Abstract
Social Anxiety Disorder (SAD) is thought to be characterized by maladaptive self-views. This study investigated whether (1) patients with SAD (n=75) differ at baseline from healthy controls (HC; n=43) in negative and positive self-views, (2) Cognitive-Behavioral Therapy (CBT) for SAD vs. waitlist control (WL) produces statistically and clinically significant changes in negative and positive self-views, (3) changes in self-views mediate the effect of CBT on social anxiety symptoms, and (4) changes in self-views during CBT related to social anxiety symptoms at 1-year post-CBT. As expected, patients endorsed more negative and fewer positive self-views than HC at baseline. Compared to WL, CBT yielded statistically and clinically significant changes, specifically, fewer negative and more positive self-views. Mediational analysis indicated that increased positive (but not reduced negative) self-views mediated the effect of CBT on social anxiety reduction. Correlational analyses determined that increased positive self-views were associated with social anxiety symptom reduction at 1-year-post-CBT.
Keywords: social anxiety, self-view, self-referential, CBT, meditation
INTRODUCTION
Social anxiety disorder (SAD) is highly prevalent (with a lifetime prevalence of 12.1%) (Kessler et al., 2005), has an early onset (Otto et al., 2001), and has a high rate of persistence that is well-predicted by symptom severity and comorbid mood disorders (Blanco et al., 2011). Individuals with SAD experience distressing levels of social fear, humiliation, and embarrassment (Stein & Stein, 2008) which can lead to significant impairment in social, educational, and occupational functioning (Schneier et al., 1994; Stein & Kean, 2000), and thus create a substantial personal as well as a societal burden (Acarturk et al., 2009; Patel, Knapp, Henderson, & Baldwin, 2002).
Cognitive-behavioral models of social anxiety (Clark & Wells, 1995; Heimberg, Brozovich, & Rapee, 2010) highlight the important role played by maladaptive self-views, exaggerated self-focus, and distorted interpretations in generating and maintaining heightened social anxiety. Individuals with SAD tend to view themselves as socially awkward, inadequate, or flawed. These negative self-views are thought to trigger exaggerated self-focused attention which can lead to self-referential evaluations that generate negative emotions, disrupt emotion regulation, and interfere with social self-efficacy and performance (Spurr & Stopa, 2002).
On an intrapersonal level, Hofmann (2007) has suggested that social fears may be related to an internal discrepancy between competing self-views. The notion of multiple possible selves refers to dynamic aspects of the self-concept, including motivation, distortion, and both momentary and enduring change (Markus & Nurius, 1986). These different versions of the self are thought to vary in accessibility across time and may be modified with training. On an interpersonal level, Moscovitch, Orr, Rowa, Reimer, and Antony (2009) have argued that the core difficulty in SAD is not social situations and other’s evaluations per se, but rather aberrant views of the social self and exposing negative self-attributes to others. Stopa (2009) has identified several self-related factors that may contribute to social fears, including maladaptive self-related content (i.e., self-concepts), structure (i.e., how information about the self is stored and retrieved), and processes (i.e., how attention is allocated to self-relevant information).
Research to date has emphasized the role of negative self-views, their relationship to social fears and avoidance, their function in maintaining SAD, and their malleability during clinical treatments for SAD (Anderson, Goldin, Kurita, & Gross, 2008; Goldin, Manber-Ball, Werner, Heimberg, & Gross, 2009; Hofmann, Moscovitch, Kim, & Taylor, 2004). However, more recent theoretical models have highlighted the importance of considering positive self-views, in addition to negative self-views, in the context of SAD (Heimberg et al., 2010). Key questions raised by these newer models include (a) whether and how clinical interventions for SAD might modify negative and positive self-views, and (b) how such changes might relate to treatment outcome. When self-views are construed broadly, there are a small number of intervention studies that suggest self-views may be modified in patients with SAD following cognitive-behavioral group therapy (Hofmann, Moscovitch, Kim, & Taylor, 2004), exposure (Hofmann, 2000), video feedback with cognitive preparation (Orr & Moscovitch, 2010), and mindfulness-based stress reduction training (Goldin, Ramel, & Gross, 2009).
One particularly efficacious intervention for SAD is cognitive-behavioral therapy (CBT) which can be administered in group (Heimberg & Becker, 2002) or individual formats (Clark, 2001). Individual-CBT, as developed by Hope and colleagues (Hope, Heimberg, Juster, & Turk, 2000), has been shown to be an effective treatment for SAD (Goldin et al., in press; Ledley et al., 2009). Cognitive-behavioral models of SAD have long suggested that successful CBT for SAD should result in adaptive changes in self-views (Rapee & Heimberg, 1997). However, few studies have examined the impact of CBT on both negative and positive self-views in the context of a randomized controlled trial, or investigated whether changes in self-views mediate the effects of CBT on SAD outcomes, or relate to longer-term clinical improvement.
Our goals in the present study were to investigate whether (1) patients with SAD would differ at baseline from healthy controls in both negative and positive self-views, (2) CBT for SAD vs. random assignment to a waitlist control (WL) would produce statistically and clinically significant changes in both negative and positive self-views, (3) changes in self-views would mediate the effects of CBT on social anxiety symptom severity, and (4) changes in self-views during CBT would be related to social anxiety symptom reduction at 1-year post-CBT. We expected that, compared to healthy controls, patients with SAD would endorse more negative and fewer positive social traits as self-descriptive. Compared to WL, we expected CBT to result in fewer negative and more positive self-views, as well as clinically significant change in both negative and positive self-views compared to normative healthy control data. We expected that increases in positive and reductions in negative self-views during CBT would mediate the effect of CBT vs. WL on social anxiety symptoms. We further expected that increases in positive and reductions in negative self-views would be related to social anxiety symptom reduction at 1-year post-CBT.
METHOD
PARTICIPANTS
Patients were seeking treatment for SAD and met DSM-IV (American Psychiatric Association [APA], 1994) criteria for a principal diagnosis of generalized SAD based on the Anxiety Disorders Interview Schedule for the DSM-IV-Lifetime version (ADIS-IV-L) (DiNardo, Brown, & Barlow, 1994). In the context of a randomized controlled trial (RCT), of the 436 individuals assessed for eligibility (see Consolidated Standards of Reporting Trials diagram in Goldin et al., 2012), 110 were administered the ADIS-IV-L in person to determine whether they met diagnostic inclusion and exclusion criteria. After 35 patients were excluded due to not meeting diagnostic criteria (n=26) or incomplete baseline assessments (n=9), the remaining 75 patients were randomly assigned to either immediate CBT for SAD (n=38) or a WL control group (n=37) who were offered CBT after the waiting period. After accounting for dropout from CBT (n=6; 16%) and WL (n=5; 14%) as well as incomplete data at post-CBT (n=5) and post-WL (n=6). We also assessed 43 HC participants for comparison to patients with SAD. Participants in this study are the same participants as reported in Goldin et al., 2012 and Boden et al., 2012.
Because participants were part of a larger fMRI study, they had to pass an MR safety screen, be right-handed as assessed by the Edinburgh Handedness Inventory (Oldfield, 1971), and were excluded for current pharmacotherapy or psychotherapy, past CBT, history of neurological or cardiovascular disorders, and current psychiatric disorders other than SAD, generalized anxiety disorder, agoraphobia without a history of panic attacks, or specific phobia. Healthy controls had to have no history of Axis I psychiatric disorders as assessed by the ADIS-IV-L.
PROCEDURE
Healthy controls were recruited via electronic bulletin boards and were assessed only once. Patients were recruited for a randomized controlled trial of CBT for SAD through clinician referrals and web-based community listings. After passing a telephone screening, the ADIS-IV-L was conducted during a face-to-face interview. After completing all baseline assessments, patients were randomly assigned to immediate CBT or WL groups using Efron’s biased coin randomization procedure (Efron, 1971) which promotes approximately equal sample sizes throughout the duration of the clinical trial. Patients in the WL and CBT completed the same measures. Patients received CBT at no cost and were not paid to participate. All participants provided informed consent in accordance with the Institutional Review Board at Stanford University.
MEASURES
To measure severity of social anxiety symptoms, we used the 24-item Liebowitz Social Anxiety Scale-Self-Report (LSAS-SR; (Fresco et al., 2001; Liebowitz, 1987), which consists of questions that assess social interaction situations (11 items) and performance situations (13 items). A 4-point Likert-type scale is used for ratings of fear and of avoidance, with a range from 0 (none and never, respectively) to 3 (severe and usually, respectively) for situations during the past week. Ratings are summed for a total LSAS-SR score (range = 0–144). The LSAS-SR has good reliability and construct validity (Rytwinski et al., 2009) and its internal consistency (Cronbach’s alpha) was excellent in this study (SAD patients = .91; HC = .93).
To measure the potential confound of social desirability, we administered the 10-item Marlowe-Crowne Social Desirability Scale (MCSDS; Crowne & Marlowe, 1960). The instrument consists of true-false items with four reverse coded items, with higher scores reflecting a greater tendency to give a socially desirable response. It has shown adequate internal consistency and reliability (Crino, Svoboda, Rubenfeld, & White, 1983).
SELF-REFERENTIAL ENCODING TASK (SRET)
The SRET (Derry & Kuiper, 1981) is considered an information processing measure of self-schema. Stimuli consisted of 25 positive and 25 negative social trait adjectives from the Affective Norms of Emotion Words database (Bradley & Lang, 1999), balanced (all ps > .51) on word frequency (positive adjectives=40.5, negative adjectives=33.6), number of letters (positive adjectives=6.9, negative adjectives=7.2), arousal (positive adjectives=5.54, negative adjectives=5.43 on a scale of 1=low to 9=high), and valence (deviation from neutral: positive adjectives=2.66, negative adjectives=2.58 on a scale of 1=most negative, 5=neutral, 9=most positive) based on the 9-point Self-Assessment Manikin rating system (Lang, 1980). The SRET was programmed using Eprime software (Schneider, Eschman, & Zuccolotto, 2002) to be exactly 5 minutes and 39 seconds in length. Each adjective was presented twice, once in each of two conditions. The self-referential condition assessed self-focused social-evaluative processing. Case identification was used as a comparison condition to control for reading negative and positive adjectives while determining whether the word consisted of upper or lower case letters. Each of the four trial types (two conditions by two valences) included five blocks. Each block consisted of a fixation cross, a prompt (either “Describes ME?” or “UPPER case?”), and five adjectives of the same valence presented one at a time for 3s each. We decided not to use neutral adjectives (as a comparison condition) because there were very few that could not be misconstrued as positive or negative by a patient with SAD. Stimulus order included a random sequence of block types and a random sequence of five words within each block. Patients pressed buttons to indicate whether or not a word was self-descriptive or appeared in uppercase letters.
INDIVIDUAL-COGNITIVE-BEHAVIORAL THERAPY FOR SAD
CBT was delivered using Managing Social Anxiety: A Cognitive-Behavioral Therapy Approach, the first edition of a manualized treatment protocol which included a therapist guide (Hope, Heimberg, & Turk, 2006) and a client workbook (Hope et al., 2000) and consisted of 16 individual one-hour sessions (except for the first in-session exposure session which lasted 1.5 hours) administered over a period of 4 months. The treatment covered five major components: (1) psychoeducation and orientation to CBT; (2) cognitive restructuring skills; (3) graduated exposure to feared social situations, within session and as homework; (4) examination and modification of core beliefs; and (5) relapse prevention and termination. Further details are available elsewhere (Hope et al., 2000; Hope et al., 2006; Ledley et al., 2009).
All four study therapists had to achieve proficiency in implementing CBT with training cases prior to treating study participants. All CBT therapists were trained by and had weekly group supervision with Dr. Heimberg, an expert in CBT for SAD and one of the principal developers of the CBT protocol. To assure treatment adherence, every therapy session was digitally recorded and rated for adherence using the Cognitive-Behavioral Therapy for Social Anxiety Disorder: Therapist Adherence Scale (Hope et al., 2006), we determined that each therapist was rated as “in protocol.” For methodological details, see (Goldin et al., 2012).
STATISTICAL ANALYSES
For the baseline comparison, we conducted between-group t-tests on positive and negative self-endorsement on the SRET. For the RCT, we conducted 2 group (CBT, WL) × 2 time (pre, post) repeated-measures analysis of variance (ANOVA) of positive and negative self-endorsement to determine the effect of CBT on self-views. We report effect sizes as Cohen’s d (Cohen, 1988) and as partial eta2 (ηp2) (Pierce, Block, & Aguinis, 2004). For the RCT, we also report effect sizes as Success Rate Difference (SRD), defined as the difference between the probabilities that a randomly chosen patient from CBT will have a response preferable to a randomly chosen patient from WL. SRD ranges from +1 (if every patient treated with CBT has a clinically preferable response to every patient in the WL) to −1 (if the reverse is true) with null value = 0. If the assumptions underlying Cohen’s d apply, then SRD=2Φ(d/√2)−1, where Φ(d/√2) is the standard normal distribution function.
To analyze clinically significant change, we used the methods described by Jacobson and Truax (1991) to determine if treatment has moved a patient from the dysfunctional to functional range. Their method C (Jacobson, Roberts, Berns, & McGlinchey, 1999) uses the baseline mean and standard deviation (SD) of the clinical patient sample and a normative sample to compute a cut-off score to determine whether a post-treatment score is more typical of the normative sample than the patient sample. Specifically, this determines whether a patient has moved to the normal control side of the halfway point between 2 SDs from the patient mean and 2 SDs from the normal control group. Chi-squared analysis was conducted to determine whether the proportion of patients demonstrating clinically significant change differed following CBT and WL.
For the mediation analysis, we investigated whether changes in positive and negative self-views, separately, mediated the effect of CBT (versus WL) on social anxiety symptoms. We implemented the MacArthur approach to mediation analysis (Kraemer, Kiernan, Essex, & Kupfer, 2008), using a linear model including the main effects of treatment group (G) and mediator (M) and the G by M interaction. G, the treatment group assigned at baseline, was coded as 0.5 and −0.5. The pre-to-post change in M temporally followed G and the outcome variable (O) was measured after treatment completion. M was centered at zero (i.e., its value at baseline) to make the standardized coefficient beta values (β) more interpretable. Then we determined that G and M were correlated, and that in the linear model, either the main effect of M or the interactive effect of G by M was statistically significant. The mediator effect size is the difference between the overall effect size of G on O and the effect size if the connection between G and M were somehow severed. Only treatment completer data were used to assure temporal precedence. We used Pearson-product correlation coefficients to determine if there was an association between CBT-related changes in self-views and changes in social anxiety symptom severity from pre-to-1-year post-CBT.
RESULTS
PRELIMINARY ANALYSES
Patients with SAD and healthy controls did not differ significantly (all ps>.18) in gender, age, education, and ethnicity, and marital status (Table 1). Patients in the CBT and WL groups also did not differ in gender, age, education, ethnicity, marital status, current or past Axis I comorbidity, past psychotherapy or pharmacotherapy (all ps > .05). The two groups also reported similar age at symptom onset (Mean±SD: CBT=13.2 ±7.9 vs. WL=13.0±6.1 years of age; t=0.16) and years since symptom onset (CBT=20.4 ±11.1 vs. WL=20.3±12.9 years; t=.02).
Table 1.
Demographics of Patients with Social Anxiety Disorder and Healthy Controls
| Variable | SAD n = 75 |
HC n = 43 |
Statistical Test |
|---|---|---|---|
| Gender (Males, n, %) | 39 (52.0%) | 23 (53.4%) | χ2 = 0.07 |
| Age (years, M ± SD) | 33.5 ± 8.9 | 33.8 ± 9.8 | t = 0.21 |
| Education (years, M ± SD) | 16.8 ± 2.3 | 17.4 ± 2.0 | t =1.34 |
| Ethnicity (n, % Caucasian) | 43 (57.3%) | 25 (58.1%) | χ2 = 0.41 |
| Marital status (n, %) | χ2 = 0.78 | ||
| Single, never married | 46 (63.0%) | 21 (48.8%) | |
| Married/with partner | 24 (32.9%) | 21 (48.8%) | |
| Divorced, separated, widowed | 3 (4.1%) | 1 (2.3%) |
Note: SAD=patients with social anxiety disorder, HC=healthy controls, M=mean, SD=standard deviation. All comparisons were non-significant (p>.05).
To rule out baseline differences in self-views, between-group t-tests of patients with SAD who were randomly assigned to (but had yet to begin) CBT or WL revealed no between-group differences on self-endorsement of positive self-views (p > .18) or negative self-views (p > .37). To rule out the possibility of a social desirability response bias on self-report measures, we examined the relationship of the Marlowe-Crowne Social Desirability Scale and endorsement of self-views. In the CBT group, we found no significant relationships between the MC and baseline SRET negative (r = .15, p > .37) and positive (r = .01, p >.97) self-endorsement. Similarly, in the WL group, we found no significant relationships between the MC and baseline SRET negative (r = −.28, p > .13) and positive (r = .34, p >.07) self-endorsement.
BASELINE RESULTS FOR PATIENTS VERSUS HEALTHY CONTROLS
For positive self-views, a between-group t-test revealed that, compared to HC, patients with SAD had lesser positive self-views, SAD Mean = 43.7%, SD = 24.2 vs. HC Mean = 88.0%, SD = 12.1; t(112) = 11.15, p < .001, ηp2 = .53, Cohen’s d = 2.18, mean between-group difference = 44.3, 95% CI [36.4, 52.2]. For negative self-views, compared to HC, patients had more negative self-views, SAD Mean = 49.4%, SD = 26.5 vs. HC Mean = 3.4%, SD = 9.1; t(112) = 11.01, p < .001, ηp2 = .52, d = 2.14, mean between-group difference = 46.0, 95% CI [37.7, 54.3].
CBT VERSUS WL EFFECTS ON SELF-VIEWS
A 2 Group (CBT, WL) × 2 Valence (positive, negative) × 2 Time (pre, post) repeated-measures ANOVA of self-views resulted in a significant 3-way group by valence by time interaction effect, F(1,51) = 14.67, p <.001, ηp2 = .22, d = 1.07, and a significant interaction of group by time, F(1,51) = 15.41, p <.001, ηp2 = .23, d = 1.10.
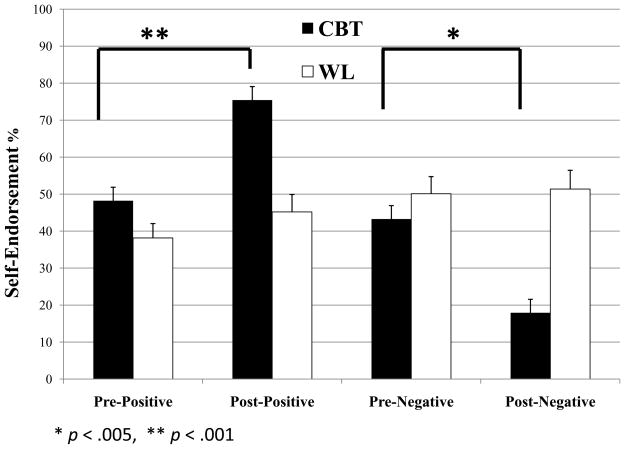
Positive Self-Views
A 2 Group (CBT, WL) × 2 Time (baseline, post) repeated-measures ANOVA on positive self-views resulted in significant effects of time, F(1,51) = 36.18, p < .001, ηp2 = .41, and group, F(1,51) = 11.17, p = .002, ηp2 = .18, qualified by a significant group by time interaction, F(2,51) = 12.21, p < .001, ηp2 = .19, d = .97, SRD = .70 (Figure 1). Follow-up paired t-tests showed pre-to-post-CBT increases in positive self-views, Δ positive self-view = 27.22; t(26) = 6.68, p < .001, ηp2 = .63, d = 2.61, mean within-group difference = 46, 95% CI [27, 65], and no change in the WL group, Δ positive self-view = 7.04; t(25) = 1.72, p > .10. For clinically significant change, the Jacobson and Truax method C determined that positive self-views > 85% was a cut-off for determining that a patient moved from dysfunctional to the functional range. Chi-squared analysis determined that, compared to WL, CBT resulted in a higher proportion of patients who achieved clinically significant change in positive self-views (CBT = 48.3% vs. WL = 10.0%; χ2 = 10.59, p < .001).
Figure 1.
Self-Endorsement Pre/Post Cognitive-Behavioral Therapy versus Waitlist Control in Patients with SAD. * p < .005, ** p < .001
Negative Self-Views
A 2 Group (CBT, WL) × 2 Time (baseline, post) repeated-measures ANOVA of negative self-views resulted in main effects of time, F(1,51) = 9.19, p = .004, ηp2 = .15, and group, F(1,51) = 14.93, p < .001, ηp2 = .23, qualified by a group by time interaction, F(2,51) = 11.19, p = .002, ηp2 = .18, d = .94, SRD = .72 (Figure 1). Follow-up paired t-tests showed CBT-related decreased negative self-views, Δ negative self-views = −25.34; t(26) = 4.97, p < .001, ηp2 = .49, d = 1.39, and no change in WL group, Δ negative self-views = 1.25; t(25) = .20, p > .84. For clinically significant change, the Jacobson and Truax method C determined that negative self-views < 6% was a cut-off for determining that a patient moved from dysfunctional to the functional range. Chi-squared analysis determined that, compared to WL, CBT resulted in a higher proportion of patients who achieved clinically significant change (CBT = 31.0% vs. WL = 3.0%; χ2 = 25.78, p < .001).
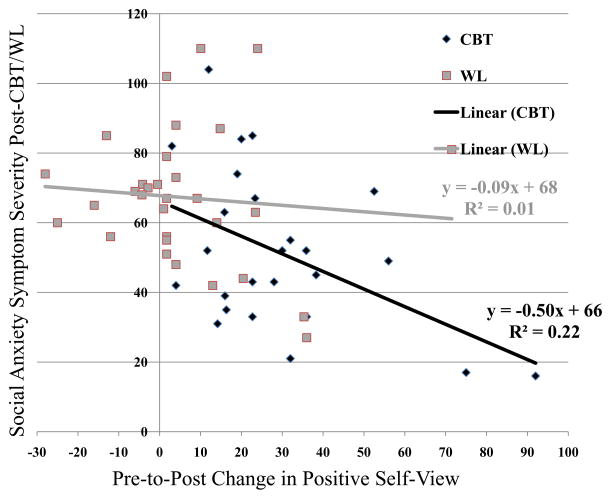
SELF-VIEWS MEDIATION OF EFFECTS OF CBT ON SOCIAL ANXIETY
As shown above, group assignment (G) at baseline to CBT vs. WL was associated with differential change in positive and negative self-views satisfying the first criterion for showing mediation. For positive self-views, the linear regression (F(3,50) = 5.24, p = .003, R2 = .23) demonstrated a main effect of M (pre-to-post change in positive self-endorsement), but no interaction of GxM on post-CBT/WL social anxiety symptoms (LSAS-SR) (Table 2, Figure 2). Thus the final criterion for mediation is satisfied. Moreover, the treatment effect on change in social anxiety, shown significant when positive self-views was ignored above, is now non-significant, indicating complete mediation. For negative self-views, the linear regression (F(3,50) = 4.49, p = .007, R2 = .20) demonstrated neither a main effect of M (p > .10) or an interaction of GxM (p > .66).
Table 2.
Change in Positive Self-Views Mediates the Effect of Cognitive-Behavioral Therapy on the Severity of Social Anxiety Symptoms
| Unstandardized Coefficient b | SE b | Standardized Coefficient β | p-value | |
|---|---|---|---|---|
| LSAS-SR | ||||
| - Intercept | 67.01 | 3.95 | ||
| - Group | −1.55 | 7.89 | −.035 | .85 |
| - Positive Self-Views | −.30 | .14 | −.31 | .03 |
| - Group × Positive Self-Views | −.41 | .27 | −.25 | .14 |
Note. LSAS-SR = Liebowitz Social Anxiety Scale Self-Report, SE = standard error
Figure 2.
Association of Pre-to-Post Changes in Positive Self-Endorsement and Post-CBT/WL Social Anxiety Symptom Severity
To investigate the specificity of the above findings, we tested whether changes in social anxiety symptoms mediated the effect of CBT on positive self-views. For positive self-views, the linear regression (F(3,50) = 10.19, p < .001, R2 = .39) showed only partial mediation characterized by a main effect of M (pre-to-post change in social anxiety symptoms; standardized coefficient beta = −.36, p = .026) and also a main effect of G (treatment group; standardized coefficient beta = .59, p = .003). Thus, the mediator did not reduce the effect of treatment group to non-significance. For negative self-views, the linear regression, F(3,50) = 8.49, p < .001, R2 = .32, demonstrated neither a main effect of M (p > .06) or an interaction of GxM (p > .43).
CBT-RELATED CHANGES IN SELF-VIEWS AND LONG-TERM OUTCOME
We also examined whether pre-to-post-CBT changes in self-views were related to pre-to-1-year post-CBT changes in social anxiety symptoms. We found that increased positive self-views were associated with decreased severity of social anxiety symptoms (LSAS-SR) at 1-year post-CBT, r(32) = −.35, p < .05. Decreased negative self-views, however, were not associated with decreased severity of social anxiety symptoms at 1-year post-CBT, r(32)=.20, p > .27.
DISCUSSION
This study found that CBT reduced negative and increased positive self-views, and that increased positive (but not reduced negative) self-views mediated the effect of CBT on social anxiety symptom reduction, as well as predicted social anxiety symptom reduction at immediate and 1-year-post-CBT.
As expected, compared to HC, patients with SAD at baseline showed a maladaptive profile of self-views characterized by few positive and many negative self-endorsements. This pattern converges with prior reports of maladaptive self-views in SAD (Goldin et al., 2009; Hofmann et al., 2004) and more generally with self-critical cognitive styles that reflect a fundamental cognitive diathesis in anxiety and mood disorders (Moscovitch, Hofmann, Suvak, & In-Albon, 2005). Importantly, the effect size for differential positive (ηp2 = .53) and negative (ηp2 = .52) self-views in patients with SAD versus non-anxious healthy controls showed an equivalent degree of distortion. This means that individuals with SAD have both fewer positive and more negative self-views than non-clinical individuals.
Compared to WL, CBT resulted in significant enhancement of positive and reduction of negative self-views (pre-to-post-CBT change in self-endorsement: positive = 27% and negative = −25%). This indicates that CBT impacts not only negative, but also positive self-concepts. However, when viewed through the lens of clinically significant change, CBT was more effective in moving positive self-views (48%) than negative self-views (31%) into the normative range.
Prior RCTs of clinical treatments have examined negative, but not positive, self-referential thoughts and self-views (Hofmann et al., 2004). The present findings add to our understanding of the effects of CBT for SAD, suggesting that cognitive restructuring and exposure to feared social situations modifies at least two different aspect of self-processing (positive and negative self-views), but that the impact on positive self-views may be more clinically meaningful than previously considered. Moscovitch and colleagues (2009) found that positive self-views (based on ratings of 13 self-attribute dimensions) were related to higher levels of certainty and importance in healthy controls. It may be the case that as patients with SAD shift after CBT into the normative range for positive self-views, they, like healthy controls, regard these positive self-views as more definitive and relevant to their well-being (than the changes in negative self-views). If so, this suggests that changes in positive self-views may be even more meaningful and impactful than changes in negative self-views.
Mediators of treatment outcome for SAD have begun to be identified. These include decreases in probability bias for negative social events (Smits, Rosenfield, McDonald, & Telch, 2006), self-focus, estimated probability and estimated cost of negative social events, safety behaviors (Hoffart, Borge, Sexton, & Clark, 2009), anticipated aversive social outcomes (Hofmann, 2004), interpersonal core beliefs (Boden et al., 2012), and increases in cognitive reappraisal self-efficacy (Goldin et al., 2012). The present study adds to our understanding of the mechanisms of change in CBT by demonstrating that changes in positive (but not negative) self-views fully mediated the effect of CBT on reduction of social anxiety symptom severity.
Mediator specificity was indicated by (a) an increase in positive self-view from pre-to-post-CBT and no change from pre-to-post-WL, (b) no evidence that changes in negative self-views mediated the effect of CBT on social anxiety symptoms, (c) no evidence that changes in social anxiety symptoms or the interaction of treatment group by changes in social anxiety fully mediated the effect of CBT on positive or negative self-views, and (d) pre-to post-CBT changes in positive (but not negative) self-views being associated with reduced social anxiety symptom severity immediately after CBT and at 1-year post-CBT. These results highlight the clinical significance of enhancement of positive self-views (and not just reduction in negative self-views) during CBT and suggest different functions for negative and positive self-views in SAD.
These findings highlight the importance of assessing self-views in SAD and investigating how self-views are modified by CBT (and other clinical interventions). Understanding the rate of change in self-views during treatment might elucidate specific subgroups of patients with SAD. For example, there might be subgroups who fail to show significant enhancement in positive self-views which might lead clinicians to modify a portion of their interventions to specifically focus on this domain of self-views. This could be as simple as having patients specifically reflect after each fear exposure on positive self-attributes and describe them verbally or in writing to elucidate and reinforce positive self-views. This might be very valuable information for both the clinician and client to record and track over time. It might also be important for clinicians to help patients understand that positive and negative self-views may change at different rates during treatment. Furthermore, a more nuanced appreciation of self-views may facilitate the effectiveness of cognitive restructuring during exposure. Additionally, it will be important to determine whether and how group experience facilitates changes in positive and negative self-views, morale, and behavior.
The use of multiple assessments of self-views during treatment (both inside and outside of therapy sessions) could be used to explicitly direct attention in patients to their own self-concepts, especially in patients who do not regularly engage in self-reflection, and to notice when and where specific self-views are most likely to occur and how they influence social functioning. An additional benefit of multiple assessments of self-views is to increase the probability that changes in self-views occur and are observed by the patient. This may serve as a basis for the patient to experience a potentially profound insight, namely, that self-views are indeed malleable and transient. Such a reappraisal of the nature of self-views may lead to greater psychological flexibility, enhanced perspective taking, and increased expectancy for a positive treatment outcome.
Surprisingly, the findings in this study suggest that enhancement of positive self-views during CBT may be even more important than reducing negative self-views in patients with SAD. This is evidenced by greater clinically significant change in positive self-views, its role as a mediator of CBT, and its relationship to longer-term CBT-related improvement in social anxiety symptom severity. If this finding is replicated, then it will be important to develop a better understanding of the factors that promote changes in positive self-views. Equipped with this knowledge, it may be possible to modify CBT for SAD in ways that explicitly and implicitly increase positive self-views. For example, it might be helpful to introduce patients to a more complex and comprehensive notion of self-views. Specifically, this could entail elucidating that positive and negative self-views reflect different aspects of the self, that they might change at different rates, have different functions, and be related to treatment outcome in different ways. One way to enhance awareness of self-views is to have patients briefly rate positive and negative self-views at the beginning and end of therapy sessions, as well as before and after in vivo social interactions and exposures. Increasing our understanding of the specific profiles of adaptive and maladaptive self-views, and how they change with treatment in patients with SAD may lead to refined classification of individual differences in patients, help direct case conceptualization, and promote a more customized delivery of CBT for SAD.
The current study was focused on how patients with SAD viewed themselves and how CBT impacted those self-views. As our understanding of the specific mechanisms underlying clinically meaningful changes in self-views develops, it will be possible to more precisely test the role of purported mechanisms in carefully tailored randomized controlled trials that enroll participants with a broader range of clinical symptoms than current-generation disorder-specific studies. For example, future randomized controlled trials might employ a temporally fine-grained, multi-dimensional assessment approach in a sample characterized by a broader range of affective disturbances. Specifically, randomized controlled trials might include random assignment to three arms: group CBT, a comparison treatment with a proposed mechanism of change that differs from CBT (e.g., a specific pharmacological intervention such as paroxetine or sertraline, or non-cognitive psychological intervention such as group Acceptance and Commitment Therapy), and a waitlist control to account for habituation to study procedures. To more fully capture changes in symptoms over time, online (e.g., smart-phone delivered) self-report and cognitive assessments could be administered throughout treatment and for 1-year post-treatment completion. These assessments would measure clinical symptoms as well as previously identified mediators of treatment change. Such studies might employ a multi-dimensional neuroimaging approach including, (a) combined fMRI BOLD and EEG assessment of self-views and cognitive reappraisal at baseline, post-treatment, and at 1-year post-treatment, and (b) daily smartphone delivered social fear exposure assessment of self- and other-beliefs, subjective distress, and cognitive reappraisal. This measurement approach would allow for an examination of the temporal dynamics of change in potential mediators (i.e., mechanisms of change) and how they relate to each other (i.e., temporally-interrelated multiple mechanisms of change) during treatment and follow-up.
Future clinical intervention studies should also be designed to address one of the biggest puzzles today, namely the question of who benefits from which type of treatment. This is the issue of treatment matching. In contrast to identifying underlying mechanisms of change (i.e., mediators of treatment response) that can enhance the effectiveness of specific interventions, the identification of individual or combinations of features of patients present prior to treatment that predict treatment response (i.e., moderators) is essential for the scientific advancement of the clinical treatment of psychological disorders. This entails recruitment of much larger sample sizes that require large multi-site studies. While the ever advancing technology to conduct such large-scale studies is in place now, what is urgently needed is an increased spirit of cooperation and collaboration across investigators, laboratories, and institutions (as well as financial and academic reward contingencies) that support and promote such efforts.
Acknowledgments
This research was supported by an NIMH Grant R01 MH076074, awarded to James Gross, Ph.D. Richard Heimberg, Ph.D. is the author of the commercially available CBT protocol which was utilized in this study.
Footnotes
ClinicalTrials.gov identifier: NCT00380731; http://www.clinicaltrials.gov/ct2/show/NCT00380731?term=social+anxiety+cognitive+behavioral+therapy+Stanford&rank=1
None of the authors of this manuscript have any biomedical financial interests or potential conflicts of interest. Philippe Goldin, Ph.D., who is independent of any commercial funder, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Acarturk C, Smit F, de Graaf R, van Straten A, ten Have M, Cuijpers P. Economic costs of social phobia: A population-based study. Journal of Affective Disorders. 2009;115:421–429. doi: 10.1016/j.jad.2008.10.008. [DOI] [PubMed] [Google Scholar]
- Anderson B, Goldin PR, Kurita K, Gross JJ. Self-representation in social anxiety disorder: linguistic analysis of autobiographical narratives. Behaviora Research and Therapy. 2008;46:1119–1125. doi: 10.1016/j.brat.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association, A. P. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Blanco C, Xu Y, Schneier FR, Okuda M, Liu SM, Heimberg RG. Predictors of persistence of social anxiety disorder: a national study. Journal of Psychiatric Research. 2011;45:1557–1563. doi: 10.1016/j.jpsychires.2011.08.004. [DOI] [PubMed] [Google Scholar]
- Boden MT, John OP, Goldin PR, Werner K, Heimberg RG, Gross JJ. The role of maladaptive beliefs in cognitive-behavioral therapy: Evidence from social anxiety disorder. Behaviour Research and Therapy. 2012;50:287–291. doi: 10.1016/j.brat.2012.02.007. http://dx.doi.org/10.1016/j.brat.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley MM, Lang PJ. Affective Norms for English Words (ANEW) Technical Manual and Affective Ratings. Gainsville, FL: Center for Research in Psychophysiology, University of Florida; 1999. [Google Scholar]
- Clark DM. A cognitive perspective on social phobia. In: Crozier WR, Alden LE, editors. International handbook of social anxiety. Chichester, England: Wiley; 2001. pp. 405–430. [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. New York, NY: Guilford Press; 1995. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Crino MD, Svoboda M, Rubenfeld S, White MC. Data on the Marlowe-Crowne and Edwards Social Desirability Scales. Psychological Reports. 1983;53:963–968. doi: 10.2466/pr0.1983.53.3.963. [DOI] [Google Scholar]
- Crowne D, Marlowe D. A new scale of social desirability independent of psychopathology. Journal of Consulting Psychology. 1960;24:349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- Derry PA, Kuiper NA. Schematic processing and self-reference in clinical depression. Journal of Abnormal Psychology. 1981;90:286–297. doi: 10.1037//0021-843X.90.4.286. [DOI] [PubMed] [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L) New York, NY: Oxford University Press; 1994. [Google Scholar]
- Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–417. doi: 10.1093/biomet/58.3.403. [DOI] [Google Scholar]
- Fresco DM, Coles ME, Heimberg RG, Liebowitz MR, Hami S, Stein MB, Goetz D. The Liebowitz Social Anxiety Scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychological Medicine. 2001;31:1025–1035. doi: 10.1017/S0033291701004056. [DOI] [PubMed] [Google Scholar]
- Goldin PR, Manber-Ball T, Werner K, Heimberg R, Gross JJ. Neural mechanisms of cognitive reappraisal of negative self-beliefs in social anxiety disorder. Biological Psychiatry. 2009;66:1091–1099. doi: 10.1016/j.biopsych.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ramel W, Gross JJ. Mindfulness meditation training and self-referential processing in social anxiety disorder: Behavioral and neural effects. Journal of Cognitive Psychotherapy. 2009;23:242–256. doi: 10.1891/0889-8391.23.3.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, Ziv M, Jazaieri H, Werner K, Kraemer H, Heimberg RG, Gross JJ. Cognitive reappraisal self-efficacy mediates the effects of individual cognitive-behavioral therapy for social anxiety disorder. Journal of Consulting and Clinical Psychology. 2012 doi: 10.1037/a0028555. Epub ahead of press http://dx.doi.org/10.1037/a0028555. [DOI] [PMC free article] [PubMed]
- Heimberg RG, Becker RE. Cognitive-behavioral group therapy for social phobia: Basic mechanisms and clinical strategies. New York: Guilford Press; 2002. [Google Scholar]
- Heimberg RG, Brozovich FA, Rapee RM. A cognitive-behavioral model of social anxiety disorder: Update and extension. In: Hofmann SG, DiBartolo PM, editors. Social anxiety: Clinical, developmental, and social perspectives. 2. New York: Academic Press; 2010. pp. 395–422. [Google Scholar]
- Hoffart A, Borge FM, Sexton H, Clark DM. Change processes in residential cognitive and interpersonal psychotherapy for social phobia: a process-outcome study. Behavior Therapy. 2009;40:10–22. doi: 10.1016/j.beth.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Self-focused attention before and after treatment of social phobia. Behavioral Research and Therapy. 2000;38:717–725. doi: 10.1016/S0005-7967(99)00105-9. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive mediation of treatment change in social phobia. Journal of Consulting and Clinical Psychology. 2004;72:393–399. doi: 10.1037/0022-006X.72.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG. Cognitive factors that maintain social anxiety disorder: a comprehensive model and its treatment implications. Cognitive Behavior and Therapy. 2007;36:193–209. doi: 10.1080/16506070701421313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Moscovitch DA, Kim HJ, Taylor AN. Changes in self-perception during treatment of social phobia. Journal of Consulting and Clinical Psychology. 2004;72:588–596. doi: 10.1037/0022-006X.72.4.588. [DOI] [PubMed] [Google Scholar]
- Hope DA, Heimberg RG, Juster HR, Turk CL. Managing social anxiety: A cognitive-behavioral approach. San Antonio, TX: The Psychological Corp; 2000. [Google Scholar]
- Hope DA, Heimberg RG, Turk CL. Therapist guide for managing social anxiety: A cognitive-behavioral therapy approach. New York: Oxford University Press; 2006. [Google Scholar]
- Jacobson NS, Roberts LJ, Berns SB, McGlinchey JB. Methods for defining and determining the clinical significance of treatment effects: Description, application, and alternatives. Journal of Consulting and Clinical Psychology. 1999;67:300. doi: 10.1037/0022-006X.67.3.300. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12. doi: 10.1037/0022-006X.59.1.12. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and Why Criteria Defining Moderators and Mediators Differ Between the Baron & Kenny and MacArthur Approaches. Health Psychology. 2008;27:S101–S108. doi: 10.1037/0278-6133.27.2(Suppl.).S101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang PJ. Behavioral treatment and bio-behavioral assessment: Computer applications. In: Sidowski JB, Johnson JH, Williams TA, editors. Technology in mental health care delivery. Norwood: Ablex Publishing; 1980. pp. 119–137. [Google Scholar]
- Ledley DR, Heimberg RG, Hope DA, Hayes SA, Zaider TI, Dyke MV, Fresco DM. Efficacy of a manualized and workbook-driven individual treatment for social anxiety disorder. Behavior Therapy. 2009;40:414–424. doi: 10.1016/j.beth.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Liebowitz MR. Social phobia. Modern Problems of Pharmacopsychiatry. 1987;22:141–173. doi: 10.1159/000414022. [DOI] [PubMed] [Google Scholar]
- Markus H, Nurius P. Possible Selves. American Psychologist. 1986;41:954–969. doi: 10.1037/0003-066X.41.9.954. [DOI] [Google Scholar]
- Moscovitch DA, Hofmann SG, Suvak MK, In-Albon T. Mediation of changes in anxiety and depression during treatment of social phobia. Journal of Consulting and Clinical Psychology. 2005;73:945. doi: 10.1037/0022-006X.73.5.945. [DOI] [PubMed] [Google Scholar]
- Moscovitch DA, Orr E, Rowa K, Reimer SG, Antony MM. In the absence of rose-colored glasses: ratings of self-attributes and their differential certainty and importance across multiple dimensions in social phobia. Behavior Research and Therapy. 2009;47:66–70. doi: 10.1016/j.brat.2008.10.007. [DOI] [PubMed] [Google Scholar]
- Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- Orr EM, Moscovitch DA. Learning to re-appraise the self during video feedback for social anxiety: Does depth of processing matter? Behavior Research and Therapy. 2010;48:728–737. doi: 10.1016/j.brat.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Maki KM, Gould RA, Worthington JJ, 3rd, Smoller JW, Rosenbaum JF. Childhood history of anxiety disorders among adults with social phobia: Rates, correlates, and comparisons with patients with panic disorder. Depression and Anxiety. 2001;14:209–213. doi: 10.1002/da.1068. [DOI] [PubMed] [Google Scholar]
- Patel A, Knapp M, Henderson J, Baldwin D. The economic consequences of social phobia. Journal of Affective Disorders. 2002;68:221. doi: 10.1016/S0165-0327(00)00323-2. [DOI] [PubMed] [Google Scholar]
- Pierce CA, Block RA, Aguinis H. Cautionary note on reporting eta-squared values from multifactor ANOVA designs. Educational and Psychological Measurement. 2004;64:916–924. doi: 10.1177/0013164404264848. [DOI] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35:741–756. doi: 10.1016/S0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Fresco DM, Heimberg RG, Coles ME, Liebowitz MR, Cissell S, Hofmann SG. Screening for social anxiety disorder with the self-report version of the Liebowitz Social Anxiety Scale. Depression and Anxiety. 2009;26:34–38. doi: 10.1002/da.20503. [DOI] [PubMed] [Google Scholar]
- Schneider W, Eschman A, Zuccolotto A. E-Prime User’s Guide. Pittsburgh: Psychology Software Tools, Inc; 2002. [Google Scholar]
- Schneier FR, Heckelman LR, Garfinkel R, Campeas R, Fallon BA, Gitow A, Liebowitz MR. Functional impairment in social phobia. Journal of Clinical Psychiatry. 1994;55:322–331. [PubMed] [Google Scholar]
- Smits JAJ, Rosenfield D, McDonald R, Telch MJ. Cognitive mechanisms of social anxiety reduction: An examination of specificity and temporality. Journal of Consulting and Clinical Psychology. 2006;74:1203. doi: 10.1037/0022-006X.74.6.1203. [DOI] [PubMed] [Google Scholar]
- Spurr JM, Stopa L. Self-focused attention in social phobia and social anxiety. Clinical Psychology Review. 2002;22:947–975. doi: 10.1016/S0272-7358(02)00107-1. [DOI] [PubMed] [Google Scholar]
- Stein MB, Kean YM. Disability and quality of life in social phobia: Epidemiologic findings. American Journal of Psychiatry. 2000;157:1606–1613. doi: 10.1176/appi.ajp.157.10.1606. [DOI] [PubMed] [Google Scholar]
- Stein MB, Stein DJ. Social anxiety disorder. Lancet. 2008;371:1115–1125. doi: 10.1016/S0140-6736(08)60488-2. [DOI] [PubMed] [Google Scholar]
- Stopa L. Why is the self important in understanding and treating social phobia? Cognitive Behaviour Therapy. 2009;38:48–54. doi: 10.1080/16506070902980737. [DOI] [PubMed] [Google Scholar]