Abstract
Background:
Obstructive sleep apnea (OSA) is very frequent and often unrecognized in surgical patients. OSA is associated with perioperative complications. We evaluated the effects of OSA on postoperative complications and hospital outcomes in patients undergoing coronary artery bypass graft (CABG) surgery.
Methods:
Candidates of elective CABG were evaluated by the Berlin questionnaire for OSA. After surgery, patients were assessed for postoperative complications, re-admission to the Intensive Care Unit (ICU), duration of intubation, re-intubation, days spent in the ICU and the hospital.
Results:
We studied 61 patients who underwent CABG from which 25 (40.9%) patients had OSA. Patients with OSA had higher body mass index (29.5 ± 3.9 vs. 26.0 ± 3.7 kg/m2, P = 0.003) and higher frequency of hypertension (68.0% vs. 30.5%, P = 0.003), dyslipidemia (36.0% vs. 5.5%, P = 0.004), and pulmonary disease (16.0 vs. 2.7%, P = 0.08). Regarding the surgical outcomes, OSA patients had longer intubation duration (0.75 ± 0.60 vs. 0.41 ± 0.56 days, P = 0.03).
Conclusions:
Obstructive sleep apnea is frequent, but unrecognized among patients undergoing CABG. In these patients, OSA is associated with prolonged intubation duration. Preventing these problems may be possible by early diagnosis and management of OSA in cardiac surgery patients. Further studies with larger sample of patients and longer follow-ups are required in this regard.
Keywords: Cardiac surgery, coronary artery bypass grafting, coronary artery disease, obstructive sleep apnea
INTRODUCTION
Obstructive sleep apnea (OSA) is a sleep-disordered breathing with repeated upper airway obstruction during sleep due to the collapsing pharyngeal airway.[1] The reported prevalence of OSA is approximately 3-7% in men and 2-5% in women in the general population with a major risk factors, including male gender, older age, and obesity.[2] Sleep apnea is an independent risk factor for several cardiovascular diseases and can increase mortality and morbidity in these patients.[3]
It has been shown that OSA is highly prevalent but mostly undiagnosed in surgical patients.[4,5] The sedation and anesthesia during surgery increase the risk of postoperative complications in these patients. It has been reported that OSA is associated with more postoperative complications including severe respiratory, cardiac, and neurological complications.[4,5,6] Screening of patients undergoing elective surgery for OSA is recommended to reduce the associated perioperative risk, and perioperative management should be adapted accordingly.[4,7]
Considering the majority of patients with OSA are undiagnosed, they are at risk during the perioperative period. Although OSA is associated with cardiovascular diseases and a high frequency of OSA is reported in surgical patients, very few studies are carried out on OSA in cardiac surgical patients.[8,9,10] Some of the studies in this regard have shown increased risk for severe postoperative complications in patients with OSA undergoing cardiac or cardiothoracic surgeries.[10,11,12]
Regarding the lack of data on the perioperative complications of patients undergoing cardiac surgery, our study aimed to assess the prevalence of OSA among patients referred for elective coronary artery bypass graft (CABG) surgery. We also evaluated surgical complications (e.g. wound infection, postoperative fever, atrial fibrillation [AF]) and hospital outcomes (e.g. Intensive Care Unit (ICU) re-admission and duration, re-intubation and intubation duration, hospitalization) in these patients.
METHODS
Patients and settings
This prospective study was conducted on patients referring for elective CABG between 2012 and 2013 to Sadi Hospital in Isfahan city, Iran. The study was approved by The Hospital Ethics Committee. Patients who were able to fill the Berlin questionnaire and willing to participate were consecutively included to the study. We excluded patients with a history of stroke, severe disability, and those being on oxygen supplement. Consent was obtained from all patients before participation.
Assessments
Data regarding patient's age, gender, weight, height, and history of hypertension, diabetes mellitus, dyslipidemia, pulmonary disease, and smoking were gathered from the patient's hospital document. The Berlin questionnaire was used to evaluate the risk to suffer from OSA. This questionnaire is a self-administered tool, which includes 10 questions in three categories, including snoring, tiredness, and the presence of comorbidities. The risk of OSA is defined as high if the patient is positive in at least two symptom categories. The questionnaire had been validated against polysomnography with sensitivity of 86%, specificity of 77%, and positive predictive value of 89%.[13] The Persian version of the questionnaire used in our study was validated and has had sensitivity of 84%, specificity of 61.5%, and positive predictive value 96% in sleep clinic patients.[14] Diagnostic accuracy of the Berlin questionnaire was considered acceptable in surgical patients.[15]
After surgery, patients were assessed for the occurrence of fever, arterial fibrillation, re-admission to the ICU, re-intubation, and the duration of intubation, being in the ICU and hospital stay until they discharged from the hospital. Information regarding these variables was gathered from the patient's hospital document.
Statistical analysis
Analyses were performed using the SPSS software (version 16.0) (SPSS Inc., Chicago IL., USA) for windows. Quantitative and qualitative variables are presented as mean ± standard deviation and number (%), respectively. Comparison of patients with and without OSA was done using an independent t-test and Chi-square test for quantitative and qualitative variables, respectively. Appropriate tests for nonparametric data were applied. P <0.05 was considered as significant in all analyses.
RESULTS
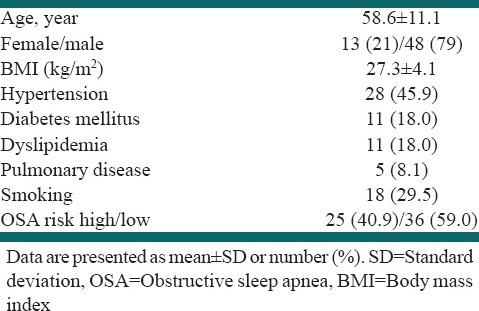
During the study period, 96 patients with cardiac surgery were investigated from which 61 patients underwent CABG and were eligible to participate in our study. Demographic data and baseline medical condition are presented in Table 1.
Table 1.
Demographic data and baseline medical condition (n=61)
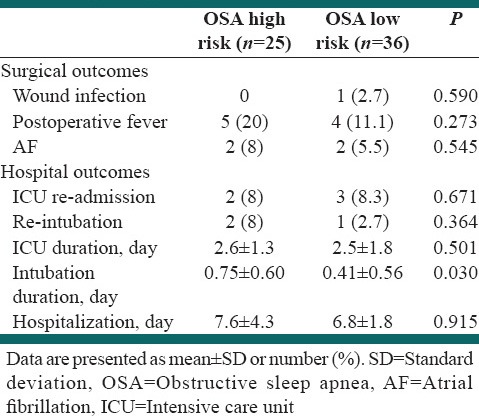
According to the Berlin questionnaire, 25 (40.9%) patients had a high risk for OSA. None of these patients had been previously diagnosed by objective sleep tests. Comparisons of the patients with and without OSA risk regarding their baseline medical conditions as well as the surgical and hospital outcomes are presented in Tables 2 and 3. Patients with OSA had higher body mass index (BMI) (29.5 ± 3.9 vs. 26.0 ± 3.7, P = 0.003) and higher frequency of hypertension (68.0% vs. 30.5%, P = 0.003), dyslipidemia (36.0% vs. 5.5%, P = 0.004), and pulmonary disease (16.0 vs. 2.7%, P = 0.08). Regarding the surgical outcomes, OSA patients had longer intubation duration (0.75 ± 0.60 vs. 0.41 ± 0.56 days, P = 0.03).
Table 2.
Comparisons of the patients with and without OSA risk regarding baseline medical conditions
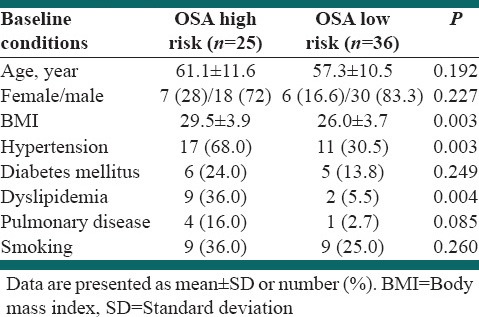
Table 3.
Comparisons of the patients with and without OSA risk regarding surgical and hospital outcomes
DISCUSSION
The aim of the present study was to investigate OSA in elective CABG candidates and its association with surgical complications and hospital outcomes. Our study showed that about 40% of CABG candidates had a high risk for OSA that is about two-fold greater than the prevalence in our general population with the same age range.[16] None of the patients with high risk for OSA had been previously diagnosed by an objective sleep test. We believe that it is related to the limited availability of specialized sleep clinics in our society. We also found that OSA is associated with increased intubation duration.
Previous studies showed that OSA is present in 25-70% of elective surgical patients and in most cases (above 80%) it is under-recognized.[15,17,18,19] Several studies showed that patients with OSA have an increased risk for postoperative complications including severe respiratory, cardiac, and neurological complications as well as worse hospital outcomes including prolonged ICU and hospital stay and re-admission.[4,6] Although more frequency of OSA and more severe associated complications are expected in cardiac patients at surgery, few studies have been focused on this population. Danzi-Soares et al. evaluated CABG candidates with both objective and subjective sleep apnea measures, and found OSA in 87% of the patients using polysomnography and in 72% using the Berlin questionnaire.[9] Using polysomnography, Mooe et al. also found OSA in 64.4% of CABG candidates.[20] The other study by van Oosten et al. using the Berlin questionnaire also found a prevalence of 47.7% for OSA in CABG patients.[21] The lower frequency of OSA in our patients compared with these studies might be related to the accuracy of the Berlin questionnaire in diagnosing OSA. It must be noted that the Berlin questionnaire only provide a suspicion for OSA that should be confirmed with appropriate measures. Furthermore, possibly a lower prevalence of OSA in our general population[16] as was also presented in a previous study on noncardiac surgical patients,[19] and also differences between the studied population especially regarding age and BMI could have effects on the results.
Severe postoperative complications and worse hospital outcomes are associated with OSA in cardiac patients at surgery. AF is frequent after CABG and associated with short- and long-term mortality.[22] Previous studies have shown that OSA increases the risk of postoperative AF in CABG patients. Using the Berlin questionnaire in CABG candidates, Mungan, et al. reported a relative risk of 1.7[10] and van Oosten et al. reported a relative risk of 1.5[21] for AF in patients with OSA compared with those without OSA. In another study, Mooe et al. with using polysomnography reported a relative risk of 2.8 for AF in OSA patients.[20] We found no increased risk of AF in patients with OSA; however, it should be noted that our study had limitations in aspect as we used patient's files as a source of information. The underlying mechanisms of the association between OSA and AF are poorly understood. Possible mechanisms are shared risk factors, autonomic instability, and atrial remodeling.[23] P wave parameters indicating atrial conduction status are known as predictors of AF after CABG.[24] Using Holter monitoring, we recently showed an association of OSA with prolonged P-max and P wave dispersion, which are risk factors for AF.[25] Hence, P wave parameters could be used to find patients at increased risk of postoperative AF, but further studies are required before confirming this subject.
There are other complications associated with OSA in CABG patients. Similar to our study, Bhama et al. have reported more pulmonary morbidity and also longer duration of hospitalization in OSA patients after CABG compared with those without OSA.[8] In a survey on 25,587 patients who underwent cardiac surgery at the Cleveland Clinic, only 37 patients have been identified previously as having OSA by sleep studies at the clinic. After cardiac surgery, these patients had a higher incidence of encephalopathy, postoperative infection (mostly mediastinitis) and increased ICU length of stay.[11] As reviewed by Vasu et al., studies in other cardiac or cardiothoracic surgical patients also showed similar results.[5] Some differences among previous studies are related to differences in the OSA measures and characteristics of the studied populations. Available evidence confirms that OSA in cardiac surgical patients, especially those who underwent CABG, is associated with severe postoperative complications and worse hospital outcomes.
The high frequency of OSA and its associated risks in surgical patients necessitate preventive and therapeutic approaches. Unfortunately, very few studies are available for this question. Some general recommendations are limiting the use of opioids and sedation after surgery, monitoring oxygenation in the postoperative period, and using continuous positive airway pressure.[5,7] In a retrospective study, Cassar et al. showed that treated OSA patients had a significantly decreased number of cardiac deaths following percutaneous coronary intervention compared with untreated OSA patients.[26] Zarbock et al. in a randomized trial of patients scheduled for elective cardiac surgery found that the treatment with nasal CPAP following extubation reduces pulmonary complications and re-admission rate to the ICU.[27] Studies on other surgical patients also showed that noninvasive positive pressure ventilation immediately after extubation can improve postoperative lung function and reduce postoperative complications in OSA patients under surgery.[28,29] These studies showed that ventilator supports such as CPAP can be useful to alleviate postoperative airway obstruction and reduce postoperative complications as well as improve hospital outcomes. However, further trials should be conducted in this regard.
There are some limitations for our study. The sample size in our study was limited for assessment of rare postoperative complications and for multivariate analysis of the factors associated with the study outcomes. Furthermore, we used subjective OSA measure, which is less accurate than polysomnography for the diagnosis of OSA. More importantly, data collection in our study was based on patient's files, and some study outcomes have not been precisely assessed or recorded in the patient's files. Finally, we assessed only in hospital complications, while OSA could be associated with long-term outcomes that need to be considered in the future studies.
CONCLUSIONS
This study showed that OSA is highly frequent, but un-recognized among patients undergoing CABG. In these patients, OSA is associated with prolonged intubation duration. Preventing these problems may be possible by early diagnosis and management of OSA in cardiac surgery patients. Screening for OSA using either subjective or objective sleep measures are recommended in these patients. Further studies with larger sample of patients and longer follow-ups are required. Furthermore, clinical trials are needed to find appropriate preventive and therapeutic approaches in OSA patients at surgery.
ACKNOWLEDGMENTS
We are thankful to the staff of the Cardiac Surgery Unit and Intensive Care Unit of the Sadi Hospital. Furthermore, we are thankful to Dr. Ali Gholamrezaei for data analysis and editing this report.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22:667–89. [PubMed] [Google Scholar]
- 2.Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5:136–43. doi: 10.1513/pats.200709-155MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Somers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, et al. Sleep apnea and cardiovascular disease: An American Heart Association/american College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health) Circulation. 2008;118:1080–111. doi: 10.1161/CIRCULATIONAHA.107.189375. [DOI] [PubMed] [Google Scholar]
- 4.Adesanya AO, Lee W, Greilich NB, Joshi GP. Perioperative management of obstructive sleep apnea. Chest. 2010;138:1s489–98. doi: 10.1378/chest.10-1108. [DOI] [PubMed] [Google Scholar]
- 5.Vasu TS, Grewal R, Doghramji K. Obstructive sleep apnea syndrome and perioperative complications: A systematic review of the literature. J Clin Sleep Med. 2012;8:199–207. doi: 10.5664/jcsm.1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gaddam S, Gunukula SK, Mador MJ. Post-operative outcomes in adult obstructive sleep apnea patients undergoing non-upper airway surgery: A systematic review and meta-analysis. Sleep Breath. 2013 doi: 10.1007/s11325-013-0925-1. [DOI] [PubMed] [Google Scholar]
- 7.Chung SA, Yuan H, Chung F. A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg. 2008;107:1543–63. doi: 10.1213/ane.0b013e318187c83a. [DOI] [PubMed] [Google Scholar]
- 8.Bhama JK, Spagnolo S, Alexander EP, Greenberg M, Trachiotis GD. Coronary revascularization in patients with obstructive sleep apnea syndrome. Heart Surg Forum. 2006;9:E813–7. doi: 10.1532/HSF98.20061072. [DOI] [PubMed] [Google Scholar]
- 9.Danzi-Soares NJ, Genta PR, Nerbass FB, Pedrosa RP, Soares FS, César LA, et al. Obstructive sleep apnea is common among patients referred for coronary artery bypass grafting and can be diagnosed by portable monitoring. Coron Artery Dis. 2012;23:31–8. doi: 10.1097/MCA.0b013e32834df5d0. [DOI] [PubMed] [Google Scholar]
- 10.Mungan U, Ozeke O, Mavioglu L, Ertan C, Karaca IO, Keskin G, et al. The role of the preoperative screening of sleep apnoea by Berlin Questionnaire and Epworth Sleepiness Scale for postoperative atrial fibrillation. Heart Lung Circ. 2013;22:38–42. doi: 10.1016/j.hlc.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Kaw R, Golish J, Ghamande S, Burgess R, Foldvary N, Walker E. Incremental risk of obstructive sleep apnea on cardiac surgical outcomes. J Cardiovasc Surg (Torino) 2006;47:683–9. [PubMed] [Google Scholar]
- 12.Hwang D, Shakir N, Limann B, Sison C, Kalra S, Shulman L, et al. Association of sleep-disordered breathing with postoperative complications. Chest. 2008;133:1128–34. doi: 10.1378/chest.07-1488. [DOI] [PubMed] [Google Scholar]
- 13.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 14.Amra B, Nouranian E, Golshan M, Fietze I, Penzel T. Validation of the Persian version of berlin sleep questionnaire for diagnosing obstructive sleep apnea. Int J Prev Med. 2013;4:334–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. Validation of the Berlin questionnaire and American society of anesthesiologists checklist as screening tools for obstructive sleep apnea in surgical patients. Anesthesiology. 2008;108:822–30. doi: 10.1097/ALN.0b013e31816d91b5. [DOI] [PubMed] [Google Scholar]
- 16.Amra B, Farajzadegan Z, Golshan M, Fietze I, Penzel T. Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath. 2011;15:425–9. doi: 10.1007/s11325-010-0353-4. [DOI] [PubMed] [Google Scholar]
- 17.Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009;10:753–8. doi: 10.1016/j.sleep.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Lockhart EM, Willingham MD, Abdallah AB, Helsten DL, Bedair BA, Thomas J, et al. Obstructive sleep apnea screening and postoperative mortality in a large surgical cohort. Sleep Med. 2013;14:407–15. doi: 10.1016/j.sleep.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amra B, Saberpur S, Ghoharian V, Tabatabai SA, Akbari M, Beni BH. Berlin questionnaire study in surgical patient in Alzahra hospital in year 2010. Adv Biomed Res. 2013;2:16. doi: 10.4103/2277-9175.107992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mooe T, Gullsby S, Rabben T, Eriksson P. Sleep-disordered breathing: A novel predictor of atrial fibrillation after coronary artery bypass surgery. Coron Artery Dis. 1996;7:475–8. [PubMed] [Google Scholar]
- 21.van Oosten EM, Hamilton A, Petsikas D, Payne D, Redfearn DP, Zhang S, et al. Effect of preoperative obstructive sleep apnea on the frequency of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol. 2014;113:919–23. doi: 10.1016/j.amjcard.2013.11.047. [DOI] [PubMed] [Google Scholar]
- 22.Kaw R, Hernandez AV, Masood I, Gillinov AM, Saliba W, Blackstone EH. Short- and long-term mortality associated with new-onset atrial fibrillation after coronary artery bypass grafting: A systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2011;141:1305–12. doi: 10.1016/j.jtcvs.2010.10.040. [DOI] [PubMed] [Google Scholar]
- 23.Digby GC, Baranchuk A. Sleep apnea and atrial fibrillation; 2012 update. Curr Cardiol Rev. 2012;8:265–72. doi: 10.2174/157340312803760811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang BC, Che WL, Li WM, Xu YW. Meta-analysis of P wave character as predictor of atrial fibrillation after coronary artery bypass grafting. Int J Cardiol. 2011;152:260–2. doi: 10.1016/j.ijcard.2011.07.098. [DOI] [PubMed] [Google Scholar]
- 25.Jazi MH, Amra B, Yazdchi MR, Jahangiri M, Tabesh F, Gholamrezaei A. P wave duration and dispersion in Holter electrocardiography of patients with obstructive sleep apnea. Sleep Breath. 2013 doi: 10.1007/s11325-013-0917-1. [DOI] [PubMed] [Google Scholar]
- 26.Cassar A, Morgenthaler TI, Lennon RJ, Rihal CS, Lerman A. Treatment of obstructive sleep apnea is associated with decreased cardiac death after percutaneous coronary intervention. J Am Coll Cardiol. 2007;50:1310–4. doi: 10.1016/j.jacc.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 27.Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen-Milles D. Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: A prospective, randomized, controlled trial in 500 patients. Chest. 2009;135:1252–9. doi: 10.1378/chest.08-1602. [DOI] [PubMed] [Google Scholar]
- 28.Neligan PJ, Malhotra G, Fraser M, Williams N, Greenblatt EP, Cereda M, et al. Continuous positive airway pressure via the Boussignac system immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesthesiology. 2009;110:878–84. doi: 10.1097/ALN.0b013e31819b5d8c. [DOI] [PubMed] [Google Scholar]
- 29.Neligan PJ, Malhotra G, Fraser M, Williams N, Greenblatt EP, Cereda M, et al. Retraction. Noninvasive ventilation immediately after extubation improves lung function in morbidly obese patients with obstructive sleep apnea undergoing laparoscopic bariatric surgery. Anesth Analg. 2010;111:519. doi: 10.1213/ANE.0b013e3181ef5e86. [DOI] [PubMed] [Google Scholar]


