Abstract
Objectives:
The purpose of this clinical trial was to explore whether lubiprostone increases the rate of mucus and mucin secretion and its viscosity in chronic constipation (CC) patients. The secretion of chloride (CS) into the gastrointestinal tract lumen is pivotal in the body's ability to process non-digestible food components. CS sets the optimal rate of hydration for non-digestible food components, their fluidity, and their adequate propulsion along the alimentary tract. Chloride is also instrumental in the secretion of alimentary tract mucus, and the formation of a gel-like, viscous mucus-buffer layer. This layer acts as the first line and vanguard of the mucosal barrier. This barrier is essential in mucosal lubrication and protection. Lubiprostone, a novel chloride channel stimulator ClC-2, is currently approved for the treatment of CC. Its impact on mucus, mucus secretion, and viscosity is not established.
Methods:
A double-blind, crossover trial was approved by the IRBs at the Kansas University Medical Center (Kansas City, KS) (study site) and at the Texas Tech University HSC (El Paso, TX) (analysis site). The study included 20 patients (17 females (F); mean age: 37 years) with symptoms of CC diagnosed according to the Rome III criteria. Patients were randomized to 1 week of therapy with lubiprostone or placebo followed by a 1 week washout and 1 week of the alternative therapy. Gastric juice was collected basally and during stimulation with pentagastrin (6 μg/kg body weight subcutaneously) at the end of weeks 1 and 3. Pentagastrin stimulation mimics food stimulation. The mucus content in gastric juice was assessed gravimetrically. The mucin content was measured after its purification using ultracentrifugation. The viscosity of the gastric secretion was measured using a digital viscometer.
Results:
In comparison with placebo, the volume of gastric secretion in patients with CC during administration of lubiprostone increased significantly by 50% (86.3 vs. 57.5 ml/h) (P<0.001) in basal conditions and increased by 25% (210.0 vs. 167.6 ml/h) (P=0.024) during stimulation with pentagastrin. The rate of gastric mucus secretion during therapy with lubiprostone was 91% higher (257.3 vs. 135 mg/h) (P=0.001) in basal conditions and 28% higher (348.1 vs. 270.8 mg/h) (NS) in stimulated conditions, although the latter was not statistically significant. The rate of gastric mucin secretion during lubiprostone therapy was 85% higher (98.4 vs. 65.5 mg/h) (P=0.011) in basal conditions and 38% (98.3 vs. 71.7 mg/h) (NS) higher in stimulated conditions. In basal conditions, the viscosity of gastric secretion during administration of lubiprostone increased by 240% at the lowest (P<0.001) and by 106% at the highest shear rate (P<0.001). In stimulated conditions, it increased by 226% (P<0.01) at the lowest shear rate and by 67% (P<0.01) at the highest shear rate.
Conclusions:
The significantly higher content of gastric mucus and mucin during therapy in basal conditions with lubiprostone in patients with CC suggests and supports the potentially leading role of lubiprostone and ClC-2 stimulation in their secretion. This increased stimulation results in profoundly increased viscosity, which in turn facilitates and/or accelerates the transit and evacuation of non-digestible food components. Although increases in mucus and mucin were observed in stimulated conditions, neither increase was statistically significant. Based on this experiment, we hypothesize that, in CC patients, the significantly increased rate of mucus and its major component, mucin secretion, during lubiprostone administration may partially explain its clinical effectiveness and also have additional clinically important effects. We propose that since the increased mucus production enhances the protective quality of the mucosal barrier, it also boosts its potential to withstand luminal aggressive components such as acid/pepsin duet, Helicobacter pylori and/or nonsteroidal anti-inflammatory drugs/aspirin, or a combination of all. Further trials are needed to test this hypothesis. As this was crossover clinical trial, the patients serve as their own controls. No interaction was found with body mass index (BMI) and treatment. The observed relationships of BMI and mucus and mucin secretions and gastric juice volume are important considerations in the design of future trials, particularly if a crossover design is not used.
Introduction
The alimentary tract mucosa is covered by an ~200-μm-thick viscoelastic mucus-buffer layer.1, 2, 3, 4 This mucus-buffer layer protects a delicate surface epithelium from various luminal chemical and physical aggressive factors. It also provides lubrication and facilitates propagation and propulsion of non-digestible food solids, as well as their evacuation, with a bowel movement.3, 4, 5, 6, 7, 8 There is a close relationship between the rate of mucus release from the mucous cells and the rate of chloride secretion. This relationship sets the optimal conditions for the hydration of mucus and formation of its viscoelastic gel layer.7, 8, 9, 10, 11, 12, 13
Chronic constipation (CC) is one of the most common gastrointestinal complaints. The prevalence of CC may reach 30% in general practice.14, 15 Available treatments are generally suboptimal owing to the lack of sustained efficacy or associated side effects.16, 17, 18
A novel chloride channel ClC-2 activator, lubiprostone, was approved and marketed in 2006.19, 20, 21, 22 Lubiprostone targets chloride secretion, which is an important pathogenic link that leads to CC.23, 24, 25, 26
The current trial was conducted to investigate the relationship of lubiprostone with gastric mucus secretion and mucin in CC patients. For this purpose, three hypotheses were tested:
Hypothesis 1: The administration of lubiprostone results in a significant increase of gastric mucus secretion in CC patients. Mucus secretion increases by at least 40% after 1 week of therapy.
Hypothesis 2: The administration of lubiprostone augments the secretion of gastric mucus glycoprotein, that is, mucin is the major component of mucus that defines the viscosus and lubricating properties of gastric mucus.
Hypothesis 3: The viscosity of the alimentary tract secretion, represented predominantly by its content of mucus and mucin, can be augmented during the administration of lubiprostone.
Our hypotheses, if confirmed in this and subsequent trials, may open new therapeutic avenues for lubiprostone in CC as an agent that improves mucus-driven lubrication and the protective barrier. As a result, lubiprostone may also prevent nonsteroidal anti-inflammatory drug and other drug-induced adverse events within the alimentary tract.
Methods
Patients
This study, supported by a grant from Takeda Pharmaceuticals International (Deerfield, IL), was approved by the IRBs at the Kansas University Medical Center (Kansas City, KS; October 2007, no. 07-022L) and at the Texas Tech University Health Sciences Center, PLF School of Medicine (El Paso, TX; April 2012, no. 00000098). All investigated subjects signed informed consents. The patients included in this study were seen at the Kansas University Medical Center.
Twenty patients, Helicobacter pylori negative, with chronic idiopathic constipation (17 females and 3 males; age range: 18–65 years), recruited according to the Rome III inclusion criteria, completed this randomized, double-blind, placebo-controlled crossover study.
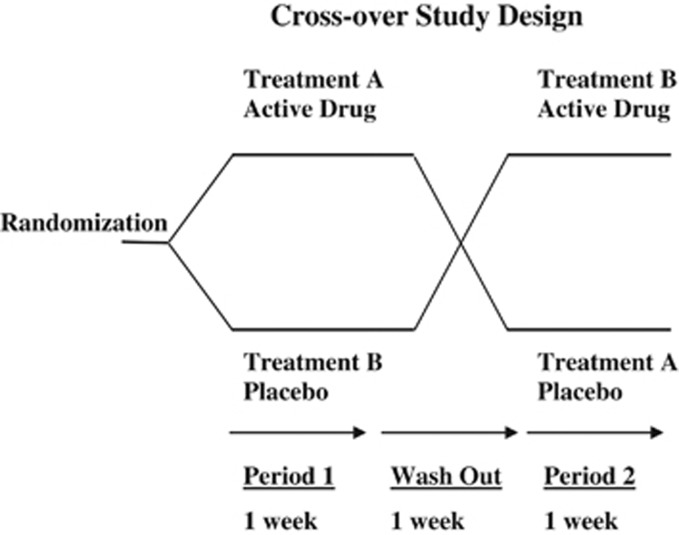
We used block randomization, with a block size of 5. An independent researcher, not involved in the clinical aspects of this trial, supervised the randomization schedule. Ten subjects (2 × 5) followed Arm A and 10 subjects (2 × 5) were assigned to Arm B (Figure 1).
Figure 1.
Double-blind, randomized, placebo-controlled crossover study design.
The double-blind aspect was preserved by the use of identical study medication (capsules) supplied by the sponsor (Takeda Pharmaceuticals International, Deerfield, IL). All study personnel remained blinded to the medication.
Exclusion criteria
Currently, pregnant or lactating women; subjects unwilling to practice adequate contraception throughout the period from screening through 14 days after study termination.
Use of laxatives 3 days immediately before randomization (except fiber or bulking agents).
Use of any of the following drugs within 3 days before randomization: prokinetic agents, medication containing opiates, anti-spasmodics, and illegal drugs.
Regular consumption of two or more drinks of alcohol per day.
Chronic nonsteroidal anti-inflammatory drug use.
Chronic use of an H2 receptor antagonist or proton pump inhibitor within 14 days before screening.
History of gastric or duodenal ulcer, chronic non-ulcer dyspepsia, or inflammatory bowel disease.
Type 1 diabetes.
Parkinson's disease.
Existence of any medical condition that requires chronic therapy.
Positive H. pylori serology.
Therapeutic intervention
Patients were randomly assigned to 1 week of lubiprostone (24 μg two times per day) or identically appearing placebo (one capsule two times per day), followed by a 1 week washout period and a second week of the alternative therapy.
Methods
The FlexSure (SmithKline Diagnostics) serologic test was performed for the evaluation of H. pylori status during the screening procedure. A urine pregnancy test was performed on female patients who were within a child-bearing age range.
Gastric secretion collection and analysis
Samples of gastric juice were collected at the end of both weeks of administered treatment.13 On the seventh day of assigned treatment, the patient was asked to fast overnight. The last test dose was administered 1.5 h before the onset of gastric juice collection. Subjects were intubated with a 14 French size nasogastric tube, Argyle Salem Sump, with radiopaque sentinel line and eye (Sherwood Medical, St Louis, MO). The tip of the tube was positioned in the dependent portion of the antrum.13 After complete aspiration of residual gastric juice, a water recovery test was conducted to assure the optimal position of the tube for aspiration of de novo elaborated secretion (95% recovery required).13
If the tube was positioned correctly, gastric secretion was collected with intermittent suction (−125 mm Hg) using a Vacutron Suction Regulator (Allied Healthcare Products, St Louis, MO). Gastric secretion volume per hour was recorded to the nearest 1 ml13 during 1 h at basal conditions and 1 h after administration of pentagastrin (6 μg/kg subcutaneously),
A measure of 0.5 ml of basal and pentagastrin-stimulated fresh gastric juice was placed in LVDVIIPlusPro Cone/plate viscometer (Brookfield Engineering Laboratory, Middleton, MA) and its viscosity was measured at shear rates between 2 and 16 (corresponding to speeds of 0.3 and 60 r.p.m.). The results were converted to centipoise (cP).
The remaining samples of gastric juice, after collection and recording of pH, were neutralized from their starting pH to a final pH of 7.0. This was accomplished using gradually decreasing molarities of NaOH, starting from 1 to 0.01 M, so that the final volume of gastric juice after pH adjustment never increased above 1% of its starting volume value.
The content of gastric mucus in aspirated secretion was measured after exhausting dialysis (with Spectra/Por CE DispoDialyzer of 1000 D cutoff) using a Spectra/Por EZ-1 Multidialyzer (Spectrum Laboratories, Rancho Dominguez, CA) and subsequently lyophilized using a freeze dryer. The final results of freeze-dried mucus weight were calculated in mg/h of gastric juice collection.
The measurements of gastric mucin within the freeze-dried mucus were performed using a TI swinging rotor in preparative ultracentrifuge (Model Optima LE-80K; Beckman Coulter Instruments, Palo Alto, CA).1, 13 Mucin was measured after its isolation and purification by equilibrium density-gradient ultracentrifugation in 46% (w/v) cesium chloride in a 0.05 M phosphate buffer–0.15 M NaCl for 48 h at ~280,000 g. The final results of the subsequently obtained freeze-dried mucin weight were calculated in mg/h of gastric juice collection.
Data processing and statistical analysis
Data are presented in basal conditions and after stimulation with pentagastrin during administration of placebo or lubiprostone. Based on studies by this laboratory,13 we calculated power to test a 40% increases in mucus production with a P=0.05 and power=0.90. The power calculation predicted that 17 patients were required. We included 20 patients to cover the possibility of dropouts.
Statistical significance was assessed by applying general linear equations, which included therapy, treatment sequence, age, and body mass index (BMI). BMI is a score calculated as follows: person's weight in pounds, multiplied by 703, divided by their height in inches squared. The score is numerical and does not have a dimension.
An α of 0.05 (two-sided) (β=0.80) was used to assess statistical significance. Statistical analyses were conducted using SPSS, version 20 (IBM, SPSS, Armonk, NY).
Results
Participants were primarily Caucasian (18/20=90%) females (17/20=85%) with an average age of 37.4 years (range: 18–65 years) and a mean BMI of 26.8 (range: 20–34 years).
The volume of gastric secretion in patients with CC during administration of lubiprostone increased significantly by 50% (86.3 vs. 57.5 mg/h) (P<0.001) in basal conditions (Table 1) and increased by 25% (210.0 vs. 167.6 mg/h) (P=0.024) during stimulation with pentagastrin, the latter mimicking food-stimulated conditions. In the multivariate analyses, no carryover affect was identified. However, BMI was significant in the model for gastric juice volume secretion both in basal conditions (P=0.029) and stimulated secretions (P=0.002). The correlation between BMI and gastric juice volume was r=0.102 in basal conditions and r=0.479 in stimulated conditions.
Table 1. The impact of lubiprostone and placebo administration on the volume of gastric secretion, mucus, and mucin in basal conditions and during stimulation with pentagastrin in patients with chronic constipation.
| CC | Lubiprostone basal (mg/h) | Placebo basal (mg/h) | P value | Lubiprostone stimulated (mg/h) | Placebo stimulated (mg/h) | P value |
|---|---|---|---|---|---|---|
| Gastric juice volume (ml/h) | 86.3±7.1 | 57.5±4.2 | <0.001 | 210±17.5 | 167.6±11.8 | 0.024 |
| Gastric mucus (mg/h) | 257.3±29.5 | 135±16.4 | 0.001 | 348.1±48.7 | 270.8±21 | 0.156 |
| Gastric mucin (mg/h) | 98.4±13.9 | 54.5±7.2 | 0.009 | 98.3±15.9 | 71.7±9.5 | 0.118 |
CC, chronic constipation.
The rate of gastric mucus secretion during therapy with lubiprostone was 91% higher (257.3 vs. 135 mg/h) (P=0.001) in basal conditions and 28% higher (348.1 vs. 270.8 mg/h) (NS) in stimulated conditions. In the multivariate analysis, no carryover affect was identified. BMI was significant in the model for basal comparisons of mucus secretion (P=0.018; r=0.299) and nonsignificant in stimulated conditions.
The rate of gastric mucin secretion during lubiprostone therapy was 85% higher (98.4 vs. 54.5 mg/h) (P=0.011) in basal conditions and 38% (98.3 vs. 71.7 mg/h) (NS) higher in stimulated conditions. In the multivariate analysis, both carryover affect and BMI were not significant.
Administration of lubiprostone increased the viscosity of gastric secretion in patients with CC in basal conditions by 240% (21.61 vs. 6.34) (P<0.001) (Table 2) at the lowest shear rate and increased viscosity by 106% at the highest shear rate (5.21 vs. 2.87) (P<0.001).
Table 2. The impact of lubiprostone administration on gastric secretion viscosity in basal conditions in patients with chronic constipation.
| Viscometer share rates | Viscosity in chronic constipation Placebo therapy (mean±s.e.m.) | Viscosity in chronic constipation Lubiprostone therapy (mean±s.e.m.) | P value |
|---|---|---|---|
| 2 | 6.34±1.01 | 21.61±2.95 | <0.001 |
| 4 | 4.21±0.66 | 12.76±1.77 | <0.001 |
| 6 | 3.48±0.53 | 9.29±1.14 | <0.001 |
| 8 | 3.11±0.46 | 7.45±0.86 | <0.001 |
| 10 | 2.87±0.42 | 7.16±0.94 | <0.001 |
| 12 | 2.74±0.38 | 6.06±0.69 | <0.001 |
| 14 | 2.63±0.35 | 5.79±0.63 | <0.001 |
| 16 | 2.53±0.33 | 5.21±0.55 | <0.001 |
The viscosity of gastric secretion in patients with CC in pentagastrin-stimulated conditions during administration of lubiprostone increased significantly by 226% (14.96 vs. 4.59) (P<0.01) (Table 3) at the lowest shear rate and increased by 67% (2.88 vs. 172) (P<0.01) at the highest shear rate.
Table 3. The impact of lubiprostone on viscosity of gastric secretion collected during pentagastrin administration in patients with chronic constipation.
| Viscometer share rates | Viscosity in chronic constipation Placebo therapy (mean±s.e.m.) | Viscosity in chronic constipation Lubiprostone therapy (mean±s.e.m.) | P value |
|---|---|---|---|
| 2 | 4.59±1.20 | 14.96±3.00 | <0.01 |
| 4 | 3.26±0.81 | 7.06±1.14 | <0.01 |
| 6 | 2.43±0.41 | 5.30±0.94 | <0.01 |
| 8 | 2.26±0.38 | 4.12±0.64 | <0.01 |
| 10 | 2.11±0.35 | 3.43±0.47 | <0.01 |
| 12 | 1.93±0.27 | 2.92±0.35 | <0.01 |
| 14 | 1.84±0.23 | 3.04±0.41 | <0.01 |
| 16 | 1.72±0.19 | 2.88±0.38 | <0.01 |
Discussion
The alimentary tract mucosal epithelium is covered by the viscoelastic mucus-buffer layer that serves as an interface between the physical and chemical forces representing the luminal content and a very delicate cell membrane of the surface columnar epithelium. This is especially true when strong circular muscle contractions are forcefully squeezing and moving its luminal content, dominated by non-digestible food particles, down the colon towards rectum.
Chloride secretion is pivotal to the optimal rate of hydration of the luminal content along the alimentary tract.23, 24, 25, 26 Furthermore, chloride secretion is instrumental for the ability of gastric mucus to form a gel-like, viscous physical property, which is instrumental in mucosal protection and lubrication.4, 23
Viscosity is the measure of the internal friction of a fluid caused by molecular attraction of major mucus components, especially mucins, non-mucin glycoprotein, and phospholipids.4
All three of our hypotheses were supported by the results of this crossover clinical trial in basal conditions, that is: (1) the administration of lubiprostone results in a significant increase of gastric mucus secretion in patients with CC, (2) lubiprostone augments the secretion of gastric mucin, the major component of mucus that defines the viscoelastic and lubricating properties of gastric mucus, and (3) the viscosity of the alimentary tract secretion, represented predominantly by its content of mucus and mucin, is augmented by the administration of lubiprostone. The direction of the findings was the same in stimulated conditions, but only significant for gastric juice volume.
These results, reported for the first time in humans, clearly indicate that in CC patients, significantly augmented mucus secretion after lubiprostone is accompanied by significant increases of mucin, and a profound increase of the viscosity of luminal secretion, inevitably resulting in significantly promoted lubrication.
We interpret these findings to indicate that increased lubrication subsequently accelerates propagation of the luminal content of non-digestible food components in a caudal direction and leads to acceleration of the small bowel as well as colonic transit times. The increased lubrication and accelerated promulgation of non-digestible food components should culminate in their successful evacuation. McKeage et al.22 demonstrated accelerated small and large bowel transit times in humans after lubiprostone administration.
The potential promotion of lubrication and resulting facilitation of propagation of the luminal content of the alimentary tract19, 22, 24, 25, 26, 27 helps to explain why this new agent is known for its efficacy in therapy of CC as well as in patients with constipation-predominant IBS.26
The chemical composition and viscous properties of mucus and mucin within the gastric, duodena, small intestinal, and colonic mucosa covered by columnar epithelium is similar.2, 3, 4, 5, 6, 13 Their secretion are also governed by the same regulatory pathways mediated by the central, peripheral, and enteric nervous system and by gastrointestinal hormones and mediators released during the passage of ingested food components.4, 7, 8, 9, 10, 11, 13 The aspiration and testing of gastric secretion in basal and pentagastrin-stimulated conditions mimics food-stimulated conditions and provides adequate information of expected changes within the upper as well as the lower alimentary tract mucosa.
CC is a common gastrointestinal condition that significantly impacts patients' quality of life. It is reported more often by females and those over 65 years of age.12, 14, 17, 18 The majority of patients are represented by normal transit and normal function of the pelvic floor.12 Thirteen percent of patients with CC may demonstrate slow transit with decreased colonic motility and 25% may reveal dyssynergic defecation, overlapping with normal or slow transit; non-digestible food particles, metabolically processed and transformed by dynamically evolving intestinal microbiota,27, 28, 29, 30, 31 are gradually propagated in a caudal direction and have to be evacuated through the final act of expulsion.16, 18
This progressive event is possible owing to a well-coordinated motility pattern involving both circular and longitudinal muscles with a profound impact of the enteric nervous system network, sometimes referred to, for its size as a little brain.12, 14, 15, 16, 17, 18
Although well-propagated strong contractions within the large intestine represent a major driving force for bowel movements, an equally important role is played by luminal lubrication in this propagation.
Study strengths and limitations
The major strengths of our study are related to the fact that it was a well-conducted, IRB-approved, double-blind clinical trial powered to test the primary hypothesis that lubiprostone increased basal mucus by at least 40%. A tight protocol was used and all volunteers completed the study. Standardized criteria were used to determine subject eligibility and to assess CC. No crossover affect was identified in the multivariate analyses. BMI appeared as a significant covariate in several analyses. No interaction between BMI and treatment was observed.
The major limitations of our study are based on the fact that the 20 enrollees were volunteers with established CC. Eighty-five percent were female and 90% were Caucasians. The study was designed to assess the impact of lubiprostone on lubrication in this select population. To fully generalize these results, additional studies would be required, which include a large sample of males, African Americans, longer treatment and follow-up phases, additional data on prior CC history and risk factors, assessment of clinically significant end points, such as frequency of bowel movements, and ease of evacuation. As patients served as their own controls in the current study, the importance of considering BMI in the analyses was identified, but did not affect these findings. If future studies are designed so that patients do not serve at their own control, this study substantiates the need to consider BMI as a factor in the study design.
Conclusions
The significantly higher content of gastric mucus and mucin during therapy with lubiprostone in patients with CC suggests and supports the potentially leading role of ClC-2 stimulation in their secretion, resulting in profoundly increased viscosity facilitating and/or accelerating transit, as well as the evacuation of non-digestible food components.
Based on this experiment, we hypothesize that in CC patients, the significantly increased rate of mucus and its major component, mucin secretion, during lubiprostone administration may partially explain its clinical effectiveness and also have additional important clinical effects. We propose that as the increased mucus production enhances the protective quality of the mucosal barrier, it also boosts its potential to withstand luminal aggressive components such as acid/pepsin duet, H. pylori and/or nonsteroidal anti-inflammatory drugs/aspirin, or a combination of all. Further trials are needed to test this hypothesis.
As this was a crossover clinical trial, the patients serve as their own controls. No interaction was found with BMI and treatment. The observed relationships of BMI and mucus and mucin secretions and gastric juice volume are important considerations in the design of future trials, particularly if a crossover design is not used.
Study Highlights
Guarantor of the article: Jerzy Sarosiek, MD, PhD, FACG, AGAF.
Specific author contributions: Jerzy Sarosiek have conceived, initiated, and wrote the research project, as well as collected samples from enrolled patients in this study protocol. Irene Sarosiek played the leading role in running and controlling all clinical aspects of this research protocol. Marek Majewski was instrumental in performing laboratory analyses and tests on collected samples. Stan Edlavitch was pivotal in proving biostatistics expertise during writing this research project and subsequent statistical data analysis. Grzegorz Wallner was essential in providing support for data analysis and for re-editing and revisions of concepts supporting manuscript preparation.
Financial support: All our research goals and objectives throughout the entire process have been accomplished within our own financial capacity.
Potential competing interests: None.
References
- Namiot Z, Sarosiek J, Rourk RM, et al. Human esophageal secretion: mucosal response to luminal acid and pepsin. Gastroenterology. 1994;106:973–981. doi: 10.1016/0016-5085(94)90756-0. [DOI] [PubMed] [Google Scholar]
- Sarosiek J, Marshall BJ, Peura DA, et al. Gastroduodenal mucus gel thickness in patients with Helicobacter pylori: a method for assessment of biopsy specimens. Am J Gastroenterol. 1991;86:729–734. [PubMed] [Google Scholar]
- Sarosiek J, Slomiany A, Slomiany BL. Evidence for weakening of gastric mucus integrity by Campylobacter pylori. Scand J Gastroenterol. 1988;23:585–590. doi: 10.3109/00365528809093916. [DOI] [PubMed] [Google Scholar]
- Slomiany BL, Sarosiek J, Slomiany A. Gastric mucus and the mucosal barrier. Dig Dis. 1987;5:125–145. doi: 10.1159/000171168. [DOI] [PubMed] [Google Scholar]
- Brownlee IA, Havle ME, Dettmar PW, et al. Colonic mucus: secretion and turnover in relation to dietary fiber intake. Proc Nutr Soc. 2003;62:245–249. doi: 10.1079/pns2003206. [DOI] [PubMed] [Google Scholar]
- Atuma C, Strugala V, Allen A, et al. The adherent gastrointestinal mucus gel layer: thickness and physical state in vivo. Am J Physiol Gastrointest Liver Physiol. 2001;280:G922–G929. doi: 10.1152/ajpgi.2001.280.5.G922. [DOI] [PubMed] [Google Scholar]
- Jordan N, Newton J, Pearson J, et al. A novel method for the visualization of the in situ mucus layer in rat and man. Clin Sci. 2006;95:97–106. [PubMed] [Google Scholar]
- Pullan RD, Thomas GA, Rhodes M, et al. Thickness of adherent mucus gel on colonic mucosa in humans and its relevance to colitis. Gut. 1994;35:353–359. doi: 10.1136/gut.35.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter AC, Allen A, Garner A. Studies on mucus biosynthesis in the gastrointestinal tract. Symp Soc Exper Biol. 1989;43:27–36. [PubMed] [Google Scholar]
- Sellers LA, Allen A, Morris ER, et al. Mechanical characterization and properties of gastrointestinal mucus gel. Biorheology. 1987;24:615–623. doi: 10.3233/bir-1987-24614. [DOI] [PubMed] [Google Scholar]
- Allen A, Flemstrom G, Garner A, et al. Gastroduodenal mucosal protection. Physiol Rev. 1993;73:823–857. doi: 10.1152/physrev.1993.73.4.823. [DOI] [PubMed] [Google Scholar]
- Rao SS. Constipation: evaluation and treatment. Gastroenterol Clin N Am. 2003;32:659–683. doi: 10.1016/s0889-8553(03)00026-8. [DOI] [PubMed] [Google Scholar]
- Jaworski T, Sarosiek I, Sostarich S, et al. Restorative impact of rabeprazole on gastric mucus and mucin production impairment during naproxen administration: its potential clinical significance. Dig Dis Sci. 2005;50:357–365. doi: 10.1007/s10620-005-1611-3. [DOI] [PubMed] [Google Scholar]
- Talley NJ, Jones M, Nuyts G, et al. Risk factors for chronic constipation based on a general practice sample. Am J Gastroenterol. 2003;198:1107–1111. doi: 10.1111/j.1572-0241.2003.07465.x. [DOI] [PubMed] [Google Scholar]
- Talley NJ, Weaver AL, Zinsmeister AR, et al. Functional constipation and outlet delay: a population-based study. Gastroenterology. 1993;105:781–790. doi: 10.1016/0016-5085(93)90896-k. [DOI] [PubMed] [Google Scholar]
- Arce DA, Ermocilla CA, Costa H. Evaluation of constipation. Am Fam Phys. 2002;65:2283–2290. [PubMed] [Google Scholar]
- Camilleri M, Thompson WG, Fleshman JW, et al. Clinical management of intractable constipation. Ann Intern Med. 1994;121:520–528. doi: 10.7326/0003-4819-121-7-199410010-00008. [DOI] [PubMed] [Google Scholar]
- Ramkumar D, Rao SS. Efficacy and safety of traditional medical therapies for chronic constipation: systematic review. Am J Gastroenterol. 2005;100:936–971. doi: 10.1111/j.1572-0241.2005.40925.x. [DOI] [PubMed] [Google Scholar]
- Rivkin A, Chagan L. Lubiprostone: chloride channel activator for chronic constipation. Clin Ther. 2006;28:2008–2021. doi: 10.1016/j.clinthera.2006.12.013. [DOI] [PubMed] [Google Scholar]
- Johnson DA. Treating chronic constipation: How should we interpret the recommendations. Clin Drug Invest. 2006;26:547–557. doi: 10.2165/00044011-200626100-00001. [DOI] [PubMed] [Google Scholar]
- Bleser SD. Chronic constipation: let symptom type and severity direct treatment. J Fam Pract. 2006;55:587–593. [PubMed] [Google Scholar]
- McKeage K, Plosker GL, Siddiqui MA. Lubiprostone. Drugs. 2006;66:873–879. doi: 10.2165/00003495-200666060-00015. [DOI] [PubMed] [Google Scholar]
- Camilleri M, Bharucha AE, Ueno R, et al. Effect of a selective chloride channel activator, lubiprostone, on gastrointestinal transit, gastric sensory, and motor functions in healthy volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G942–G947. doi: 10.1152/ajpgi.00264.2005. [DOI] [PubMed] [Google Scholar]
- Winpenny JP. Lubiprostone. Drugs. 2005;65:416–422. [PubMed] [Google Scholar]
- Bayes M, Rabasseda X, Prous JR. Gateways to clinical trials. Meth Find Exper Clin Pharmacol. 2003;25:483–506. [PubMed] [Google Scholar]
- Lacy BE, Campbell Levy L. Lubiprostone: a chloride channel activator. J Clin Gastroenterol. 2007;41:345–351. doi: 10.1097/01.mcg.0000225665.68920.df. [DOI] [PubMed] [Google Scholar]
- Musch MW, Wang Y, Claud EC, et al. Lubiprostone decreases mouse colonic inner mucus layer thickness and alters intestinal microbiota. Dig Dis Sci. 2013;58:668–677. doi: 10.1007/s10620-012-2509-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiodini R, Chamberlin W, Sarosiek J, et al. Crohn's disease and the mycobacterioses: a quarter century later where it has been and where it is going. Clin Microbiol Rev. 2012;38:52–92. doi: 10.3109/1040841X.2011.638273. [DOI] [PubMed] [Google Scholar]
- Davis BR, Chiodini R, Sarosiek J, et al. Bacterial genomic sequences within submucosal tissues suggest distinct populations within the Crohn's disease spectrum. Gastroenterology. 2012;142:S1068. [Google Scholar]
- Guinane CM, Cotter PD. Role of gut microbiota in health and chronic gastrointestinal disease. Ther Adv Gastroenterol. 2013;6:295–308. doi: 10.1177/1756283X13482996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghoshal UC, Shukla R, Ghoshal U, et al. The gut microbiota and irritable bowel syndrome: friend or foe. Int J Inflamm. 2012;2012:1–12. doi: 10.1155/2012/151085. [DOI] [PMC free article] [PubMed] [Google Scholar]