Abstract
Background:
Sentinel lymph node biopsy (SLNB) is standard care to evaluate axillary involvement in early breast cancer. It has fewer complications than complete lymph node dissection; however, using blue dye in SLNB is controversial. We have evaluated the detection rate and local complications associated with methylene blue dye (MBD) used in SLNB in early breast cancer patients and compared these results to patent blue dye (PBD).
Materials and Methods:
In a cohort prospective study, 312 patients with early breast cancer without axillary lymph node involvement were divided into two groups according to dye type. All of the patients received radiotracer and one type of blue dye. We filled out a checklist for the patients that contained demographic data, size of tumor, stage, detection of sentinel lymph node, and complications and then analyzed the data.
Results:
Demographic and histopathologic characteristics were not significantly different in both groups. Mean (standard deviation [SD]) tumor size in all patients was 2.4 (0.8) cm. Detection rate in the MBD group was 77.5% with dye alone and 94.2% with dye and radioisotope; and in the PBD group it was 80.1% and 92.9% respectively (P > 0.05). We had blue discoloration of the skin in 23.7% in the PBD and 14.1% in the MBD group (P < 0.05) local inflammation was detected in one patient in the PBD and five in the MBD group (P < 0.05). Skin necrosis and systemic complications were not observed.
Conclusion:
Methylene blue has an acceptable detection rate, which may be a good alternative in SLNB. Complication such as blue discoloration of the skin was also lower with MBD.
Keywords: Blue dye, breast cancer, local complication, sentinel lymph node
INTRODUCTION
Breast cancer is the most prevalent cancer in women worldwide as well as in our country, greatly affecting the quality of life of those affected.[1] However, nowadays newer and less invasive techniques in breast cancer detection and staging can help in better prognosis and treatment of those affected. Sentinel lymph node biopsy (SLNB) involves identifying, removing, and analyzing the first lymph node (the sentinel lymph node [SLN]) that drains lymphatic fluid from the primary tumor and it is the preferred technique for staging in patients without clinical axillary lymphadenopathy. Moreover, compared with complete axillary dissection, SLNB has less complications such as lymphedema, nerve injury or future lymphangiosarcoma. Furthermore, axillary lymph node involvement is the most important predictor in breast cancer patients.[2,3,4]
Two techniques exist to locate the SLN (radionuclide injection and blue dye injection), and simultaneous use of both methods has better detection rates.[5,6] SLN mapping is used in many cancers such as melanoma, breast, endometrial, vulvar, thyroid, colon, nonsmall cell lung cancer, and squamous cell carcinoma of the head and neck.[7] Different types of blue dye are used for SLNB; however, none of them are considered to be the gold standard. Isosulfan blue is one of the most common dyes that is used in researches, but due to the anaphylactic reaction that patients have after its injection there are some concerns regarding it use.[6] Patent blue dye (PBD) is another dye used in SLN evaluation with reports of anaphylactic reactions as well.[8] Methylene blue dye (MBD) is an available dye that has less systemic complications in the literature. Furthermore, it is less expensive than the others and in countries with limited resources this is an important feature,[9] but there have been reports of skin and fat necrosis associated with its usage.[5]
In the current study, we compared two commonly available blue dyes in our region (MBD and PBD) to detect the SLN, and we evaluated their local complications.
MATERIALS AND METHODS
This was a prospective cohort study carried out on 312 patients with early breast cancer without axillary lymph node involvement. It was carried out in the teaching medical centers of the Mashhad University of Medical Sciences, Mashhad, Iran, between February 2010 and December 2012.
The patients were divided into two groups according to the type of dye selection (156 in each group). This study was performed in two centers with the same surgery team that also participated in our research. One type of blue dye is used more in each center based on availability. After admission to the hospital, the patients randomly received one of the blue dyes.
Patients with a diagnosis of breast cancer (diagnosed by needle biopsy or open surgical biopsy) with T1, T2 (tumor size <5 cm), without axillary lymph node involvement in a clinical exam, were enrolled in the study. They were divided into two groups according to the type of dye injection. Patients with T3, T4, and inflammatory cancers, and palpable axillary lymphatic nodes, including pregnant patients, those who were going to have an axillary surgery, male patients, and those with a history of neo-adjuvant chemotherapy were not included.
All patients received a preoperative intradermal injection of technetium-99 m-phytate in the periareolar area and had a subsequent lymphoscintigraphy in our nuclear medicine department the morning of the surgery. Then, in the operating room the surgeon injected 2 cc of blue dye in the subareolar before the procedure.
Biopsy technique
After general anesthesia and dye injection, a 3-4 cm incision was made in the axillary region (on the hairline), the blue node [Figure 1] or a node with a blue lymphatic channel (stained node) with high radioactivity (hot node) was identified and diagnosed as the SLN and was sent to the pathologic department for frozen section examination. If there was >10% background radioactivity, more sentinel nodes would have been detected. However, if there was <10% radioactivity of the first node in the axillary basin after SLN removal then surgery could be terminated.[10] In addition, all of the surgeons of the team were experts and had passed the learning curve for SLNB.
Figure 1.
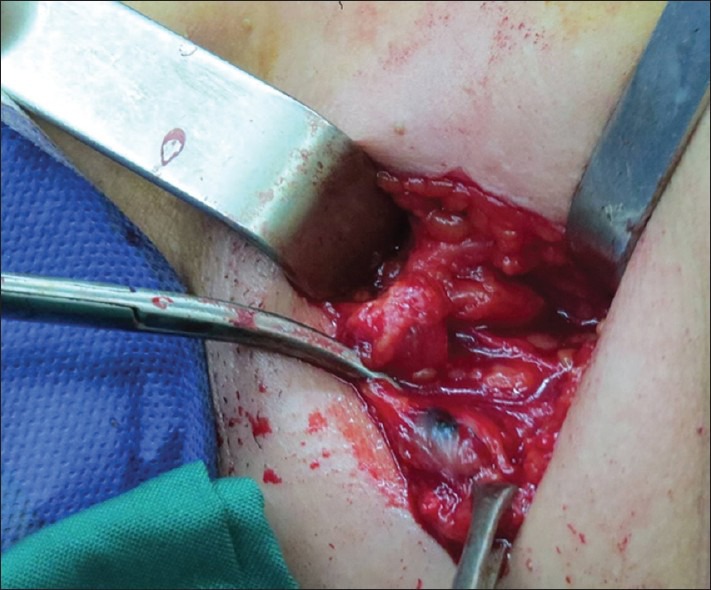
An intraoperative picture of sentinel lymph node surgery in axilla that shows a blue node colored with methylene blue dye
We performed the biopsy in two hospitals, so we had two radioactivity detectors. The gamma-probe (navigator) system with sound effects counts radioactivity of the node in 10 s and shows the number. The higher activity of the node is shown with a higher green number and higher sound. The Euro probe system has a similar function but uses color changes as well. The hot node has a higher sound and number and is indicated by a red color. The probe has two sizes, one for the axilla and smaller incisions like for parathyroid or nonpalpable mass surgery. Both of the detectors had good sensitivity that did not influence the detection rate.[11]
In addition, if the node was just hot with no blue staining or was not hot but had blue staining, it was recorded separately on a checklist. Then we examined the frozen section to detect SLN metastasis. After axillary node detection, the surgeon did the proper breast surgery for the patient (lumpectomy or mastectomy). We evaluated the local complications of the dye injection after surgery.
The study was approved by the Ethics Committee of the Mashhad University of Medical Sciences, Mashhad, Iran (Code No. 2293). All patients signed an informed consent form to participate in the study.
After collecting data, we used SPSS version 11.5 (SPSS Inc., Chicago, IL) to analyze the data. We used the Chi-square test for qualitative parameters and the independent simple t-test and Mann–Whitney U-test for qualitative parameters to compare the two groups. We used logistic regression to evaluate local complications. A P < 0.05 was considered significant.
RESULTS
We had 312 patients, and their mean age was 51.5 (11.8) years old.
There were not any significant differences between the two groups in the demographic data like age, tumor size, number of detected sentinel node and histopathology [Table 1]. Mean tumor size was 2.45 cm (SD = 0.8). Range of detected SLN was 1-3 lymph nodes in each surgery. In 120 (38%) of the patients, the SLN had metastasis as was shown in the frozen section examination and so the surgeon did axillary dissection. Figure 2 shows the range of tumor size in the patients.
Table 1.
Patient's demographic and histopathologic data
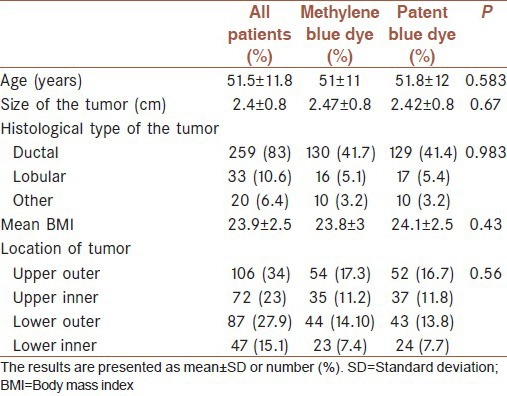
Figure 2.
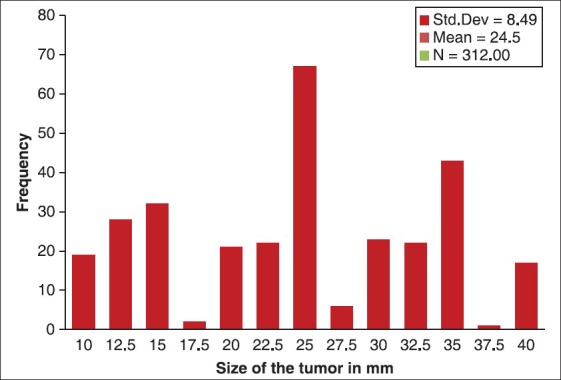
Range of tumor size
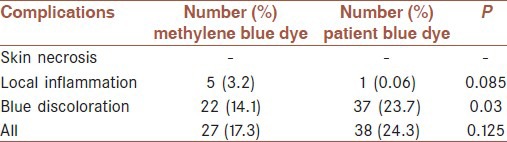
Sentinel lymph node detection rate was not significantly different between the two groups Table 2 shows the SLN detection rate between the two groups. We had no skin necrosis; however, blue tattooing of the skin [Figure 3] was significantly higher in the patent blue group with 23.7% versus 14.1% (P = 0.03) and local inflammation was higher in the MBD group with 3.2% versus 0.6% (P < 0.05). Table 3 shows local complications in both groups. We had no systemic complications, but local complications were recorded in 27 patients (17.3%) in the MBD and in 38 (24.3%) in the PBD group (P = 0.125). Local complications were relieved without any other surgical intervention.
Table 2.
Detection rate of sentinel lymph node in patients differences were not significant between the two groups (P>0.05)
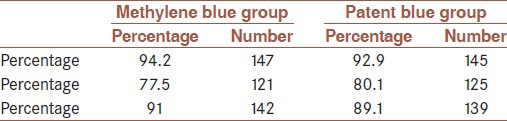
Figure 3.

Blue tattooing of the skin after methylene blue dye injection
Table 3.
Comparison of local complications of blue dyes between 2 groups
DISCUSSION
We use radiotracer and one kind of blue dyes (Patent Blue or Methylene Blue) for SLN surgery in our early stage breast cancer patients. The comparison between the two groups showed they are similar in demographic data and histopathology of tumors. SLN detection rate was not significantly different between the two groups; it was in patent blue patients 80% versus 77.5% in MBD alone. In combination of blue dye and radiotracer, we had an acceptable detection rate in both groups at 94.2% (147 patients out of 156) in the MBD group and 92.4% (145 out of 156) in the PBD group (P > 0.05).
Sentinel lymph node biopsy in early stage breast cancer patients (no clinical axillary lymphadenopathy) reduce complications associated with complete axillary lymph node dissection. It is also the preferred method of breast cancer staging in women with early breast cancer who are clinically node negative by a physical examination and imaging studies.[2,3,12] In addition, the combination of blue dye with a radiotracer increases the detection rate of SLNs.[5,6] However, between the different types of blue dye, none of them is the gold standard in SLNB according to the current literature and local or systemic complications with different detection rates have been indicated.[5,8,9]
These complications are allergic and nonallergic reactions like skin rash, and erythema, and systemic reactions like urticarial and anaphylaxis and interference with pulse oximetry, skin, and body fluid discoloration and local complications like skin necrosis.[9,13,14] Isosulfan blue dye is one of the most popular dyes under study for SLNB in breast cancer research, even in our country. However, concerns regarding its systemic reaction, especially in higher rates of anaphylaxis reaction, exist[15,16] PBD is another routine dye in SLNB that is used in our country, and some authors have reported anaphylactic reaction after its use.[17,18] MBD has been introduced as an available, cheap, and safe dye with very low systemic reaction.[9,19] Nonetheless, some studies have reported blue discoloration of the skin,[20] local inflammation, and skin or fat necrosis after MBD injections.[5,21,22,23] However, most of the necrosis was reported after peritumoral and subdermal injections.[21,24]
In our study the differences of tumor size, age, histopathology, rate of lymph node metastasis were not statistically significant between the two groups understudy. The detection rate for blue dye alone was 77.5% in MBD and 80.1% in PBD. Furthermore, it was lower in MBD, but that was not statistically significant (P > 0.05). Wallace et al. reported 64.1% (No of nodes) and 88.5% (No of patients) detection rate in 148 patients (209 detected node) with Vital Blue Dye alone, and 98.6% by radiotracer and dye and these results were higher than ours.[25]
With a combination of blue dye and radiotracer we had acceptable detection rates in both groups; 92.9% in PBD and 94.2% in MBG (P > 0.05) and this was similar to Pesek et al.'s meta-analysis article. They concluded that a radiotracer should be used with blue dye to reduce the false negative rates in SLNB.[26] We had lower detection rates in both groups with blue dye alone than the combination group. However, Takamaru believes that because of the limitation of gamma-probe equipment in some centers, using dye-guided SLN alone reduces unnecessary axillary dissection in breast cancer patients. Takamaru et al. reported a high detection rate with blue dye alone in 96.8% of the 374 patients they studied.[27] The range of sentinel nodes in his study was between 1 and 10, but we had 1-3 nodes in every surgery and perhaps this was the reason for lower detection rates in our patients with dye alone.
There are more reports of anaphylaxis related to the usage of patent blue and Isosulfan blue than MBD, but skin necrosis was more common after MBD.[28] Reyes et al. reported two patients with skin necrosis after MBD injection.[21] In our study, none of our patients needed more surgical intervention due to dye complications.
We had local inflammation in 5 (3.2%) patients from the MBD group in comparison with 1 (0.6%) in PBD and blue tattooing in 14.1% in MBD and 23.7% in the PBD group (P = 0.03).
Our result showed more local inflammation in the MBD group and more tattooing in PBD. Zakaria et al. reported on three groups of 308 patients with different injection sites and concentrations of methylene blue. They concluded that subareolar injections and lower concentrations had lower complications (2%) in comparison to peritumoral and high concentrations (21%) (P = 0.0003).[5] They reported 99.7% overall detection of SLNs. In our study, we injected MBD into the subareolar, and we had a good detection rate (94.2%) without any necrosis.
Govaert et al. conducted a retrospective review of 33 patients, and they showed that intradermal injections of patent blue caused long-term blue discoloration of the skin in the injection site.[20] Also, Varghes et al. used MBD with the subareolar and subdermal injection method and found it safe and effective in SLN detection with only blue tattooing as a complication.[29] The two study results are similar to ours; however, we had a shorter follow-up than Govaert's report. Moreover, we had no systemic reactions or skin necrosis in our series, and we had a significantly lower rate of blue discoloration in the MBD group than PBD. We had good detection rates with MBD compared to PBD with a low complication rate and no systemic reactions in our patients. Due to the low rate of these complications and rare anaphylactic reactions to methylene blue, larger studies with more patients than what was in our study are recommended.[30]
CONCLUSION
Our results suggest that MBD is a safe and cost-effective dye with an acceptable detection rate and low complications and could be used as an available blue dye in SLN surgery in breast cancer patients.
AUTHORS CONTRIBUTION
ASF contributed in study design, doing surgery, following patients, writing draft of article and editing. RS contributed in doing lymphoscintigraghy of the patients, data analysis, study design, editing the final draft. OR contributed in data collection, searching about similar researches, writing the manuscript. AA and MNF and AT contributed in doing surgery, following patients and writing the draft.
ACKNOWLEDGMENT
This article is driven from medical thesis by Omid Rohbakshfar MD (code number 2672) and supported by Mashhad University of Medical Sciences.
Footnotes
Source of Support: Mashhad University of Medical Sciences, Mashhad, Iran
Conflict of Interest: The authors declare no conflict of interest in this project.
REFERENCES
- 1.Sadjadi A, Nouraie M, Ghorbani A, Alimohammadian M, Malekzadeh R. Epidemiology of breast cancer in the Islamic Republic of Iran: First results from a population-based cancer registry. East Mediterr Health J. 2009;15:1426–31. [PubMed] [Google Scholar]
- 2.Simmons R, Thevarajah S, Brennan MB, Christos P, Osborne M. Methylene blue dye as an alternative to isosulfan blue dye for sentinel lymph node localization. Ann Surg Oncol. 2003;10:242–7. doi: 10.1245/aso.2003.04.021. [DOI] [PubMed] [Google Scholar]
- 3.Bafford A, Gadd M, Gu X, Lipsitz S, Golshan M. Diminishing morbidity with the increased use of sentinel node biopsy in breast carcinoma. Am J Surg. 2010;200:374–7. doi: 10.1016/j.amjsurg.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 4.Pruthi S, Haakenson C, Brost BC, Bryant K, Reid JM, Singh R, et al. Pharmacokinetics of methylene blue dye for lymphatic mapping in breast cancer-implications for use in pregnancy. Am J Surg. 2011;201:70–5. doi: 10.1016/j.amjsurg.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Zakaria S, Hoskin TL, Degnim AC. Safety and technical success of methylene blue dye for lymphatic mapping in breast cancer. Am J Surg. 2008;196:228–33. doi: 10.1016/j.amjsurg.2007.08.060. [DOI] [PubMed] [Google Scholar]
- 6.Blessing WD, Stolier AJ, Teng SC, Bolton JS, Fuhrman GM. A comparison of methylene blue and lymphazurin in breast cancer sentinel node mapping. Am J Surg. 2002;184:341–5. doi: 10.1016/s0002-9610(02)00948-0. [DOI] [PubMed] [Google Scholar]
- 7.Keller B, Yawalkar N, Pichler C, Braathen LR, Hunger RE. Hypersensitivity reaction against patent blue during sentinel lymph node removal in three melanoma patients. Am J Surg. 2007;193:122–4. doi: 10.1016/j.amjsurg.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Lanitis S, Filippakis G, Sidhu V, Al Mufti R, Lee TH, Hadjiminas DJ. Atypical anaphylactic reaction to patent blue during sentinel lymph node biopsy for breast cancer. Ann R Coll Surg Engl. 2008;90:338–9. doi: 10.1308/003588408X285702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramin S, Azar FP, Malihe H. Methylene blue as the safest blue dye for sentinel node mapping: Emphasis on anaphylaxis reaction. Acta Oncol. 2011;50:729–31. doi: 10.3109/0284186X.2011.562918. [DOI] [PubMed] [Google Scholar]
- 10.Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: Overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33. doi: 10.1016/S1470-2045(10)70207-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sadeghi R, Alesheikh G, Zakavi SR, Fattahi A, Abdollahi A, Assadi M, et al. Added value of blue dye injection in sentinel node biopsy of breast cancer patients: Do all patients need blue dye? Int J Surg. 2014;12:325–8. doi: 10.1016/j.ijsu.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 12.Newman EA, Newman LA. Lymphatic mapping techniques and sentinel lymph node biopsy in breast cancer. Surg Clin North Am. 2007;87:353–64, viii. doi: 10.1016/j.suc.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 13.Bézu C, Coutant C, Salengro A, Daraï E, Rouzier R, Uzan S. Anaphylactic response to blue dye during sentinel lymph node biopsy. Surg Oncol. 2011;20:e55–9. doi: 10.1016/j.suronc.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Liang MI, Carson WE., 3rd Biphasic anaphylactic reaction to blue dye during sentinel lymph node biopsy. World J Surg Oncol. 2008;6:79. doi: 10.1186/1477-7819-6-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Montgomery LL, Thorne AC, Van Zee KJ, Fey J, Heerdt AS, Gemignani M, et al. Isosulfan blue dye reactions during sentinel lymph node mapping for breast cancer. Anesth Analg. 2002;95:385–8. doi: 10.1097/00000539-200208000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Aydogan F, Celik V, Uras C, Salihoglu Z, Topuz U. A comparison of the adverse reactions associated with isosulfan blue versus methylene blue dye in sentinel lymph node biopsy for breast cancer. Am J Surg. 2008;195:277–8. doi: 10.1016/j.amjsurg.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Barthelmes L, Goyal A, Newcombe RG, McNeill F, Mansel RE NEW START and ALMANAC Study Groups. Adverse reactions to patent blue V dye - The NEW START and ALMANAC experience. Eur J Surg Oncol. 2010;36:399–403. doi: 10.1016/j.ejso.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 18.Joshi M, Hart M, Ahmed F, McPherson S. Adverse reaction; patent blue turning patient blue. BMJ Case Rep 2012. 2012 doi: 10.1136/bcr-2012-007339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harkrider WW, Diebold AE, Maloney T, Espenan G, Wang YZ, Stafford SJ, et al. An extended phase II trial of iodine-125 methylene blue for sentinel lymph node identification in women with breast cancer. J Am Coll Surg. 2013;216:599–605. doi: 10.1016/j.jamcollsurg.2012.12.044. [DOI] [PubMed] [Google Scholar]
- 20.Govaert GA, Oostenbroek RJ, Plaisier PW. Prolonged skin staining after intradermal use of patent blue in sentinel lymph node biopsy for breast cancer. Eur J Surg Oncol. 2005;31:373–5. doi: 10.1016/j.ejso.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Reyes F, Noelck M, Valentino C, Grasso-Lebeau L, Lang J. Complications of methylene blue dye in breast surgery: Case reports and review of the literature. J Cancer. 2010;2:20–5. [PMC free article] [PubMed] [Google Scholar]
- 22.Salhab M, Al Sarakbi W, Mokbel K. Skin and fat necrosis of the breast following methylene blue dye injection for sentinel node biopsy in a patient with breast cancer. Int Semin Surg Oncol. 2005;2:26. doi: 10.1186/1477-7800-2-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ha KY, Parish D, Hamilton R, Wang JC. Fat necrosis in the breast from methylene blue dye injection. Proc (Bayl Univ Med Cent) 2013;26:298–9. doi: 10.1080/08998280.2013.11928990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stradling B, Aranha G, Gabram S. Adverse skin lesions after methylene blue injections for sentinel lymph node localization. Am J Surg. 2002;184:350–2. doi: 10.1016/s0002-9610(02)00945-5. [DOI] [PubMed] [Google Scholar]
- 25.Wallace AM, Han LK, Povoski SP, Deck K, Schneebaum S, Hall NC, et al. Comparative evaluation of [(99m) tc] tilmanocept for sentinel lymph node mapping in breast cancer patients: Results of two phase 3 trials. Ann Surg Oncol. 2013;20:2590–9. doi: 10.1245/s10434-013-2887-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pesek S, Ashikaga T, Krag LE, Krag D. The false-negative rate of sentinel node biopsy in patients with breast cancer: A meta-analysis. World J Surg. 2012;36:2239–51. doi: 10.1007/s00268-012-1623-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takamaru T, Kutomi G, Satomi F, Shima H, Ohno K, Kameshima H, et al. Use of the dye-guided sentinel lymph node biopsy method alone for breast cancer metastasis to avoid unnecessary axillary lymph node dissection. Exp Ther Med. 2014;7:456–60. doi: 10.3892/etm.2013.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Masannat Y, Shenoy H, Speirs V, Hanby A, Horgan K. Properties and characteristics of the dyes injected to assist axillary sentinel node localization in breast surgery. Eur J Surg Oncol. 2006;32:381–4. doi: 10.1016/j.ejso.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 29.Varghese P, Abdel-Rahman AT, Akberali S, Mostafa A, Gattuso JM, Carpenter R. Methylene blue dye – a safe and effective alternative for sentinel lymph node localization. Breast J. 2008;14:61–7. doi: 10.1111/j.1524-4741.2007.00519.x. [DOI] [PubMed] [Google Scholar]
- 30.Jangjoo A, Forghani MN, Mehrabibahar M, Sadeghi R. Anaphylaxis reaction of a breast cancer patient to methylene blue during breast surgery with sentinel node mapping. Acta Oncol. 2010;49:877–8. doi: 10.3109/02841861003769964. [DOI] [PubMed] [Google Scholar]


