Abstract
Background:
Childhood obesity is a global health problem with short- and long-term health consequences. This systematic review presents a summary of the experiences on different family-, school-, and clinic-based interventions.
Materials and Methods:
Electronic search was conducted in MEDLINE, PubMed, ISI Web of Science, and Scopus scientific databases. We included those studies conducted among obese individuals aged up to 18 years. Our search yielded 105 relevant papers, 70 of them were conducted as high quality clinical trials.
Results:
Our findings propose that school-based programs can have long-term effects in a large target group. This can be related to this fact that children spend a considerable part of their time in school, and adopt some parts of lifestyle there. They have remarkable consequences on health behaviors, but as there are some common limitations, their effects on anthropometric measures are not clear. Due to the crucial role of parents in development of children's behaviors, family-based interventions are reported to have successful effects in some aspects; but selection bias and high dropout rate can confound their results. Clinic-based interventions revealed favorable effects. They include dietary or other lifestyle changes like increasing physical activity or behavior therapy. It seems that a comprehensive intervention including diet and exercise are more practical. When they have different designs, results are controversial.
Conclusion:
We suggest that among different types of interventional programs, a multidisciplinary approach in schools in which children's family are involved, can be the best and most sustainable approach for management of childhood obesity.
Keywords: Adolescent, child, control, obesity, prevention
INTRODUCTION
The epidemic of childhood obesity is no more limited to high-income countries,[1,2,3,4,5,6,7,8] and has become as one of the most important global health problems of the 21th century.[9] The World Health Organization (WHO) experts have estimated that there are 43 million overweight children under the age of 5 and by 2020 more than 60% of global disease burden will be the result of obesity related disorders.[2,10] Childhood obesity is associated with several short term and long-term health hazards as cardiovascular diseases, hypertension, type 2 diabetes, fatty liver disease, orthopedic problems, low self-esteem, etc.[11,12] Childhood obesity can reduce life expectancy by 2-5 years.[2] Moreover, the increasing trend of obesity has enormous economic outcomes.[13] Two main underlying causes of excess weight are genes and environment.[14,15] Although both genes and environment have a role in an obesity epidemic, gene defects needs to time to show their phenotype; so obesogenic environment is responsible for obesity.[11]
Primordial/primary prevention of pediatrics obesity and establishment of a healthy lifestyle behaviors from early life are the favored against the epidemic of obesity at the global level.[16]
Effective interventions for prevention and control of childhood obesity should be considered for different aspects.[11,17,18,19,20,21,22,23,24] Experts recommend specific eating and physical activity (PA) behaviors through counseling.[14] Along with clinic-based interventions, researchers have attempted to manage obesity by virtue of family, community, school, and after school programs. Based on Cochrane review of obesity prevention programs in children, most of the well-designed interventions had positive results especially in 6-12-year-old children.[25] Clearly targeted interventions for children and population-based approach for adolescents may be useful and make economic sense. The purpose of this investigation was to systematically review the effects of various clinical-, family-, and community-based interventions targeting the control of childhood obesity and make a suggestion for future interventions.
MATERIALS AND METHODS
Literature search
Relevant literature reporting the interventions for controlling excess weight in children and adolescents was identified through electronic search of papers published from 2000 to 2012 in MEDLINE, PubMed, ISI Web of Science, and Scopus. Keywords such as “childhood obesity”, “overweight,” “weight disorder,” “intervention,” “treatment,” “management,” “control,” “PA,” “nutrition,” “behavior therapy,” and “diet therapy” were used. The searches yielded 1768 articles.
Study selection and eligibility criteria
Having removed duplicates, the relevant papers were selected in three phases. In the first and second phases, titles and abstracts of papers were screened and irrelevant papers were excluded. In the last phase, the full text of recruited papers was explored deeply to select only relevant papers. All these three screening phases were done by two independent reviewers (RK and FA). Discrepancies were resolved by consultation and consensus.
Studies were included if they met the following criteria: Studies on 2-18-year-old children; community, family, school, and clinic interventions or a combination of them; English language; and conducted among obese or overweight children and adolescents. Systematic reviews, meta-analysis, and editorials were excluded. Articles were firstly assessed on their abstracts and 234 were removed.
Data extraction and abstraction
The required information that was extracted from all eligible papers was as follow:
-
(i)
General characteristics of the study (first author's name, publication year, study year, study design, sampling method,
-
(ii)
Characteristics of the study population (age and sex of studied participants and sample size, follow-up),
-
(iii)
Type and duration of the intervention, measure(s) used to assess child weight, and
-
(iv)
Main finding. One reviewer (FA) extracted the data while another (RK) randomly selected 10% of them and checked their extracted data.
The selection process of our systematic review is presented in Figure 1.
Figure 1.
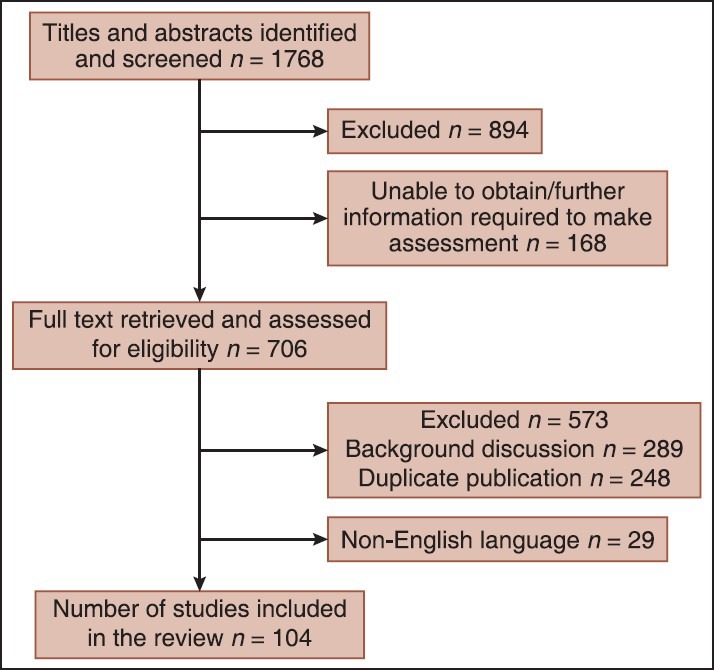
Flow chart of study selection process
RESULTS
The interventions were categorized as school-based, family-based, and clinic-based programs as described below:
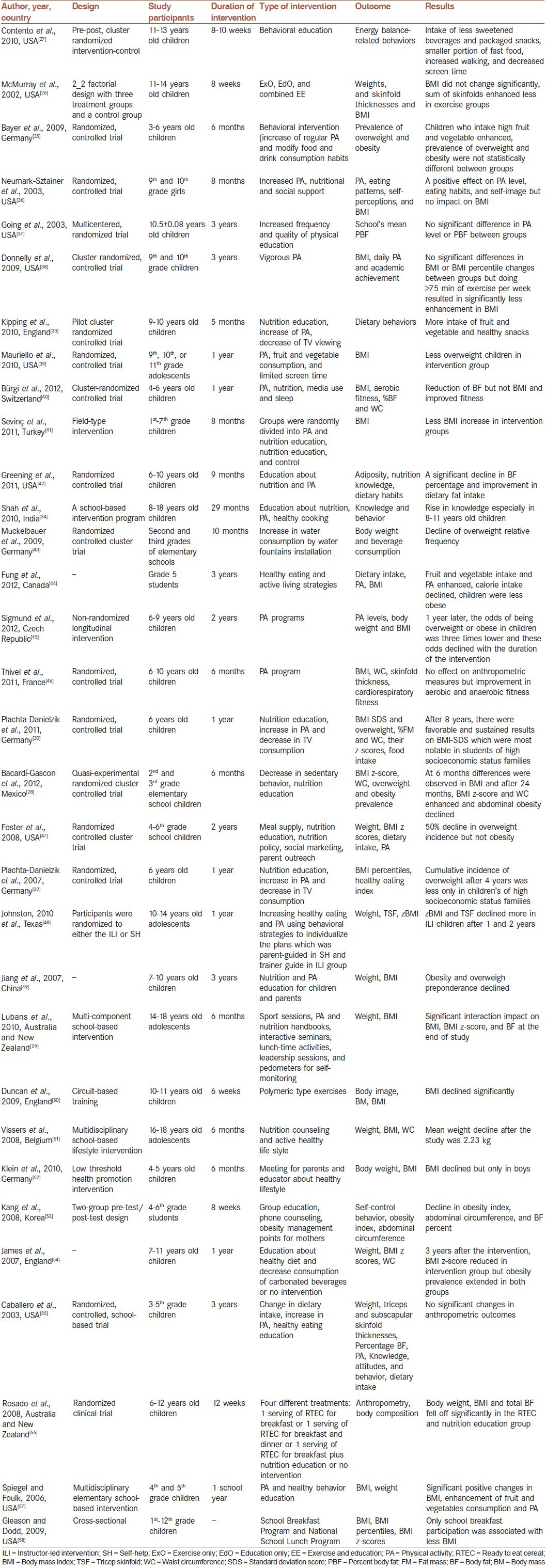
School-based programs
A summary of the school-based obesity prevention and control programs is presented in Table 1. In brief, such interventions are suggested to be feasible and effective;[26] because students spend a considerable part of their time in school,[27] moreover teachers and peers can be engaged in such programs.[28] These kinds of programs can improve health behaviors in a large target group. They are characterized by nutritional education and changes in dietary habits, as well as increase in PA through structured programs.[29] Findings of various studies proposed that the effects of such interventions will be preserved for several years after intervention.[30,31,32] This effect has been of special concern about consuming fruits and vegetables, and healthy snacks, as well as increased PA. Nevertheless, the impact of school-based programs on obesity prevention is controversial and remains to be determined by large studies with long-term follow-up research. Some studies have not evaluated the effect of intervention on anthropometric measures,[27,33,34] but they have shown positive impacts on eating and activity behaviors. The most common limitation of these studies is presenting self-reported data, non-randomized selection of schools, short duration of study, and not masking the interventional groups.
Table 1.
School-based weight control studies
Family-based programs
Reaching a healthy weight is not successful unless children have support for making healthy behavior choices; obviously, providers of this support are families. Family is an applicable target for health promoting interventions. Family-based intervention programs are considered as one of the most successful methods for obesity treatment or prevention.[59] Engaging parents in childhood obesity prevention programs may make weight loss easier for children; because they can provide confirmatory conditions to help their children to choose healthy behaviors, furthermore they are important role models for their children.[60] It is difficult for parents to know and accept that their child has excess weight, and that recommended diets would not have adverse health effect for their children;[61] therefore, they often do not comprehend the necessity of obesity prevention. Families are able to construct children's lifestyle habits, perhaps through their “parenting style” and management of “family functioning.”[62] Table 2 shows family-based interventions for management of childhood obesity. As it demonstrates, most of these programs were successful in decreasing body mass index (BMI) z-score and some health consequences of overweight. After participation of parents in these kinds of programs, their children consumed more fiber and were less sedentary. In some cases, significant decrease in fat mass is documented, as well.[63,64] It has shown that low parental confidence predicts dropout rate from family-based behavioral treatment.[65] The main limitation of family-based studies is the small sample size, high dropout rate, no follow-up data, and selection of motivated families.
Table 2.
Family-based studies for controlling childhood obesity

Clinic-based programs
Table 3 presents a summary of clinic-based weight management programs conducted in the pediatric age group. Although most researchers have tried low calorie-low fat diets for treating obesity, experts have recommended to consider a diet with balanced macronutrients.[14] Nevertheless, different dietary changes have been tried to control excess weight in children and adolescents. High protein (HP) diets seems to make more satiety, but two studies did not confirm their advantage versus standard diets.[90,91]
Table 3.
Clinic-based weight control studies for children and adolescents
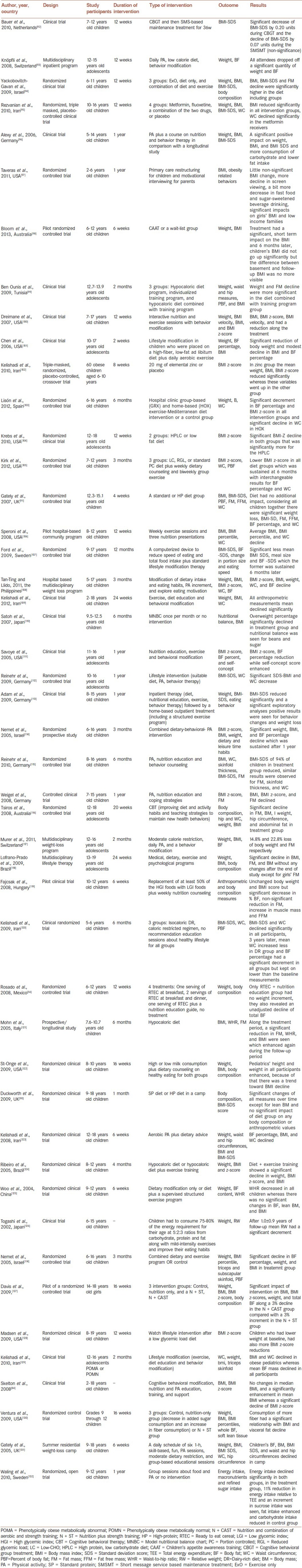
In studies in which diet, exercise or both of them were taken into account, nutrition plus PA had more effect on anthropometric indices.[99,103,124] One study showed that combination of aerobic and strength training along with diet therapy results in BMI decrease in comparison with strength training plus diet recommendation.[127] A successful experience is reported about the favorable effects of zinc supplementation on anthropometric and metabolic indices.[102,133]
Obesity behavioral therapy has different parts such as motivational interviewing, goal setting, positive reinforcement, monitoring, and cognitive restructuring.[134] Most of behavioral therapies had positive consequences on weight, BMI, or dietary and PA habits.[92,98,107,108,116]
All interventions that consisted of nutrition, exercise, and counseling had significant effects on body weight or other obesity-related factors[84,93,96,100,101,105,109,111,112,113,114,115,117,118,120,128,135] except for a study, which had beneficial effects only on obesity related behaviors.[97] The main limitation of some of these studies is lack of comparison with the control group, and short-term follow-up of participants, and the uncertain sustainability of such kinds of interventions.
DISCUSSION
This review evaluated three different approaches in childhood obesity management. As the design of most studies is a clinical trial, it makes their comparison easier. Schools are a safe place for learning healthy skills and continuing them during life. Most (29/32) of the papers reported a positive effect of school-based intervention on dietary habits or anthropometric measures. One of negative effects of this kind intervention is discrimination resulted from stigmatization. This may persuade them to get involved in healthier lifestyle or might have opposite results. All of the studies conducted in the family setting (n = 26), had favorable results on obesity criteria. Although some of them had negligible effects. Clinic-based intervention had different methods but almost the same results.
Some studies had no effects on anthropometric index. However, they had resulted in dietary habits or physical fitness improvement.[35,36,46,55,72,97,78,132] One explanation for this can be self-reported dietary intake and PA data. On the other words, children may not pay attention to the instruction they were given.
Teachers can train students how to choose nutritious and low-calorie foods. In addition, exercise training can be reinforced in the school curriculum.[14] Most students with excess weight prefer to eat fatty, sweetened, and salty snacks; they also choose fast foods as their first meal preference. If attendants get involved in obesity prevention programs, they can provide an environment for children to purchase healthy snacks and foods. Families can also make a circumstance which facilitates dietary and behavioral changes. Furthermore, if parents recognize the importance of weight control, they will be motivated to persuade their children for weight control. Families, especially mothers, are the best paradigm for children to learn a healthful eating pattern and activity habits.[136] Through family meals, children can eat more whole grains, fruits, vegetables, low fat milk, and consume less sweets and unhealthy fats. Parents should involve kids in preparing food to make a positive effect on their attitudes toward obesity prevention. It seems that the family has a key role in long-term weight control.[71] It has been shown that if family confidence is low, rate of dropout from weight loss programs will increase.[65] In this regard, providing parenting styles and skills as well as child management strategies are really critical.[81,137] Principally clinic-setting programs have brought nutrition, PA, and education or counseling together to achieve their goals and they have demonstrated long lasting results.[138] Most experts advise a low calorie low fat diet for obesity management; but they may have side-effects such as binge eating.[139] Actually weight loss is allowed in severe obesity and in other cases weight maintenance is an appropriate policy.[114] Some studies recommend HP or low carbohydrate diets because they cause more satiety.[140] A review article revealed that low carbohydrate ad libitum diets are as effective as calorie restricted diets.[140] In addition, a Cochrane review showed that low fat diets have no extra advantages in comparison with other diets with calorie restriction.[141] Another review article revealed moderate effect of exercise on adiposity and not on BMI.[142] Clearly, PA is efficient when lasts for more than 60 min, is moderate to vigorous, and is done in all weekdays.[134] As low calorie diets are harmful for growth, and complying with them is difficult, some studies suggested that vigorous exercise can be a suitable substitute for diet therapy.[137,139] As always emphasized, to be effective, PA should be considered as an enjoyable fun, and should be integrated into daily lifestyle. Obesity causes mental problems in children and adolescents,[118] so behavior therapy seems to be vital. It sounds that group treatment is more successful than individual ones;[75,79] specifically when parents are engaged. Counselors should persuade children and adolescents to eat breakfast, to have structured meal plan to increase consumption of fruits, vegetables, and family meals, as well as to decrease the intake of sweetened beverages, calorie-dense foods, and eating out, as well as reducing the sedentary behaviors and the screen time.[14,91] Counselors also need to teach families about healthy shopping and cooking habits. Unfortunately, most studies did not show favorable effects, many of them had small sample sizes or had short-term follow-up or lacked of the control group. Managing extra group support sessions or using technologies such as E-mail or SMS for monitoring weight losers can be a good idea.[63,92,143]
CONCLUSION
The findings suggest that among different types of interventional programs for management of childhood obesity, a multidisciplinary approach in schools in which children's family are involved, can be the most feasible and effective approach. As teachers and parents are the best role models, it will be easier to accustom children with healthy dietary, PA, and behavioral habits. Future studies are needed to determine the long-term effects and sustainability of different programs.
AUTHORS’ CONTRIBUTION
FAS contributed in the conception of the work, conducting the review, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. RK contributed in the conception and design of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Cheng TO. Childhood obesity in modern China. Int J Cardiol. 2012;157:315–7. doi: 10.1016/j.ijcard.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Bereket A, Atay Z. Current status of childhood obesity and its associated morbidities in Turkey. J Clin Res Pediatr Endocrinol. 2012;4:1–7. doi: 10.4274/jcrpe.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bac A, WoŸniacka R, Matusik S, Golec J, Golec E. Prevalence of overweight and obesity in children aged 6-13 years-alarming increase in obesity in Cracow, Poland. Eur J Pediatr. 2012;171:245–51. doi: 10.1007/s00431-011-1519-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El Mouzan MI, Al Herbish AS, Al Salloum AA, Al Omar AA, Qurachi MM. Regional variation in prevalence of overweight and obesity in Saudi children and adolescents. Saudi J Gastroenterol. 2012;18:129–32. doi: 10.4103/1319-3767.93818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang M, Guo F, Tu Y, Kiess W, Sun C, Li X, et al. Further increase of obesity prevalence in Chinese children and adolescents — Cross-sectional data of two consecutive samples from the city of Shanghai from 2003 to 2008. Pediatr Diabetes. 2012;13:572–7. doi: 10.1111/j.1399-5448.2012.00877.x. [DOI] [PubMed] [Google Scholar]
- 6.Midha T, Nath B, Kumari R, Rao YK, Pandey U. Childhood obesity in India: A meta-analysis. Indian J Pediatr. 2012;79:945–8. doi: 10.1007/s12098-011-0587-6. [DOI] [PubMed] [Google Scholar]
- 7.Mushtaq MU, Gull S, Abdullah HM, Shahid U, Shad MA, Akram J. Prevalence and socioeconomic correlates of overweight and obesity among Pakistani primary school children. BMC Public Health. 2011;11:724. doi: 10.1186/1471-2458-11-724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jelastopulu E, Kallianezos P, Merekoulias G, Alexopoulos EC, Sapountzi-Krepia D. Prevalence and risk factors of excess weight in school children in West Greece. Nurs Health Sci. 2012;14:372–80. doi: 10.1111/j.1442-2018.2012.00691.x. [DOI] [PubMed] [Google Scholar]
- 9.John J, Wolfenstetter SB, Wenig CM. An economic perspective on childhood obesity: Recent findings on cost of illness and cost effectiveness of interventions. Nutrition. 2012;28:829–39. doi: 10.1016/j.nut.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Bruney TS. Childhood obesity: Effects of micronutrients, supplements, genetics, and oxidative stress. J Nurse Pract. 2011;7:647–53. [Google Scholar]
- 11.Procter KL. The aetiology of childhood obesity: A review. Nutr Res Rev. 2007;20:29–45. doi: 10.1017/S0954422407746991. [DOI] [PubMed] [Google Scholar]
- 12.Marcus MD, Levine MD, Kalarchian MA, Wisniewski L. Cognitive behavioral interventions in the management of severe pediatric obesity. Cogn Behav Pract. 2003;10:147–56. [Google Scholar]
- 13.Kral JG, Kava RA, Catalano PM, Moore BJ. Severe Obesity: The Neglected Epidemic. Obes Facts. 2012;5:254–69. doi: 10.1159/000338566. [DOI] [PubMed] [Google Scholar]
- 14.Barlow SE, Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 15.Karnik S, Kanekar A. Childhood obesity: A global public health crisis. Int J Prev Med. 2012;3:1–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Lytle LA. Dealing with the childhood obesity epidemic: A public health approach. Abdom Imaging. 2012;37:719–24. doi: 10.1007/s00261-012-9861-y. [DOI] [PubMed] [Google Scholar]
- 17.Knowlden AP, Sharma M. Systematic review of family and home-based interventions targeting paediatric overweight and obesity. Obes Rev. 2012;13:499–508. doi: 10.1111/j.1467-789X.2011.00976.x. [DOI] [PubMed] [Google Scholar]
- 18.Tounian P. Programming towards childhood obesity. Ann Nutr Metab. 2011;58(Suppl 2):30–41. doi: 10.1159/000328038. [DOI] [PubMed] [Google Scholar]
- 19.Higgins V, Dale A. Ethnicity and childhood overweight/obesity in England. Pediatr Obes. 2012;7:E22–6. doi: 10.1111/j.2047-6310.2012.00051.x. [DOI] [PubMed] [Google Scholar]
- 20.D’Auria JP. Weighing in: Prevention of childhood overweight and obesity. J Pediatr Health Care. 2011;25:E26–30. doi: 10.1016/j.pedhc.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Haynos AF, O’Donohue WT. Universal childhood and adolescent obesity prevention programs: Review and critical analysis. Clin Psychol Rev. 2012;32:383–99. doi: 10.1016/j.cpr.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Roy M, Millimet DL, Tchernis R. Federal nutrition programs and childhood obesity: Inside the black box. Rev Econ Househ. 2012;10:1–38. [Google Scholar]
- 23.Huus K, Ludvigsson JF, Enskär K, Ludvigsson J. Risk factors in childhood obesity-findings from the All Babies In Southeast Sweden (ABIS) cohort. Acta Paediatr. 2007;96:1321–5. doi: 10.1111/j.1651-2227.2007.00408.x. [DOI] [PubMed] [Google Scholar]
- 24.Pelone F, Specchia ML, Veneziano MA, Capizzi S, Bucci S, Mancuso A, et al. Economic impact of childhood obesity on health systems: A systematic review. Obes Rev. 2012;13:431–40. doi: 10.1111/j.1467-789X.2011.00968.x. [DOI] [PubMed] [Google Scholar]
- 25.Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;20:CD001871. doi: 10.1002/14651858.CD001871.pub2. [DOI] [PubMed] [Google Scholar]
- 26.Mcmurray RG, Harrell JS, Bangdiwala SI, Bradley CB, Deng S, Levine A. A school-based intervention can reduce body fat and blood pressure in young adolescents. J Adolesc Health. 2002;31:125–32. doi: 10.1016/s1054-139x(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 27.Contento IR, Koch PA, Lee H, Calabrese-Barton A. Adolescents demonstrate improvement in obesity risk behaviors after completion of choice, control & change, a curriculum addressing personal agency and autonomous motivation. J Am Diet Assoc. 2010;110:1830–9. doi: 10.1016/j.jada.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bacardí-Gascon M, Pérez-Morales ME, Jiménez-Cruz A. A six month randomized school intervention and an 18-month follow-up intervention to prevent childhood obesity in Mexican elementary schools. Nutr Hosp. 2012;27:755–62. doi: 10.3305/nh.2012.27.3.5756. [DOI] [PubMed] [Google Scholar]
- 29.Lubans DR, Morgan PJ, Callister R, Collins CE, Plotnikoff RC. Exploring the mechanisms of physical activity and dietary behavior change in the program x intervention for adolescents. J Adolesc Health. 2010;47:83–91. doi: 10.1016/j.jadohealth.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 30.Plachta-Danielzik S, Landsberg B, Lange D, Seiberl J, Müller MJ. Eight-year follow-up of school-based intervention on childhood overweight – The Kiel Obesity Prevention Study. Obes Facts. 2011;4:35–43. doi: 10.1159/000324552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muckelbauer R, Libuda L, Clausen K, Reinehr T, Kersting M. A simple dietary intervention in the school setting decreased incidence of overweight in children. Obes Facts. 2009;2:282–5. doi: 10.1159/000229783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Plachta-Danielzik S, Pust S, Asbeck I, Czerwinski-Mast M, Langnäse K, Fischer C, et al. Four-year follow-up of school-based intervention on overweight children: The KOPS study. Obesity (Silver Spring) 2007;15:3159–69. doi: 10.1038/oby.2007.376. [DOI] [PubMed] [Google Scholar]
- 33.Kipping RR, Jago R, Lawlor DA. Diet outcomes of a pilot school-based randomised controlled obesity prevention study with 9-10 year olds in England. Prev Med. 2010;51:56–62. doi: 10.1016/j.ypmed.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 34.Shah P, Misra A, Gupta N, Hazra DK, Gupta R, Seth P, et al. Improvement in nutrition-related knowledge and behaviour of urban Asian Indian school children: Findings from the ’Medical education for children/Adolescents for Realistic prevention of obesity and diabetes and for healthy aGeing’ ( MARG) intervention study. Br J Nutr. 2010;104:427–36. doi: 10.1017/S0007114510000681. [DOI] [PubMed] [Google Scholar]
- 35.Bayer O, von Kries R, Strauss A, Mitschek C, Toschke AM, Hose A, et al. Short- and mid-term effects of a setting based prevention program to reduce obesity risk factors in children: A cluster-randomized trial. Clin Nutr. 2009;28:122–8. doi: 10.1016/j.clnu.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 36.Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New Moves: A school-based obesity prevention program for adolescent girls. Prev Med. 2003;37:41–51. doi: 10.1016/s0091-7435(03)00057-4. [DOI] [PubMed] [Google Scholar]
- 37.Going S, Thompson J, Cano S, Stewart D, Stone E, Harnack L, et al. The effects of the Pathways Obesity Prevention Program on physical activity in American Indian children. Prev Med. 2003;37:S62–9. doi: 10.1016/j.ypmed.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 38.Donnelly JE, Greene JL, Gibson CA, Smith BK, Washburn RA, Sullivan DK, et al. Physical activity across the curriculum (PAAC): A randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev Med. 2009;49:336–41. doi: 10.1016/j.ypmed.2009.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mauriello LM, Ciavatta MM, Paiva AL, Sherman KJ, Castle PH, Johnson JL, et al. Results of a multi-media multiple behavior obesity prevention program for adolescents. Prev Med. 2010;51:451–6. doi: 10.1016/j.ypmed.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bürgi F, Niederer I, Schindler C, Bodenmann P, Marques-Vidal P, Kriemler S, et al. Effect of a lifestyle intervention on adiposity and fitness in socially disadvantaged subgroups of preschoolers: A cluster-randomized trial (Ballabeina) Prev Med. 2012;54:335–40. doi: 10.1016/j.ypmed.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 41.Sevinç Ö, Bozkurt A, Gündoğdu M, Aslan Übaş, Ağbuğa B, Aslan Þ, et al. Evaluation of the effectiveness of an intervention program on preventing childhood obesity in Denizli, Turkey. Turk J Med Sci. 2011;41:1097–105. [Google Scholar]
- 42.Greening L, Harrell KT, Low AK, Fielder CE. Efficacy of a school-based childhood obesity intervention program in a rural southern community: TEAM Mississippi Project. Obesity (Silver Spring) 2011;19:1213–9. doi: 10.1038/oby.2010.329. [DOI] [PubMed] [Google Scholar]
- 43.Muckelbauer R, Libuda L, Clausen K, Kersting M. Long-term process evaluation of a school-based programme for overweight prevention. Child Care Health Dev. 2009;35:851–7. doi: 10.1111/j.1365-2214.2009.00993.x. [DOI] [PubMed] [Google Scholar]
- 44.Fung C, Kuhle S, Lu C, Purcell M, Schwartz M, Storey K, et al. From "best practice" to "next practice": The effectiveness of school-based health promotion in improving healthy eating and physical activity and preventing childhood obesity. Int J Behav Nutr Phys Act. 2012;9:27. doi: 10.1186/1479-5868-9-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sigmund E, El Ansari W, Sigmundová D. Does school-based physical activity decrease overweight and obesity in children aged 6-9 years? A two-year non-randomized longitudinal intervention study in the Czech Republic. BMC Public Health. 2012;12:570. doi: 10.1186/1471-2458-12-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Thivel D, Isacco L, Lazaar N, Aucouturier J, Ratel S, Doré E, et al. Effect of a 6-month school-based physical activity program on body composition and physical fitness in lean and obese schoolchildren. Eur J Pediatr. 2011;170:1435–43. doi: 10.1007/s00431-011-1466-x. [DOI] [PubMed] [Google Scholar]
- 47.Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121:e794–802. doi: 10.1542/peds.2007-1365. [DOI] [PubMed] [Google Scholar]
- 48.Johnston CA, Tyler C, Fullerton G, McFarlin BK, Poston WS, Haddock CK, et al. Effects of a school-based weight maintenance program for Mexican-American children: Results at 2 years. Obesity (Silver Spring) 2010;18:542–7. doi: 10.1038/oby.2009.241. [DOI] [PubMed] [Google Scholar]
- 49.Jiang J, Xia X, Greiner T, Wu G, Lian G, Rosenqvist U. The effects of a 3-year obesity intervention in schoolchildren in Beijing. Child Care Health Dev. 2007;33:641–6. doi: 10.1111/j.1365-2214.2007.00738.x. [DOI] [PubMed] [Google Scholar]
- 50.Duncan MJ, Al-Nakeeb Y, Nevill AM. Effects of a 6-week circuit training intervention on body esteem and body mass index in British primary school children. Body Image. 2009;6:216–20. doi: 10.1016/j.bodyim.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 51.Vissers D, De Meulenaere A, Vanroy C, Vanherle K, Van de Sompel A, Truijen S, et al. Effect of a multidisciplinary school-based lifestyle intervention on body weight and metabolic variables in overweight and obese youth. e-SPEN. Eur e-J Clin Nutr Metab. 2008;3:e196–202. [Google Scholar]
- 52.Klein D, De Toia D, Weber S, Wessely N, Koch B, Dordel S, et al. Effects of a low threshold health promotion intervention on the BMI in pre-school children under consideration of parental participation. e-SPEN. Eur e-J Clini Nutr Metab. 2010;5:e125–31. [Google Scholar]
- 53.Kang HS, Ryu MH, Park S. The effects of a weight loss program focusing on maternal education on childhood obesity. Asian Nurs Res. 2008;2:150–8. doi: 10.1016/S1976-1317(08)60038-9. [DOI] [PubMed] [Google Scholar]
- 54.James J, Thomas P, Kerr D. Preventing childhood obesity: Two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS) BMJ. 2007;335:762. doi: 10.1136/bmj.39342.571806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: A school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rosado JL, del R Arellano M, Montemayor K, García OP, Caamaño Mdel C. An increase of cereal intake as an approach to weight reduction in children is effective only when accompanied by nutrition education: A randomized controlled trial. Nutr J. 2008;7:28. doi: 10.1186/1475-2891-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Spiegel SA, Foulk D. Reducing overweight through a multidisciplinary school-based intervention. Obesity (Silver Spring) 2006;14:88–96. doi: 10.1038/oby.2006.11. [DOI] [PubMed] [Google Scholar]
- 58.Gleason PM, Dodd AH. School breakfast program but not school lunch program participation is associated with lower body mass index. J Am Diet Assoc. 2009;109:S118–28. doi: 10.1016/j.jada.2008.10.058. [DOI] [PubMed] [Google Scholar]
- 59.Gruber KJ, Haldeman LA. Using the family to combat childhood and adult obesity. Prev Chronic Dis. 2009;6:A106. [PMC free article] [PubMed] [Google Scholar]
- 60.Ball GD, Ambler KA, Keaschuk RA, Rosychuk RJ, Holt NL, Spence JC, et al. Parents as agents of change (PAC) in pediatric weight management: The protocol for the PAC randomized clinical trial. BMC Pediatr. 2012;12:114. doi: 10.1186/1471-2431-12-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Warschburger P, Kröller K. “Childhood overweight and obesity: Maternal perceptions of the time for engaging in child weight management”. BMC Public Health. 2012;12:295. doi: 10.1186/1471-2458-12-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wen LM, Simpson JM, Baur LA, Rissel C, Flood VM. Family functioning and obesity risk behaviors: Implications for early obesity intervention. Obesity (Silver Spring) 2011;19:1252–8. doi: 10.1038/oby.2010.285. [DOI] [PubMed] [Google Scholar]
- 63.Kalavainen M, Utriainen P, Vanninen E, Korppi M, Nuutinen O. Impact of childhood obesity treatment on body composition and metabolic profile. World J Pediatr. 2012;8:31–7. doi: 10.1007/s12519-011-0324-2. [DOI] [PubMed] [Google Scholar]
- 64.Savoye M, Nowicka P, Shaw M, Yu S, Dziura J, Chavent G, et al. Long-term results of an obesity program in an ethnically diverse pediatric population. Pediatrics. 2011;127:402–10. doi: 10.1542/peds.2010-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gunnarsdottir T, Njardvik U, Olafsdottir AS, Craighead LW, Bjarnason R. The role of parental motivation in family-based treatment for childhood obesity. Obesity (Silver Spring) 2011;19:1654–62. doi: 10.1038/oby.2011.59. [DOI] [PubMed] [Google Scholar]
- 66.Danielsen YS, Nordhus IH, Júlíusson PB, Mæhle M, Pallesen S. Effect of a family-based cognitive behavioural intervention on body mass index, self-esteem and symptoms of depression in children with obesity (aged 7-13): A randomised waiting list controlled trial. Obes Res Clin Pract. 2013;7:e116–28. doi: 10.1016/j.orcp.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 67.West F, Sanders MR, Cleghorn GJ, Davies PS. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav Res Ther. 2010;48:1170–9. doi: 10.1016/j.brat.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 68.Vos RC, Huisman SD, Houdijk EC, Pijl H, Wit JM. The effect of family-based multidisciplinary cognitive behavioral treatment on health-related quality of life in childhood obesity. Qual Life Res. 2012;21:1587–94. doi: 10.1007/s11136-011-0079-1. [DOI] [PubMed] [Google Scholar]
- 69.Sacher PM, Kolotourou M, Chadwick PM, Cole TJ, Lawson MS, Lucas A, et al. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity (Silver Spring) 2010;18(Suppl 1):S62–8. doi: 10.1038/oby.2009.433. [DOI] [PubMed] [Google Scholar]
- 70.Teder M, Mörelius E, Bolme P, Nordwall M, Ekberg J, Timpka T. Family-based behavioural intervention programme for obese children: A feasibility study. BMJ Open. 2012;2:e000268. doi: 10.1136/bmjopen-2011-000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Edwards C, Nicholls D, Croker H, Van Zyl S, Viner R, Wardle J. Family-based behavioural treatment of obesity: Acceptability and effectiveness in the UK. Eur J Clin Nutr. 2006;60:587–92. doi: 10.1038/sj.ejcn.1602353. [DOI] [PubMed] [Google Scholar]
- 72.Bean MK, Wilson DB, Thornton LM, Kelly N, Mazzeo SE. Dietary intake in a randomized-controlled pilot of NOURISH: A parent intervention for overweight children. Prev Med. 2012;55:224–7. doi: 10.1016/j.ypmed.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gunnarsdottir T, Njardvik U, Olafsdottir AS, Craighead L, Bjarnason R. Childhood obesity and co-morbid problems: Effects of Epstein's family-based behavioural treatment in an Icelandic sample. J Eval Clin Pract. 2012;18:465–72. doi: 10.1111/j.1365-2753.2010.01603.x. [DOI] [PubMed] [Google Scholar]
- 74.Melin A, Lenner RA. Prevention of further weight gain in overweight school children, a pilot study. Scand J Caring Sci. 2009;23:498–505. doi: 10.1111/j.1471-6712.2008.00651.x. [DOI] [PubMed] [Google Scholar]
- 75.Kalavainen MP, Korppi MO, Nuutinen OM. Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. Int J Obes (Lond) 2007;31:1500–8. doi: 10.1038/sj.ijo.0803628. [DOI] [PubMed] [Google Scholar]
- 76.Hughes AR, Stewart L, Chapple J, McColl JH, Donaldson MD, Kelnar CJ, et al. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT) Pediatrics. 2008;121:e539–46. doi: 10.1542/peds.2007-1786. [DOI] [PubMed] [Google Scholar]
- 77.Avery A, Pallister C, Allan J, Stubbs J, Lavin J. An initial evaluation of a family-based approach to weight management in adolescents attending a community weight management group. J Hum Nutr Diet. 2012;25:469–76. doi: 10.1111/j.1365-277X.2012.01277.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Looney SM, Raynor HA. Are changes in consumption of “healthy” foods related to changes in consumption of "unhealthy" foods during pediatric obesity treatment? Int J Environ Res Public Health. 2012;9:1368–78. doi: 10.3390/ijerph9041368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Garipağaoğlu M, Sahip Y, Darendeliler F, Akdikmen O, Kopuz S, Sut N. Family-based group treatment versus individual treatment in the management of childhood obesity: Randomized, prospective clinical trial. Eur J Pediatr. 2009;168:1091–9. doi: 10.1007/s00431-008-0894-8. [DOI] [PubMed] [Google Scholar]
- 80.Pinard CA, Hart MH, Hodgkins Y, Serrano EL, McFerren MM, Estabrooks PA. Smart choices for healthy families: A pilot study for the treatment of childhood obesity in low-income families. Health Educ Behav. 2012;39:433–45. doi: 10.1177/1090198111425686. [DOI] [PubMed] [Google Scholar]
- 81.Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: A randomized, controlled trial. Pediatrics. 2007;119:517–25. doi: 10.1542/peds.2006-1746. [DOI] [PubMed] [Google Scholar]
- 82.Jiang JX, Xia XL, Greiner T, Lian GL, Rosenqvist U. A two year family based behaviour treatment for obese children. Arch Dis Child. 2005;90:1235–8. doi: 10.1136/adc.2005.071753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stark LJ, Spear S, Boles R, Kuhl E, Ratcliff M, Scharf C, et al. A pilot randomized controlled trial of a clinic and home-based behavioral intervention to decrease obesity in preschoolers. Obesity (Silver Spring) 2011;19:134–41. doi: 10.1038/oby.2010.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Skelton JA, DeMattia LG, Flores G. A pediatric weight management program for high-risk populations: A preliminary analysis. Obesity (Silver Spring) 2008;16:1698–701. doi: 10.1038/oby.2008.243. [DOI] [PubMed] [Google Scholar]
- 85.Papadaki A, Linardakis M, Larsen TM, van Baak MA, Lindroos AK, Pfeiffer AF, et al. The effect of protein and glycemic index on children's body composition: The DiOGenes randomized study. Pediatrics. 2010;126:e1143–52. doi: 10.1542/peds.2009-3633. [DOI] [PubMed] [Google Scholar]
- 86.Berkowitz RI, Wadden TA, Gehrman CA, Bishop-Gilyard CT, Moore RH, Womble LG, et al. Meal replacements in the treatment of adolescent obesity: A randomized controlled trial. Obesity (Silver Spring) 2011;19:1193–9. doi: 10.1038/oby.2010.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Epstein LH, Paluch RA, Beecher MD, Roemmich JN. Increasing healthy eating vs. reducing high energy-dense foods to treat pediatric obesity. Obesity (Silver Spring) 2008;16:318–26. doi: 10.1038/oby.2007.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Duggins M, Cherven P, Carrithers J, Messamore J, Harvey A. Impact of family YMCA membership on childhood obesity: A randomized controlled effectiveness trial. J Am Board Fam Med. 2010;23:323–33. doi: 10.3122/jabfm.2010.03.080266. [DOI] [PubMed] [Google Scholar]
- 89.Davis AM, James RL, Boles RE, Goetz JR, Belmont J, Malone B. The use of TeleMedicine in the treatment of paediatric obesity: Feasibility and acceptability. Matern Child Nutr. 2011;7:71–9. doi: 10.1111/j.1740-8709.2010.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Duckworth LC, Gately PJ, Radley D, Cooke CB, King RF, Hill AJ. RCT of a high-protein diet on hunger motivation and weight-loss in obese children: An extension and replication. Obesity (Silver Spring) 2009;17:1808–10. doi: 10.1038/oby.2009.95. [DOI] [PubMed] [Google Scholar]
- 91.Gately PJ, King NA, Greatwood HC, Humphrey LC, Radley D, Cooke CB, et al. Does a high-protein diet improve weight loss in overweight and obese children? Obesity (Silver Spring) 2007;15:1527–34. doi: 10.1038/oby.2007.181. [DOI] [PubMed] [Google Scholar]
- 92.Bauer S, de Niet J, Timman R, Kordy H. Enhancement of care through self-monitoring and tailored feedback via text messaging and their use in the treatment of childhood overweight. Patient Educ Couns. 2010;79:315–9. doi: 10.1016/j.pec.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 93.Knöpfli BH, Radtke T, Lehmann M, Schätzle B, Eisenblätter J, Gachnang A, et al. Effects of a multidisciplinary inpatient intervention on body composition, aerobic fitness, and quality of life in severely obese girls and boys. J Adolesc Health. 2008;42:119–27. doi: 10.1016/j.jadohealth.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 94.Yackobovitch-Gavan M, Nagelberg N, Phillip M, Ashkenazi-Hoffnung L, Hershkovitz E, Shalitin S. The influence of diet and/or exercise and parental compliance on health-related quality of life in obese children. Nutr Res. 2009;29:397–404. doi: 10.1016/j.nutres.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 95.Rezvanian H, Hashemipour M, Kelishadi R, Tavakoli N, Poursafa P. A randomized, triple masked, placebo-controlled clinical trial for controlling childhood obesity. World J Pediatr. 2010;6:317–22. doi: 10.1007/s12519-010-0232-x. [DOI] [PubMed] [Google Scholar]
- 96.Alexy U, Reinehr T, Sichert-Hellert W, Wollenhaupt A, Kersting M, Andler W. Positive changes of dietary habits after an outpatient training program for overweight children. Nutr Res. 2006;26:202–8. [Google Scholar]
- 97.Taveras EM, Gortmaker SL, Hohman KH, Horan CM, Kleinman KP, Mitchell K, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: The High Five for Kids study. Arch Pediatr Adolesc Med. 2011;165:714–22. doi: 10.1001/archpediatrics.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bloom T, Sharpe L, Mullan B, Zucker N. A pilot evaluation of appetite-awareness training in the treatment of childhood overweight and obesity: A preliminary investigation. Int J Eat Disord. 2013;46:47–51. doi: 10.1002/eat.22041. [DOI] [PubMed] [Google Scholar]
- 99.Ben Ounis O, Elloumi M, Lac G, Makni E, Van Praagh E, Zouhal H, et al. Two-month effects of individualized exercise training with or without caloric restriction on plasma adipocytokine levels in obese female adolescents. Ann Endocrinol (Paris) 2009;70:235–41. doi: 10.1016/j.ando.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 100.Dreimane D, Safani D, MacKenzie M, Halvorson M, Braun S, Conrad B, et al. Feasibility of a hospital-based, family-centered intervention to reduce weight gain in overweight children and adolescents. Diabetes Res Clin Pract. 2007;75:159–68. doi: 10.1016/j.diabres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 101.Chen AK, Roberts CK, Barnard RJ. Effect of a short-term diet and exercise intervention on metabolic syndrome in overweight children. Metabolism. 2006;55:871–8. doi: 10.1016/j.metabol.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 102.Kelishadi R, Hashemipour M, Adeli K, Tavakoli N, Movahedian-Attar A, Shapouri J, et al. Effect of zinc supplementation on markers of insulin resistance, oxidative stress, and inflammation among prepubescent children with metabolic syndrome. Metab Syndr Relat Disord. 2010;8:505–10. doi: 10.1089/met.2010.0020. [DOI] [PubMed] [Google Scholar]
- 103.Lisón JF, Real-Montes JM, Torró I, Arguisuelas MD, Alvarez-Pitti J, Martínez-Gramage J, et al. Exercise intervention in childhood obesity: A randomized controlled trial comparing hospital-versus home-based groups. Acad Pediatr. 2012;12:319–25. doi: 10.1016/j.acap.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 104.Krebs NF, Gao D, Gralla J, Collins JS, Johnson SL. Efficacy and safety of a high protein, low carbohydrate diet for weight loss in severely obese adolescents. J Pediatr. 2010;157:252–8. doi: 10.1016/j.jpeds.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kirk S, Brehm B, Saelens BE, Woo JG, Kissel E, D’Alessio D, et al. Role of carbohydrate modification in weight management among obese children: A randomized clinical trial. J Pediatr. 2012;161:320–71. doi: 10.1016/j.jpeds.2012.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Speroni KG, Tea C, Earley C, Niehoff V, Atherton M. Evaluation of a pilot hospital-based community program implementing fitness and nutrition education for overweight children. J Spec Pediatr Nurs. 2008;13:144–53. doi: 10.1111/j.1744-6155.2008.00149.x. [DOI] [PubMed] [Google Scholar]
- 107.Ford AL, Bergh C, Södersten P, Sabin MA, Hollinghurst S, Hunt LP, et al. Treatment of childhood obesity by retraining eating behaviour: Randomised controlled trial. BMJ. 2009;340:B5388. doi: 10.1136/bmj.b5388. [DOI] [PubMed] [Google Scholar]
- 108.Tan-Ting AM, Llido L. Outcome of a hospital based multidisciplinary weight loss program in obese Filipino children. Nutrition. 2011;27:50–4. doi: 10.1016/j.nut.2009.11.028. [DOI] [PubMed] [Google Scholar]
- 109.Kelishadi R, Malekahmadi M, Hashemipour M, Soghrati M, Soghrati M, Mirmoghtadaee P, et al. Can a trial of motivational lifestyle counseling be effective for controlling childhood obesity and the associated cardiometabolic risk factors? Pediatr Neonatol. 2012;53:90–7. doi: 10.1016/j.pedneo.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 110.Satoh A, Menzawa K, Lee S, Hatakeyama A, Sasaki H. Dietary guidance for obese children and their families using a model nutritional balance chart. Jpn J Nurs Sci. 2007;4:95–102. [Google Scholar]
- 111.Savoye M, Berry D, Dziura J, Shaw M, Serrecchia JB, Barbetta G, et al. Anthropometric and psychosocial changes in obese adolescents enrolled in a Weight Management Program. J Am Diet Assoc. 2005;105:364–70. doi: 10.1016/j.jada.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 112.Reinehr T, Widhalm K, l’Allemand D, Wiegand S, Wabitsch M, Holl RW, et al. Two-year follow-up in 21,784 overweight children and adolescents with lifestyle intervention. Obesity (Silver Spring) 2009;17:1196–9. doi: 10.1038/oby.2009.17. [DOI] [PubMed] [Google Scholar]
- 113.Adam S, Westenhofer J, Rudolphi B, Kraaibeek HK. Effects of a combined inpatient-outpatient treatment of obese children and adolescents. Obes Facts. 2009;2:286–93. doi: 10.1159/000234415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics. 2005;115:e443–9. doi: 10.1542/peds.2004-2172. [DOI] [PubMed] [Google Scholar]
- 115.Reinehr T, Schaefer A, Winkel K, Finne E, Toschke AM, Kolip P. An effective lifestyle intervention in overweight children: Findings from a randomized controlled trial on “Obeldicks light”. Clin Nutr. 2010;29:331–6. doi: 10.1016/j.clnu.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 116.Tsiros MD, Sinn N, Brennan L, Coates AM, Walkley JW, Petkov J, et al. Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am J Clin Nutr. 2008;87:1134–40. doi: 10.1093/ajcn/87.5.1134. [DOI] [PubMed] [Google Scholar]
- 117.Murer SB, Knöpfli BH, Aeberli I, Jung A, Wildhaber J, Wildhaber-Brooks J, et al. Baseline leptin and leptin reduction predict improvements in metabolic variables and long-term fat loss in obese children and adolescents: A prospective study of an inpatient weight-loss program. Am J Clin Nutr. 2011;93:695–702. doi: 10.3945/ajcn.110.002212. [DOI] [PubMed] [Google Scholar]
- 118.Lofrano-Prado MC, Antunes HK, do Prado WL, de Piano A, Caranti DA, Tock L, et al. Quality of life in Brazilian obese adolescents: Effects of a long-term multidisciplinary lifestyle therapy. Health Qual Life Outcomes. 2009;7:61. doi: 10.1186/1477-7525-7-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fajcsak Z, Gabor A, Kovacs V, Martos E. The effects of 6-week low glycemic load diet based on low glycemic index foods in overweight/obese children - Pilot study. J Am Coll Nutr. 2008;27:12–21. doi: 10.1080/07315724.2008.10719670. [DOI] [PubMed] [Google Scholar]
- 120.Kelishadi R, Zemel MB, Hashemipour M, Hosseini M, Mohammadifard N, Poursafa P. Can a dairy-rich diet be effective in long-term weight control of young children? J Am Coll Nutr. 2009;28:601–10. doi: 10.1080/07315724.2009.10719792. [DOI] [PubMed] [Google Scholar]
- 121.Mohn A, Catino M, Capanna R, Giannini C, Marcovecchio M, Chiarelli F. Increased oxidative stress in prepubertal severely obese children: Effect of a dietary restriction-weight loss program. J Clin Endocrinol Metab. 2005;90:2653–8. doi: 10.1210/jc.2004-2178. [DOI] [PubMed] [Google Scholar]
- 122.St-Onge MP, Goree LL, Gower B. High-milk supplementation with healthy diet counseling does not affect weight loss but ameliorates insulin action compared with low-milk supplementation in overweight children. J Nutr. 2009;139:933–8. doi: 10.3945/jn.108.102079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kelishadi R, Hashemi M, Mohammadifard N, Asgary S, Khavarian N. Association of changes in oxidative and proinflammatory states with changes in vascular function after a lifestyle modification trial among obese children. Clin Chem. 2008;54:147–53. doi: 10.1373/clinchem.2007.089953. [DOI] [PubMed] [Google Scholar]
- 124.Ribeiro MM, Silva AG, Santos NS, Guazzelle I, Matos LN, Trombetta IC, et al. Diet and exercise training restore blood pressure and vasodilatory responses during physiological maneuvers in obese children. Circulation. 2005;111:1915–23. doi: 10.1161/01.CIR.0000161959.04675.5A. [DOI] [PubMed] [Google Scholar]
- 125.Woo KS, Chook P, Yu CW, Sung RY, Qiao M, Leung SS, et al. Effects of diet and exercise on obesity-related vascular dysfunction in children. Circulation. 2004;109:1981–6. doi: 10.1161/01.CIR.0000126599.47470.BE. [DOI] [PubMed] [Google Scholar]
- 126.Togashi K, Masuda H, Rankinen T, Tanaka S, Bouchard C, Kamiya H. A 12-year follow-up study of treated obese children in Japan. Int J Obes Relat Metab Disord. 2002;26:770–7. doi: 10.1038/sj.ijo.0801992. [DOI] [PubMed] [Google Scholar]
- 127.Davis JN, Tung A, Chak SS, Ventura EE, Byrd-Williams CE, Alexander KE, et al. Aerobic and strength training reduces adiposity in overweight Latina adolescents. Med Sci Sports Exerc. 2009;41:1494–503. doi: 10.1249/MSS.0b013e31819b6aea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Madsen KA, Garber AK, Mietus-Snyder ML, Orrell-Valente JK, Tran CT, Wlasiuk L, et al. A clinic-based lifestyle intervention for pediatric obesity: Efficacy and behavioral and biochemical predictors of response. J Pediatr Endocrinol Metab. 2009;22:805–14. doi: 10.1515/jpem.2009.22.9.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kelishadi R, Hashemipour M, Sarrafzadegan N, Mohammadifard N, Alikhasy H, Beizaei M, et al. Effects of a lifestyle modification trial among phenotypically obese metabolically normal and phenotypically obese metabolically abnormal adolescents in comparison with phenotypically normal metabolically obese adolescents. Matern Child Nutr. 2010;6:275–86. doi: 10.1111/j.1740-8709.2009.00207.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ventura E, Davis J, Byrd-Williams C, Alexander K, McClain A, Lane CJ, et al. Reduction in risk factors for type 2 diabetes mellitus in response to a low-sugar, high-fiber dietary intervention in overweight Latino adolescents. Arch Pediatr Adolesc Med. 2009;163:320–7. doi: 10.1001/archpediatrics.2009.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gately PJ, Cooke CB, Barth JH, Bewick BM, Radley D, Hill AJ. Children's residential weight-loss programs can work: A prospective cohort study of short-term outcomes for overweight and obese children. Pediatrics. 2005;116:73–7. doi: 10.1542/peds.2004-0397. [DOI] [PubMed] [Google Scholar]
- 132.Waling M, Lind T, Hernell O, Larsson C. A one-year intervention has modest effects on energy and macronutrient intakes of overweight and obese Swedish children. J Nutr. 2010;140:1793–8. doi: 10.3945/jn.110.125435. [DOI] [PubMed] [Google Scholar]
- 133.Hashemipour M, Kelishadi R, Shapouri J, Sarrafzadegan N, Amini M, Tavakoli N, et al. Effect of zinc supplementation on insulin resistance and components of the metabolic syndrome in prepubertal obese children. Hormones (Athens) 2009;8:279–85. doi: 10.14310/horm.2002.1244. [DOI] [PubMed] [Google Scholar]
- 134.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl 4):S229–53. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 135.Weigel C, Kokocinski K, Lederer P, Dötsch J, Rascher W, Knerr I. Childhood obesity: Concept, feasibility, and interim results of a local group-based, long-term treatment program. J Nutr Educ Behav. 2008;40:369–73. doi: 10.1016/j.jneb.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 136.Klohe-Lehman DM, Freeland-Graves J, Clarke KK, Cai G, Voruganti VS, Milani TJ, et al. Low-income, overweight and obese mothers as agents of change to improve food choices, fat habits, and physical activity in their 1-to-3-year-old children. J Am Coll Nutr. 2007;26:196–208. doi: 10.1080/07315724.2007.10719602. [DOI] [PubMed] [Google Scholar]
- 137.Kitzman-Ulrich H, Wilson DK, St George SM, Lawman H, Segal M, Fairchild A. The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clin Child Fam Psychol Rev. 2010;13:231–53. doi: 10.1007/s10567-010-0073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Latzer Y, Edmunds L, Fenig S, Golan M, Gur E, Hochberg Z, et al. Managing childhood overweight: Behavior, family, pharmacology, and bariatric surgery interventions. Obesity (Silver Spring) 2009;17:411–23. doi: 10.1038/oby.2008.553. [DOI] [PubMed] [Google Scholar]
- 139.Polivy J. Psychological consequences of food restriction. J Am Diet Assoc. 1996;96:589–92. doi: 10.1016/S0002-8223(96)00161-7. [DOI] [PubMed] [Google Scholar]
- 140.Gibson LJ, Peto J, Warren JM, dos Santos Silva I. Lack of evidence on diets for obesity for children: A systematic review. Int J Epidemiol. 2006;35:1544–52. doi: 10.1093/ije/dyl208. [DOI] [PubMed] [Google Scholar]
- 141.Summerbell CD, Cameron C, Glasziou PP. WITHDRAWN: Advice on low-fat diets for obesity. Cochrane Database Syst Rev. 2008:CD003640. doi: 10.1002/14651858.CD003640.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.McGovern L, Johnson JN, Paulo R, Hettinger A, Singhal V, Kamath C, et al. Clinical review: Treatment of pediatric obesity: A systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93:4600–5. doi: 10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- 143.de Niet J, Timman R, Bauer S, van den Akker E, Buijks H, de Klerk C, et al. The effect of a short message service maintenance treatment on body mass index and psychological well-being in overweight and obese children: A randomized controlled trial. Pediatr Obes. 2012;7:205–19. doi: 10.1111/j.2047-6310.2012.00048.x. [DOI] [PubMed] [Google Scholar]


