Summary
Lifecourse epidemiology studies long-term effects of social and environmental exposures on health and diseases.1, 2 A key challenge to the three models of lifecourse epidemiology is translating its empirical evidence into intervention planning especially among populations where the critical social and environmental exposures happened in the past or they are difficult to intervene. In this article, molecular pathological epidemiology (MPE) is reviewed, which was first described in 2010.3 MPE reflects the recent technological advances in molecular pathology, and has revealed that a disease (e.g. colorectal cancer), which has been studied as a single entity, actually consists of a multitude of subtypes with differing biological features (e.g. combination of KRAS mutation +/−, BRAF mutation +/−, and more). Since each subtype theoretically is associated with a different set of epidemiologic risk factors, the social and environmental determinants of health through the life course need to be reexamined from the “unique disease principle” perspective of MPE. Investigating molecular heterogeneity of disease and disease development process can help epidemiologists to identify modifiable factors at the ongoing disease development process caused by early-life exposures among adult populations.
Three Models of Lifecourse Epidemiology
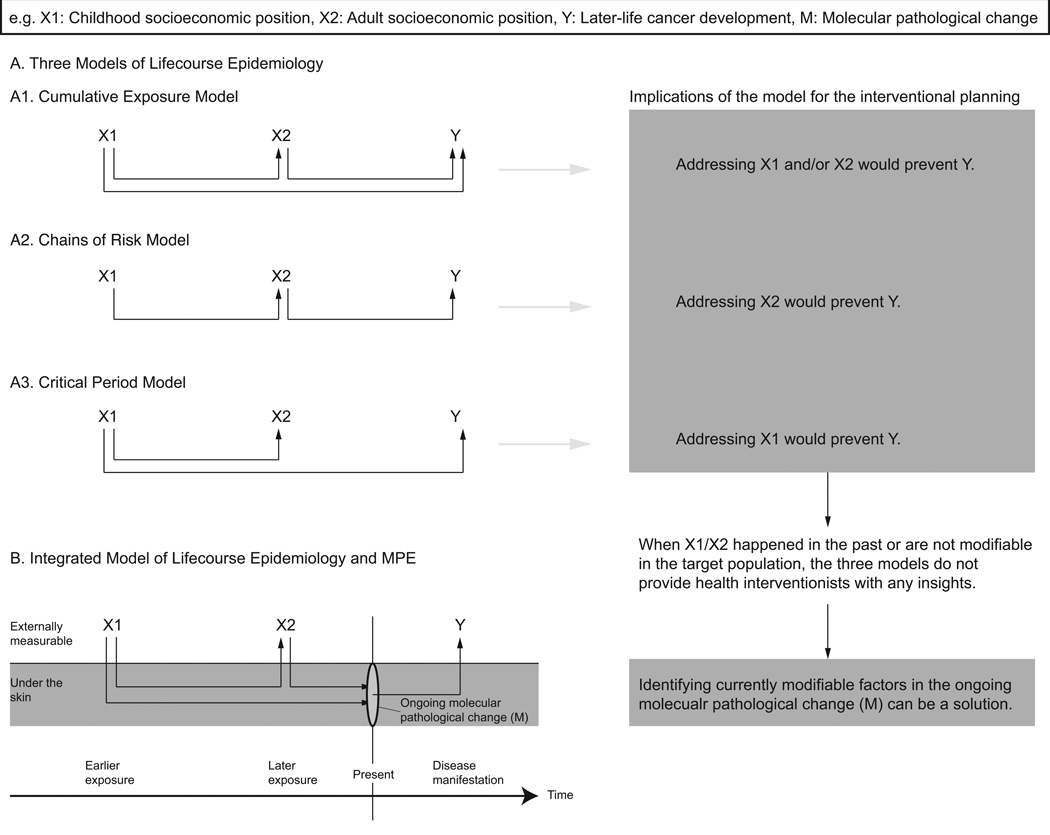
Lifecourse epidemiology (life course epidemiology) studies “long term effects on later health or disease risk of physical or social exposures during gestation, childhood, adolescence, young adulthood and later adult life.”1 It is based on the premise that various kinds of social and environmental exposures during early life independently, cumulatively and/or interactively influence health status in later adult life. To frame disease development at the population level and to guide the most effective timing of medical and public health interventions, three conceptual models of lifecourse epidemiology (“lifecourse models”) have been proposed and used for the recent decade,1, 2, 4 Figure shows an example of the models using an exposure at the earlier time period (childhood socioeconomic position), an exposure at the later time period (adult socioeconomic position), and the disease consequence (later-life cancer development).
Figure 1. Three models of lifecourse epidemiology (A) and the integrated model of molecular pathological epidemiology (MPE) and lifecourse epidemiology (B).
In section B, the ongoing molecular pathological change under the skin (orange area) can be traced from the perspective of MPE. Although addressing X1/X2 ( e.g. low socioeconomic position) can be a fundamental solution to prevent the development of Y ( e.g. cancer), X1/X2 happened in the past or are not modifiable in many situations. Therefore, the ongoing molecular pathological change at the present moment ( M; e.g. precancerous phase of adenoma) needs to be a target for behavioral interventions or preventive medical treatments to intervene the further disease development ( Y). Y reflects heterogeneity of disease process. In the other case where the vertical line of “ present” is located between X1 and X2 ( not shown), X2 can be the other targeting modifiable factor in addition to M.
First, the cumulative exposure model posits that the accumulation of different types of exposures (e.g. environmental toxins, socioeconomic disadvantages, or deleterious behaviors) causes long-term damage, leading to disease development. These risk factors can occur independently or in combination (X1 and X2 to Y in Figure, section A1). Second, the chains of risk model (the social trajectory model) refers to a sequence of linked exposures that increase disease risk because an earlier harmful experience triggers the exposure to a subsequent deleterious exposure (X1 to X2 to Y in Figure, section A2). In this model, the earlier exposure (X1) has no direct effect on the disease development. Third, the critical period model (the latency/sensitive periods model) posits that exposures during critical or sensitive periods of life can exert a long-term impact on subsequent health independently of or interactively with other exposures (X2 is not a causal variant of Y in Figure, section A3). In relation to this model, the biological programming hypothesis proposes that exposure to adverse conditions (e.g. nutritional deprivation) in utero “programs” the metabolic regulatory functions of the fetus in such a way as to make the developing child prone to obesity, diabetes and other diseases in later life.5 These three lifecourse models are useful for understanding chronological relationships among multiple exposures and disease outcome.
Challenges of Lifecourse Epidemiology in Intervention Planning
There are challenges in translating evidence from lifecourse epidemiology into health promotion planning among adult populations. This point is illustrated by introducing two randomized controlled trials. The first example is a randomized housing mobility experiment in the United States, which showed that moving from a high-poverty neighborhood to a lower-poverty neighborhood improved physical health (obesity and type 2 diabetes), mental health, and subjective wellbeing.6 While the conclusion itself is quite robust in terms of causal inference, the trial cannot provide a generalizable solution to lifecourse-driven health disparities. It is true that current place of residence can be modifiable as they did in the above-mentioned experiment; however, previous places of residence is not be modifiable and thus potential negative impacts on health of the earlier-life experience of residence in high-poverty neighborhoods have been left behind (i.e. the effect of X1/X2 in Figure will come out in later life even after people move to a low-poverty neighborhood). Therefore, although improving high-poverty neighborhoods or moving to a low-poverty neighborhood are potentially useful interventions, the challenge of addressing potential ongoing disease development process caused by earlier life exposures (the effect of X1/X2 in Figure) still remains.
The second example is based on the potential health benefit from social integration, which was first reported in 1979, and has subsequently been repeatedly corroborated in observational studies.2 However, a series of randomized control trials of social support (Enhancing Recovery for Coronary Heart Disease Patients [ENRICHD] and Families in Recovery from Stroke [FIRST]) showed that experimental provision of social support did not dramatically prevent recurrent myocardial infarction or improve post-stroke functional status among survivors. The results of these trials imply that the “naturally grown” social support in human social networks over decades are biologically different from the social support increased by the experiments. This example reveals that the biological mechanism to connect the naturally grown social and environmental exposures and disease outcomes has not been fully elucidated yet.2 Although lifecourse epidemiology has emphasized “biological programming” (please see the second section) and “embodiment” (how extrinsic factors experienced at different life stages are inscribed into an individual’s body functions or structures)1, it is now necessary to understand the more detailed dynamics “under the skin” reflecting the intrinsic uniqueness of people’s life course and disease etiology.
Molecular Pathological Epidemiology (MPE)
MPE can provide a unique viewpoint and a potential solution to the challenges of lifecourse epidemiology. MPE was first described as an integrative field of molecular pathology and epidemiology in 2010, and is defined as the “epidemiology of molecular heterogeneity of disease”.3 The biomedical and biotechnological advancements during the last ten to twenty years led to a better understanding of molecular pathology and heterogeneity of disease. Epidemiology as a field of study of human diseases needed to incorporate the knowledge and techniques of molecular pathology, which resulted in the emergence of MPE.7 For example, molecular subtyping revealed that colorectal cancer should be no longer considered as a single entity from an etiological viewpoint, but classified into biologically different subtypes according to various tumor molecular biomarkers or their combinations.8, 9 As the "unique tumor principle" implies, all the cancers are innately unique, and therefore the cancer development process and the prognosis can be also heterogeneous.10 This argument is applicable not only to cancer but also to all the other kinds of diseases (e.g. obesity) in different life courses of different individuals (“unique disease principle” of MPE).3
In this sense, MPE posits that disease development results from the accumulation of genetic and epigenetic alterations, and from the interplay of affected cells (e.g. neoplastic cells) with endogenous and environmental influences such as inhalants, diet, microbiota, and other lifestyle factors. Considering that exposures likely cause specific molecular perturbations resulting in disease etiology, it is highly likely that social and environmental exposures are associated with specific molecular alterations. MPE has several strengths in epidemiologic research, including use of molecular pathological analysis of culprit cells/tissues which enable subtyping of a disease based on pathogenetic mechanisms,3 and its population-based approach to identify a link from an exposure to molecular pathological changes across populations. The concept of MPE has rapidly been applied in a variety of settings in epidemiology and medical sciences since 2010; the evidence is summarized in Ogino et al, 2013,3 Lochhead et al, 2014,11 and Bishehsari et al12.
Most importantly, MPE provides lifecourse epidemiology with a rich biological foundation for its models. Molecular pathological changes induced by social and environmental exposures will be identified and measured (Figure, section B). For example, evidence suggests that sedentary behavior and greater body mass index are associated with a colorectal cancer subtype with less dys-regulation of the WNT/CTNNB1 (β-catenin) signaling pathway.3 Thus, the MPE-based approach can suggest a specific role of WNT/CTNNB1 in the link between physical activity and colorectal cancer risk. This type of mechanistic specificity is not possible with conventional epidemiologic studies that assume homogeneity in “colorectal cancer” diagnosis.
An Integrated Model of Lifecourse Epidemiology and MPE
MPE has two specific implications for lifecourse models (Figure, section B). First, a vertical line indicating “present” and distinguishing the “past” from the “future” can be added in the integrated model. MPE can literally reveal the present state of molecular pathological features in a target population, and thus it can lead health interventionists to think of health promotion planning from where the target population currently is located in the chronological sequence of disease pathogenesis. For example, intervening on X1 or X2 is too late in the sequence and will not alter disease prognosis. Instead, identifying the most easily modifiable factors at the present moment is the important mission of epidemiology in order to break the “embodiment” link between social and environmental exposures and the disease development and progression. Even if the critical period of disease development is located in the past or the exposures themselves are difficult to modify, MPE can provide what can be done to prevent the future progression of disease along causal pathway, given the present situation of a certain target population and given the available resources.
For example, aspirin represents one of the potentially effective interventions for ongoing molecular pathological changes throughout the colorectal neoplasia pathway.13 Aspirin inactivates PTGS2 (cyclooxygenase-2) and suppresses the production of prostaglandin G2, leading to the inhibition of downstream signaling events of reduced apoptosis and enhanced cellular proliferation. Randomized and observational studies have consistently shown that daily aspirin use is associated with the reduction in colorectal neoplasia risk.13 Therefore, if the etiological mechanism from a focal lifecourse exposure to colorectal cancer is related to the PTGS2 pathway, aspirin use can fully or partially inhibit the lifecourse-factor-driven cancer development. Most likely, the PTGS2 pathway is associated with some lifecourse exposures and not with other lifecourse exposures. However, note that caution needs to be exercised with the use of aspirin as a preventive strategy because of its known side effects (e.g. gastric bleeding).
Second, the integration of lifecourse epidemiology and MPE (“the integrated model of lifecourse epidemiology and MPE”) can unify the three lifecourse models into one by analyzing molecular pathological changes in (potentially) culprit cells/tissues. The biological complexity of multiple factors in the etiology of health and diseases is what exactly needs to be understood, and the heterogeneity of disease etiology may play a role in generating disease heterogeneity. Molecular pathological changes in (potentially) culprit cells/tissues may have multiple roots in what happened in the past (Figure, section B), and therefore it implies that the separation of lifecourse effects of exposures into the three distinct causal types may end up imposing an oversimplified “trichotomy”.4
Conclusions
In short, reflecting the recent technological innovations in molecular pathology, it is the time for lifecourse epidemiology to reexamine its models and to incorporate the molecular pathological change under the skin in addition to social and environmental exposures. The integrated model of lifecourse epidemiology and MPE can be a novel approach, which can identify more effective interventions and the more appropriate timing in primary prevention. Once epidemiologists and health interventionists are asked to plan a health promotion program for the community population, they cannot conclude that “it is too late because the causal exposures have already happened”. Instead, they need to identify the factors currently modifiable in the target population at any levels (i.e. from molecular to societal) in relation to the ongoing molecular pathological change. The integrated model of lifecourse epidemiology and MPE definitely helps them to do so.
Acknowledgments
Funding statement: This research received a grant from The Konosuke Matsushita Memorial Foundation. AN is awarded by Japan Society for the Promotion of Science (JSPS) for his research at Yale University. RN and SO were supported in part by National Institute of Health (NIH) grant R01 CA151993 (to SO).
Footnotes
Contributionship statement: AN was involved in the concept and design for the present article. AN and IK wrote the preliminary manuscript with the literature search. IK, KCK, KW, RN, and SO contributed to the critical revision of the manuscript. All authors saw and approved the final version of this manuscript.
Ethical approval: N/A.
Conflict of interest: We declare that we have no conflict of interest.
Contributor Information
Akihiro Nishi, Email: akihiro.nishi@yale.edu.
Ichiro Kawachi, Email: ikawachi@hsph.harvard.edu.
Karestan C Koenen, Email: kck5@mail.cumc.columbia.edu.
Kana Wu, Email: hpkwu@channing.harvard.edu.
Reiko Nishihara, Email: reiko_nishihara@dfci.harvard.edu.
Shuji Ogino, Email: shuji_ogino@dfci.harvard.edu.
References
- 1.Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J Epidemiol Community Health. 2003;57(10):778–783. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berkman L. Social Epidemiology: Social Determinants of Health in the United States: Are We Losing Ground? Annual Review of Public Health. 2009;30:27–41. doi: 10.1146/annurev.publhealth.031308.100310. [DOI] [PubMed] [Google Scholar]
- 3.Ogino S, Lochhead P, Chan AT, Nishihara R, Cho E, Wolpin BM, et al. Molecular pathological epidemiology of epigenetics: emerging integrative science to analyze environment, host, and disease. Mod Pathol. 2013;26(4):465–484. doi: 10.1038/modpathol.2012.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gilman SE. The successes and challenges of life course epidemiology: a commentary on Gibb, Fergusson and Horwood (2012) Soc Sci Med. 2012;75(12):2124–2128. doi: 10.1016/j.socscimed.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Lumey LH, Stein AD, Susser E. Prenatal famine and adult health. Annu Rev Public Health. 2011;32:237–262. doi: 10.1146/annurev-publhealth-031210-101230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ogino S, King EE, Beck AH, Sherman ME, Milner DA, Giovannucci E. Interdisciplinary education to integrate pathology and epidemiology: towards molecular and population-level health science. Am J Epidemiol. 2012;176(8):659–667. doi: 10.1093/aje/kws226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ogino S, Chan AT, Fuchs CS, Giovannucci E. Molecular pathological epidemiology of colorectal neoplasia: an emerging transdisciplinary and interdisciplinary field. Gut. 2011;60(3):397–411. doi: 10.1136/gut.2010.217182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colussi D, Brandi G, Bazzoli F, Ricciardiello L. Molecular pathways involved in colorectal cancer: implications for disease behavior and prevention. Int J Mol Sci. 2013;14(8):16365–16385. doi: 10.3390/ijms140816365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ogino S, Fuchs CS, Giovannucci E. How many molecular subtypes? Implications of the unique tumor principle in personalized medicine. Expert Rev Mol Diagn. 2012;12(6):621–628. doi: 10.1586/erm.12.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lochhead P, Chan AT, Nishihara R, Fuchs CS, Beck AH, Giovannucci E, et al. Etiologic field effect: reappraisal of the field effect concept in cancer predisposition and progression. Mod Pathol. 2014 doi: 10.1038/modpathol.2014.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bishehsari F, Mahdavinia M, Vacca M, Malekzadeh R, Mariani-Costantini R. Epidemiological transition of colorectal cancer in developing countries: environmental factors, molecular pathways, and opportunities for prevention. World J Gastroenterol. 2014;20(20):6055–6072. doi: 10.3748/wjg.v20.i20.6055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogino S, Lochhead P, Giovannucci E, Meyerhardt JA, Fuchs CS, Chan AT. Discovery of colorectal cancer PIK3CA mutation as potential predictive biomarker: power and promise of molecular pathological epidemiology. Oncogene. 2014;33(23):2949–2955. doi: 10.1038/onc.2013.244. [DOI] [PMC free article] [PubMed] [Google Scholar]