Abstract
Background
Asian Americans are a rapidly growing racial/ethnic group in the United States. Our current understanding of Asian-American cardiovascular disease mortality patterns is distorted by the aggregation of distinct subgroups.
Objectives
To examine heart disease and stroke mortality rates in Asian-American subgroups to determine racial/ethnic differences in cardiovascular disease mortality within the United States.
Methods
We examined heart disease and stroke mortality rates for the 6 largest Asian-American subgroups (Asian Indian, Chinese, Filipino, Japanese, Korean, and Vietnamese) from 2003–2010. U.S. death records were used to identify race/ethnicity and cause of death by ICD-10 coding. Using both U.S. Census and death record data, standardized mortality ratios (SMR), relative SMRs (rSMR), and proportional mortality ratios (PMR) were calculated for each sex and ethnic group relative to Non-Hispanic Whites (NHW).
Results
10,442,034 death records were examined. While NHW men and women had the highest overall mortality rates, Asian Indian men and women and Filipino men had greater proportionate mortality burden from ischemic heart disease. The proportionate mortality burden of hypertensive heart disease and cerebrovascular disease, especially hemorrhagic stroke, was higher in every Asian-American subgroup compared to NHWs.
Conclusions
The heterogeneity in cardiovascular disease mortality patterns among diverse Asian-American subgroups calls attention to the need for more research to help direct more specific treatment and prevention efforts, in particular with hypertension and stroke, to reduce health disparities for this growing population.
Keywords: cardiovascular disease, stroke, etiology, ethnicity, disparities
Introduction
Asian Americans are the fastest growing racial/ethnic group in the United States, with a population of more than 18 million that is projected to reach nearly 34 million by 2050 (1,2). The 6 largest Asian-American subgroups in the U.S. are Asian Indians, Chinese, Filipinos, Japanese, Koreans, and Vietnamese; these 6 subgroups make up 84% of the Asians in the U.S., based on 2010 Census data (3). Asian Americans have seen a 46% growth in population from 2000 to 2010, more than any other major race group (3). It is estimated that the majority of future growth in the Asian-American population (94%) will come from immigrants who arrived after 2005 and their descendants (4). While in 2005 most Asians living in the U.S. were foreign-born (58%), by 2050 these individuals will account for less than half (47%) of the Asian-American population in the country (4). Current understanding of Asian-American cardiovascular disease (CVD) mortality patterns is distorted by the underrepresentation and aggregation of Asian Americans in epidemiologic surveys, which masks the heterogeneity of CVD and survival among diverse Asian-American subgroups (5–7).
While the U.S. Census first started disaggregating Asian subgroups in 1980, explicit disaggregation of Asian subgroups on national death records did not occur until 2003. As of 2010, 34 of the 50 U.S. States have mortality data explicitly disaggregated by the 6 largest Asian subgroups (8–10). Previous mortality data from the State of California and New York City have demonstrated Asian Indians and Filipinos having higher ischemic heart disease mortality, while Chinese and Japanese having higher stroke mortality compared to non-Hispanic Whites (NHW) (11–14).
There is currently a knowledge gap on the cardiovascular health of these rapidly expanding populations with little evidence to create public health policy, to offer appropriate clinical guidelines, and to recommend research agendas. In this study, we examined heart disease and stroke mortality rates in Asian-American subgroups to determine racial/ethnic differences in CVD mortality within the United States.
Methods
We examined CVD mortality rates from 2003–2010, assessing the Multiple Cause of Death mortality database from the National Center for Health Statistics (NCHS) by Asian subgroup (Asian Indian, Chinese, Filipino, Japanese, Korean, or Vietnamese) in the 34 states that as of 2010 had adopted the 2003 revision of the U.S. Standard Certificate of Death. Prior to the 2003 standard, reporting of Asian races on death certificates took a fill-in-the-blank approach, whereas the 2003 standard provides a specific check box for each Asian subgroup. While all states reported Asian subgroups to varying degrees across the time studied, we believe that states who adopted the 2003 standard had increased accuracy for subgroup reporting. The states included: Arkansas, California, Connecticut, Delaware, Florida, Georgia, Hawaii, Idaho, Illinois, Indiana, Kansas, Maine, Michigan, Minnesota, Montana, Nebraska, Nevada, New Hampshire, New Jersey, New Mexico, New York, North Dakota, Ohio, Oklahoma, Oregon, Rhode Island, South Carolina, South Dakota, Texas, Utah, Vermont, Washington, Wisconsin, Wyoming, and the District of Columbia. Mortality data for the NHW population came from the same 34 states. The primary cause of death was identified on mortality records using International Classification of Diseases, 10th revision (ICD-10), focusing on cardiovascular (I00–I09, I11, I13, I20–I51.9, I60–I69) diseases (15). The underlying cause listed on the death certificate was utilized as the primary cause of death. No other cardiac diseases if listed as sequential conditions were used in the analysis. Race/ethnicity was recorded on death certificates by the funeral director or medical examiner; questions regarding race and ethnicity on the 2003 U.S. Standard Certificate of Death match those on the 2010 U.S. Census form. We selected only the Asian subgroups represented explicitly on both the 2003 U.S. Standard Certificate of Death and 2010 U.S. Census form. We derived population data for the years 2003–2010 using linear interpolation from the 2000 and 2010 U.S. Census. We calculated average age-standardized heart disease and stroke mortality rates per 100,000 population per year using direct standardization to the NHW population in 2007. We calculated mortality rates for all heart disease as per NCHS classification (“Diseases of Heart”) and also broken down by specific etiology (ischemic, hypertensive, rheumatic, and heart failure) (16). Similarly, we examined mortality rates from all cause cerebrovascular disease, as well as for ischemic and hemorrhagic stroke separately.
We calculated standardized mortality ratios (SMR), relative SMRs (rSMR), and proportional mortality ratios (PMR) for each sex and ethnic group relative to NHWs (definitions and interpretation in Table 1). We calculated SMRs as the age-standardized, sex-specific death rate from the primary cause of death in each subgroup divided by the expected sex-specific death rate, which was the comparable rate for the NHW population. Our approach is a useful modification of the standard approach to SMRs, where the observed mortality of the Asian subgroup would be divided by the expected mortality for the NHW population. Here, we divide the expected mortality for Asian subgroup by the expected mortality for NHW. Intuitively, our approach and the standard approach should yield similar results, and divergences between the 2 approaches were minimal, based on our results. The rSMR is calculated by dividing the cause-specific SMR by the all-cause SMR, and it expresses the cause-specific mortality experience of a population relative to its overall mortality experience. The PMR is calculated by taking the proportion of observed deaths from a specified cause in each Asian subgroup divided by the proportion of deaths observed in the referent population (NHW). PMRs are unadjusted risk ratios and serve as an unstandardized measure of relative overall disease burden. They estimate the relative importance of a specific cause, such as ischemic heart disease, as a cause of death in Asian-American subpopulations. All other quantities being equal, a member of a subgroup with a PMR of 2 is twice as likely to die of a particular cause of death as a member of the referent group. Unlike SMRs and rSMRs which require population data in the denominator, PMRs rely exclusively on a single data source (death records). All deaths were available for analysis (a full population), so results are presented descriptively, and no statistical inferences (e.g., confidence intervals, p-values) are presented. To aid in visualization and interpretation of results, Loess smoothing curves were created for PMR data by cause of death to help differentiate the relationships between PMR and age for each racial/ethnic group (17). Loess curves were created for ages 45 years and older for improved accuracy given the overall low number of cardiovascular disease deaths in those <45 years old.
Table 1.
Metrics to compare Cardiovascular Disease Mortality
| Metric | Definition | Interpretation if rate is > 1 |
Calculation | |
|---|---|---|---|---|
| SMR (Standardized Mortality Ratio) | The relative rate of death due to CVD between group* and reference^ | Group is more likely to die of CVD than reference |
|
|
| rSMR (Relative SMR) | The relative rate of death due to CVD over all cause | CVD (compared to other causes) has a higher rate of death in group than reference |
|
|
| PMR (Proportionate Mortality Ratio) | Ratio of percent cause of death due to CVD between group and reference | CVD accounts for a larger percentage of deaths in group than reference |
|
group = specified Asian American subgroup by sex;
reference = all Non-Hispanic Whites
Results
Heart Disease
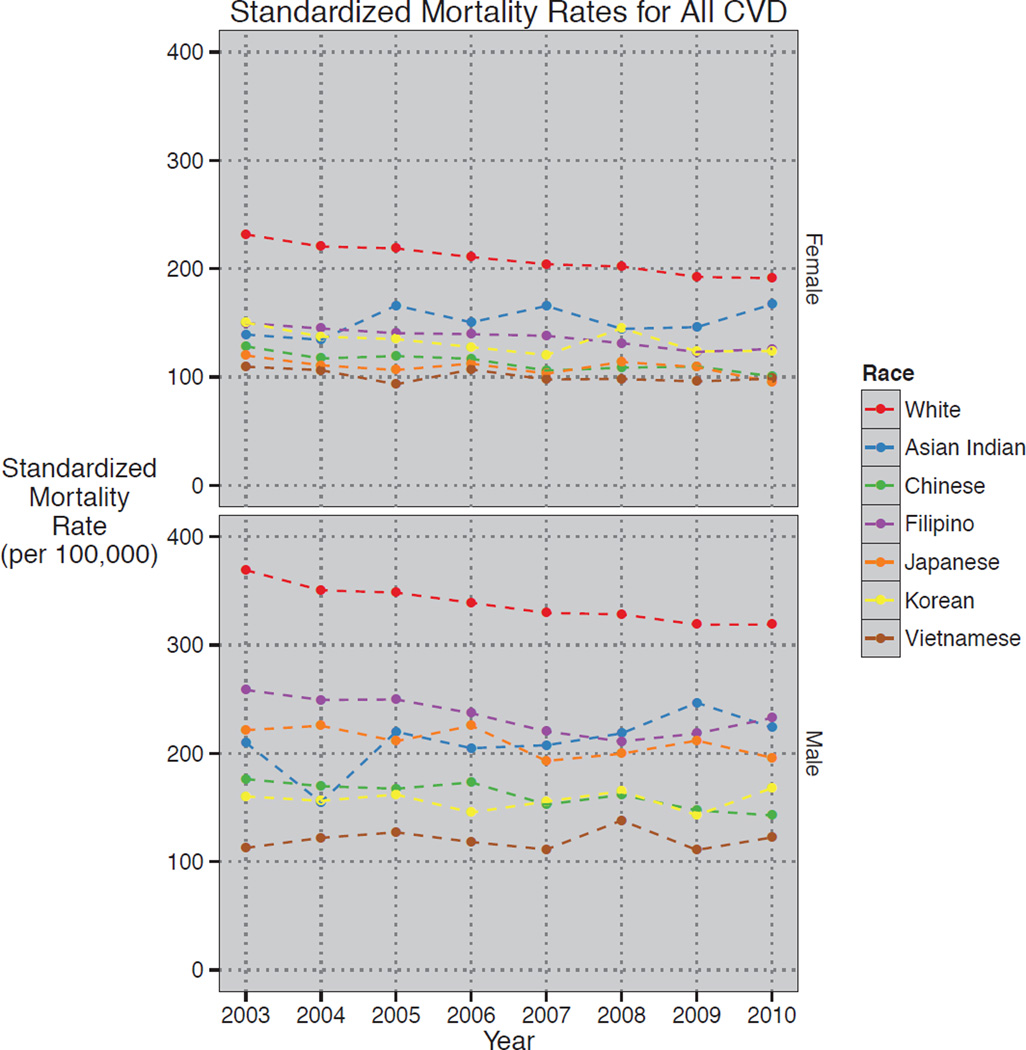
We examined 10,442,034 U.S. death records from 2003–2010. The number of observed deaths, age-standardized mortality rates, and PMRs for all heart disease and heart disease subtypes (ischemic, hypertensive, heart failure) are presented by racial/ethnic group and sex in Table 2. The total number of deaths and average mortality rates for all heart disease and heart disease types were highest among NHW men and women. Proportionate mortality burden due to ischemic disease, as reflected by PMRs, were highest in Asian Indian men (1.43) and women (1.12), followed by Filipino men (1.15). The majority of men and women from other Asian subgroups had less proportionate mortality (lower PMRs) from ischemic disease compared with NHW men (1.08) and women (0.92), respectively. Every Asian subgroup except for the Vietnamese population had greater proportionate mortality from hypertensive disease compared with NHW women (1.10) and men (0.90), especially Chinese (1.69), Filipino (1.50), and Asian Indian (1.46) women and Filipino (1.38), Chinese (1.27), and Asian Indian (1.18) men. Conversely, every Asian subgroup had lower mortality rates and proportionate mortality from heart failure when listed as the primary cause of death compared with NHWs. When examined over time (2003–2010), the standardized mortality rate from all heart disease decreased each subsequent year for NHW women and men. For Asian American subgroups however, the slope of decline across the same timeframe was less, and in the case of Asian Indian women and men was inverted, with higher standardized mortality rates from all heart disease in 2010 compared to 2003 (Figure 1). Additional data including SMRs and rSMRs for all heart disease and specific etiologies (including rheumatic heart disease) as well as stroke (ischemic and hemorrhagic) are provided in the Online Supplement, Tables 1,2.
Table 2.
Heart Disease Mortality by Asian American Subgroup (2003–2010)
| CAUSE* | ||||||
|---|---|---|---|---|---|---|
| Women | Men | |||||
| Deaths | Rate† | PMR | Deaths | Rate† | PMR | |
| Asian Indian | ||||||
| All Cause | 9,676 | 14,409 | ||||
| Diseases of the Heart | 2,716 | 147.15 | 1.06 | 4,562 | 205.59 | 1.19 |
| Ischemic | 1,972 | 108.28 | 1.12 | 3,738 | 167.45 | 1.43 |
| Hypertensive | 179 | 9.73 | 1.46 | 216 | 8.31 | 1.18 |
| Heart Failure | 175 | 11.31 | 0.73 | 126 | 8.73 | 0.35 |
| Chinese | ||||||
| All Cause | 33,239 | 36,990 | ||||
| Diseases of the Heart | 8,116 | 110.05 | 0.92 | 8,865 | 156.61 | 0.90 |
| Ischemic | 5,709 | 77.61 | 0.95 | 6,846 | 121.12 | 1.02 |
| Hypertensive | 712 | 9.63 | 1.69 | 597 | 10.09 | 1.27 |
| Heart Failure | 496 | 6.79 | 0.61 | 384 | 7.63 | 0.42 |
| Filipino | ||||||
| All Cause | 28,573 | 30,430 | ||||
| Diseases of the Heart | 7,171 | 132.23 | 0.94 | 8,761 | 232.68 | 1.08 |
| Ischemic | 4,880 | 90.81 | 0.94 | 6,354 | 168.80 | 1.15 |
| Hypertensive | 543 | 10.25 | 1.50 | 533 | 13.62 | 1.38 |
| Heart Failure | 416 | 8.38 | 0.59 | 369 | 11.52 | 0.49 |
| Japanese | ||||||
| All Cause | 26,009 | 23,085 | ||||
| Diseases of the Heart | 5,883 | 106.79 | 0.85 | 6,137 | 208.61 | 1.00 |
| Ischemic | 3,661 | 66.23 | 0.78 | 4,314 | 146.60 | 1.03 |
| Hypertensive | 404 | 7.32 | 1.23 | 277 | 9.48 | 0.95 |
| Heart Failure | 384 | 6.75 | 0.60 | 278 | 9.49 | 0.49 |
| Korean | ||||||
| All Cause | 12,203 | 10,740 | ||||
| Diseases of the Heart | 2,663 | 128.90 | 0.82 | 2,124 | 152.61 | 0.74 |
| Ischemic | 1,936 | 94.74 | 0.87 | 1,685 | 121.16 | 0.86 |
| Hypertensive | 201 | 9.59 | 1.30 | 128 | 9.24 | 0.94 |
| Heart Failure | 148 | 7.39 | 0.49 | 58 | 4.56 | 0.22 |
| Vietnamese | ||||||
| All Cause | 8,793 | 11,351 | ||||
| Diseases of the Heart | 1,680 | 97.21 | 0.72 | 2,039 | 116.21 | 0.68 |
| Ischemic | 1,187 | 70.12 | 0.74 | 1,547 | 88.23 | 0.75 |
| Hypertensive | 106 | 6.47 | 0.95 | 129 | 6.58 | 0.90 |
| Heart Failure | 98 | 6.28 | 0.45 | 74 | 5.81 | 0.26 |
| White | ||||||
| All Cause | 5,204,786 | 4,991,750 | ||||
| Diseases of the Heart | 1,353,029 | 209.51 | 0.98 | 1,355,950 | 336.08 | 1.02 |
| Ischemic | 870,390 | 134.99 | 0.92 | 979,180 | 240.75 | 1.08 |
| Hypertensive | 72,426 | 11.19 | 1.10 | 56,819 | 13.59 | 0.90 |
| Heart Failure | 150,252 | 22.36 | 1.17 | 101,072 | 27.77 | 0.82 |
Source: NCHS Diseases of the Heart (ICD-10 codes I00–I09, I11, I13, I20–I51); Ischemic (I20–I25); Hypertensive (I11, I13), Heart Failure (I50)
Average age-adjusted yearly mortality rate per 100,000 population
Figure 1. Standardized Mortality Rates for All Cardiovascular Disease by Asian-American Subgroups by Year (2003–2010).
Age-adjusted mortality rates due to all cardiovascular disease per year from 2003–2010 for Asian American subgroups compared to non-Hispanic Whites.
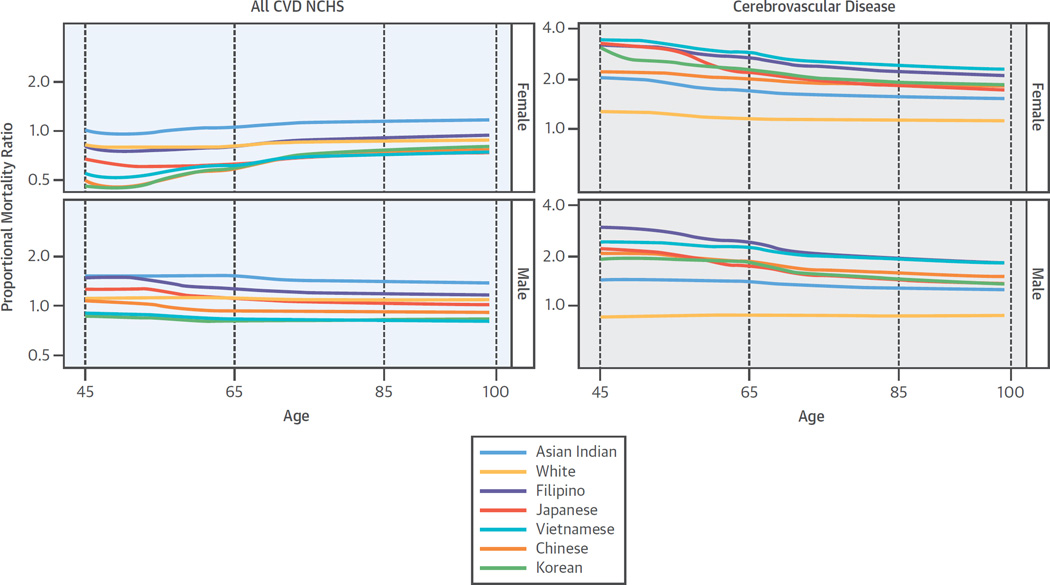
The Central Illustration shows Loess smoothing curves representing PMRs by age (45 years and older) and ethnicity for all heart disease. As seen in the figure, Asian Indians had PMRs consistently higher than NHWs at any age. Filipino men had higher PMRs when younger (45–65 years) which then approximated NHW men with increasing age. The remaining Asian subgroups had PMRs similar to or below NHWs at all ages. Loess curves by heart disease etiology (ischemic, hypertensive, rheumatic heart disease and heart failure) as well as stroke type (ischemic, hemorrhagic) are also provided in the supplemental appendix (Online Supplement Figures 1,2).
Central Illustration. Proportional Mortality Ratios by Age for Cardiovascular Disease & Cerebrovascular Disease Mortality (2003–2010)*.
Left Panel: Cardiovascular Disease Mortality
Proportional mortality ratios from ages 45 and older for all cardiovascular disease stratified by Asian American subgroups and sex compared to non-Hispanic Whites.
Right Panel: Cerebrovascular Disease Mortality
Proportional mortality ratios from ages 45 and older for all cerebrovascular disease stratified by Asian American subgroups and sex compared to non-Hispanic Whites.
*Loess smoothing curves represent PMRs by age (45 and older) and ethnicity for all cardiovascular and cerebrovascular disease.
Cerebrovascular Disease
Similar to heart disease, the highest number of deaths from cerebrovascular disease was observed in NHW women (356,142) and men (225,562), as described in Table 3. However, when examining age-adjusted mortality rates, there was more heterogeneity seen. Among all cerebrovascular disease, while NHW women (55.26 per 100,000 population) had the highest age-standardized mortality rates, in men Filipinos (65.33), Japanese (56.57), and Vietnamese (51.93) had higher mortality rates compared to NHWs (50.30). When broken down by stroke type, NHW women (32.71) and men (32.92) had the highest mortality rates for ischemic stroke. For hemorrhagic stroke, both men and women from every Asian subgroup except Asian Indians had higher mortality rates and greater proportionate mortality than NHWs. The Central Illustration represents PMR curves for all cerebrovascular disease, which in contrast to heart disease, were higher in every Asian subgroup and at any age compared with NHWs. As seen in the figure, the PMR curves were highest around ages 45–65 in all Asian-American subgroups for both women and men before tapering slightly with increasing age. The Vietnamese and Filipino populations had the highest Loess curves and the greatest proportionate mortality burden from cerebrovascular disease.
Table 3.
Cerebrovascular Disease Mortality by Asian American Subgroup (2003–2010)
| CAUSE* | ||||||
|---|---|---|---|---|---|---|
| Women | Men | |||||
| Deaths | Rate† | PMR | Deaths | Rate† | PMR | |
| Asian Indian | ||||||
| All Cause | 9,676 | 14,409 | ||||
| All Cerebrovascular | 720 | 39.27 | 1.39 | 734 | 37.88 | 0.89 |
| Ischemic Stroke | 387 | 19.58 | 1.20 | 363 | 16.56 | 0.75 |
| Hemorrhagic Stroke | 177 | 8.43 | 1.78 | 215 | 8.51 | 1.45 |
| Chinese | ||||||
| All Cause | 33,239 | 36,990 | ||||
| All Cerebrovascular | 3,144 | 41.99 | 1.66 | 2,732 | 47.39 | 1.29 |
| Ischemic Stroke | 1,535 | 20.04 | 1.38 | 1,279 | 22.22 | 1.03 |
| Hemorrhagic Stroke | 778 | 10.08 | 2.28 | 833 | 13.12 | 2.19 |
| Filipino | ||||||
| All Cause | 28,573 | 30,430 | ||||
| All Cerebrovascular | 2,905 | 49.79 | 1.78 | 2,493 | 65.33 | 1.44 |
| Ischemic Stroke | 1,246 | 22.43 | 1.30 | 1,075 | 30.09 | 1.06 |
| Hemorrhagic Stroke | 856 | 13.32 | 2.92 | 826 | 18.27 | 2.64 |
| Japanese | ||||||
| All Cause | 26,009 | 23,085 | ||||
| All Cerebrovascular | 2,418 | 44.82 | 1.63 | 1,689 | 56.57 | 1.28 |
| Ischemic Stroke | 1,235 | 21.28 | 1.42 | 882 | 28.37 | 1.14 |
| Hemorrhagic Stroke | 537 | 10.55 | 2.01 | 399 | 13.63 | 1.68 |
| Korean | ||||||
| All Cause | 12,203 | 10,740 | ||||
| All Cerebrovascular | 1,092 | 47.33 | 1.57 | 677 | 44.79 | 1.10 |
| Ischemic Stroke | 448 | 18.81 | 1.10 | 289 | 18.12 | 0.80 |
| Hemorrhagic Stroke | 259 | 9.96 | 2.07 | 208 | 11.36 | 1.89 |
| Vietnamese | ||||||
| All Cause | 8,793 | 11,351 | ||||
| All Cerebrovascular | 955 | 50.12 | 1.90 | 906 | 51.93 | 1.40 |
| Ischemic Stroke | 371 | 18.19 | 1.26 | 355 | 19.36 | 0.93 |
| Hemorrhagic Stroke | 304 | 13.66 | 3.37 | 333 | 15.20 | 2.86 |
| White | ||||||
| All Cause | 5,204,786 | 4,991,750 | ||||
| All Cerebrovascular | 356,142 | 55.26 | 1.20 | 225,562 | 50.30 | 0.79 |
| Ischemic Stroke | 214,257 | 32.71 | 1.23 | 126,967 | 32.92 | 0.76 |
| Hemorrhagic Stroke | 56,683 | 9.31 | 1.06 | 48,013 | 11.33 | 0.94 |
Source: NCHS Cerebrovascular Diseases (ICD-10 codes I60–I69); Ischemic (I63); Hemorrhagic (I60–I62)
Average age-adjusted yearly mortality rate per 100,000 population
Sensitivity Analyses
To address any potential geographic or population bias, we conducted sensitivity analyses examining cardiovascular disease mortality rates and calculated mortality ratios for NHWs from all 50 states, in addition to the 34 states where Asian-American subgroup data has been made available. We found no systemic or substantive differences in mortality rates or calculated SMRs, rSMRs, or PMRs for Asian-American subgroups using either 34- or 50-state data. In addition, we determined mortality rates and ratios for non-Hispanic Blacks and Hispanics over the same timeframe (2003–2010) in the 50-state data. These data are available for review and comparison in the Online Supplement, Tables 3,4,5.
Discussion
The major findings of this study demonstrate differences in CVD mortality seen among Asian-American subgroups with varying degrees of proportionate mortality burden. The higher proportionate mortality from hypertensive disease and hemorrhagic stroke among every Asian-American subgroup should prompt the need to further evaluate and address hypertension treatment and control in Asian-American populations. To our knowledge, this is the first study that has characterized CVD mortality using U.S. death certificate data from multiple Asian-American populations.
Heart Disease
Despite increasing diversity within the U.S., most of the knowledge available on CVD mortality is derived from NHW populations. Until recently, Asians/Pacific Islanders had been aggregated in census and mortality data, making it difficult to calculate accurate mortality rates for Asian-American subgroups. Previous studies using data from specific Asian-American subgroups are consistent with our results. Chinese and Japanese immigrants have been shown to have lower CVD mortality rates than NHWs (11–14,18). The Ni-Hon-San Study compared CVD rates and risk factors in Japanese men living in Japan, Hawaii, and California (19). Coronary heart disease mortality rates in Hawaii were intermediate between rates in Japan and California, illustrating the effects of immigration and acculturation on CVD risk (20). When comparing U.S. mortality rates in Asian-American subgroups to mortality data from each country of origin (India, China, Philippines, Japan, Vietnam, and Korea) as collected and reported by the World Health Organization, CVD mortality rates were in general much higher among Asian Americans (21, 22).
The higher PMRs for ischemic disease seen in the Asian Indian population are consistent with previously collected data demonstrating higher prevalence rates for this group (23). Coronary heart disease in Asian Indians has been well-documented in both native and immigrant populations (24–27). Mortality data from California has established coronary heart disease as the leading cause of death in Asian Indians, especially at younger ages for men (11). Several theories have been proposed to explain the higher prevalence of ischemic disease in Asian Indians including diabetes, prothrombotic factors, and abnormal lipoproteins (28–30). Data from the INTERHEART registry suggest that Asian Indians have a greater burden of traditional cardiovascular risk factors, particularly at a younger age (31). Acute coronary syndrome and overall cardiovascular mortality occur approximately 7–11 years earlier, with increased severity in Asian Indians compared with other ethnic groups (31, 32). Data from this analysis confirm the prematurity of death from ischemic disease in Asian Indians living in the U.S. As demonstrated by the Loess curves (Central Illustration, Asian Indians had the highest PMRs for all heart disease compared to other Asian-American subgroups and NHWs. In stark contrast to other racial/ethnic groups, heart disease mortality rates in Asian Indians were higher in 2010 than in 2003, providing an important target for public health efforts. The higher proportionate mortality for ischemic disease observed among Filipino men has not been previously reported, and also warrants further attention.
There was greater proportionate mortality from hypertensive disease in every Asian-American subgroup. Previous research has demonstrated higher hypertension prevalence in the Filipino, Japanese, and Vietnamese populations, but not in other Asian-American subgroups (33,34). Further research is needed to better understand whether this reflects actual differences in pathophysiology, treatment, or control of hypertension among Asian Americans, or could be related to coding differences on death certificates. Regardless, these data present an opportunity at both the individual patient and population levels for improving awareness, treatment, and control of hypertension in Asian Americans.
Cerebrovascular Disease
Proportionate mortality from cerebrovascular disease was higher in every Asian-American subgroup compared to NHWs. Previous evidence has shown increased stroke rates among the Filipino, Japanese, and Asian Indian immigrant populations in both the United States and United Kingdom (19,35). Klatsky et al. reported that Filipinos, Chinese, and Japanese were more likely to have hemorrhagic stroke or subarachnoid hemorrhage compared to NHWs (36). Traditional risk factors for stroke such as hypertension, diabetes, and dyslipidemia vary in prevalence among Asian subgroups, and suggest multiple pathways that increase risk for stroke and mortality based on ethnicity. For example, hypertension appears to correlate more closely with hemorrhagic stroke risk in the Filipino population while diabetes and dyslipidemia may play more of a role among Asian Indians (35,36). Although there is uniformly higher proportionate mortality from stroke for all Asian American subgroups compared to NHWs, the known ethnic differences in cardiovascular risk factors may warrant unique and targeted approaches for prevention and management. Future studies should include socioeconomic and geographic data, which will help to elucidate mechanisms leading to cerebrovascular disease in Asian Americans. Previous studies have shown a decrease in stroke prevalence with increased duration of residence in the United States for Japanese and Chinese immigrants (12,37). It is unknown whether Asian Americans experience higher stroke mortality within the “stroke belt” (southeastern U.S.) compared with other regions, as has been demonstrated in African Americans and NHWs (38). As seen in the Loess curves (Central Illustration), every Asian subgroup had higher PMRs for cerebrovascular disease compared with NHWs, particularly the Filipino and Vietnamese populations.
Limitations
Limitations of our study include data based on national death certificates, which may contain errors in the documented cause of death. The challenge of determining whether the underlying cause of death was cardiovascular and to further distinguish among the different categories of cardiovascular disease must be acknowledged. The diagnosis of heart failure, for example, can be a consequence of either ischemic or hypertensive heart disease or both, and therefore must be interpreted with caution when listed on the death certificate as the underlying cause of death. Census and mortality data may have been subject to misclassification of ethnicity, which may have affected death rates (39,40). An NCHS study found that misreporting of Asian-American race/ethnicity leads to an underreporting of Asian-American death rates by approximately 11% (41). The U.S. Census race/ethnicity reporting, however, is based on the gold standard of self-report. The correlation between rSMRs (which use mortality data in the numerator and census data in the denominator) and PMRs (which use mortality data in both numerator and denominator) in this population-based analysis indicates reproducibility in estimates derived separately from census and mortality data. Another limitation is the incomplete adoption of the 2003 revision of the U.S. Standard Certificate of Death that reports Asian- American subgroup race/ethnicity. Although only 34 states had implemented the 2003 revision at the time of this analysis, the geographic distribution is widespread. Additionally, based on 2010 U.S. Census data, 84% of the Asian-American population resides within the 34 states that were analyzed. We could not account for potential confounders of mortality, such as socioeconomic status, education, nativity (foreign versus U.S. born), level of acculturation, or area of residence (beyond the state level) given the use of death certificate data. However, county-level data will soon be available making it possible to examine socioeconomic and geographic disparities among Asian-American subgroups that also may contribute to the heterogeneity seen in CVD mortality rates. Finally, we could not examine CVD mortality rates for other Asian-American subgroups that were not represented on the U.S. death certificate, which per 2010 Census data, accounts for approximately 16% of the Asian-American population.
Conclusion
In the United States, the proportion of the population accounted for by Asian-American subgroups is significant and increasing. Despite seeing yearly improvements in CVD mortality rates among NHWs, Asian-American subgroups have not attained similar rates of improvement, suggesting that the messages on prevention and management of CVD are not effectively reaching this population. Declines in CVD mortality during the last decade were not proportionately enjoyed by all racial/ethnic subgroups. The lack of national mortality statistics for CVD among Asian Americans has made it difficult to recommend research agendas, to create public health policy, and to offer appropriate clinical guidelines. Using disaggregated mortality data, this analysis demonstrates differences in CVD mortality among diverse Asian-American subgroups. These findings stress the importance of increasing efforts in prevention, health education, and community outreach to help target the highest risk groups. Community health programs such as PRANA (Prevention and Awareness for South Asians) and Project AsPire (Asian American Partnership in Research and Endowment) are helping to raise awareness of cardiovascular health disparities among Asian-American subgroups (42,43). Public health initiatives that are culturally-competent and increase awareness and screening for traditional cardiovascular risk factors may help lower the burden of CVD mortality within Asian American communities.
Supplementary Material
PERSPECTIVES.
Competency in Medical Knowledge
Aggregation of Asian Americans in epidemiologic studies masks the heterogeneity of cardiovascular disease among diverse subgroups, yet when compared to non-Hispanic whites, Asian Indians and Filipinos exhibit proportionately greater mortality from ischemic heart disease and Asian Americans generally face proportionately greater mortality related to hypertensive heart disease and cerebrovascular disease.
Competency in Patient Care
Physicians should incorporate culturally-competent approaches to management of Asian American patients to lower their cardiovascular risk.
Translational Outlook
Additional studies are needed to elucidate the mechanisms responsible for the disparities in cardiovascular disease outcomes among rapidly enlarging subgroups of Asian Americans seeking those most amenable to interventions that reduce risk.
Acknowledgements
This study was supported by grant from the National Institute on Minority Health and Health Disparities (1 R01 MD 007012-01 CAUSES: Causes of Asian American mortality Understood by Socio-Economic Status).
Abbreviations
- NHW
Non-Hispanic Whites
- PMR
proportional mortality ratios
- SMR
standardized mortality ratios
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: All authors declare they have no conflicts of interest.
References
- 1.Palaniappan LP, Araneta MR, Assimes TL, et al. Call to action: cardiovascular disease in Asian Americans: a science advisory from the AHA. Circulation. 2010;122:1242–1252. doi: 10.1161/CIR.0b013e3181f22af4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim G, Chiriboga DA, Jang Y, Lee S, Huang CH, Parmelee P. Health status of older Asian Americans in California. J Am Geriatr Soc. 2010;58:2003–2008. doi: 10.1111/j.1532-5415.2010.03034.x. [DOI] [PubMed] [Google Scholar]
- 3.Selected Population Profile in the United States. United States Census Bureau. United States Department of Commerce; [Retrieved 20 May 2013]. [Google Scholar]
- 4.Passel J, Cohn DUS. Population Projections: 2005–2050. Pew Hispanic Center. 2008 Feb 11; [Google Scholar]
- 5.Keppel KG, Pearcy JN, Heron MP. Is there progress toward eliminating racial/ethnic disparities in the leading causes of death? Public Health Rep. 2010;125:689–697. doi: 10.1177/003335491012500511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. White House Office of the Press Secretary. Executive Order: Increasing Participation of Asian Americans. 2009 Oct 14; [Google Scholar]
- 7.Narayan KM, Aviles-Santa L, Oza-Frank R, et al. Report of a National Heart, Lung, And Blood Institute Workshop: heterogeneity in cardiometabolic risk in Asian Americans In the U.S. Opportunities for research. J Am Coll Cardiol. 2010;55:966–973. doi: 10.1016/j.jacc.2009.07.075. [DOI] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics, Centers for Disease Control and Prevention. Report to evaluate the U.S. standard certificates. 2001 [Google Scholar]
- 9.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57:1–134. [PubMed] [Google Scholar]
- 10.Kochanek KD, Xu J, Murphy SL, Minino AM, Kung H. Deaths: Preliminary Data for 2009. Natl Vital Stat Rep. 2010;59:1–68. [PubMed] [Google Scholar]
- 11.Palaniappan L, Wang Y, Fortmann SP. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14:499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Wild SH, Laws A, Fortmann SP, Varady AN, Byrne CD. Mortality from coronary heart disease and stroke for six ethnic groups in California, 1985 to 1990. Ann Epidemiol. 1995;5:432–439. doi: 10.1016/1047-2797(95)00058-5. [DOI] [PubMed] [Google Scholar]
- 13.Worth RM, Kato H, Rhoads GG, Kagan K, Syme SL. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: mortality. Am J Epidemiol. 1975;102:481–490. doi: 10.1093/oxfordjournals.aje.a112186. [DOI] [PubMed] [Google Scholar]
- 14.Fang J, Madhavan S, Alderman MH. Cardiovascular mortality of Chinese in New York City. J Urban Health. 1999;76:51–61. doi: 10.1007/BF02344461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. International statistical classification of diseases and related health problems, tenth revision (ICD-10) 2nd ed. Geneva: Switzerland; 2004. [Google Scholar]
- 16.National Center for Health Statistics. NCHS instruction manual, part 9: ICD–10 cause-of-death lists for tabulating mortality statistics. Hyattsville, MD: 2009. Available from: http://www.cdc.gov/nchs/data/dvs/Part9InstructionManual2009.pdf. [Google Scholar]
- 17.Cleveland, William S. "Robust Locally Weighted Regression and Smoothing Scatterplots". Journal of the American Statistical Association. 1979;74:829–836. [Google Scholar]
- 18.Benfante R. Studies of cardiovascular disease and cause-specific mortality trends in Japanese-American men living in Hawaii and risk factor comparisons with other Japanese populations in the Pacific region: A review. Hum Biol. 1992;64:791–805. [PubMed] [Google Scholar]
- 19.Marmot MG, Syme SL, Kagan A, Kato H, Cohen JB, Belsky J. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: Prevalence of coronary and hypertensive heart disease and associated risk factors. Am J Epidemiol. 1975;102:514–525. doi: 10.1093/oxfordjournals.aje.a112189. [DOI] [PubMed] [Google Scholar]
- 20.Sekikawa A, Satoh T, Hayakawa T, Ueshima H, Kuller LH. Coronary heart disease mortality among men aged 35–44 years by prefecture in Japan in 1995–1999 compared with that among white men aged 35–44 by state in the United States in 1995–1998: Vital statistics data in recent birth cohort. Jpn Circ J. 2001;65:887–892. doi: 10.1253/jcj.65.887. [DOI] [PubMed] [Google Scholar]
- 21.National Academy of Sciences. U.S. Health in International Perspective: Shorter Lives, Poorer Health. [PubMed] [Google Scholar]
- 22.World Health Organization. Mortality estimates by cause, age, sex for the year. Geneva: WHO; 2008. [accessed May 2, 2013]. Available at http:www/who-int/healthinfo/global_burden_disease/en/ [Google Scholar]
- 23.Holland AT, Wong EC, Lauderdale DS, Palaniappan LP. Spectrum of cardiovascular diseases in Asian-American racial/ethnic subgroups. Ann Epidemiol. 2011;21:608–614. doi: 10.1016/j.annepidem.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Balarajan R. Ethnic differences in mortality from ischaemic heart disease and cerebrovascular disease in England and Wales. BMJ. 1991;302:560–564. doi: 10.1136/bmj.302.6776.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE) Lancet. 2000;356:279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 26.Enas EA, Garg A, Davidson MA, Nair VM, Huet BA, Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States. Indian Heart J. 1996;48:343–353. [PubMed] [Google Scholar]
- 27.Xavier D, Pais P, Devereaux PJ, et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 28.Mather HM, Keen H. The Southall Diabetes Survey: Prevalence of known diabetes in Asians and Europeans. Br Med J (Clin Res Ed) 1985;291:1081–1084. doi: 10.1136/bmj.291.6502.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Markovitz JH, Kulkarni K, Goldschmidt-Clermont P, Kiefe CI, Rustagi P, Sekar P, Nanda N. Increased platelet activation and fibrinogen in Asian Indians. Potential implications for coronary risk. Eur Heart J. 1998;19:720–726. doi: 10.1053/euhj.1997.0800. [DOI] [PubMed] [Google Scholar]
- 30.Chuang CZ, Subramaniam PN, LeGardeur BY, Lopez A. Risk factors for coronary artery disease and levels of lipoprotein(a) and fat-soluble antioxidant vitamins in Asian Indians of USA. Indian Heart J. 1998;50:285–291. [PubMed] [Google Scholar]
- 31.Joshi P, Islam S, Pais P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 32.Rosengren A, Wallentin L, Simoons M, et al. Age, clinical presentation, and outcome of acute coronary syndromes in the Euroheart acute coronary syndrome survey. Eur Heart J. 2006;27:789–795. doi: 10.1093/eurheartj/ehi774. [DOI] [PubMed] [Google Scholar]
- 33.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the Asian adult population: United States: 2004–2006. Adv Data. 2008:1–2. [PubMed] [Google Scholar]
- 34.Ye J, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: Results from a National Health Survey. Ann Epidemiol. 2009;19:718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gunarathne A, Patel JV, Gammon B, Gill PS, Hughes EA, Lip GY. Ischemic stroke in South Asians: a review of the epidemiology, pathophysiology, and ethnicity-related clinical features. Stroke. 2009;40:e415–e423. doi: 10.1161/STROKEAHA.108.535724. [DOI] [PubMed] [Google Scholar]
- 36.Klatsky AL, Friedman GD, Sidney S, Kipp H, Kubo A, Armstrong MA. Risk of hemorrhagic stroke in Asian American ethnic groups. Neuroepidemiology. 2005;25:26–31. doi: 10.1159/000085310. [DOI] [PubMed] [Google Scholar]
- 37.Fang J, Foo SH, Jeng JS, Yip PK, Alderman MH. Clinical characteristics of stroke among Chinese in New York City. Ethn Dis. 2004;14:378–383. [PubMed] [Google Scholar]
- 38.Howard G, Howard VJ. Ethnic disparities in stroke: The scope of the problem. Ethn Dis. 2001;11:761–768. [PubMed] [Google Scholar]
- 39.Ahmad OB, Boschi-Pinto C, Lopez AD, et al. Age Standardization of Rates: A New WHO Standard. GPE Discussion Paper Series: World Health Organization. 2001 [Google Scholar]
- 40.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: A summary of current research, 1999. Vital Health Stat. 1999;2:1–13. [PubMed] [Google Scholar]
- 41.Sorlie PD, Rogot E, Johnson NJ. Validity of demographic characteristics on the death certificate. Epidemiology. 1992;3:181–184. doi: 10.1097/00001648-199203000-00018. [DOI] [PubMed] [Google Scholar]
- 42.PRANA (Prevention and Awareness for South Asians) http://www.pamf.org/southasian. [Google Scholar]
- 43.Project AsPire (Asian American Partnership in Research and Endowment) http://asian-health.med.nyu.edu/research/aspire. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.