Abstract
Background:
The Rome II and III diagnostic criteria for dyssynergic defecation recommended the exclusion of irritable bowel syndrome (IBS). This study determined the effect of biofeedback therapy on dyssynergic constipation in patients with or without IBS.
Materials and Methods:
This study was a nonrandomized, single blinded, semi experimental study. Dyssynergic defecation patients with and without IBS were asked to undergo biofeedback therapy 8 sessions. The defecation dynamics and balloon expulsion time were evaluated before, at the end and 1 month after the biofeedback therapy. IBS symptoms were graded using a 4-point Likert scale. Mann–Whitney U-test, Wilcoxon test and Friedman test were applied to analyze data using SPSS software package (SPSS Inc., Chicago, IL, USA).
Results:
After the biofeedback therapy, the IBS symptoms have been decreased significantly (the median of 2 before and 1 after therapy, P < 0.01). The biofeedback therapy significantly decreased the anismus index in IBS group by the mean of 0.75 ± 0.31, 0.28 ± 0.07 and 0.28 ± 0.06 in three phases, respectively. Similar results were found in non-IBS patients (the mean of 0.74 ± 0.32, 0.28 ± 0.08, 0.27 ± 0.08 in three phases, respectively). The symptoms of constipation (sensation of incomplete evacuation, difficult and painful defecation), defecation facilitative manual maneuver frequency, pelvic floor muscles resting amplitude and strain amplitude decreased and squeezing amplitude improved significantly after biofeedback therapy in both groups with and without IBS (P < 0.001). There were not significant differences between patients with and without IBS (P > 0.05) with respect to outcome. No complication was observed in treatment groups.
Conclusion:
Dyssynergic constipation patients with and without IBS will likely benefit from biofeedback therapy.
Keywords: Biofeedback, dyssynergic constipation, irritable bowel syndrome
INTRODUCTION
Constipation is one of the most common health problems recently and affects all education and socioeconomic levels.[1] Simply, constipation has been defined as <3 stools/week.[2] However, recent studies report that most constipated patients complain about excessive straining, incomplete evacuation, or hard stools rather than infrequent stooling.[2,3,4,5]
Even though there is some overlap, 3 subtypes of constipation have been characterized: Dyssynergic defecation, slow transit constipation, and irritable bowel syndrome (IBS) with constipation.[2,6,7,8,9] One of the most frequent forms of chronic constipation is dyssynergic defecation. It has been estimated that nearly one-third of constipation patients in tertiary care centers have dyssynergic defecation.[10,11] Chiarioni et al.[9] characterized this functional defecation disorder by incomplete evacuation of fecal material from the rectum due to paradoxical contraction or failure to relax pelvic floor muscles, particularly the puborectalis muscle and the external anal sphincter, when straining to defecate.[12]
Several studies have been conducted on this functional defecation disorder, providing greater clarity in your understanding and encouraging to apply of behavioral therapy, more concretely, biofeedback techniques.[12,13] Their results suggested biofeedback therapy when patients with pelvic floor dyssynergia do not benefit from conservative interventions, such as dietary recommendations, bowel scheduling, and medications.[14,15]
It is defined that biofeedback involves the use of pressure measurements (manometry) or averaged electromyographic activity within the anal canal to teach patients how to relax pelvic floor muscles when straining to defecate.[12] Biofeedback is performed in rehabilitation medicine settings. In recent years several randomized controlled trials (RCT) have been conducted and reported that biofeedback is more effective than laxatives,[16] relaxation training,[2] pharmacological treatment (for example diazepam) and placebo.[15] Based on the results of Chiarioni et al., biofeedback appears to be the treatment of choice for dyssynergic defecation in chronic constipated adults.[9]
In addition, 82% of chronic constipation patients have the criteria for IBS.[3] Incomplete evacuation and excessive straining are common symptoms in both dyssynergic defecation and patients with IBS.[4,5] Association of symptoms of incomplete evacuation and rectal hypersensitivity in IBS has been shown.[6] The primary is abdominal bloating and abdominal pain/discomfort is major symptom of IBS usually improved by successful bowel evacuations.[17] Biofeedback therapy may improve not only the constipation symptoms but also symptoms through the increasing the chances of successful bowel movements in dyssynergic constipation patients with IBS.
In contrast, if the rectal hypersensitivity is not corrected, the outcome of biofeedback therapy in dyssynergic defecation with IBS may adversely be affected by the existence of incomplete evacuation and rectal hypersensitivity in IBS. Biofeedback therapy using the manometric technique has been reported to be an effective treatment for dyssynergic defecation.[12] Chiarioni et al. reported that bloating symptoms in chronic constipation patients improved after biofeedback therapy.[9] In addition, improvement of both constipation and abdominal bloating/discomfort in patients suffering from both anorectal dyssynergia and IBS was indicated. Nevertheless, the Rome II and III criteria recommended that patients with coexisting dyssynergic defecation and IBS have to be excluded before the diagnosis of dyssynergic defecation.[18,19] If the outcome of the biofeedback therapy is not affected by the existence of IBS in dyssynergic defecation, the Rome criteria may mislead physicians and prevent many patients who suffer from both IBS and dyssynergic benefit from biofeedback therapy. On the contrary, if the existence of IBS adversely affects the treatment result, excluding constipation patients with IBS from the anorectal physiologic tests and biofeedback therapy will save the management cost in this patient group.[10]
Therefore the main aim of this study was to determine the effect of biofeedback therapy in dyssynergic defecation patients with and without IBS and compare the outcome of biofeedback therapy in both groups. This is particularly important because the Rome III criteria clearly exclude patients with IBS from consideration of a diagnosis of dyssynergic defecation. As a result, it is vague whether patients with dyssynergic defecation and simultaneous IBS symptoms should or should not be considered as proper candidates for treatment with biofeedback therapy.
MATERIALS AND METHODS
Study design and participants
This study was a nonrandomized, single blinded, semi experimental which approved in Tehran University of medical science ethics committee with 91/d/130/2135 reference number. Adult female outpatients, 15-75 years old with constipation who were referred from colorectal surgeon and gastroenterology clinic to physical medicine and rehabilitation clinic, Firoozgar Hospital, Tehran, Iran as defined by the Rome III criteria, both with and without IBS were invited to participate in the study. The patients had failed standard treatment of constipation with fiber diet, exercises, laxatives and anti IBS drugs for IBS group.
For sample size calculation to detect a 13% difference between Anismus index mean in both group with IBS and non-IBS following formula[20] was applied:
The standard deviation (SD) from pilot study was estimated to be 0.14. For a two-sided 5% significant level, Zα = 1.96 and for 80% power, Zβ = 0.84. Substituting these values into above formula, N = 2 (1.96 + 0.84)2 0.142/0.132 or approximately 19 participants in each group.
Patients had to fulfill Rome III criteria for pelvic floor dyssynergia[7,10] - (1) Two or more symptoms of functional constipation for at least 12-week in past year included straining, lumpy or hard stools, sensation of incomplete evacuation, sensation of anorectal blockage, manual maneuvers to facilitate defecation, <3 defecation per week. (2) Manometric, electromyography (EMG), or radiologic evidence for inappropriate contraction or failure to relax the pelvic floor muscles during attempts to defecate. (3) Evidence for inadequate propulsive forces during attempts. (4) Evidence of incomplete evacuation. Patients are matched in two groups in terms of age, education and duration of symptoms.
Patients who presented the followings were excluded from the study:
History of gastroenterology, pelvic and spinal surgery (except appendectomy, cholecystectomy and hysterectomy).
Neurological disease included multiple sclerosis, stroke, spinal cord injury, Parkinson disease and cognitive impairment.
Usage of opioids and drugs may cause constipation.
Pregnancy.
Previous biofeedback therapy.
History of chronic disease such as heart or renal disease and hypothyroidism.
Rectal prolapses, fissures and rectal bleeding.
Electrolyte impairment, anemia and history of serious weight loss.
Patients who had recurrent abdominal pain/discomfort >3 days/month for the past 3 months associated with >2 of the followings are placed in dyssynergic constipation with IBS group. (a) Improvement with defecation. (b) Onset associated with change in stool frequency. (c) Onset associated with change in stool form and <25% loose or watery stools. All of the patients provided written informed consent before inclusion in the study.
Procedure and variable assessment — informed consent was obtained from the participants. All the patients received biofeedback therapy 8 sessions, twice weekly (With myotrack infinity, made in Canada instrument). Each 45-60 min session consisted of visual, verbal and auditory feedback technique with solid rectal probe that use from surface EMG.[2,10]
Verbal feedback was provided every 10 min by a physiotherapist that was not aware of patient's IBS status. Auditory feedback was provided with music and visual feedback with fulfilling of puzzle on monitor. Each session, therapist explained about strain, squeeze and sequence of biofeedback therapy. Gel lubricated rectal probe was placed in rectum while patient was supine. Ground electrode was placed on anterior superior iliac spine. Surface electromyographic signal of pelvic floor muscle recorded in strain, squeeze and rest. Since surface EMG has not great accuracy and some factors like muscular fatigue and electrode movement may change the signal, mean of 5 contractions were recorded.
Biofeedback phases, initially for training, therapist set the device's threshold up to each patient's squeeze threshold. Whether the patient could squeeze enough, she received auditory, verbal and visual feedback and 10 s resting between two squeezes. All the patients were instructed in performing diaphragmatic breathing exercises during the treatment period. In the 4th session patients were evaluated, if mean amplitude of pelvic floor muscles during strain was < 5 μV, slow twitch muscle fibers exercises with 15 s squeeze on 60% of maximal threshold were done. However if strain maneuver after 3 sessions was not efficient, resting exercises with amplitude of < 5 μV were done.[2,8,10,16]
During biofeedback therapy and 4-week follow-up period, patients were advised to use only magnesium hydroxide syrup and bisacodyle suppository if constipation continues after 48 h. Medications for IBS, including antispasmodics, tegaserod and antidepressants (tegaserode has been removed from market since 2007 due to cardiovascular outcomes) were prohibited during the study period [Figure 1].
Figure 1.
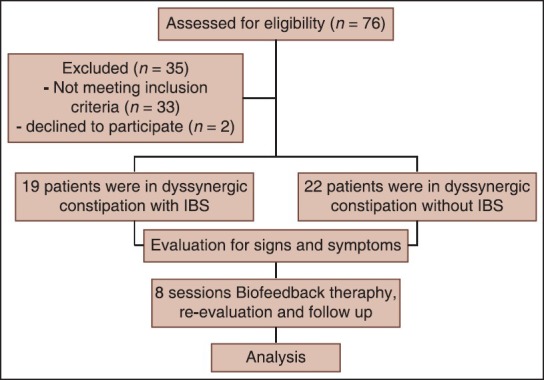
Consort diagram
Primary IBS symptoms (abdominal bloating and abdominal discomfort/pain) and other gastrointestinal symptoms including early satiety, anorexia, nausea and heart burn were evaluated immediately before the first biofeedback session, after session 8 and 4-week after the end of treatment, using a 4-point Likert scale[10] (0 = No symptom, 1 = mild symptoms, 2 = moderate symptoms, 3 = severe symptoms) according to patient's feeling.
Mean amplitude of pelvic floor muscles during rest, strain and squeeze and anismus index were recorded[10] at three phases (before the first biofeedback session, after session 8 and 4-week after the end of treatment).
Constipation symptoms[10] (sensation of incomplete evacuation, difficult and painful defecation) were evaluated using a 10 cm visual analog scale. In addition, stool frequency per week, frequency and types of laxative consumed, defecation facilitative manual maneuver frequency were recorded.
Balloon expulsion time, 30 ml volume, with Foley catheter (16 or 18 French) was used to record the time that patients need to defecate the balloon. If time was above 5 min, the researcher depleted and brought out balloon. This variable was evaluated at three phases.[2,10]
Statistical analysis
The data were analyzed using SPSS software for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics were expressed as the means ± SD for continuous variables, median and range (min-max) for ordinal variables and frequency and percentage for categorical variables. Mann–Whitney U-test was used for comparing two groups in three phases separately. Friedman's two-way ANOVA test was applied to analyze ordinal outcomes. A repeated measure ANOVA was used to analyze continuous outcomes. Post-hoc tests were done using the Bonferroni correction. Mauchly's test of Sphericity indicated that the assumption of sphericity had been violated and therefore, a Greenhouse-Geisser correction was used. A P < 0.05 was considered to be statistically significant.
RESULTS
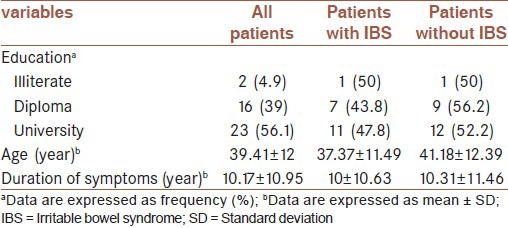
Forty-one female patients completed the biofeedback treatment protocol. Among them 19 patients (46.3%) also fulfilled the criteria of IBS. The mean age of patients was 39.41 ± 12 ranged from 19 to 62. Twenty-three patients had high level of education (56.1%), 16 finished high school and two patients were under high school. Patients who had IBS were younger in age (37.37 ± 11.49), but there was not any statistically significant difference (P > 0.05). Education levels were similar between patients with and without IBS (P > 0.05). Duration of symptoms was approximately similar in both groups with and without IBS (P > 0.05) [Table 1].
Table 1.
Patient epidemiological characteristics
In three phases (baseline, treatment and follow-up), the prevalence of each constipation symptom (sensation of incomplete evacuation, difficult and painful defecation), stool frequency per week, frequency and types of laxative consumed, defecation facilitative manual maneuver frequency, balloon expulsion times, anismus index, resting-amplitude, squeezing-amplitude, and strain-amplitude were similar between patients with and without IBS (>0.05). As a result, coexistence of IBS did not have a significant effect on the outcome of biofeedback therapy. According to the mean of 4-point Likert scale, after the biofeedback therapy, the IBS symptoms have been decreased significantly (P < 0.01). Significant differences between baseline assessment and treatment (P < 0.01), and between baseline assessment and follow-up (P < 0.01), but not between treatment and follow-up (P > 0.05) has been shown. Thus biofeedback therapy also had an effective impact on improvement of IBS symptoms.
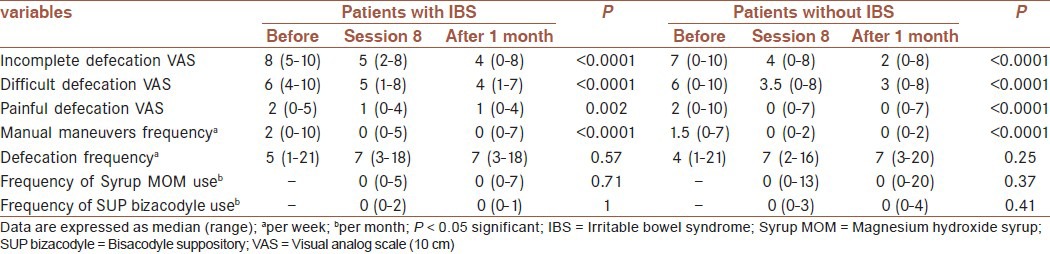
As shown in Table 2, the results of Friedman's two-way ANOVA test determined that the biofeedback therapy significantly decreased the subjective symptoms of constipation (sensation of incomplete evacuation, difficult and painful defecation) and defecation facilitative manual maneuver frequency in both patients with and without IBS (P < 0.01). Respect to the differences between phases for each outcomes, the results revealed significant differences between baseline assessment and treatment (P < 0.01), and between baseline assessment and follow-up (P < 0.01), but not between treatment and follow-up (P > 0.05). Defecation frequency has been improved in both groups with and without IBS but no significant result has been shown. There were no significant differences in frequency and types of laxative consumed in two phases.
Table 2.
Subjective patient symptoms and anorectal function parameters before, at the end of and after biofeedback therapy in dyssynergic constipation patients with and without IBS
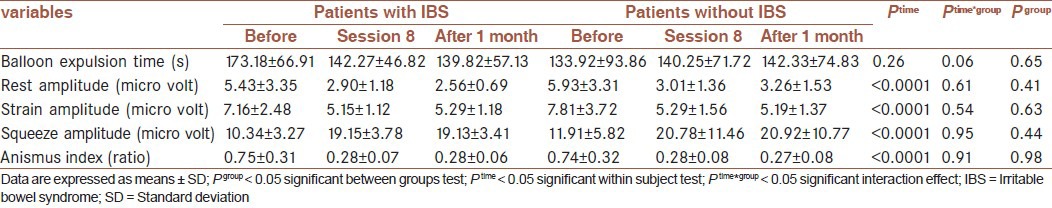
In terms of objective symptoms, repeated measures ANOVA with a Greenhouse-Geisser correction results were shown in Table 3. The between groups tests for each outcomes indicated that there were not significant differences between patients with and without IBS (P > 0.05). The within subject test indicated that there is a significant time effect (P < 0.0001). In other words, the patients with and without IBS do change over time, both groups were getting less anismus index, pelvic floor muscles resting amplitude and strain amplitude and more squeezing amplitude over time. Post-hoc tests using the Bonferroni correction for each outcomes revealed that significant differences between baseline assessment and treatment (P < 0.0001), and between baseline assessment and follow-up (P < 0.0001), but not between treatment and follow-up (P > 0.05). The interaction of time and group is not significant, which means that the patients with and without IBS are changing over time, but are changing in the same ways. The results for balloon expulsion times were not significant.
Table 3.
Objective patient symptoms and anorectal function parameters before, at the end of and after biofeedback therapy in dyssynergic constipation patients with and without IBS
DISCUSSION
The main purpose of this study was to evaluate the effect of biofeedback therapy in dyssynergic defecation patients with and without IBS and compare in both groups to inhibit exclusion of IBS patients with Rome III criteria from dyssynergic defecation and consider all two groups to treat with biofeedback properly and inhibit mislead of physicians in treating IBS patients that form about half of dyssynergic constipation in society.
Heyman in 2007 studied 84 dyssynergic constipation patients in three groups as RCT study, they all did squeeze and strain exercises, one group had EMG biofeedback therapy too and after 3 months follow-up EMG biofeedback group had best outcome.[15]
Patcharatrakul in 2011 studied patients with dyssynergic constipation in two groups of IBS and none IBS patients, they all had 4 sessions biofeedback therapy and there was no difference between their outcomes.[10]
The results obtained in this study have shown that 46.3% of patients with dyssynergic constipation fulfilled the Rome II criteria for IBS and the existence of IBS did not affect the outcome of the biofeedback therapy. The patients with or without IBS indicated a similar improvement of their constipation symptoms after the biofeedback therapy. Therefore this study demonstrated that dyssynergic defecation can be treated effectively with EMG-biofeedback therapy. Through EMG-biofeedback, the patients have been taught to relax external anal sphincter during straining to defecate, decreasing significantly the anismus index. This learning process led to reduction of obstructive symptoms, with a significant decrease in sensation of incomplete evacuation, difficulty evacuation level and perianal pain at defecation. Our results are in consistency with the findings of Patcharatrakul and Gonlachanvit.[10]
In addition, the biofeedback therapy improved IBS symptoms. This finding is in agreement with other studies that reported an improvement of abdominal pain and bloating after biofeedback therapy in patients with constipation.[16,21,22] Nevertheless, Rome II and III criteria recommended that dyssynergic constipation patients with IBS must be excluded before the diagnosis of dyssynergic defecation. This may mislead physicians and prevent more than half of the patients with dyssynergic defecation benefit from the appropriate diagnostic tests and therapy.
The results of this study suggest that dyssynergic constipation can imitate IBS and that the identification and treatment of anorectal dyssynergia can improve IBS symptoms. Consequently, constipation patients with IBS who have symptoms that interfere with their quality of life should undergo colonic and anorectal physiological tests similarly to constipation patients without IBS to establish the presence of anorectal dyssynergia. In this study, we demonstrated a subjective and objective improvement of their overall constipation symptoms. This finding is similar to that reported in previous studies that used manometry[2,23,24,25,26,27,28] or EMG-based techniques.[16] Little sample size and short time follow-up were the limitations of this study, The most important strength of this study is its new topic, how other studies evaluated the influence of biofeedback therapy in dyssynergic constipation patients with and without IBS separately.
CONCLUSION
This study demonstrates that EMG-biofeedback is an effective behavioral treatment for constipation in dyssynergic patients with and without IBS. In addition, the existence of IBS in dyssynergic constipation patients does not affect the outcome of the biofeedback therapy. Dyssynergic constipation patients with or without IBS will likely benefit from biofeedback therapy.
AUTHOR'S CONTRIBUTIONS
TA, FM, BF and G.RR carried out the design and coordinated the study, participated in most of the experiments and prepared the manuscript. SSD and SMD provide assistance in the design of the study, coordinated and carried out all the experiments and participated in manuscript preparation. RBB carried out all the biofeedback therapy. RM and BM diagnosed constipation and participated in manuscript preparation. All authors have read and approved the content of the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Stessman M. Biofeedback: Its role in the treatment of chronic constipation. Gastroenterol Nurs. 2003;26:251–60. doi: 10.1097/00001610-200311000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Rao SS, Seaton K, Miller M, Brown K, Nygaard I, Stumbo P, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2007;5:331–8. doi: 10.1016/j.cgh.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 3.Rao SS, Tuteja AK, Vellema T, Kempf J, Stessman M. Dyssynergic defecation: Demographics, symptoms, stool patterns, and quality of life. J Clin Gastroenterol. 2004;38:680–5. doi: 10.1097/01.mcg.0000135929.78074.8c. [DOI] [PubMed] [Google Scholar]
- 4.Wald A. Chronic constipation: Advances in management. Neurogastroenterol Motil. 2007;19:4–10. doi: 10.1111/j.1365-2982.2006.00835.x. [DOI] [PubMed] [Google Scholar]
- 5.Choung RS, Locke GR, 3rd, Rey E, Schleck CD, Baum C, Zinsmeister AR, et al. Factors associated with persistent and nonpersistent chronic constipation, over 20 years. Clin Gastroenterol Hepatol. 2012;10:494–500. doi: 10.1016/j.cgh.2011.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tack J, Müller-Lissner S, Stanghellini V, Boeckxstaens G, Kamm MA, Simren M, et al. Diagnosis and treatment of chronic constipation — a European perspective. Neurogastroenterol Motil. 2011;23:697–710. doi: 10.1111/j.1365-2982.2011.01709.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao SS, Mudipalli RS, Stessman M, Zimmerman B. Investigation of the utility of colorectal function tests and Rome II criteria in dyssynergic defecation (Anismus) Neurogastroenterol Motil. 2004;16:589–96. doi: 10.1111/j.1365-2982.2004.00526.x. [DOI] [PubMed] [Google Scholar]
- 8.Rao SS, Valestin J, Brown CK, Zimmerman B, Schulze K. Long-term efficacy of biofeedback therapy for dyssynergic defecation: Randomized controlled trial. Am J Gastroenterol. 2010;105:890–6. doi: 10.1038/ajg.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiarioni G, Heymen S, Whitehead WE. Biofeedback therapy for dyssynergic defecation. World J Gastroenterol. 2006;12:7069–74. doi: 10.3748/wjg.v12.i44.7069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patcharatrakul T, Gonlachanvit S. Outcome of biofeedback therapy in dyssynergic defecation patients with and without irritable bowel syndrome. J Clin Gastroenterol. 2011;45:593–8. doi: 10.1097/MCG.0b013e31820c6001. [DOI] [PubMed] [Google Scholar]
- 11.Gonlachanvit S, Patcharatrakul T. Causes of idiopathic constipation in Thai patients: Associations between the causes and constipation symptoms as defined in the Rome II criteria. J Med Assoc Thai. 2004;87(Suppl 2):S22–8. [PubMed] [Google Scholar]
- 12.Simón MA, Bueno AM. Behavioural treatment of the dyssynergic defecation in chronically constipated elderly patients: A randomized controlled trial. Appl Psychophysiol Biofeedback. 2009;34:273–7. doi: 10.1007/s10484-009-9100-7. [DOI] [PubMed] [Google Scholar]
- 13.Sagae UE, Lima DM, Alves KR, Kurachi G, Tanaka TM, Bonatto MW, et al. Effectiveness of biofeedback therapy in patients with chronic constipation. J Coloproctol (Rio de Janeiro) 2012;32:65–71. [Google Scholar]
- 14.Heymen S, Jones KR, Scarlett Y, Whitehead WE. Biofeedback treatment of constipation: A critical review. Dis Colon Rectum. 2003;46:1208–17. doi: 10.1007/s10350-004-6717-8. [DOI] [PubMed] [Google Scholar]
- 15.Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with pelvic floor dyssynergia-type constipation. Dis Colon Rectum. 2007;50:428–41. doi: 10.1007/s10350-006-0814-9. [DOI] [PubMed] [Google Scholar]
- 16.Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130:657–64. doi: 10.1053/j.gastro.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 17.Clouse RE, Mayer EA, Aziz Q, Drossman DA, Dumitrascu DL, Mönnikes H, et al. Functional abdominal pain syndrome. Gastroenterology. 2006;130:1492–7. doi: 10.1053/j.gastro.2005.11.062. [DOI] [PubMed] [Google Scholar]
- 18.Rao SS. Constipation: Evaluation and treatment of colonic and anorectal motility disorders. Gastrointest Endosc Clin N Am. 2009;19:117–39. doi: 10.1016/j.giec.2008.12.006. vii. [DOI] [PubMed] [Google Scholar]
- 19.Bharucha AE, Wald A, Enck P, Rao S. Functional anorectal disorders. Gastroenterology. 2006;130:1510–8. doi: 10.1053/j.gastro.2005.11.064. [DOI] [PubMed] [Google Scholar]
- 20.Friedman LM, Furberg CD, DeMets DL. New York: Springer; 2010. Fundamentals of Clinical Trials. [Google Scholar]
- 21.Chiarioni G, Salandini L, Whitehead WE. Biofeedback benefits only patients with outlet dysfunction, not patients with isolated slow transit constipation. Gastroenterology. 2005;129:86–97. doi: 10.1053/j.gastro.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 22.Wang J, Luo MH, Qi QH, Dong ZL. Prospective study of biofeedback retraining in patients with chronic idiopathic functional constipation. World J Gastroenterol. 2003;9:2109–13. doi: 10.3748/wjg.v9.i9.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Camilleri M, Bharucha AE. Behavioural and new pharmacological treatments for constipation: Getting the balance right. Gut. 2010;59:1288–96. doi: 10.1136/gut.2009.199653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hak NG, El-Hemaly M, El-Nakeeb A, Salah T, Hamdy E, El-Hanafy E, et al. Outcome & predictors of success of biofeedback for patients with spastic pelvic floor syndrome. Egypt J Surg. 2012;31:148–54. [Google Scholar]
- 25.Faried M, El Nakeeb A, Youssef M, Omar W, El Monem HA. Comparative study between surgical and non-surgical treatment of anismus in patients with symptoms of obstructed defecation: A prospective randomized study. J Gastrointest Surg. 2010;14:1235–43. doi: 10.1007/s11605-010-1229-4. [DOI] [PubMed] [Google Scholar]
- 26.Landmann RG, Wexner SD. Paradoxical puborectalis contraction and increased perineal descent. Clin Colon Rectal Surg. 2008;21:138–45. doi: 10.1055/s-2008-1075863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Jong TP, Klijn AJ, Vijverberg MA, de Kort LM, van Empelen R, Schoenmakers MA. Effect of biofeedback training on paradoxical pelvic floor movement in children with dysfunctional voiding. Urology. 2007;70:790–3. doi: 10.1016/j.urology.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Whitehead WE, Bharucha AE. Diagnosis and treatment of pelvic floor disorders: What's new and what to do. Gastroenterology. 2010;138:1231–5.e1. doi: 10.1053/j.gastro.2010.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]


