Abstract
Introduction:
Bronchoalveolar lavage (BAL) is a diagnostic procedure by which cells and other components from bronchial and alveolar spaces are obtained for various studies. One of the main advantages of BAL is that it can be done as a day care procedure. Material obtained by BAL can give a definite diagnosis in conditions such as infections and malignancies.
Aims:
The aims and objective of this study were to assess the utility of BAL as a diagnostic tool to determine the diagnostic accuracy of the material obtained from BAL in various infections and neoplastic lesions to study the limitations of BAL in certain lung disorders.
Materials and Methods:
This study was done in a tertiary care center in Hyderabad. Bronchoscopy was done as an outpatient procedure and lavage fluid obtained analyzed. This is a prospective study done from January 2012 to Jun 2013. Ninety-one BALs were analyzed for total and differential count, microbiological examination and cytological evaluation. Cases selected included nonresolving pneumonias, diffuse lung infiltrates, infiltrates in immunosuppressed hosts and ventilator-associated pneumonias.
Results:
Bronchoalveolar lavage was done in 91 cases over a period of 1½ years. Definite diagnosis was not given in 7 cases. Four cases were inadequate. Tuberculosis was diagnosed in 22 cases, fungal infections in 7 cases. Thirty-eight cases of bacterial pneumonias were diagnosed, Klebsiella was the most common organism. Malignancy was diagnosed in 13 cases.
Conclusion:
Definite diagnosis can be made in tuberculosis, fungal infections, bacterial pneumonias and in malignancies.
Keywords: Bronchoalveolar lavage, infections, malignancy
Introduction
Bronchoalveolar lavage (BAL) is a saline wash of the bronchial tree introduced in 1970. It is an investigative technique. It became a diagnostic tool in India in 1994. The number of studies on BAL in Indian literature are few. We take this opportunity to highlight the utility of BAL material in making a definite diagnosis. Its advantages outweigh its limitations. BAL material has a very important role in diagnosis of infections and malignancies. It is a relatively safe procedure and is well tolerated. With the number of conditions that can be diagnosed, we strongly suggest that BAL should be used as a diagnostic tool and just not an investigating procedure. BAL provides material for various microbiological tests. One major limitation of BAL is a large range of normal values. American thoracic society guidelines for clinical practice has given the normal ranges for healthy adult nonsmokers.[1]
Materials and Methods
Bronchoalveolar lavage was done in patients where clinical, radiological and routine laboratory investigations did not clinch a diagnosis. Clinical presentation included fever with cough, shortness of breath and chest pain.
Bronchoalveolar lavage was obtained in 91 cases over 1½ year period that is January 2012 to Jun 2013. Procedure was done under sterile conditions using 5 mm flexible fiber optic bronchoscope after spraying 10% lignocaine locally. Sedation was used for anxious patients. Procedure was done through nasal approach after instilling lignocaine gel. BAL aliquots of 20 mL 0.9% saline were used via syringe and a total of 120-150 mL was used. Suction of 100 mm of water was applied and about 70% of total instillate was retrieved. This fluid was sent to the lab in different containers for total and differential counts, cytology and microbiological examinations. Total count was done in Neubaeur chamber. Differential count was done on air-dried slide stained by Leishmans stain. Routine hematoxylin and eosin and PAP stains were done for cytology screening. Stains for acid fast bacilli (AFB) were done on all BAL samples, and fungal stains were done when there was a clinical and cytological suspicion and in all samples from immunosuppressed patients. Adequacy of samples was assessed based on definite criteria. Ciliated columnar cells of more than 5% was indicative of contamination and not representative.
We used Chamberlain et al.[2] criteria to reject samples. The criteria are -
Paucity of alveolar macrophages <10/10 hpfs.
Extensive epithelial cells.
Mucopurulent exudates.
Numerous red blood cells.
Degenerating changes.
Results
Bronchoalveolar lavage was done in 91 cases. Age of patients ranged from 12 years to 82 years; 66 were males and 25 were females. Out of the 91 cases [Table 1] four were inadequate. We diagnosed tuberculosis in 22 cases, malignancy in 13 cases, fungal infection in 7 cases and 38 bacterial infections. Accurate diagnosis was not possible in 7 cases. Out of 38 bacterial infections [Table 2] Klebsiella was the commonest organism isolated (39%), followed by pseudomonas in 23%, Acinetobacterium was grown in 13% cases, Escherichia coli in 15% and Methicillin-resistant Staphylococcus aureus, in 7.8% cases. AFB were seen in 22 cases, and bacterial load varied from patient to patient. Out of 13 malignancies four were adenocarcinomas, five squamous cell carcinomas [Figure 1] two small cell carcinomas and two poorly differentiated carcinomas. There were seven fungal lesions; 4 cases had candida, two of these also had coexisting AFB. Aspergillosis in two [Figure 2], one was pneumocystis carinii infection. We could not give a definite diagnosis in 7 cases where there was a mixed inflammatory infiltrate, AFB and fungal stains were negative, and cultures were negative.
Table 1.
Distribution of cases based on cytological diagnosis
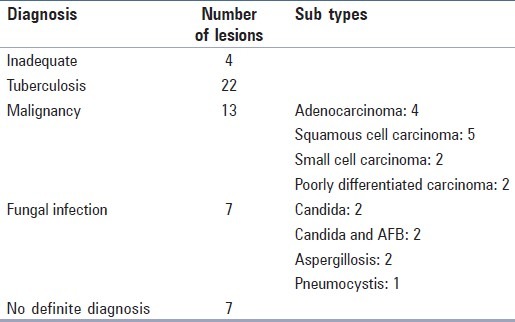
Table 2.
Distribution of the cases based on bacteria isolated
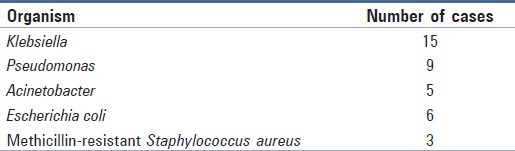
Figure 1.
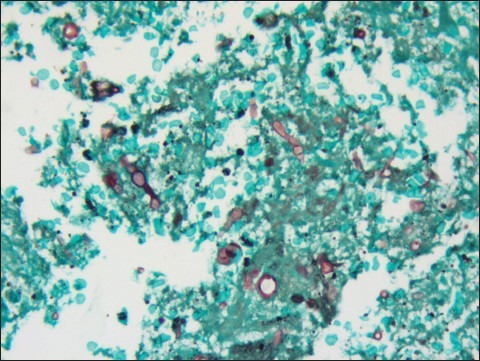
Septate branching hyphae (GMS ×400)
Figure 2.
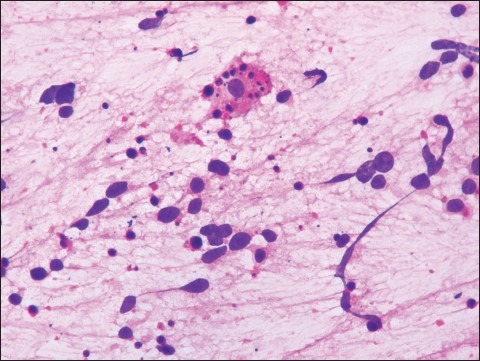
Neoplastic cells diffusely scattered and alveolar macrophages (H and E, ×400)
Discussion
Bronchoalveolar lavage is a useful and safe procedure for sampling cellular elements of lung. BAL as a diagnostic tool can be used to accurately diagnose various infections and also obtain material for culture and sensitivity. It is a preferred investigative tool over invasive techniques like needle biopsies and thoracoscopy. The incidence of tuberculosis is on the rise. BAL samples the epithelial lining of alveoli and hence rate of detection of tuberculosis is more. It facilitates early detection of tuberculosis in sputum negative tuberculosis.
Patients with positive tuberculin test and abnormal chest radiographs pose a diagnostic dilemma to clinicians. Bronchoscopy is useful in such cases to obtain lavage, where other modalities are not contributory. In a study by Baughman,[3]87% of bronchoscopy specimens were positive for tuberculosis. In our series, 24% of the cases were diagnosed as tuberculosis. Three cases were culture positive.
Bronchoalveolar lavage can be a very useful in the diagnosis of fungal infections. BAL has a sensitivity of 98%. It is almost equal to bronchial biopsy in sensitivity and specificity. We did fungal stains in lavages from immunosuppressed patients and when there is clinical or cytological suspicion. In fungal lesions, morphological analysis on Gomori's Methenamine Silver stained smears helps in diagnosing various fungi. BAL in addition provides material for culture and sensitivity.
The diagnosis of neoplastic lesions of the lung is a diagnostic problem for pulmonologists because some malignant lesions mimic infectious or inflammatory conditions. In such a clinical setting, BAL has a relevant role in detecting neoplastic cells or can also rule out malignant lesions.[4]
The role of BAL is based on growth pattern, cytological characteristics and correlation of morphology with imaging features and diagnostic value added by new investigations.[5] Application of BAL in diagnosing lung malignancy was first reported in mid 1980s.[6] Levy et al.[7] compared the yield of various diagnostic procedures and concluded that yield of BAL was high (66%) as compared to washings (57%), brushings (40%), transbronchial biopsy (44%).
Bronchoalveolar lavage is insufficient to diagnose the specific type of interstitial lung diseases (ILDs). BAL does not have any prognostic value and cannot predict response to therapy.[1]
In addition therapeutic uses of BAL, include removal of tenacious mucous plugs in asthma and cystic fibrosis. Whole lung lavages are helpful in silicosis and alveolar microlithiasis.
One major clinical limitation of BAL is a large range of normal values. Various soluble constituents like cytokines or other inflammatory mediators and collagen metabolism markers are used for research purpose. None of these markers have diagnostic utility.
Conclusion
Bronchoalveolar lavage is a useful diagnostic tool in diagnosing bacterial pneumonias, tuberculous lesions, fungal infections, and malignancies. Its role is limited in diagnosing and prognosticating ILDs.
The number of lesions with a definite diagnosis outnumber the lesions that cannot be diagnosed hence we opine that BAL is a useful diagnostic modality not only for routine diagnosis, but also for ancillary techniques and research purpose.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Meyer KC, Raghu G, Baughman RP, Brown KK, Costabel U, du Bois RM, et al. An official American Thoracic Society clinical practice guideline: The clinical utility of bronchoalveolar lavage cellular analysis in interstitial lung disease. Am J Respir Crit Care Med. 2012;185:1004–14. doi: 10.1164/rccm.201202-0320ST. [DOI] [PubMed] [Google Scholar]
- 2.Chamberlain DW, Braude AC, Rebuck AS. A critical evaluation of bronchoalveolar lavage. Criteria for identifying unsatisfactory specimens. Acta Cytol. 1987;31:599–605. [PubMed] [Google Scholar]
- 3.Baughman RP, Dohn MN, Loudon RG, Frame PT. Bronchoscopy with bronchoalveolar lavage in tuberculosis and fungal infections. Chest. 1991;99:92–7. doi: 10.1378/chest.99.1.92. [DOI] [PubMed] [Google Scholar]
- 4.Poletti V, Chilosi M, Olivieri D. Diagnostic invasive procedures in diffuse infiltrative lung diseases. Respiration. 2004;71:107–19. doi: 10.1159/000076670. [DOI] [PubMed] [Google Scholar]
- 5.Poletti V, Poletti G, Murer B, Saragoni L, Chilosi M. Bronchoalveolar lavage in malignancy. Semin Respir Crit Care Med. 2007;28:534–45. doi: 10.1055/s-2007-991526. [DOI] [PubMed] [Google Scholar]
- 6.Weynants P, Cordier JF, Cellier CC, Pages J, Loire R, Brune J. Primary immunocytoma of the lung: The diagnostic value of bronchoalveolar lavage. Thorax. 1985;40:542–3. doi: 10.1136/thx.40.7.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy H, Horak DA, Lewis MI. The value of bronchial washings and bronchoalveolar lavage in the diagnosis of lymphangitic carcinomatosis. Chest. 1988;94:1028–30. doi: 10.1378/chest.94.5.1028. [DOI] [PubMed] [Google Scholar]


