Cardiovascular disease (CVD), particularly coronary vascular disease, is a primary contributor to diabetes-related morbidity and mortality worldwide. Specifically, dysfunction of coronary microcirculation is common in this patient population, often occurring in the absence of or preceding epicardial coronary atherosclerosis, thereby leading to impaired coronary blood flow (CBF) regulation and increased risk of myocardial ischemia/infarct. Clinically, coronary microvascular function can be assessed by determination of coronary flow reserve (CFR) (ratio of maximal hyperemic to basal CBF), and impaired CFR is a powerful independent correlate of cardiac mortality in diabetic patients (1). Importantly, recent evidence revealed that diabetic patients with preserved CFR (above the median) have cardiac event rates similar to nondiabetic patients (1). Thus, treatment strategies designed to restore CFR (i.e., coronary microvascular function) hold promise to reduce acute and long-term cardiac mortality in patients with diabetes.
Diabetes is associated with increased activation of the renin-angiotensin-aldosterone system (RAAS), and evidence suggests that the aldosterone-binding mineralocorticoid receptor (MR) contributes to obesity and diabetes-related vascular dysfunction (2,3). Even modest elevations in circulating aldosterone levels correlate with increased acute ischemic events and cardiovascular death in diabetic patients with coronary artery disease (4). Furthermore, accumulating evidence demonstrates that inhibition of angiotensin II (AngII) action, via ACE inhibition or angiotensin receptor blockade (ARB), does not appreciably lower circulating aldosterone levels, suggesting a residual role for MR activation in CVD pathogenesis (5). This is consistent with initial clinical trials demonstrating reduced mortality with MR antagonist treatment in heart failure patients already receiving ACE inhibitors or ARBs (6,7). Increased and persistent MR activation is likely even more pertinent in obesity and diabetes due to increased production of aldosterone and aldosterone secretagogues by adipose tissue (8,9). These data highlight the potential of MR antagonists to confer cardiovascular protection above that provided by standard ACE inhibition and ARB therapy in obesity and diabetes.
In this issue of Diabetes, Garg et al. (10) specifically addressed the clinical utility of interrupting the RAAS in a double-blind, randomized, controlled study of well-controlled diabetic patients without ischemic heart disease. Specifically, CFR derived from quantitative positron emission tomography was assessed in 64 men and women with diabetes before and after 6-month treatment with an ACE inhibitor (enalapril) combined with the MR antagonist spironolactone compared with treatment with enalapril plus hydrochlorothiazide (matching the blood pressure−lowering effect of spironolactone). An enalapril plus placebo group was also included. Results demonstrate that the addition of spironolactone to enalapril improved CFR, extending a previous crossover design study by this group showing that 6-week treatment with enalapril plus the MR antagonist eplerenone increased CFR in a smaller cohort of diabetic patients (11). Moreover, in the current study, the increase in CFR with spironolactone occurred absent of changes in systemic metabolic and lipid parameters and cardiac function, mass, and extracellular volume and remained significant after controlling for baseline CFR, change in BMI, race, and statin use. In conjunction with the lack of increased CFR following hydrochlorothiazide treatment, these results support a blood pressure−independent effect of spironolactone to improve coronary microvascular function in diabetes, presumably via its action on MR within the coronary vascular wall.
While the study by Garg et al. (10) did not include long-term follow-up to determine whether improved CFR leads to reduced cardiovascular event rates in diabetic patients, it does provide important insight into the relationship of AngII and the MR (Fig. 1). A major strength of this study is the use of the ACE inhibitor enalapril in combination with spironolactone as ACE inhibitors themselves, unlike ARBs, improve CFR in patients with diabetes (12,13). Therefore, we can speculate that the improved CFR following spironolactone was additive to that already present due to ACE inhibition, although the latter was not determined during the run-in portion of the current study. Furthermore, as AngII-dependent activation of coronary vascular smooth muscle MR in vitro has been previously reported (14), a portion of the benefit of ACE inhibition on CFR may result from reduced AngII action via the MR. However, the study by Jaffe and Mendelsohn (14) demonstrated that AngII activation of the MR is inhibited by ARB treatment, suggesting complex interactions underlying the discrepancy of the CFR benefit in ACE inhibition versus ARBs in diabetes. Further studies are necessary to directly evaluate the pre- and posttreatment effects of ACE inhibition with and without MR blockade on coronary function in diabetes. Regardless, the current study supports combination ACE/MR inhibition as a powerful therapy to improve CFR in patients with diabetes.
Figure 1.
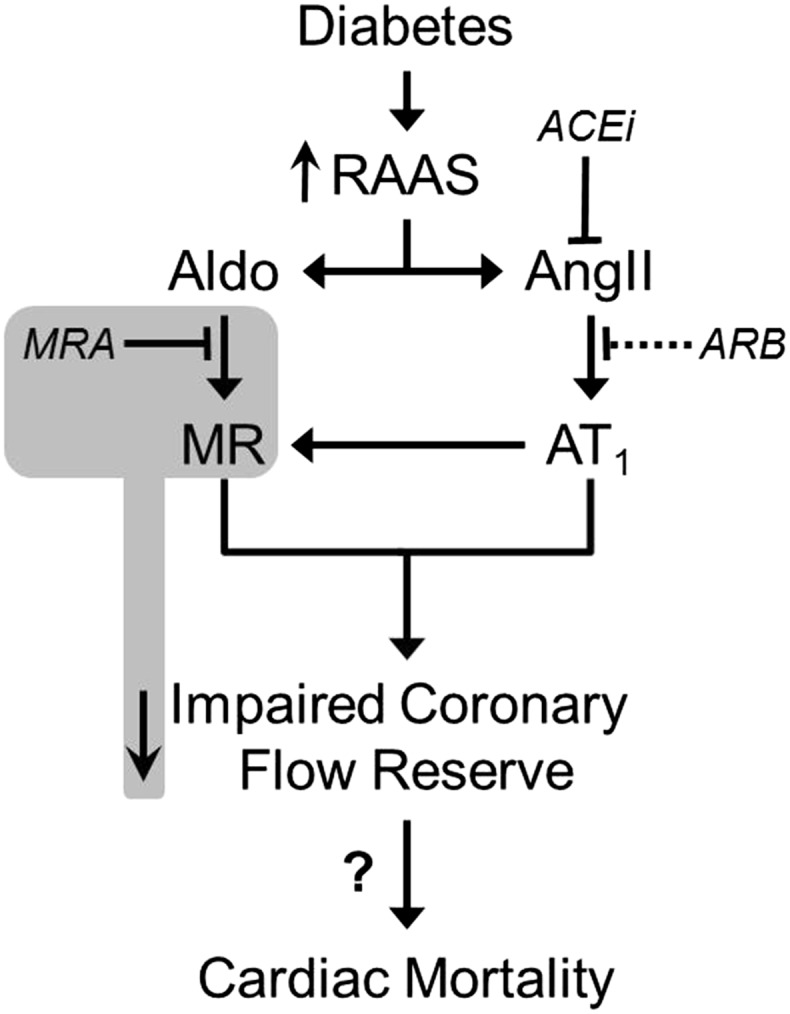
Diabetes-related impairment of CFR is improved by certain inhibitors of RAAS. Increased RAAS activation in diabetes impairs CFR, and this impairment can be reduced by MR antagonists (MRA) (gray box; reported in Garg et al. [10]) and ACE inhibitors (ACEi), but not ARBs. The effect of these antagonists on long-term cardiac mortality in patients with diabetes remains unclear. Solid lines indicate effective treatment options; dashed lines indicate ineffective treatment options. Aldo, aldosterone; AT1, AngII receptor, type 1.
It should be noted that the study population examined included both men (∼63%) and women (∼37%) and, unfortunately, is likely underpowered to examine for distinct sex differences. Future studies should evaluate whether there are differential female/male benefits for MR-related therapies in light of recent evidence. In particular, recent analysis of the Women’s Ischemia Syndrome Evaluation (WISE) trial revealed that adding eplerenone to ACE inhibition did not improve coronary endothelial function or CFR in women with symptoms of ischemia but without obstructive coronary artery disease (15). Furthermore, direct inhibition of MR-dependent proinflammatory gene expression by estrogen-bound estrogen receptor α was recently reported as demonstrating a novel mechanism of protection for premenopausal women from deleterious vascular MR signaling and subsequent CVD (16).
Finally, the study by Garg et al. (10) adds to accumulating data suggesting a distinct role for vascular MR as a mediator of coronary, but not peripheral, vascular dysfunction in patients with obesity and diabetes. Indeed, an earlier study from this group demonstrated no increase in brachial artery flow-mediated dilation following ACE/MR inhibition in the same patients exhibiting increased CFR (11). Several recent studies also report no benefit of MR blockade on peripheral flow-mediated dilation in obese patients (17,18). The basis for this discrepancy remains unclear but may be a consequence of the unique developmental origins of coronary vascular cells (19).
In summary, the study by Garg et al. (10) presents important evidence in diabetic patients of an additive benefit of ACE/MR inhibition to improve CFR. Ongoing studies should focus on delineating the cell type−specific deleterious effects of coronary vascular MR signaling and whether MR blockade improves coronary responses to (patho)physiologic perturbations (i.e., metabolic and ischemic dilation), particularly in obesity and diabetes.
Article Information
Acknowledgments. The authors would like to thank Brenda Hunter for her editorial assistance.
Funding. The research of the authors is supported by funding from the National Institutes of Health (R01-HL73101and R01-HL107910 to J.R.S.) and the Department of Veterans Affairs Biomedical Laboratory Research and Development Merit (0018 to J.R.S.) and Career Development Award-2 (IK2 BX002030 to S.B.B.). This work was supported with resources and the use of facilities at the Harry S. Truman Memorial Veterans Hospital in Columbia, MO.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying article, p. 236.
References
- 1.Murthy VL, Naya M, Foster CR, et al. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation 2012;126:1858–1868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bender SB, McGraw AP, Jaffe IZ, Sowers JR. Mineralocorticoid receptor-mediated vascular insulin resistance: an early contributor to diabetes-related vascular disease? Diabetes 2013;62:313–319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schäfer N, Lohmann C, Winnik S, et al. Endothelial mineralocorticoid receptor activation mediates endothelial dysfunction in diet-induced obesity. Eur Heart J 2013;34:3515–3524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ivanes F, Susen S, Mouquet F, et al. Aldosterone, mortality, and acute ischaemic events in coronary artery disease patients outside the setting of acute myocardial infarction or heart failure. Eur Heart J 2012;33:191–202 [DOI] [PubMed] [Google Scholar]
- 5.Messaoudi S, Azibani F, Delcayre C, Jaisser F. Aldosterone, mineralocorticoid receptor, and heart failure. Mol Cell Endocrinol 2012;350:266–272 [DOI] [PubMed] [Google Scholar]
- 6.Pitt B, Remme W, Zannad F, et al. Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival Study Investigators . Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003;348:1309–1321 [DOI] [PubMed] [Google Scholar]
- 7.Pitt B, Zannad F, Remme WJ, et al. Randomized Aldactone Evaluation Study Investigators . The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med 1999;341:709–717 [DOI] [PubMed] [Google Scholar]
- 8.Jeon JH, Kim KY, Kim JH, et al. A novel adipokine CTRP1 stimulates aldosterone production. FASEB J 2008;22:1502–1511 [DOI] [PubMed] [Google Scholar]
- 9.Briones AM, Nguyen Dinh Cat A, Callera GE, et al. Adipocytes produce aldosterone through calcineurin-dependent signaling pathways: implications in diabetes mellitus-associated obesity and vascular dysfunction. Hypertension 2012;59:1069–1078 [DOI] [PubMed] [Google Scholar]
- 10.Garg R, Rao AD, Baimas-George M, et al. Mineralocorticoid receptor blockade improves coronary microvascular function in individuals with type 2 diabetes. Diabetes 2015;64:236−242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joffe HV, Kwong RY, Gerhard-Herman MD, Rice C, Feldman K, Adler GK. Beneficial effects of eplerenone versus hydrochlorothiazide on coronary circulatory function in patients with diabetes mellitus. J Clin Endocrinol Metab 2007;92:2552–2558 [DOI] [PubMed] [Google Scholar]
- 12.Kawata T, Daimon M, Hasegawa R, et al. Effect on coronary flow velocity reserve in patients with type 2 diabetes mellitus: comparison between angiotensin-converting enzyme inhibitor and angiotensin II type 1 receptor antagonist. Am Heart J 2006;151:798.e9−e15 [DOI] [PubMed]
- 13.Kjaer A, Kristoffersen US, Tarnow L, Parving H-H, Hesse B. Short-term oral treatment with the angiotensin II receptor antagonist losartan does not improve coronary vasomotor function in asymptomatic type 2 diabetes patients. Diabetes Res Clin Pract 2009;84:34–38 [DOI] [PubMed] [Google Scholar]
- 14.Jaffe IZ, Mendelsohn ME. Angiotensin II and aldosterone regulate gene transcription via functional mineralocortocoid receptors in human coronary artery smooth muscle cells. Circ Res 2005;96:643–650 [DOI] [PubMed] [Google Scholar]
- 15.Bavry AA, Handberg EM, Huo T, et al. Aldosterone inhibition and coronary endothelial function in women without obstructive coronary artery disease: an ancillary study of the National Heart, Lung, and Blood Institute-sponsored Women’s Ischemia Syndrome Evaluation. Am Heart J 2014;167:826–832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mueller KB, Lu Q, Mohammad NN, et al. Estrogen receptor inhibits mineralocorticoid receptor transcriptional regulatory function. Endocrinology. 22 July 2014 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 17.Garg R, Kneen L, Williams GH, Adler GK. Effect of mineralocorticoid receptor antagonist on insulin resistance and endothelial function in obese subjects. Diabetes Obes Metab 2014;16:268–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hwang MH, Yoo JK, Luttrell M, et al. Mineralocorticoid receptors modulate vascular endothelial function in human obesity. Clin Sci (Lond) 2013;125:513–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tomanek RJ. Formation of the coronary vasculature during development. Angiogenesis 2005;8:273–284 [DOI] [PubMed] [Google Scholar]


