areas were found to feel disadvantaged regarding the distance (p < 0.001) and adequacy of hospital services (p < 0.001). Participants from rural areas were 2.13 (1.789 to 2.543) times and 1.64 (1.207 to 2.234) times more likely to report distance and adequacy of hospital services as a barrier compared with their urban counterparts, respectively. Also, significantly more rural participants stated being unaware (p = 0.002), destiny/God’s will (p = 0.002), and the perception that VI due to old age is untreatable or irreversible (p ≤ 0.001) as being barriers, although the frequencies for the latter two barriers were relatively low. Rural participants were 1.20 (1.000 to 1.433), 1.88 (1.234 to 2.848), and 1.65 (1.244 to 2.184) times more likely to report unawareness, destiny/God’s will, and the perception that VI due to old age is untreatable or irreversible as a barrier compared with their urban counterparts, respectively. However, significantly less rural-dwelling participants reported that their eyes were not bad enough to seek help (p ≤ 0.001) and they were 0.70 (0.602 to 0.818) times less likely to state that their eyes were not bad enough to seek help as a barrier compared with participants residing in the urban areas.
Formal secondary school education was found to be significantly associated with the reporting of being unaware (p = 0.016), cost (p = 0.014), distance (p = 0.005), and other (p ≤ 0.001) as barriers. Participants with at least secondary education were 0.39 (0.179 to 0.862), 0.62 (0.416 to 0.909), and 0.34 (0.156 to 0.749) times less likely to report unawareness, cost, and distance as a barrier, respectively. However, participants with at least secondary education were 2.64 (1.571 to 4.431) times more likely to report other barriers not included in the study. As many as 87% of urban dwellers had no secondary school education compared with 94% in rural areas, indicating that education provision to rural areas is worse than urban areas.
Stratification of participants according to whether they exhibited near or distance VI impacted significantly on stated barriers only for those that cited barriers including the following: aware of the problem but their eyes were not yet bad enough to seek treatment (p = 0.017), hospital services adequacy (p ≤ 0.001), other health priorities (p = 0.007), and those who stated that VI is normal with aging (p = 0.008). With regard to the strength and direction of association for the stated barriers, significant odds ratios are approximately equal to 1 (OR ≈ 1.00) showing that the odds are almost equal for both groups of participants exhibiting near or distance VI. As many as 261 (30%) participants with near VI stated that their eyes were not yet bad enough to seek treatment, as opposed to 43 (21%) participants with distance VI.
For the subset of participants that were asked about finances, personal income only had a significant impact on the barrier selection of hospital services adequacy (p = 0.004) and distance (p ≤ 0.001). Participants with a personal income of more than US$2 per day were 2.80 (1.362 to 5.757) times more likely to report adequacy of hospital services compared with those with a personal income of less than this value. On the other hand, participants with a personal income of more than US$2 per day were 0.10 (0.024 to 0.425) times less likely to report the distance to a service facility as a barrier compared with those with a personal income of less than this value. For family income, having a collective income of more than US$2 per day had a significant impact on the selection of the participant being unaware of a problem (p = 0.041), hospital services adequacy (p = 0.003), and distance (p ≤ 0.001) being selected as barriers. Participants with a collective family income of more than US$2 per day were 0.40 (0.164 to 0.987) and 0.22 (0.089 to 0.520) times less likely to report being unaware of the problem and distance as a barrier, respectively. However, participants with a collective family income of more than US$2 per day were 2.66 (1.357 to 5.201) times more likely to report hospital services adequacy as a barrier compared with participants with a collective family income of less than that value.
Trend analysis was conducted to test the relationship between age and the barriers selected. Results are as shown in Table 4; significant trends were obtained between ages and the following barriers: lack of felt need (p = 0.001), cost (p = 0.004), hospital services (p = 0.017), distance (p < 0.001), other priorities (p < 0.001), and VI is normal with aging (p < 0.001). Age odds ratios are in reference to the baseline age category of 15 to 29 years. Participants aged at least 70 years were 4.13 (1.37 to 12.43) and 9.64 (1.10 to 84.37) times more likely to report distance and that VI is normal with aging as a barrier compared with those aged between 15 and 29 years, respectively. On the other hand, participants aged at least 70 years are 0.18 (0.04 to 0.85) times less likely to report eyes are not bad enough to seek treatment compared with participants aged between 15 and 29 years. In addition, participants aged between 50 and 69 years are 1.88 (1.01 to 3.52) times more likely to report cost.
TABLE 4.
Statistical analysis
Multivariate analysis using logistic regression was used to establish the adjusted odds ratios for the following explanatory variables controlling for potential confounding: location, education, collective family income, and age. Models considered are shown in Table 5. After adjusting for education, income, and age, participants residing in rural areas were 6.03 (2.71 to 13.42) times more likely to report distance as a barrier. However, participants residing in rural areas were 0.44 (0.24 to 0.82) times less likely to report time as a barrier. The remaining results in Table 5 show insignificant results or significant results within the confidence intervals of the previous results stated in Table 4.
TABLE 5.
Logistical regression
DISCUSSION
The results of this study provide a clear indication that the perceived cost of spectacles and spectacle services comprises the most substantial barrier to uptake of refractive services in Nampula, Mozambique. Neither sex, location, nor VI type had a significant impact on who selected cost as a barrier, suggesting that positive responses for cost came from participants from a variety of situations and backgrounds. These findings are in general agreement with the existing body of evidence that identifies cost or affordability as the major barrier to uptake of eye health services.4–6,12 The personal and family financial situations of participants were found not to have an association with cost being stated as a barrier, indicating it is perceived as a barrier to both advantaged and disadvantaged families. However, wealth may be relative and should be considered in context. For example, a family considered advantaged in Mozambique may not be considered advantaged in neighboring South Africa.
Participants with either a personal income or a combined family income of more than US$2 per day were found to be more likely to report adequacy of hospital services compared with those with a personal income of less than this value. This may reflect their desire to get value for the resources they may allocate to improving their vision. Participants who have less resources may be relying on charity to cover their medical costs, and so feel less entitled to a good quality service. Participants with a personal income or a combined family income of more than US$2 per day were also found to be less likely to report the distance to a service facility as a barrier, perhaps explained by their means to pay for transport.
For refractive services in Mozambique to be fully equitable, they should be available to everyone, regardless of their ability to pay. A policy may be needed to ensure that the most vulnerable members of society can, for example, access subsidized care. A cross subsidization system would allow funds generated through provision of services to wealthier patients to facilitate refractive services to the poor. The Aravind Eye Care System in India has successfully adopted this approach for many years.27 More research is needed to establish if a similar system would be suitable for implementation in the Mozambican context bearing in mind that the health system is more government focussed in the Mozambique. This creates policy and political challenges whereby governments are averse to income generation strategies. It is clear that careful planning, as well as innovative thinking, is needed if the barrier of cost is to be overcome. The value of social entrepreneurial models has been described in other low-income settings and can result in the expansion of services and poverty reduction.28 Such strategies that seek to mobilize optometrists through an ownership program with affordability restrictions on pricing should be investigated.
Refractive error was selected as a VISION 2020 priority condition, not only because of the burden of VI that it represents but also because of how easily and affordably it can be treated.29,30 Ready-made spectacles are suitable for correcting a significant proportion of refractive errors, most notably presbyopia. With ready-made spectacle now being available for a few dollars per unit, cost should become less of a barrier.12 This is particularly pertinent for the most vulnerable groups in any society.
Affordability must be considered, however, as well as cost. Affordability depends as much on the cost of preserving sight as it does on the degree the patient prizes his or her sight and the ability for it to be paid for.8 The authors are currently working on a willingness-to-pay study, which will provide a greater understanding of affordability for refractive services in Mozambique. Early-stage analysis indicates that mean willingness-to-pay values ranged from US$12 to US$15.
In all countries and contexts, eye health costs money. Where possible, eye health services should be able to stand alone in terms of covering expenditure. There is the potential for the burden of URE to be vastly reduced or eliminated by developing self-sustainable systems including for human resources development and delivery of spectacles.30 If the returns on the service provided do not cover the costs, there is reason for concern.31 In the long term, stability can only be guaranteed through high indigenous local demand.8 The more people that benefit from a service, the more likely it is to be cost-effective.32
Efficient use of resources can also affect affordability. The refractive service offered should be of the best possible quality. Improving quality may involve initial investment but will save money in the long term. Many improvements can come at low or no cost, such as a change in standard operating procedures for the eye health team to make the service they provide more efficient. Although this study found that the adequacy of refractive services was only stated as a barrier by 4% of participants, offering poor quality services is a waste of resources. It may also damage future or repeat uptake of the services on offer and may fail to deliver on the opportunity to eliminate cases of avoidable blindness.27 Strong leadership and good management, including the use of best practice business techniques, will be essential to the success of the refractive service system.33–35 Further research and planning are needed to understand and maximize the benefits of the establishment of a professional board of optometry, clinical competency framework, and regulatory body for the fledgling profession of optometry in Mozambique.
The high proportion of subjects citing lack of felt need as a perceived barrier suggests that investment to address the advocacy needs around eye health and to highlight the benefits of addressing refractive error would seem prudent. The findings also suggest that the advocacy needs are particularly important among those with near VI, who appear more likely, compared with those with distance VI, to suggest a lack of felt need. Such a difference might be explained, at least in part, by the possibility that near VI may create a less severe impact on functionality or participation in everyday life and may also be grounded in the belief that such visual loss is a normal aspect of aging. Although improving the vision of patients with URE will likely improve their lives, the lack of felt need suggests that outcomes of refractive services may be less dramatic than the outcomes of other eye health interventions, such as cataract surgery. However, as several studies have shown, the impact of correcting refractive error on productivity makes it a worthwhile intervention.36–38 Increased advocacy and education can serve to maximize the societal benefit achieved.
The finding that people from rural locations perceived themselves to be disadvantaged by the distance and adequacy of hospital services was predictable given that eye health services are mostly centered in urban locations. Poor infrastructure and limited transport options exacerbate the problem. The necessity to provide dedicated refractive services to all rural populations who live outside the urban catchment area of health and social services provides a challenge.22,39,40 This is particularly pertinent to Mozambique, where limited financial and material resources reduce the ability of the people living rurally to get the eye care they need.
It is also possible that rural dwellers felt they would be discriminated against if they accessed urban-based services, on the grounds of where they live. More research is needed on the impact of the rural/urban cultural divide and how location may negatively influence access to services. For a service to be universal, all patients must be treated appropriately and equally. If the VISION 2020 objective of eliminating the main causes of avoidable blindness by the year 2020 is to be met, the distribution of refractive services within Mozambique must take into account the needs of those in rural areas.
Significantly more rural participants were also more likely to state they were unaware they had a problem than urban participants, suggesting that eye health advocacy efforts in rural areas need to be strengthened. Also, significantly more rural participants stated the perception that VI for old age is untreatable or destiny/God’s will as being barriers—possibly explained by those living in rural areas generally having more traditional views and less education than those in urban areas. These barriers, along with fear of eyesight getting worse if treated and/or a family member restricting access, may be associated with entrenched cultural traditions or a lack of information about eye health services. Fear of ridicule also falls into this bracket, although anecdotal evidence from Mozambique suggests many people regard wearing spectacles as a mark of prosperity, resulting in people wearing them to boost their status in society, even if they do not really need them.
Cultural or belief-based barriers of this sort have been described in other studies as “difficult to change,” as they may require a sustained long-term effort by the subject, communities, and the service provided to overcome the challenge.4 The results indicate that in Nampula, despite these barriers being more commonly identified with people in rural areas, in the wider context, these are not the most pressing barriers to uptake of refractive services. Collectively, these five barriers were only selected by 10% of participants. This indicates that Mozambican society (or at least those people residing in Nampula) would have limited social or cultural reservations to using refractive services, were they accessible. This is encouraging, particularly when considered alongside the finding that there was not a strong association between sex in Mozambique and stated barriers, as it suggests that Mozambican society has relatively progressive views on correcting refractive error and wearing spectacles when they are needed. It should be noted that female subjects were 0.34 times less likely to report destiny as a barrier compared with male subjects, although the proportions of positive responses were relatively low.
Elderly patients were found to be more likely to report distance as a barrier, compared with younger participants. As people get older, their mobility may be reduced, making them less able to travel to health facilities. The needs of older people will need to be considered when planning eye health services.
Participants without a formal secondary school education were found to be more likely to be unaware of the problem and more concerned with cost. This is understandable on the basis that they are potentially less likely to understand about eye health and their income would likely be lower than those who are educated. However, as shown above, income did not appear to influence cost being selected as a barrier. More research is needed to explore this relationship. Those without secondary education were also found to be less likely to report distance as a barrier. This relationship may be linked to their increased likelihood of being unaware of the problem.
The RARE for Mozambique found that URE prevalence was 2.6% (95% CI, 2.1 to 3.2%), with spectacle coverage of 0%. Presbyopia prevalence was 25.8% (95% CI, 12.0% to 30.5%), with only 2.2% spectacle coverage.23 By way of comparison, the RARE study in Eritrea found that URE prevalence was 6.4% (95% CI, 5.6 to 7.2%) with spectacle coverage of 22.2%, whereas for presbyopia, prevalence was 32.9% (95% CI, 30.3 to 35.7%) with spectacle coverage of 9.9%.24 Comparing RARE results indicates how inaccessible refractive error services are in Mozambique compared with Eritrea. Spectacle coverage is unacceptably low and the results of this current study suggest that cost is the main barrier to explain why this is the case.
In 2011, a Rapid Assessment of Avoidable Blindness (RAAB) study was completed in Nampula Province. The RAAB is a relatively simple, cheap, and rapid survey methodology to provide data on avoidable blindness. It includes assessing the visual acuity of people who are 50 years and older, where prevalence of blindness is the highest. The RAAB study included an analysis of the barriers to cataract surgery. The cost of transport was found to present a significant challenge, accounting for 75% of all barriers stated. Other barriers included lack of awareness on possibility of treatment (9.9%) and believing that blindness is an irreversible result of aging (5.9%).41 Despite differing methodologies, like the current study, the RAAB found that people in Nampula stated that cost is the most significant barrier, preventing them from accessing required eye health services. However, results from a RAAB study completed in 2014 in Sofala Province in central Mozambique found that being unaware that treatment is possible for cataracts was the most frequently stated barrier.42 This was stated by more than 35% of female subjects and more than 25% of male subjects. Cost of surgery was only stated by less than 5% of female subjects and by no male subject. The comparison with the Sofala RAAB suggests that there may be regional variations in access to eye health services. Further research is needed to explore these variations.
In hindsight, the methodology of the current study would have been made more robust if the participants had been asked to rank their selected barrier choices. As many as 455 out of 1087 participants selected two or more barriers. Applying a ranking system to the responses of these participants would have allowed a deeper analysis of the barriers to uptake of refractive services.
CONCLUSIONS
Cost and affordability are the most significant barriers to uptake of refractive services in Mozambique, comprising more than 35% of all responses and identified by more than half of all participants. The RARE study conducted in tandem with this investigation confirms that the barriers to spectacle services are currently not just perceived but are very real in Mozambique. A spectacle coverage rate of 0% for URE and 2.2% for presbyopia compares very unfavorably with observations in other sub-Saharan countries and highlights the inaccessibility of refractive services in the Nampula region, which are likely reflective of the broader situation in Mozambique (and potentially Lusophone Africa). A greater understanding of attitudes toward cost and affordability of refractive services is needed. The results from this study on the barriers to refractive services uptake, along with the prevalence data from the Mozambican RARE, will be critical to the national planning of refractive error services.
Stephen Thompson
Dublin Institute of Technology
Optometry Department, Kevin St
Dublin 8
Republic of Ireland
e-mail: stephenjamesthompson@hotmail.co.uk
ACKNOWLEDGMENTS
This research was produced as part of the Mozambique Eyecare Project, which is funded by Irish Aid. Funding and support were also provided by the Mozambique Eyecare Project partners and the Institute of Development Studies. The authors thank the African Vision Research Institute for its support.
Received May 29, 2014; accepted July 29, 2014.
REFERENCES
- 1.World Bank. Data on Mozambique: 2013. Available at: http://www.worldbank.org/en/country/mozambique. Accessed May 25 2014.
- 2.Mozambique National Institute of Statistics. Population/total population. Nampula (2007). Available at: http://www.ine.gov.mz/en/. Accessed May 25, 2014.
- 3.World Health Organization. Action Plan for the Prevention of Avoidable Blindness and Visual Impairment, 2009-2013. Available at: http://www.who.int/blindness/ACTION_PLAN_WHA62-1-English.pdf. Accessed September 16, 2014.
- 4. Marmamula S, Keeffe JE, Raman U, Rao GN. Population-based cross-sectional study of barriers to utilisation of refraction services in South India: Rapid Assessment of Refractive Errors (RARE) Study. BMJ Open 2011; 1: e000172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kuper H, Polack S, Eusebio C, Mathenge W, Wadud Z, Foster A. A case-control study to assess the relationship between poverty and visual impairment from cataract in Kenya, the Philippines, and Bangladesh. PLoS Med 2008; 5: 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Laviers H, Burhan I, Omar F, Jecha H, Gilbert C. Evaluation of distribution of presbyopic correction through primary healthcare centres in Zanzibar, East Africa. Br J Ophthalmol 2011; 95: 783– 7. [DOI] [PubMed] [Google Scholar]
- 7. Melese M, Alemayehu W, Friedlander E, Courtright P. Indirect costs associated with accessing eye care services as a barrier to service use in Ethiopia. Trop Med Int Health 2004; 9: 426– 31. [DOI] [PubMed] [Google Scholar]
- 8. Sommer A. Toward affordable, sustainable eye care. Int Ophthalmol 1994; 18: 287– 92. [DOI] [PubMed] [Google Scholar]
- 9. Preslan MW, Novak A. Baltimore Vision Screening Project. Phase 2. Ophthalmology 1998; 105: 150– 3. [DOI] [PubMed] [Google Scholar]
- 10. Keeffe JE, Weih LM, McCarty CA, Taylor HR. Utilisation of eye care services by urban and rural Australians. Br J Ophthalmol 2002; 86: 24– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dandona R, Dandona L, Naduvilath TJ, McCarty CA, Rao GN. Utilisation of eyecare services in an urban population in southern India: the Andhra Pradesh eye disease study. Br J Ophthalmol 2000; 84: 22– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ramke J, du Toit R, Palagyi A, Brian G, Naduvilath T. Correction of refractive error and presbyopia in Timor-Leste. Br J Ophthalmol 2007; 91: 860– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lewallen S, Courtright P. Blindness in Africa: present situation and future needs. Br J Ophthalmol 2001; 85: 897– 903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gurung R. Cataract surgical outcome and gender-specific barriers to cataract services in Tilganga Eye Centre and its outreach microsurgical eye clinics in Nepal. Community Eye Health 2007; 20: 14– 5. [PMC free article] [PubMed] [Google Scholar]
- 15. Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ 2008; 86: 63– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ebeigbe JA. Traditional eye medicine practice in Benin-City, Nigeria. S Afr Optom 2013; 72: 167– 72 Available at: http://www.saoptometrist.co.za/EBEIGBE_DEC2013.pdf. Accessed September 16, 2014. [Google Scholar]
- 17. George A, Iyer A. Unfree markets: socially embedded informal health providers in northern Karnataka, India. Soc Sci Med 2013; 96: 297– 304. [DOI] [PubMed] [Google Scholar]
- 18. Abdullah KN, Al-Sharqi OZ, Abdullah MT. Barriers to the uptake of eye care services in developing countries: a systematic review of interventions. Heal Educ J 2013; 72: 742– 54 Available at: http://hej.sagepub.com/content/72/6/742. Accessed September 16, 2014. [Google Scholar]
- 19. Taylor HR, Keeffe JE. World blindness: a 21st century perspective. Br J Ophthalmol 2001; 85: 261– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Carlton J, Karnon J, Czoski-Murray C, Smith KJ, Marr J. The clinical effectiveness and cost-effectiveness of screening programmes for amblyopia and strabismus in children up to the age of 4–5 years: a systematic review and economic evaluation. Health Technol Assess 2008; 12: iii, xi-194. [DOI] [PubMed] [Google Scholar]
- 21. O’Donoghue L, McClelland JF, Logan NS, Rudnicka AR, Owen CG, Saunders KJ. Refractive error and visual impairment in school children in Northern Ireland. Br J Ophthalmol 2010; 94: 1155– 9. [DOI] [PubMed] [Google Scholar]
- 22. Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ 2001; 79: 237– 43. [PMC free article] [PubMed] [Google Scholar]
- 23. Loughman J, Nxele L, Faria C, Thompson S, Ramson P, Chinanayi F, Naidoo K. Prevalence of refractive error, presbyopia and spectacle coverage in Nampula District, Mozambique: A Rapid Assessment of Refractive Error Study. J Visual Impair. Submitted. [Google Scholar]
- 24. Chan VF, Mebrahtu G, Ramson P, Wepo M, Naidoo KS. Prevalence of refractive error and spectacle coverage in Zoba Ma’ekel Eritrea: a rapid assessment of refractive error. Ophthalmic Epidemiol 2013; 20: 131– 7. [DOI] [PubMed] [Google Scholar]
- 25.United Nations Statistics Division. Population Density and Urbanization: 2013. Available at: http://unstats.un.org/unsd/demographic/sconcerns/densurb/densurbmethods.htm. Accessed May 25, 2014. [Google Scholar]
- 26. Bourne R, Price H, Taylor H, Leasher J, Keeffe J, Glanville J, Sieving PC, Khairallah M, Wong TY, Zheng Y, Mathew A, Katiyar S, et al. New systematic review methodology for visual impairment and blindness for the 2010 Global Burden of Disease study. Ophthalmic Epidemiol 2013; 20: 33– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lindfield R, Foster A. Is quality affordable? Community Eye Health 2008; 21: 53– 5. [PMC free article] [PubMed] [Google Scholar]
- 28. Naidoo KS, Jaggernath J. Uncorrected refractive errors. Indian J Ophthalmol 2012; 60: 432– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Holden BA, Resnikoff S. The role of optometry in vision 2020. Community Eye Health 2002; 15: 33– 6. [PMC free article] [PubMed] [Google Scholar]
- 30. Holden BA, Sulaiman S, Knox K. The challenge of providing spectacles in the developing world. Community Eye Health 2000; 13: 9– 10. [PMC free article] [PubMed] [Google Scholar]
- 31. Smith AF. Ophthalmic services research: towards increasing the role of economic and operations research methods in the delivery of eye care services. Br J Ophthalmol 1995; 79: 515– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Baltussen R, Sylla M, Mariotti SP. Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull World Health Organ 2004; 82: 338– 45. [PMC free article] [PubMed] [Google Scholar]
- 33. Smith AF, Smith JG. The economic burden of global blindness: a price too high! Br J Ophthalmol 1996; 80: 276– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rahmathullah R, Barrows J, Sheffield VM. Making refractive error services sustainable: the International Eye Foundation model. Community Eye Health 2007; 20: 45– 6. [PMC free article] [PubMed] [Google Scholar]
- 35. Taylor HR, Pezzullo ML, Nesbitt SJ, Keeffe JE. Costs of interventions for visual impairment. Am J Ophthalmol 2007; 143: 561– 5. [DOI] [PubMed] [Google Scholar]
- 36. Frick KD, Foster A. The magnitude and cost of global blindness: an increasing problem that can be alleviated. Am J Ophthalmol 2003; 135: 471– 6. [DOI] [PubMed] [Google Scholar]
- 37. Frick KD, Foster A, Bah M, Faal H. Analysis of costs and benefits of the Gambian Eye Care Program. Arch Ophthalmol 2005; 123: 239– 43. [DOI] [PubMed] [Google Scholar]
- 38. Smith TS, Frick KD, Holden BA, Fricke TR, Naidoo KS. Potential lost productivity resulting from the global burden of uncorrected refractive error. Bull World Health Organ 2009; 87: 431– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kovai V, Krishnaiah S, Shamanna BR, Thomas R, Rao GN. Barriers to accessing eye care services among visually impaired populations in rural Andhra Pradesh, South India. Indian J Ophthalmol 2007; 55: 365– 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ho VH, Schwab IR. Social economic development in the prevention of global blindness. Br J Ophthalmol 2001; 85: 653– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kimani K. Rapid Assessment of Avoidable Blindness (RAAB) Nampula Province, Mozambique. Sightsavers International; 2011. [Google Scholar]
- 42. Bedri A. RAAB study in Mozambique helps better planning of eye health services. Vis Devel 2014; 1: 8– 9. [Google Scholar]


