Abstract
Objectives
We examine effects of school support as a structural HIV prevention intervention for adolescent female orphans in Zimbabwe after 5 years.
Methods
328 orphan adolescent girls were followed in a clustered randomized control trial from 2007 to 2010. The experimental group received school fees, uniforms, and school supplies and were assigned a school-based “helper.” In 2011-12, the control group received delayed partial treatment of school fees only. At the final data point in 2012, survey, HIV, and HSV-2 biomarker data were collected from approximately 88% of the sample. Bivariate and multivariate analyses were conducted on endpoint outcomes, controlling for age, religious affiliation, and baseline SES.
Results
The two groups did not differ on HIV or HSV-2 biomarkers. The comprehensive five-year intervention continued to reduce the likelihood of marriage, improve school retention, improve SES (food security), and marginally maintain gains in quality of life, even after providing school fees to the control group.
Conclusions
Paying school fees and expenses resulted in significant improvements in life outcomes for orphan adolescent girls. Biological evidence of HIV infection prevention, however, was not observed. Our study adds to the growing body of research on school support as HIV prevention for girls in sub-Saharan Africa, but as yet, no clear picture of effectiveness has emerged.
Adolescent girls in sub-Saharan Africa are at considerable risk for HIV, with prevalence about twice that of boys in most countries [1,2]. Girls have an earlier sexual debut than boys [3] and it is common for girls in sub-Saharan Africa to have sexual relationships with older male partners and to exchange sex for items such as food, money, school fees, and gifts [4]. Moreover, marriage provides little protection for adolescent females. For example, in Zambia and Kenya, marriage increased the odds of HIV for females by roughly 50% among geographic samples aged 15-19 years [5].
Despite a drop in HIV prevalence over the past decade [6], the most recent Zimbabwe population-based data indicates that HIV prevalence for females age 15-24 years was 7.3% compared to 3.6% for same-age males [7]. Girls’ sexual debut is later in Zimbabwe than in any other sub-Saharan country, and it is typically associated with marriage [8]. Marriage doubled the risk of HIV for rural 15-19 year old Zimbabwe women, based on data from the 2006 Zimbabwe Demographic and Health Survey [9]. Among a large sample of urban young women in Zimbabwe, about half of whom were orphans, marriage increased the age-adjusted odds of HIV by 2.6 and the odds of genital herpes (HSV-2) by 7.7 [10]. HSV-2 carries its own health burden, but more importantly raises the risk of acquiring HIV three-fold [11]. The elevated rate of HIV infection among young married women compared to their unmarried counterparts has been associated with more frequent intercourse, lack of condom use, and older partners who are more likely to be HIV positive [12, 13].
Over the past decade, there has been growing interest in determining whether keeping adolescent girls in school can help to mitigate the risk for HIV [14, 15]. Behavioral economists theorize that providing the poor with school subsidies through various cash transfer schemes improves socioeconomic status (SES) with better access to food; and that educational opportunities will positively affect expectations for the future and preferences for healthier lifestyles [15, 16]. One of the benefits of school subsidies may be a delay in marriage for girls, along with its associated HIV risks.
Two large sub-Saharan Africa studies have examined HIV biomarker and behavioral risk factors in randomized trials of school support interventions. Both examined HIV and HSV-2 outcomes at endpoint, but not at baseline. In Western Kenya, Duflo and colleagues [17] found that girls receiving a school subsidy in the form of two student uniforms during upper primary school experienced more years of schooling and a lower likelihood of marriage compared to no-treatment control girls after seven years, but they found no difference in either HIV or HSV-2 infection. On the other hand, Baird and colleagues [18] found that, after two years, a combination of secondary school fees and conditional cash transfers (monthly payments of $1-5 to students and $4-10 to parents, conditional on the students’ enrollment in school) reduced both school dropout and HIV prevalence among girls who were enrolled in school at baseline, but had no effect on marriage, pregnancy, sexual debut, or unprotected sexual intercourse.
In this paper, we describe HIV-related outcomes of school support for rural Zimbabwean orphan adolescent girls after five years. Our study is similar to the above two studies in that it is a cluster randomized controlled trial testing the effect of school subsidies on HIV-related outcomes for adolescent girls in a high HIV-prevalence sub-Saharan country. Support was conditional on staying in school and school fees were paid directly to the schools. Like the other two studies, we collected survey information on risk factors, along with HIV and HSV-2 biomarker data at the final data point.
A major difference is that our study focused on orphans. “Orphan” is defined as a child, less than 18 years old, with one or both parents deceased [19]. Adolescent orphans are an important group in sub-Saharan Africa because of their huge numbers and their disadvantage in HIV risk relative to non-orphans. Population-based data estimate that 41% of youth aged 15-17 years in Zimbabwe are orphans [7]. A recent meta-analysis of mostly sub-Saharan studies found that orphan youth face double the risk for HIV compared to non-orphans [20].
We previously reported that after two years, when the average age of participants was 14 years, the intervention reduced school dropout by 82% and marriage by 63% and also improved protective attitudes related to future expectations, gender equity, and concerns about the consequences of sex compared to controls [21]. After three years, we found that the intervention was cost effective in increasing years of schooling completed, reducing marriage as an HIV risk factor, and improving health-related quality of life (HRQoL) [22]. Given our positive findings, we decided we were ethically obligated to offer school fees to control students, starting in the fourth and final year of the project (2011). Subsequently, however, we received additional funding to continue the study for two more years to collect biomarker outcomes and a final round of survey data. Thus, at the final data point in 2012, we compared a comprehensive (5 year) intervention group with a delayed (1.5 years) partial intervention group.
Our study is unique in testing a structural HIV prevention intervention to keep sub-Saharan orphan adolescent girls in school over a five-year period. Our focus is on contextual influences and environments that influence young women's exposure to sexual risk factors of HIV, including school dropout, marriage, and HSV-2. We focused on school as a social context that may positively influence orphan girls by providing structure, behavioral monitoring, and access to pro-social adults and peers. We hypothesized that school attendance would reduce adolescent orphan girls’ exposure to sexual risk factors of HIV, including school dropout, teen marriage, and HSV-2.
We also found, however, that religion can be a powerful contextual influence, and that girls affiliated with Apostolic sects were at much higher risk of early marriage and school dropout than those from other religious denominations in Zimbabwe [9]. For this reason, we included religion as a covariate in our models. Apostolic sects are more likely to reject western medicine, HIV testing and gender equity in favor of traditional practices of faith healing, male dominance, and polygamy [23, 24]. Although very little research has been conducted on the Apostolic Church in Zimbabwe, it is the largest and fastest growing denomination in the country with 38% of adult women and 28% of men reporting membership [7].
The research question for our final main effects study is as follows: After five years, what is the impact of comprehensive school support on HIV and HSV-2 infection, sexual debut, marriage, school achievement, HRQoL, and SES (access to food), controlling for age, baseline SES, and religious affiliation? Our study is important in that it is one of only a few conducted in sub-Saharan Africa that examines the impact of schooling on girls’ HIV risk factors and infection.
METHODS
Design
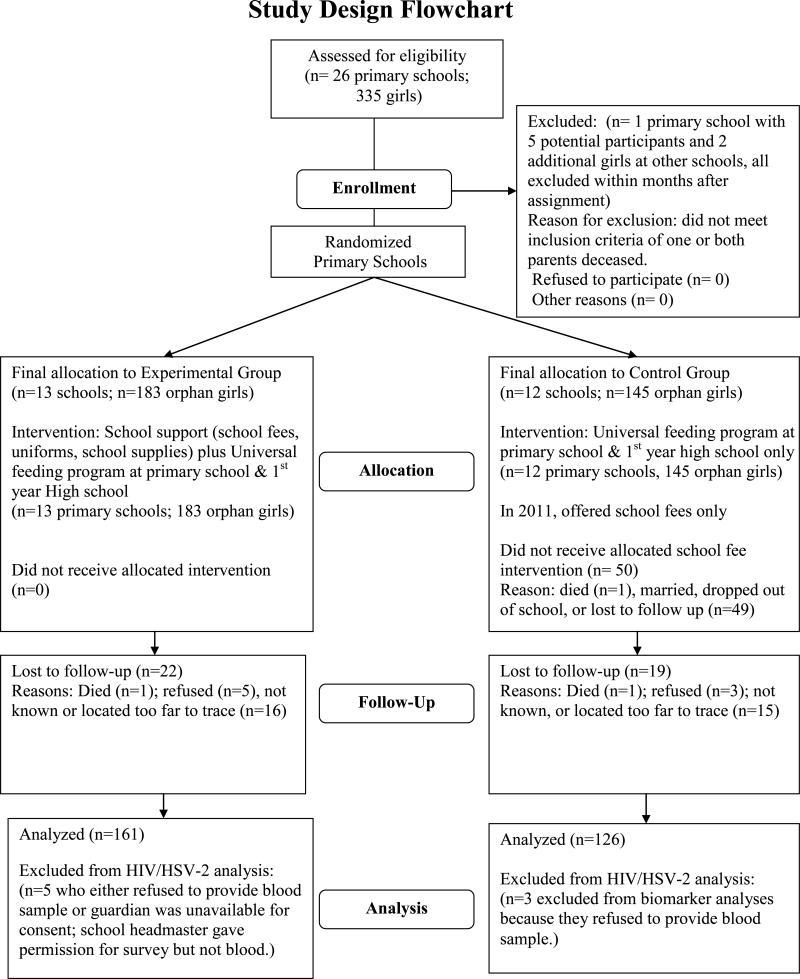
In 2007, all orphan girls in grade 6 at 25 rural primary schools in Manicaland, Zimbabwe were invited to participate in the research study. All those eligible (328) agreed to participate. Schools were randomized to either a no-treatment control group or a school support intervention group, consisting of fees, uniforms, supplies and a school-based female “helper” [21]. The role of the helper was to monitor participant attendance; if the student was absent, she was to find out why and if any assistance (e.g., medical care) was needed. The average age of participants at baseline was 12 years and intervention and control arms were equivalent on demographic and outcome measures [21]. None of the participants had ever been married or pregnant at baseline and all were in school (grade 6).
Three annual follow-up surveys were administered in 2008, 2009, and 2010. Based on continued positive effects from the intervention at the 2010 survey, control group students were offered school fees (only) starting in January 2011. The study was then extended two additional years with continued support for both groups and one additional survey and biomarker data collection in 2012.
The institutional review boards of PIRE (US) and the Medical Research Council of Zimbabwe reviewed and approved all study procedures. At baseline, we obtained permission from either a surviving parent or custodial guardian and assent from all participants for study participation [21]. To participate in the study extension, all participants were re-consented, with an option to participate in either the survey or the blood sample, or both.
Data Collection
A total of 287 participants (88%) completed the fifth survey (Wave 5) in 2012. The self-administered questionnaire used audio computer-assisted self-interviewing (ACASI) technology available in both English and Shona. We also collected blood specimens for HIV and HSV-2 prevalence outcomes. Details of biomarker data collection and analyses are described in a separate publication [25]. Eight participants responded to the survey but did not provide a biomarker specimen. Five of these were married members of Apostolic sects who refused to provide a biomarker blood sample for religious reasons.
Survey Measures
All variables were measured at Wave 5 unless otherwise noted.
Outcome Variables
Sexual debut measured dichotomous responses to the question “Have you ever had sexual intercourse?” Ever married indicated whether the participant was either currently or had ever been married or living with a man. Ever pregnant indicated whether the participant was pregnant or had ever given birth or had a miscarriage, abortion, or stillbirth. School Dropout indicated the participant was not in school at Wave 5, when participants should have been in their final year of high school. Years of schooling indicated the highest grade in school the participant had completed. Persons finishing primary school completed 7 years. Ten years was the maximum possible for those who had progressed normally.
Meals per day measured responses to the question “How many meals do you have in a day?” and was selected as a more sensitive measure of SES for rural adolescent orphans rather than the more common asset index, which tends to reflect community-level infrastructural development (e.g., electricity) as well as involvement in the cash economy (ownership of durable goods) [26, 27]. Wave 5 responses served as an outcome, as suggested by behavioral economic theory [15, 16]. HRQoL was measured with the EQ-5D assessment instrument with Zimbabwe-specific scoring [28]. Respondents reported whether they had no problems, some problems, or extreme problems including an inability to function on each of five items: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. HRQoL was measured only at Waves 4 and 5 as part of a separately funded sub-study of cost effectiveness [22].
Explanatory Variable
Condition indicates whether the participant is in the comprehensive intervention group or the delayed partial intervention group.
Covariates
Age was calculated on the participant's birth date and date of survey. Religion was measured by asking each girl the specific name of her religion at survey check-in. This resulted in 48 different sects (plus “no religion”) which were then classified by Zimbabwe researchers as follows: Roman Catholic, Protestant, Pentecostal, Apostolic Sect, and none. Only two participants said they had “no religion” and these were grouped with the “Apostolic Sect” (since both groups were more likely to hold traditional Shona beliefs) and coded as 1; the rest were coded 0 (referent) “Other.” Meals per day, as a measure of SES at baseline, served as the third covariate in the multivariate models.
In order to test the effects of attrition on baseline equivalence for the two groups, we included additional variables described elsewhere [21]: orphan status (paternal vs maternal or double); whether the child had a school uniform at baseline; school absence; educational aspirations (expected to go beyond high school); future educational, financial, and health expectations; gender equity attitudes; and wife beating attitudes.
Statistical Analyses
First, bivariate analyses were conducted, comparing the comprehensive intervention and delayed partial control groups on demographic and outcome variables, first with Wave 1 data (to examine bias due to attrition) and then at Wave 5. Then, logistic and ordinary least squares regressions were used to assess the impact of the comprehensive 5-year intervention, adjusting for age, religious affiliation, and meals/day (SES) at baseline on study outcomes. Survey procedures in SAS 9.3 [29] accounted for clustering in primary schools at baseline.
RESULTS
As seen in Table 1, a similar and very high proportion of participants in both conditions participated in the Wave 5 survey (87-88%) and blood sample (85%). Baseline analyses for these participants showed that responses were equivalent by condition on all baseline variables at p<0.05.
Table 1.
Attrition and Baseline equivalence of two study conditions participating at Wave 5
| Attrition at Wave 5 | Comprehensive Intervention Group N (%) | Delayed Partial Intervention Group N (%) | χ2 / t (p) |
|---|---|---|---|
| Baseline Sample (2007) | N = 183 | N = 145 | |
| Wave 5 Sample (2012) | 161 (88.0%) | 126 (87%) | 0.1 (0.77) |
| Provided Blood Sample at Wave 5 | 156 (85%) | 123 (85%) | 0.01 (0.92) |
| Equivalence of Retained Wave 5 Sample at Baseline | N (%) or Mean (SD) | N (%) or Mean (SD) | χ2 / t (p) |
|---|---|---|---|
| Individual-Level Variables | N = 161 | N=126 | |
| Age | 12.2 (0.97) | 12.3 (0.91) | 0.77 (0.44) |
| Orphan status: | 1.17 (0.28) | ||
| Paternal | 85 (52.8%) | 74 (59.2%) | |
| Maternal or Double orphan | 76 (47.2%) | 51 (40.8%) | |
| SES Count index | 3.22 (2.47) | 3.30 (2.28) | 0.27 (0.78) |
| Meals per day | 2.38 (0.89) | 2.45 (0.84) | 0.71 (0.48) |
| School Uniform (yes) | 95 (62.9%) | 73 (59.8%) | 0.27 (0.60) |
| School Absence | 2.00 (1.32) | 2.15 (1.38) | 0.95 (0.35) |
| Educational aspiration (higher than secondary school) | 149 (92.6%) | 108 (85.7%) | 3.53 (0.06) |
| Future Expectations | |||
| Graduate from Sec. School | 3.43 (1.28) | 3.30 (1.38) | −0.78 (0.43) |
| Graduate from College/Univ. | 3.20 (1.28) | 3.26 (1.38) | 0.40 (0.69) |
| Enough money by age 30 | 3.49 (1.17) | 3.33 (1.32) | −1.10 (0.27) |
| Live to age 35 | 3.19 (1.20) | 3.02 (1.15) | −1.26 (0.21) |
| Gender Equity Attitude | 2.57 (0.99) | 2.60 (0.94) | 0.27 (0.79) |
| Wife Beating Attitude | 2.10 (1.49) | 2.36 (1.65) | 1.39 (0.17) |
| Sexual Debut | 9 (5.6%) | 5 (4.0%) | 0.38 (0.54) |
| School-Level Variables | N=13 | N=12 | |
| Mean Number of Students | 506 (325.22) | 502 (190.49) | −0.03 (0.97) |
| Religious-affiliated Primary Schools | 3 (23%) | 4 (33%) | 0.33 (0.57) |
At Wave 5 (Table 2), no differences for either HIV or HSV-2 were found by study condition. Prevalence was similar, by condition, among the never married, with a trend toward higher HIV and HSV-2 infection among the married comprehensive intervention group compared to the delayed partial intervention group. Biological event rates were low, however, and differences were not significant. Since a sizeable minority of children infected through maternal to child transmission are thought to survive until adolescence in Zimbabwe [30-32], we further examined the number of HIV positive girls who were both: 1) HSV-2 negative; and 2) reported that they never had sex and never were married or pregnant. Four girls (33%) met the criteria (two from each condition; data not shown).
Table 2.
Comparison of Characteristics by Study Condition at Wave 5
| Comprehensive Intervention Group Mean (SD) or N (%) | Delayed Partial Intervention Group Mean (SD) or N (%) | χ2 / t (p) | |
|---|---|---|---|
| HIV Positive | 7 (4.5%) | 5 (4.1%) | 0.03 (0.86) |
| Among Unmarried | 5 (3.6%) | 4 (4.1%) | 0.1 (0.81) |
| Among Married | 2 (13.3%) | 1 (3.9%) | 1.2 (0.26) |
| HSV-2 Positive | 10 (6.4%) | 6 (4.9%) | 0.30 (0.58) |
| Among Unmarried | 6 (4.3%) | 3 (3.1%) | 0.2 (0.64) |
| Among Married | 4 (26.7%) | 3 (11.5%) | 1.5 (0.22) |
| Sexual Debut | 23 (14.3%) | 30 (23.8%) | 4.26 (0.04) |
| Ever Married | 18 (l1.2%) | 29 (23.6%) | 7.23 (0.01) |
| Ever Pregnant | 19 (11.8%) | 28 (22.2%) | 5.60 (0.02) |
| Ever Married & Never Pregnant | 2 (1.2%) | 3 (2.4%) | |
| Ever Pregnant but Never Married | 3 (1.9%) | 2 (1.6%) | |
| Schooling | |||
| Years of Schooling | 9.51 (1.1) | 8.74 (1.5) | −4.9 (< 0.01) |
| School Dropout | 17 (10.6%) | 37 (29.4%) | 16.4 (< 0.01) |
| Meals per day | 2.66 (0.74) | 2.30 (0.86) | −3.74 (< 0.01) |
| HRQoL (Health-Related Quality of Life) | 0.82 (0.11) | 0.79 (0.15) | 3.02 ( 0.03) |
| Religious Affiliation | 0.30 (0.60) | ||
| Apostolic | 55 (34.2%) | 47 (37.3%) | |
| Other | 106 (65.8%) | 79 (62.7%) | |
| Age | 16.8 (0.93) | 17.0 (0.91) | 1.30 (0.20) |
Fewer girls among the comprehensive intervention group reported sexual debut, marriage, or pregnancy compared to the delayed partial intervention group. Almost all married girls had experienced pregnancy; very few pregnant girls did not report being married. Those in the comprehensive intervention group were less likely to drop out of school and achieved almost one additional year of schooling compared to the delayed partial intervention group. They also reported eating more meals per day and having better quality of life. There was no difference in age or religious affiliation by condition.
Table 3 presents the results of regression analyses with covariates. None of the variables in the model predicted HIV infection. Age marginally increased the odds of HSV-2 infection. The comprehensive intervention greatly reduced the odds of marriage, while Apostolic religion and each year of advancing age greatly increased it. The comprehensive intervention increased years of schooling, and greatly decreased the odds of school drop-out. Age and Apostolic religion decreased years of schooling and increased the odds of dropping out of school. The comprehensive intervention increased the number of meals eaten per day. Apostolic religion was negatively associated with the number of meals eaten, while the number of meals eaten at baseline was a positive predictor. The comprehensive intervention marginally increased quality of life in the full model, while Apostolic religion and advancing age (marginally) decreased it.
Table 3.
Logistic/OLS Regression on Study Outcomes at Wave 5
| HIV infection | HSV2 infection | |||
|---|---|---|---|---|
| Predictors | OR | 95% CI | OR | 95% CI |
| Condition (Comprehensive vs. Delayed Partial) | 1.15 | 0.47 – 2.79 | 1.46 | 0.50 – 4.26 |
| Age | 1.14 | 0.65 – 1.97 | 1.62† | 0.98 – 2.68 |
| Religion at Wave 5 (Apostolic vs. others) | 2.08 | 0.71 – 6.16 | 0.90 | 0.25 – 3.26 |
| # of meals at Wave 1 | 1.21 | 0.51 – 2.84 | 1.03 | 0.42 – 2.53 |
| Predictors | Sexual debut | Marriage | School Dropout | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Condition (Comprehensive vs. Delayed Partial) | 0.52 | 0.23 - 1.21 | 0.37* | 0.16 – 0.88 | 0.24*** | 0.10 - 0.55 |
| Age | 2.48*** | 1.64 - 3.75 | 3.34*** | 1.97 – 5.66 | 2.79*** | 1.76 – 4.42 |
| Religion at Wave 5 (Apostolic vs. others) | 4.18*** | 1.97 - 8.86 | 4.45*** | 2.25 – 8.82 | 3.88*** | 2.18 – 6.93 |
| # of meals at Wave 1 | 0.96 | 0.62 - 1.49 | 0.99 | 0.59 – 1.65 | 0.95 | 0.58 - 1.54 |
| Years of Schooling | Meals per Day | HRQoL (Health-Related Quality of Life) | ||||
|---|---|---|---|---|---|---|
| Predictors | β | 95% CI | β | 95% CI | β | 95% CI |
| Condition (Comprehensive vs. Delayed Partial) | 0.68*** | 0.41 - 0.98 | 0.37** | 0.13 – 0.61 | 0.03† | −0.01 – 0.07 |
| Age | −0.46*** | −0.68 - −0.25 | 0.03 | −0.08 – 0.14 | −0.02† | −0.04 – 0.001 |
| Religion at Wave 5 (Apostolic vs. others) | −0.55** | −0.89 - −0.22 | −0.26* | −0.51 – −0.02 | −0.04* | −0.08 - −0.001 |
| # of Meals at Wave 1 | 0.11 | −0.09 - 0.31 | 0.22** | 0.06 – 0.37 | 0.01 | −0.01 – 0.38 |
p <0.10
*p ≤ 0.05
***p ≤ 0.001
p ≤ 0.05
p ≤ 0.001
p < 0.10
p ≤ 0.05
p ≤ 0.01
p ≤ 0.001.
DISCUSSION
Study results comparing a five-year comprehensive school support intervention for orphaned adolescent girls with a partial intervention offered during the final 1.5 years of the study showed continuation of the impacts on school retention and marriage found after the first two years [21]. The magnitude of difference by condition was somewhat smaller (64% reduction in school dropout after five years compared to 82% after two years [21]; 53% reduction in marriage after five years compared to 63% after two years), but still impressive. We also found theoretically important differences in SES (meals per day), and quality of life continued to be improved with the comprehensive intervention, although after school support was offered to controls, gains were reduced (0.03 in 2012 vs. 0.06 in 2010) [22] and now were only marginally significant.
Our study is one of a small group of sub-Saharan studies seeking to determine whether providing adolescent girls with support to stay in school can help to prevent HIV infection. Like the Duflo et al. study (limited to the school subsidy group vs the no-treatment group) [17], we found positive impacts on schooling and marriage but no impact on either HIV or HSV-2 biomarkers with our 5-year comprehensive intervention. However, the Duflo intervention was much more modest and biomarkers were measured five years after the intervention ended.
On the other hand, Baird's Malawi conditional cash transfer intervention (CCT) was comprehensive (cash plus secondary school fees) but implemented for just two years [18]. Compared to the no-treatment control, that study demonstrated an impact on HIV outcomes, although HSV-2 differences did not reach significance. In that study, as with ours, there was a low event rate for biological outcomes (in the Baird study, 17 of 799 controls were HIV positive compared to 3 of 235 in the CCT group). Given the low prevalence, the authors advise caution when interpreting findings. Surprisingly, few behavioral HIV risk factors in the Baird study were affected by the intervention. The control group was more likely to report an older partner (≥ 25 years of age) which could be a plausible mechanism, given that men become infected at older ages compared to women. But values were again very low (20 of 826 among controls and 1 of 235 in the CCT group).
In the present study, comprehensive school support for orphans from Grade 6 through high school did not result in lower HIV or HSV-2 infection for the five-year comprehensive intervention group compared to the group receiving just 1.5 years of delayed partial intervention. These findings are somewhat surprising, given the impact on marriage and the extensive literature suggesting its importance as an HIV risk factor for young women. HIV prevalence in Zimbabwe has been dropping in recent years [33], however, and our study was underpowered to detect small effect size differences by condition, given the relatively small sample size and low event rates found.
Age and religion were also important predictors of marriage. Each year of advancing age tripled the odds of marriage, and Apostolic sect affiliation raised the odds of marriage by more than four-fold. Because many Apostolic sects discourage the use of medical clinics, marriage poses an even greater risk for these girls. The two participants (one from each condition) who died in childbirth during the course of the study were Apostolic. Five Apostolic married girls who agreed to the survey refused to give a blood specimen, and others refused to participate in the study at all after they got married, reducing our ability to examine the relationship between religious affiliation and infection. Given the public health implications, we believe that religious affiliation is an important area for future research.
The intervention increased years of schooling, which has been found to improve young women's potential for future economic well- being and health [34]. The intervention's positive impact on SES, as measured by meals eaten per day, supports the theory that assistance to stay in school can improve SES and access to food [15, 16], even without cash payments to participants or their guardians. School fees, uniforms, and school supplies (e.g., pens and writing paper) offset household expenses, leaving more money for food. Our findings are consistent with the growing literature on cash transfer interventions in developing countries like Zimbabwe, seeking to increase income and improve school enrolment and attendance among poor households [35, 36]. Our intervention is similar to conditional cash transfer programs that require recipients to enroll in and attend school, and provides further evidence supporting structural interventions for public health goals.
Several limitations suggest caution in interpreting these findings. First, the observed comprehensive intervention effect may have been compromised by offering a delayed partial intervention to the control group. That decision, while ethically appropriate in light of positive findings at the end of the initial study [22], may have biased the findings in the direction of type 2 error. Second, we observed lower than expected biomarker prevalence, reducing the power to detect an effect from the intervention. Third, the usefulness of the HIV measure was further compromised by a potentially high proportion of orphan infection by maternal to child transmission in Zimbabwe [30-32]. Just as in the other two similar studies cited [17, 18], we did not collect biomarker data at baseline to rule out such cases. If we had, it is likely that the event rate of new (sexually transmitted) infections among our sample would have been smaller, reducing even further the study's power to detect differences. Although we examined the HIV positive participants who were HSV-2 negative and reported never having sex and never being married or pregnant and found that this group comprised roughly one third of each group, there is considerable measurement error associated with both self-report and serological diagnoses for HSV-2 [25]. Therefore, such retrospective analyses are only suggestive and cannot be confirmed. Finally, generalization of these findings is limited to rural orphaned Shona girls in Zimbabwe.
In conclusion, the results of this 5-year trial offer evidence of important positive effects from providing comprehensive school support to orphan girls in sub-Saharan Africa. Although the present study did not find reductions in HIV and HSV-2 biomarker outcomes with the 5-year comprehensive intervention, it did find positive impacts on key HIV-related risk factors, even after offering school fees to the control group. These findings, in the context of other similar research, suggest that school support as a contextual intervention in resource-poor countries is both promising and complex, requiring more study to determine how and under what circumstances such programs can best protect the health and well-being of girls and young women in sub-Saharan Africa.
Supplementary Material
Figure 1.
Study Design Flowchart
Acknowledgments
This study was funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (R01HD55838, Denise Hallfors, P.I.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health & Human Development, or the National Institutes of Health. We also wish to express our sincere appreciation to Marcia Hobbs and the staff of the Zimbabwe National Microbiology Reference Laboratory for their invaluable help with biomarker data collection and analysis; James January, Witness Chekumanyara, Patience Matende, Monica Zimunya, and the school Heads and Helpers for their help in the study over the five years; Frances Cowan for guiding us in a rigorous and practical plan for collecting biomarkers; Shane Hartman for his expert help in formatting and preparing the manuscript for submission; Susan Newcomer for her constant help and encouragement; and the courageous young women who participated in our study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Implications and Contributions
This study is important as one of a very few examining the impact of schooling on girls’ HIV risk factors and infection in sub-Saharan Africa, and unique in its focus on orphans. Although other significant benefits were found, biological HIV/HSV-2 reductions were not observed after five years of comprehensive intervention.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS) UNAIDS World AIDS Day Report. UNAIDS; Geneva: 2011. [May 2, 2014]. 2011. Available at http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/JC2216_WorldAIDSday_report_2011_en.pdf. [Google Scholar]
- 2.Hervish A, Clifton D, Population Reference Bureau . The Status Report on Adolescents and Young People in Sub-Saharan Africa: Opportunities and Challenges. United Nations Population Fund (UNFPA) and the Population Reference Bureau; Johannesburg and Washington D.C.: 2012. [May 2, 2014]. Available at http://www.prb.org/pdf12/status-report-youth-subsaharan-Africa.pdf. [Google Scholar]
- 3.Khan S, Mishra V. Youth Reproductive and Sexual Health. DHS Comparative Reports No. 19. International Inc.; Calverton, Maryland, USA: Macro: 2008. [April 11, 2014]. Available at https://dhsprogram.com/pubs/pdf/CR19/CR19.pdf. [Google Scholar]
- 4.Luke N. Age and economic asymmetries in the sexual relationships of adolescent girls in sub-Saharan Africa. Stud Fam Plann. 2003;34(2):67–86. doi: 10.1111/j.1728-4465.2003.00067.x. [DOI] [PubMed] [Google Scholar]
- 5.Glynn JR, Carael M, Auvert B, et al. Why do young women have a much higher prevalence of HIV than young men? A study in Kisumu, Kenya and Ndola, Zambia. AIDS. 2001;15(Suppl 4):S51–60. doi: 10.1097/00002030-200108004-00006. [DOI] [PubMed] [Google Scholar]
- 6.Gregson S, Gonese E, Hallett TB, et al. HIV decline in Zimbabwe due to reductions in risky sex? Evidence from a comprehensive epidemiological review. Int J Epidemiol. 2010;39(5):1311–1323. doi: 10.1093/ije/dyq055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zimbabwe National Statistics Agency (ZIMSTAT), ICF International . Zimbabwe Demographic and Health Survey 2010-11. ZIMSTAT and ICF International Inc.; Calverton, Maryland: 2012. [Google Scholar]
- 8.Kothari MT, Wang S, Head SK, Abderrahim N. DHS Comparative Reports No. 29. ICFInternational; Calverton, Maryland, USA: 2012. Trends in Adolescent Reproductive and Sexual Behaviors. [Google Scholar]
- 9.Hallfors DD, Cho H, Iritani BJ, et al. Preventing HIV by providing support for orphan girls to stay in school: does religion matter? Ethn Health. 2013;18(1):53–65. doi: 10.1080/13557858.2012.694068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birdthistle IJ, Floyd S, Machingura A, et al. From affected to infected? Orphanhood and HIV risk among female adolescents in urban Zimbabwe. AIDS. 2008;22(6):759–766. doi: 10.1097/QAD.0b013e3282f4cac7. [DOI] [PubMed] [Google Scholar]
- 11.Freeman EE, Weiss HA, Glynn JR, et al. Herpes simplex virus 2 infection increases HIV acquisition in men and women: systematic review and meta-analysis of longitudinal studies. AIDS. 2006;20(1):73–83. doi: 10.1097/01.aids.0000198081.09337.a7. [DOI] [PubMed] [Google Scholar]
- 12.Clark S. Early marriage and HIV risks in sub-Saharan Africa. Stud Fam Plann. 2004;35(3):149–60. doi: 10.1111/j.1728-4465.2004.00019.x. [DOI] [PubMed] [Google Scholar]
- 13.Clark S, Bruce J, Dude A. Protecting young women from HIV/AIDS: the case against child and adolescent marriage. Int Fam Plan Perspect. 2006;32(2):79–88. doi: 10.1363/3207906. [DOI] [PubMed] [Google Scholar]
- 14.Jukes M, Simmons S, Bundy D. Education and vulnerability: the role of schools in protecting young women and girls from HIV in southern Africa. AIDS. 2008;22(Suppl 4):S41–56. doi: 10.1097/01.aids.0000341776.71253.04. [DOI] [PubMed] [Google Scholar]
- 15.Pettifor A, MacPhail C, Nguyen N, Rosenberg M. Can money prevent the spread of HIV? A review of cash payments for HIV prevention. AIDS Behav. 2012;16(7):1729–1738. doi: 10.1007/s10461-012-0240-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiszbein A, Schady N. Conditional cash transfers: reducing present and future poverty. World Bank; Washington, DC: 2009. [Google Scholar]
- 17.Duflo E, Dupas P, Kremer M. [March 6, 2014];Education, HIV, and early fertility: Experimental evidence from Kenya. 2012 Dec 31; doi: 10.1257/aer.20121607. Unpublished manuscript available at: http://www.stanford.edu/~pdupas/DDK_EducFertHIV.pdf. [DOI] [PMC free article] [PubMed]
- 18.Baird SJ, Garfein RS, McIntosh CT, Ozler B. Effect of a cash transfer programme for schooling on prevalence of HIV and herpes simplex type 2 in Malawi: a cluster randomised trial. Lancet. 2012;379(9823):1320–9. doi: 10.1016/S0140-6736(11)61709-1. [DOI] [PubMed] [Google Scholar]
- 19.The Joint United Nations Programme on HIV/AIDS (UNAIDS), the United Nations Children's Fund (UNICEF), and the United States Agency for International Development (USAID) Children on the brink 2004: A joint report of new orphan estimates and a framework for action. United Nations Children's Fund; New York: 2004. [April 10, 2014]. Available at http://www.unicef.org/publications/files/cob_layout6-013.pdf. [Google Scholar]
- 20.Operario D, Underhill K, Chuong C, Cluver L. HIV infection and sexual risk behaviour among youth who have experienced orphanhood: systematic review and meta-analysis. J Int AIDS Soc. 2011;14:25. doi: 10.1186/1758-2652-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hallfors DD, Cho H, Rusakaniko S, et al. Supporting Adolescent Orphan Girls to Stay in School as HIV Risk Prevention: Evidence from a Randomized Controlled Trial in Zimbabwe. American Journal of Public Health. 2011;101(6):1082–1088. doi: 10.2105/AJPH.2010.300042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller T, Hallfors D, Cho H, et al. Cost-Effectiveness of School Support for Orphan Girls to Prevent HIV Infection in Zimbabwe. Prev Sci. 2013;14(5):503–512. doi: 10.1007/s11121-012-0315-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mpofu E, Dune TM, Hallfors DD, et al. Apostolic faith church organization contexts for health and wellbeing in women and children. Ethn Health. 2011;16(6):551–66. doi: 10.1080/13557858.2011.583639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maguranyanga B, UNICEF-Zimbabwe, Collaborating Centre for Operational Research, and Evaluation . Apostolic Religion, Health, and Utilization of Maternal and Child Health Services in Zimbabwe. United Nations Children's Fund; New York: 2011. [December 27, 2013]. Available at: http://www.unicef.org/zimbabwe/ZIM_resources_apastolicreligion.pdf. [Google Scholar]
- 25.Luseno WK, Hallfors DD, Cho H, et al. Use of HIV and HSV-2 biomarkers in Sub-Saharan adolescent prevention research: a comparison of two approaches. J Prim Prev. 2014;35(3):181–191. doi: 10.1007/s10935-014-0343-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Howe LD, Hargreaves JR, Ploubidis GB, et al. Subjective measures of socio-economic position and the wealth index: a comparative analysis. Health Policy Plan. 2011;26(3):223–32. doi: 10.1093/heapol/czq043. [DOI] [PubMed] [Google Scholar]
- 27.Bingenheimer JB. Wealth, wealth indices and HIV risk in East Africa. International Family Planning Perspectives. 2007;33(2):83–4. doi: 10.1363/3308307. [DOI] [PubMed] [Google Scholar]
- 28.Jelsma J, Hansen K, De Weerdt W, et al. How do Zimbabweans value health states? Popul Health Metr. 2003;1(1):11. doi: 10.1186/1478-7954-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.SAS Software, Version 9.3. SAS Institute Inc.; Cary, NC, USA.: [Google Scholar]
- 30.Mahomva A, Greby S, Dube S, et al. HIV prevalence and trends from data in Zimbabwe, 1997-2004. Sex Transm Infect. 2006;82(Suppl 1):i42–7. doi: 10.1136/sti.2005.019174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dube S, Boily MC, Mugurungi O, et al. Estimating vertically acquired HIV infections and the impact of the prevention of mother-to-child transmission program in Zimbabwe: insights from decision analysis models. J Acquir Immune Defic Syndr. 2008;48(1):72–81. doi: 10.1097/QAI.0b013e31816bcdbb. [DOI] [PubMed] [Google Scholar]
- 32.Ferrand RA, Corbett EL, Wood R, et al. AIDS among older children and adolescents in Southern Africa: projecting the time course and magnitude of the epidemic. AIDS. 2009;23(15):2039–46. doi: 10.1097/QAD.0b013e32833016ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marsh KA, Nyamukapa CA, Donnelly CA, et al. Monitoring trends in HIV prevalence among young people, aged 15 to 24 years, in Manicaland, Zimbabwe. J Int AIDS Soc. 2011;14:27. doi: 10.1186/1758-2652-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schultz PT. Why governments should invest more to educate girls. World Development. 2002;30(2):207–225. [Google Scholar]
- 35.Robertson L, Mushati P, Eaton JW, et al. Effects of unconditional and conditional cash transfers on child health and development in Zimbabwe: a cluster-randomised trial. Lancet. 2013;381(9874):1283–92. doi: 10.1016/S0140-6736(12)62168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment. QJ Econ. 2011;2011;126(4):1709–1753. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.