Abstract
OBJECTIVE
To evaluate 3- and 6-month weight-loss outcomes achieved when physicians refer overweight/obese patients to an automated 3-month Internet-based behavioral weight-loss intervention.
RESEARCH DESIGN AND METHODS
A total of 154 patients age 18–70 years with a BMI between 25 and 45 kg/m2 and access to a personal computer and the Internet were randomly assigned to 3 months of Internet behavioral intervention (IBI; n = 77) with 12 weekly videos teaching behavioral weight-loss skills, a platform for submitting self-monitored data, and automated feedback or an education-only Internet-delivered eating and activity control group (IDEA; n = 77). Outcome measures were weight loss after 3 months (primary outcome) and 6 months and changes in weight-control behaviors (secondary outcomes).
RESULTS
In intent-to-treat analyses with baseline weight carried forward for missing data, IBI produced significantly larger mean (SD) weight losses than IDEA at 3 months (5.5 kg [4.4] vs. 1.3 kg [2.1]) and 6 months (5.4 kg [5.6] vs. 1.3 kg [4.1]) (P < 0.001). Participants in IBI compared with IDEA were also more likely to achieve a clinically significant weight loss of 5% of initial body weight at 3 months (53.3 vs. 9.1%) and 6 months (48.1 vs. 15.6%) (P < 0.001) and reported more frequent use of weight control–related strategies.
CONCLUSIONS
Physician referral to an Internet-based behavioral weight-loss intervention produced clinically significant weight loss for over half of the patients studied. Further research is needed to determine the effectiveness of implementing this intervention more broadly within diverse health care settings.
Introduction
Over two-thirds of U.S. adults are overweight or obese and therefore at increased risk of developing type 2 diabetes (1,2). Physicians are in an excellent position to identify these individuals and advise them to lose weight, which has been shown to reduce the risk of developing diabetes and to improve a variety of health outcomes (3,4). However, few physicians provide their patients with counseling to achieve weight loss (5). The physician counseling literature suggests that having physicians advise their patients to lose weight, while referring them to an effective program or allied health counselors rather than trying to offer counseling themselves, may be the most effective model for obesity treatment (3).
Unfortunately, there are few options for reimbursed weight-loss programs to which physicians can refer their patients (6). Behavioral weight-loss programs (BWLs) such as the lifestyle intervention used in the Diabetes Prevention Program (DPP) produce weight losses of 7–10%, reduce the risk of developing type 2 diabetes, and improve cardiovascular disease risk factors (7–10). However, these programs typically involve frequent group or individual sessions, are costly to both patients and providers, may not appeal to large numbers of patients seeking to lose weight, and are not widely available outside of research studies (8). Efforts to translate the DPP for delivery by medical and allied health professionals (e.g., in primary care practices) and in community settings such as the YMCA have produced a modest mean weight loss of 3.2–4.3% of initial body weight as determined by meta-analysis (11). There are also continued concerns about the cost, reach, accessibility, and long-term sustainability of these programs, which have relied heavily on in-person treatment delivery that is not well financed by the current health care system (11).
Shortcomings associated with in-person treatment delivery may be mitigated by adapting BWLs for Internet delivery (12,13), but there have been few randomized controlled trials testing these programs as a resource for physicians to refer their overweight and obese patients. In early studies of patients recruited through health care providers, the Internet was used to provide tailored or personal advice but not a structured BWL with a clearly defined curriculum of training in empirically validated behavioral weight-loss strategies. Attrition was high in these studies, and weight losses were quite limited (14,15). More recent studies of physician referral to Internet programs have used stronger behavioral programs but have provided substantial contact with health care coaches in person, by phone, and/or via e-mail (16–19). Although weight losses have been better in some of these studies [e.g., 4.8 kg at 12 months (16) and 5.1 kg at 24 months (18)], the human interaction once again makes these programs more expensive to deliver and less easily disseminated.
The primary objective of the Rx Weight Loss Trial was to examine the weight losses produced by a nearly fully automated Internet BWL compared with a healthy eating and activity Internet newsletter control condition, after a 3-month program and at 3-month follow-up, among patients who were randomized after accepting a referral to the trial by their physicians.
Research Design and Methods
Design Overview
Participants were referred to the Rx Weight Loss Trial by 35 physicians at 5 primary care and 1 endocrinology practice in Rhode Island. Physicians identified potential participants during routine care and reviewed the study and inclusion/exclusion criteria with them. Physicians were especially encouraged to refer individuals with one or more obesity-related comorbidities, such as diabetes, hypertension, or metabolic syndrome. A referral form was signed by both the physician and patient and faxed to the researchers. Interested participants were contacted by the research staff, phone screened for eligibility, and scheduled for an orientation session, at which time further information was provided about the study and informed consent completed. Participants were scheduled for a baseline assessment and randomization/program kickoff visit ∼1 week later.
Participants were randomly assigned to a 3-month Internet behavior therapy program or Internet-Delivered Eating and Activity (IDEA) control condition with information on healthy eating habits and physical activity. During both the randomization/program kickoff visit and in their lesson materials, participants in both conditions received information pertaining to a healthy rate of weight loss and safe engagement in physical activity. The importance of regular contact with the referring physician for adjustments in medications was stressed. Access to the Internet interventions ended after 12 weeks in both groups. Both groups were assessed at the end of the 3-month program (posttreatment) and after 3 additional months of follow-up and received $25 and $50, respectively, for completing the assessments. Study procedures were approved by the Institutional Review Board of The Miriam Hospital.
Participants
Participants were 154 overweight or obese English-speaking individuals with a BMI of 25–45 kg/m2, age 18–70 years old, with access to a personal computer and the Internet. Exclusion criteria included a weight loss of ≥5% of initial body weight within the last 6 months, current participation in another weight-loss program or current use of weight-loss medication, participation in a weight-loss program at the study clinic within the last 2 years, living with another study participant, pregnant or breastfeeding within the last 6 months, a plan to become pregnant or move to a new geographic region within 6 months, current chemotherapy or radiation treatment for cancer, untreated serious mental illness, or hospitalization for mental illness within the last 12 months.
Randomization and Interventions
Participants were randomly assigned to one of the two treatment conditions using a computer-generated permuted blocking procedure, stratified by sex. A 1:1 randomization scheme was used. The allocation sequence was concealed until a patient consented to participate and had completed the baseline assessment.
Internet Behavioral Intervention
The Internet Behavioral Intervention (IBI) program included 12 weekly multimedia behavioral lessons, a website for submitting self-monitoring data, and weekly automated feedback provided to the participant on their progress to date. Participants were introduced to the IBI program at the 60-min randomization/program kickoff visit; they were given a goal of losing 1 to 2 lbs/week and achieving a total weight loss of ≥10% of initial body weight. To accomplish this, they were prescribed a calorie goal of 1,200–1,500 kcal/day depending on initial body weight with ≤30% calories from fat (40–60 g of fat/day) and a physical activity goal that gradually increased to 200 min/week of physical activity using activities similar in intensity to brisk walking. The remainder of the randomization/program kickoff visit was used to teach skills for self-monitoring daily food intake, physical activity minutes, and body weight. Participants received paper diaries and a calorie reference book for this purpose.
Standard behavioral strategies for changing their eating and activity were taught to the participants by having them view weekly 10–15-min interactive multimedia behavioral weight-loss lessons. In contrast to previous studies using static lessons with text and graphics (20), interactive lessons incorporating video, animation, audio, quizzes, and exercises for goal setting, planning, and problem-solving were developed to improve patient engagement (21). These lessons were based on strategies used in the DPP and Look AHEAD trials and included topics such as restaurant eating, changing the home environment, and social support (9,22). Daily values for body weight, caloric intake, fat intake (g), and physical activity minutes were submitted at least weekly to the Rx Weight Loss website. In response to their submissions, participants received a weekly automated tailored feedback message. The feedback messages were generated via an algorithm that compared participants’ self-reported values to their goals for weekly and overall weight loss, caloric intake, and physical activity minutes. Participants received praise for meeting goals and, when goals were not met, received specific recommendations for behavioral strategies to implement, along with support and encouragement. Automated e-mail reminder messages were sent weekly to participants who were not using the study website. Although in our prior research we found that human feedback was associated with larger weight losses than automated messages (20), we used automated messages in this trial because of the cost savings and ease of dissemination.
At weeks 4, 8, and 12, a letter was sent to the referring physician (and copied to the participant) indicating the number of weeks the participant had submitted data and their weight loss at that point. The letters were intended to provide physicians with information on the outcome of their referral, facilitate communication about health behaviors between physicians and patients, and enhance patients’ sense of accountability for their health and health behaviors.
IDEA
Participants in this education-only control condition were seen at the randomization/program kickoff visit and instructed to access the Rx Weight Loss website at least once weekly to view a new printable lesson with static text and graphics in the Adobe portable document format. These newsletters provided general educational information on the benefits of losing weight and healthy eating and physical activity habits. Participants were not taught behavioral weight-loss strategies and were not instructed to self-monitor their behaviors, but were encouraged to explore online resources such as choosemyplate.gov, which contains information and tools for weight loss. This condition mimicked what patients may receive during routine care: a recommendation to lose weight accompanied by general educational information. IDEA also served as a method for controlling for access to Internet-based resources.
Outcomes and Follow-up
The primary outcome was change in body weight (kg, percent of initial body weight). Weight was measured in the research setting at baseline, 3 months (end of treatment), and 6 months (follow-up) in light street clothing, without shoes, and on a calibrated scale by blinded research staff. A secondary outcome was engagement with the Internet-based treatment system, which was measured by the number of weeks (out of 12) that participants logged in to the website, and, in the IBI group only, the number of weeks that calories, physical activity minutes, and body weight were reported for at least 5 of the 7 days. At baseline, participants reported their demographic characteristics and physician-diagnosed medical conditions. At baseline, 3, and 6 months, participants reported the number of weeks in the past 3 months that they had: 1) reduced the number of calories consumed; 2) decreased fat intake; 3) increased fruits and vegetables consumed; and 4) increased exercise levels. These items were drawn from the Weight Control Practices questionnaire used in the Look AHEAD trial (23).
Statistical Analysis
PASW Statistics 19 (SPSS, Inc., 2009, Chicago, IL; http://www.spss.com) was used for all analyses. Changes in weight and levels of engagement with the Internet-based treatment system were examined via separate repeated-measures ANOVA that followed the intent-to-treat (ITT) principle in which missing data were replaced by baseline weights (assuming no weight loss). A secondary ITT analysis using multiple imputation by chained equations was used to confirm the pattern of results from the initial ITT analysis given that replacing missing data with baseline values could adversely affect tests of statistical significance (24). Given no difference in the pattern of results, the more conservative analysis with missing data replaced by baseline weights (assuming no weight loss) was selected for detailed reporting. Correlations were used to evaluate associations between engagement with the Internet-based treatment system and change in weight. Paired and independent samples t tests, respectively, were used to evaluate within-groups changes in rates of weight-control behaviors and to compare IBI and IDEA on rates of weight-control behaviors at baseline, 3, and 6 months. Unless noted otherwise, tests of significance were conducted at α = 0.05; all tests were two-tailed. This trial was designed to have 80% power to detect significant between-groups differences in weight loss of ≥2 kg at 3 and 6 months after randomization with 250 participants. An interim analysis comparing between-groups weight loss was conducted with 150 participants (4 more were in progress at the time), which resulted in early stopping of the trial due to clear evidence of efficacy. The analysis, and decision to stop the trial, were consistent with the α spending function approach to interim data analysis in which a more stringent criterion for statistical significance is used, in this case P < 0.004 (25).
Results
Recruitment and Retention
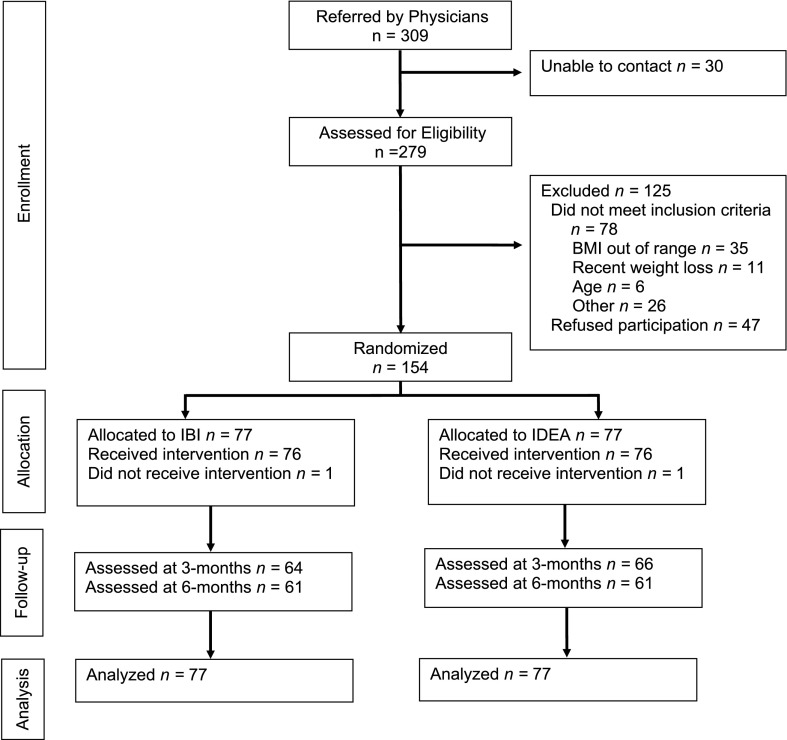
The CONSORT diagram is depicted in Fig. 1. A total of 154 participants were randomized; 84.4% completed the assessment at the end of the 3 months, and 79.2% completed the 6 month follow-up. All attrition was attributed to loss of contact with participants. Retention rates were comparable in IBI and IDEA at both 3 months (83.1% in IBI vs. 85.7% in IDEA) and 6 months (79.2% in IBI vs. 79.2% in IDEA). There were also no statistically significant differences in baseline characteristics between participants who did and did not attend a postbaseline assessment.
Figure 1.
Flow of participants through the trial. The CONSORT flow diagram includes data on physician referrals, patient enrollment, allocation to treatment groups, follow-up, and primary analysis.
Sample Characteristics
Participants’ baseline characteristics are reported in Table 1. Eighty percent of the participants were women. Participants averaged 53.2 (10.9) years of age and had an entry weight of 94.9 (16.4) kg. The most commonly endorsed physician-diagnosed medical conditions were hypertension (n = 80; 51.9% of sample), arthritis (n = 53; 34.4% of sample), cancer history (n = 22; 14.3% of sample), and type 2 diabetes (n = 20; 13.0% of sample). At baseline, IDEA participants reported higher rates of decreasing fat intake as a weight-loss strategy; there were no other statistically significant baseline differences between IBI and IDEA.
Table 1.
Baseline characteristics of participants assigned to the IBI and IDEA control conditions
| Full sample (N = 154) | IBI condition (n = 77) | IDEA condition (n = 77) | |
|---|---|---|---|
| Sex, no. (%) | |||
| Men | 31 (20.1) | 15 (19.5) | 16 (20.8) |
| Women | 123 (79.9) | 62 (80.5) | 61 (79.2) |
| Age, mean (SD), years | 53.2 (10.9) | 52.8 (10.2) | 53.6 (11.6) |
| Race, no. (%) | |||
| American Indian | 4 (2.6) | 1 (1.3) | 3 (3.9) |
| Asian | 2 (1.3) | 1 (1.3) | 1 (1.3) |
| Black | 7 (4.6) | 3 (3.9) | 4 (5.2) |
| White | 136 (88.3) | 70 (90.9) | 66 (85.7) |
| Other | 10 (6.5) | 5 (6.5) | 5 (6.5) |
| Ethnicity, no. (%) | |||
| Hispanic | 8 (5.2) | 5 (6.5) | 3 (3.9) |
| Non-Hispanic | 146 (94.8) | 72 (93.5) | 74 (96.1) |
| Marital status, no. (%) | |||
| Single | 33 (21.4) | 14 (18.2) | 19 (24.7) |
| Married | 97 (63.0) | 50 (64.9) | 47 (61.0) |
| Separated/divorced | 24 (15.6) | 13 (16.9) | 11 (14.3) |
| Education, no. (%) | |||
| High school or less | 19 (12.3) | 5 (6.5) | 14 (18.2) |
| Some college | 44 (28.6) | 27 (35.1) | 17 (22.1) |
| College or university degree | 32 (20.8) | 14 (18.2) | 18 (23.4) |
| Graduate degree | 59 (38.3) | 31 (40.2) | 28 (36.3) |
| Weight, mean (SD), kg | 94.9 (16.4) | 95.5 (16.8) | 94.3 (16.1) |
| BMI, mean (SD), kg/m2 | 34.9 (4.8) | 34.9 (4.7) | 34.9 (5.0) |
There were no statistically significant differences between IBI and IDEA at baseline.
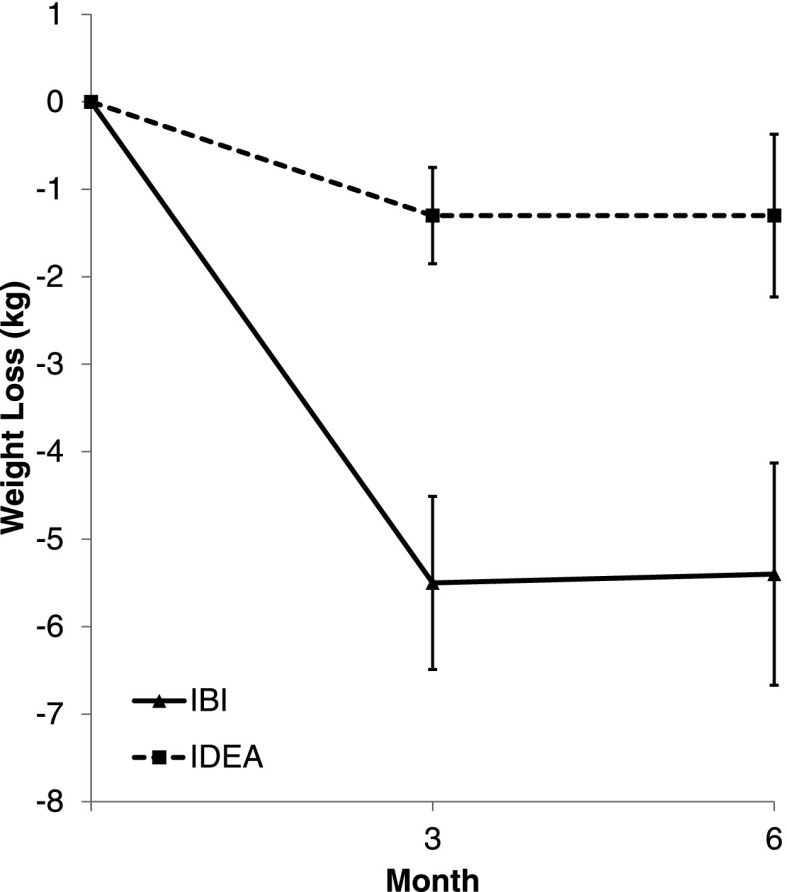
ITT Analysis
Group-specific changes in weight at months 3 and 6 are depicted in Table 2 and Fig. 2. The IBI condition produced significantly greater weight loss than IDEA at 3 months, 5.5 (4.4) vs. 1.3 (2.4) kg, and at 6 months, 5.4 (5.6) vs. 1.3 (4.1) kg (P < 0.0001 for the overall effect of group). Moreover, 53% of IBI lost at least 5% of their body weight at 3 months, and 48% met the 5% weight goal at 6 months. Of the individuals in IBI that lost at least 5% of their body weight at 3 months, 34% lost at least an additional 1 kg from 3 to 6 months (mean [SD] loss of 2.9 [1.7] kg), 29% gained at least 1 kg from 3 to 6 months (mean [SD] gain of 2.8 [1.2] kg), and 37% were within 1 kg of their 3-month weight at 6 months. Twenty-one percent of IBI participants lost at least 10% of their body weight at each assessment point. The proportion of IBI participants achieving clinically significant weight losses exceeded those in IDEA (Table 2). Nearly a third (25–30%) of participants in IDEA gained weight at 3 and 6 months, respectively, whereas this occurred in only 2–7% of participants assigned to IBI (Supplementary Fig. 1). The secondary analysis using multiple imputation produced the same pattern of results and statistically significant effects (not shown).
Table 2.
Change in weight at months 3 and 6 (ITT) for participants assigned to the IBI and IDEA control condition
| IBI (n = 77) | IDEA (n = 77) | |
|---|---|---|
| Weight loss (kg), mean (SD) | ||
| 3 months | 5.5 (4.4) | 1.3 (2.4)*** |
| 6 months | 5.4 (5.6) | 1.3 (4.1)*** |
| Weight loss (% of initial weight), mean (SD) | ||
| 3 months | 5.8 (4.4) | 1.4 (2.7)*** |
| 6 months | 5.6 (5.6) | 1.4 (4.6)*** |
| Participants with no loss or weight gain, no. (%) | ||
| 3 months | 1 (1.3) | 20 (26.0)*** |
| 6 months | 5 (6.5) | 23 (29.9)*** |
| Participants with ≥5% weight loss, no. (%) | ||
| 3 months | 41 (53.3) | 7 (9.1)*** |
| 6 months | 37 (48.1) | 12 (15.6)*** |
| Participants with ≥10% weight loss, no. (%) | ||
| 3 months | 16 (20.8) | 1 (1.3)*** |
| 6 months | 16 (20.8) | 4 (5.2)** |
**P < 0.01, ***P < 0.001 for comparison of IBI and IDEA.
Figure 2.
Change in weight at months 3 and 6 in the ITT population for participants assigned to the IBI and IDEA control condition. Means with 95% CI bars.
Engagement With the Website
IBI and IDEA did not differ significantly in the number of weeks (out of 12) that the website was used during the initial 3-month program (10.0 ± 3.0 in IBI and 9.5 ± 3.1 in IDEA; P = 0.301). Using the website for a greater number of weeks was associated with larger weight loss in the IBI condition (r = 0.41; P < 0.001) but not in the IDEA condition (r = 0.18; P = 0.110).
Participants in the IBI condition reported their daily caloric intake, physical activity minutes, and daily weight on the intervention website at least 5 days out of the week on 6.7 (4.7) of the 12 weeks. Frequency of reporting was correlated with weight loss (r = 0.54; P < 0.001).
Weight-Control Behaviors
The frequency of each weight-loss behavior increased significantly from baseline to 3 months in IBI and IDEA (P values <0.001), but IBI participants reported making changes during a greater number of weeks during this 3-month period (Table 3). Although the frequency of these changes decreased over time (Table 3), at 6 months, IBI participants still reported a greater frequency of reducing calorie and fat intake than IDEA.
Table 3.
IBI and IDEA control condition participants’ reports of their weight-control behaviors
| Baseline |
3 months |
6 months |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| IBI (n = 77) | IDEA (n = 77) | P value | IBI (n = 64) | IDEA (n = 66) | P value | IBI (n = 61) | IDEA (n = 61) | P value | |
| Reduce calories consumed | 2.1 (3.7) | 2.0 (3.1) | 0.942 | 11.0 (2.5)* | 5.9 (4.7)* | <0.001 | 6.6 (5.2)*‡ | 4.3 (4.8)*‡ | 0.013 |
| Decrease fat intake | 0.9 (2.4) | 2.2 (3.6) | 0.009 | 10.6 (2.9)* | 5.9 (5.0)* | <0.001 | 7.2 (4.9)*‡ | 5.1 (5.2)* | 0.023 |
| Increase fruits and vegetables | 2.9 (4.0) | 3.4 (4.4) | 0.481 | 9.9 (3.9)* | 7.6 (4.6)* | 0.002 | 7.8 (5.0)*‡ | 6.1 (4.9)*‡ | 0.063 |
| Increase exercise levels | 1.9 (3.3) | 2.8 (3.7) | 0.882 | 8.7 (4.0)* | 5.5 (4.9)* | <0.001 | 4.6 (5.1)*‡ | 3.2 (4.6)‡ | 0.096 |
Data represent mean (SD) number of weeks in the past 3 months that the behavior was endorsed.
*Value is significantly different from baseline value (P < 0.05).
‡Value is significantly different from 3-month value (P < 0.05).
Conclusions
The Rx Weight Loss Trial found that overweight and obese patients referred by their physician to an Internet behavioral weight-loss program lost on average 5.5 kg at the end of the 3-month program and maintained this weight loss in full at 6 months. In addition, 53% achieved a clinically significant weight loss of at least 5% of initial body weight at 3 months and 48% at 6 months. These results far exceeded the weight losses achieved by the patients who were randomly assigned to an Internet newsletter control condition and provide an effective, potentially low-cost option that physicians could use with their overweight and obese patients to reduce the risk of type 2 diabetes and other weight-related diseases.
Engagement with the IBI website was quite high during treatment and correlated with weight-loss outcomes. Prior work suggests that feedback messages, perhaps to an even greater degree than online lessons, contributed to improved weight-loss outcomes in similar programs (26). IBI participants also reported more frequent use of key behaviors, such as reducing calorie and fat intake, than was seen in IDEA. This suggests that successful skills acquisition and implementation is at least partially responsible for the superior weight losses in IBI. The use of key strategies was greatest during the 3-month treatment and then appeared to decrease; this finding emphasizes the need to develop approaches to maintaining adherence to these behaviors longer term. Likewise, additional research could be helpful in determining the relative importance of IBI components (e.g., goal-setting, lessons, self-monitoring, feedback, and reports to referring physicians).
Weight losses in the IBI condition appear to exceed those we achieved using a similar 3-month intervention in a community setting (3.5 kg weight loss at 3 months) (26). This difference in outcome may reflect differences in the two study groups. For example, participants referred by physicians may have more health concerns and therefore greater motivation to lose weight compared with individuals participating in a community wellness campaign. The difference may also suggest that there are added beneficial effects from physicians’ referrals and their involvement in the process. For example, the letters sent monthly to physicians (and copied to patients) reporting weight-loss progress may have increased the patients’ sense of accountability for their weight-loss success. Further research is needed to determine whether involving the physician improves outcomes and how best to maximize this effect.
Previous studies of weight-loss interventions in primary care settings have primarily involved physician counseling, physician counseling combined with weight-loss medications, or delivery of the intervention by other office staff (27). In many cases, the interventions were not based on empirically tested behavioral weight-loss strategies, and the results of these studies have been variable (27). We are aware of few studies that used web-based approaches in primary care, and as noted above, many of these have involved substantial face-to-face (27,28) or remote counseling (16–19). Our results suggest that comparable weight losses, at least initially, can be achieved with a nearly (i.e., with the exception of the randomization/program kickoff visit) fully automated Internet program. Likewise, our findings appear consistent with efforts to translate behavioral weight-loss interventions, such as the DPP, for delivery by medical and allied health professionals and in community settings that have achieved mean weight loss of 3.2–4.3% of initial body weight after 12 months (11). Compared with these other efforts, the Rx Weight Loss approach may incur fewer problems with cost, reach, accessibility, and long-term sustainability that have been a cause for concern with programs delivered in-person (11).
There are several limitations to this study. First, the study lasted only 6 months, and thus, it is not clear if these weight losses will be maintained long term. Since participants in behavioral weight-loss programs typically lose weight for the first 3–6 months of treatment (8) and then gradually regain weight, our study did not follow participants through the period during which they are at greatest risk of regain. Previous studies have consistently shown that continued contact is important for maintaining weight losses (8); providing further ongoing intervention and tailoring of the program to specific needs of the participant may promote long-term efficacy (29,30). Second, the study required several visits to an academic medical center that may have influenced outcomes. At the randomization/program kickoff visit, both groups were seen face-to-face and introduced to the website and the key elements of the weight-loss intervention (self-monitoring and goal-setting) were reviewed with participants in IBI. In the future, this information could be presented to participants via Internet-streamed video. Third, although some physicians referred many more patients than others (data not shown), we do not know the factors that influenced this. Nor do we know why some patients who agreed to a referral decided not to enroll. An exploration of factors affecting willingness of both physicians and patients to participate in such a program could be important if the program were to be made widely available. Fourth, while weight loss has been reliably shown to improve cardiovascular disease risk factors such as glucose control (31), we did not measure changes in these physiological indicators. Lastly, the sample had low racial and ethnic minority representation and was generally well educated; the generalizability of the results to other populations, including older adults and those with disabilities should be tested.
Strengths of the study include the system of referrals from physicians, which required very little time on their part, and the fact that the approach we used is nearly fully automated and can thus be scaled for use with large numbers of patients at minimal additional cost. Moreover, we compared the IBI program to a control group that received weekly printable lessons via the Internet, thus controlling for engagement with the website and ongoing attention to weight control. The clinically significant weight loss in IBI but not the control group suggests that physician advice to lose weight combined with common diet and exercise information is insufficient and that behavioral strategies and feedback are also required to produce meaningful weight loss.
In conclusion, physician referral to a behavioral Internet intervention, which includes weekly behavioral lessons and weekly automated feedback to patients on their self-monitoring records, with periodic written feedback to the physician, can be an effective approach for weight loss in overweight and obese individuals. Given that ∼80% of U.S. adults use the Internet (32,33), this approach may provide a cost-effective alternative or complement to the face-to-face counseling models of obesity treatment, including that which is currently reimbursable by the Centers for Medicare & Medicaid Services (34), and could be paired with other Internet-based resources for diabetes management and risk reduction (35). Additional translational research is needed to determine whether this intervention can be fully implemented within current health care settings and reimbursement models while preserving the positive weight-loss outcomes.
Supplementary Material
Article Information
Acknowledgments. The authors thank the study participants for their contribution to the research; the physicians for referring patients to the trial; and Pam Coward, Katelyn Gettens, and Rachel Ogilvie, The Weight Control and Diabetes Research Center of The Miriam Hospital, for assistance with study implementation.
Funding. This study was funded by a grant from the National Heart, Lung, and Blood Institute (RC1-HL-100002).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. J.G.T. researched data, conducted the statistical analysis, and cowrote the manuscript. T.M.L. contributed to the discussion and reviewed and edited the manuscript. R.R.W. researched data and cowrote the manuscript. J.G.T. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. A portion of the findings reported in this article was presented in poster form at the 30th Annual Scientific Meeting of The Obesity Society, San Antonio, TX, 20–24 September 2012.
Footnotes
Clinical trial reg. no. NCT01222858, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc14-1474/-/DC1.
A slide set summarizing this article is available online.
References
- 1.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA 2012;307:491–497 [DOI] [PubMed] [Google Scholar]
- 2.Bray GA. Obesity increases risk for diabetes. Int J Obes Relat Metab Disord 1992;16(Suppl. 4):S13–S17 [PubMed] [Google Scholar]
- 3.Kreuter MW, Chheda SG, Bull FC. How does physician advice influence patient behavior? Evidence for a priming effect. Arch Fam Med 2000;9:426–433 [DOI] [PubMed] [Google Scholar]
- 4.Eden KB, Orleans CT, Mulrow CD, Pender NJ, Teutsch SM. Does counseling by clinicians improve physical activity? A summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002;137:208–215 [DOI] [PubMed] [Google Scholar]
- 5.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA 1999;282:1576–1578 [DOI] [PubMed] [Google Scholar]
- 6.Tsai AG, Asch DA, Wadden TA. Insurance coverage for obesity treatment. J Am Diet Assoc 2006;106:1651–1655 [DOI] [PubMed] [Google Scholar]
- 7.McTigue KM, Harris R, Hemphill B, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2003;139:933–949 [DOI] [PubMed] [Google Scholar]
- 8.Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am 2011;34:841–859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diabetes Prevention Program (DPP) Research Group . The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002;25:2165–2171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knowler WC, Fowler SE, Hamman RF, et al. Diabetes Prevention Program Research Group . 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff (Millwood) 2012;31:67–75 [DOI] [PubMed] [Google Scholar]
- 12.Neve M, Morgan PJ, Jones PR, Collins CE. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev 2010;11:306–321 [DOI] [PubMed] [Google Scholar]
- 13.Thomas JG, Bond DS. Review of innovations in digital health technology to promote weight control. Curr Diab Rep 2014;14:485. [DOI] [PubMed] [Google Scholar]
- 14.Rothert K, Strecher VJ, Doyle LA, et al. Web-based weight management programs in an integrated health care setting: a randomized, controlled trial. Obesity (Silver Spring) 2006;14:266–272 [DOI] [PubMed] [Google Scholar]
- 15.McConnon A, Kirk SF, Cockroft JE, et al. The Internet for weight control in an obese sample: results of a randomised controlled trial. BMC Health Serv Res 2007;7:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McTigue KM, Conroy MB, Hess R, et al. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemed J E Health 2009;15:851–858 [DOI] [PubMed] [Google Scholar]
- 17.Bennett GG, Warner ET, Glasgow RE, et al. Be Fit, Be Well Study Investigators . Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Arch Intern Med 2012;172:565–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 2011;365:1959–1968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ma J, Yank V, Xiao L, et al. Translating the Diabetes Prevention Program lifestyle intervention for weight loss into primary care: a randomized trial. JAMA Intern Med 2013;173:113–121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med 2006;166:1620–1625 [DOI] [PubMed] [Google Scholar]
- 21.Norman GJ, Zabinski MF, Adams MA, Rosenberg DE, Yaroch AL, Atienza AA. A review of eHealth interventions for physical activity and dietary behavior change. Am J Prev Med 2007;33:336–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wadden TA, West DS, Delahanty L, et al. Look AHEAD Research Group . The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it [published correction appears in Obesity (Silver Spring) 2007;15:1339]. Obesity (Silver Spring) 2006;14:737–752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raynor HA, Jeffery RW, Ruggiero AM, Clark JM, Delahanty LM, Look AHEAD (Action for Health in Diabetes) Research Group . Weight loss strategies associated with BMI in overweight adults with type 2 diabetes at entry into the Look AHEAD (Action for Health in Diabetes) trial. Diabetes Care 2008;31:1299–1304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lachin JM. Statistical considerations in the intent-to-treat principle. Control Clin Trials 2000;21:167–189 [DOI] [PubMed] [Google Scholar]
- 25.DeMets DL, Lan KK. Interim analysis: the alpha spending function approach. Stat Med 1994;13:1341–1352; discussion 1353–1356 [DOI] [PubMed] [Google Scholar]
- 26.Wing RR, Crane MM, Thomas JG, Kumar R, Weinberg B. Improving weight loss outcomes of community interventions by incorporating behavioral strategies. Am J Public Health 2010;100:2513–2519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yoong SL, Carey M, Sanson-Fisher R, Grady A. A systematic review of behavioural weight-loss interventions involving primary-care physicians in overweight and obese primary-care patients (1999-2011). Public Health Nutr 2013;16:2083–2099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennett GG, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web-based weight loss in primary care: a randomized controlled trial. Obesity (Silver Spring) 2010;18:308–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kreuter MW, Bull FC, Clark EM, Oswald DL. Understanding how people process health information: a comparison of tailored and nontailored weight-loss materials. Health Psychol 1999;18:487–494 [DOI] [PubMed] [Google Scholar]
- 30.Saperstein SL, Atkinson NL, Gold RS. The impact of Internet use for weight loss. Obes Rev 2007;8:459–465 [DOI] [PubMed] [Google Scholar]
- 31.Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord 1992;16:397–415 [PubMed] [Google Scholar]
- 32.Duggan M, Smith A. Cell internet use 2013 [Internet], 2013. Available from http://pewinternet.org/Reports/2013/Cell-Internet.aspx. Accessed 31 July 2014
- 33.File T. Computer and Internet Use in the United States. Current Population Survey Reports. Washington, D.C., U.S. Census Bureau, 2013, p. 20–568 [Google Scholar]
- 34.Centers for Medicare & Medicaid Services. Decision memo for intensive behavioral therapy for obesity (CAG-00423N) [article online], 2013. Available from http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?&NCAId=253. Accessed 20 August 2013
- 35.Kaufman N. Internet and information technology use in treatment of diabetes. Int J Clin Pract Suppl 2010;166:41–46 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.