Abstract
Objective
To examine the association between marital interaction quality during daily life and subclinical cardiovascular disease (CVD). Studies have shown that marital status and quality of marriage are associated with cardiovascular health. However, little is known about the role of marital interaction quality during daily life in contributing to these effects.
Methods
The sample consisted of 281 healthy, employed middle-aged adults who were married or living with a partner in a marital-like relationship (mean age = 42.0 years, 88% white, 52% men). Marital interaction quality was assessed using hourly real-time Ecological Momentary Assessments (EMAs) for 4 days, with participants rating their current or recent partner interactions on positive and negative characteristics (e.g., agreeableness and conflict). Carotid artery intima medial thickness (IMT) was assessed using ultrasound imaging.
Results
Adjusting for demographics, positive marital interaction was inversely associated with IMT, [b = −.02 F(1, 275) = 9.18, p = .002], and negative marital interaction was positively associated with IMT, [b = .02 F(1, 275) = 10.29, p = .001]. These associations were not accounted for by behavioral and biological cardiovascular disease (CVD) risk factors and were consistent across age, sex, race, and education. The associations were also independent of marital interaction frequency, nonmarital social interaction quality, and personality factors. Global reports of marital quality, in contrast, were not associated with IMT.
Conclusions
Marital quality as measured during real-time interactions between partners was associated with subclinical cardiovascular disease in healthy middle-aged adults. This study supports the utility of real-time social interaction assessment for characterizing links between social relationships and cardiovascular health.
Keywords: marital quality, marital interaction, ecological momentary assessment, intima-media thickness, cardiovascular disease
Introduction
There is compelling evidence that being married is associated with reduced risk for premature all-cause and cardiovascular mortality (1–3). Marriages vary in quality, though, and marital quality may also have health implications (4). A growing literature suggests that marital quality may be linked with reduced coronary heart disease (CHD) morbidity and mortality in men and women in community (5) and patient samples (6–8).
Studies have increasingly examined the association between questionnaire measures of marital quality and markers of subclinical cardiovascular disease (CVD). Subclinical markers of CVD risk allow for the examination of correlates of future risk in healthy samples without confounding from medication use and psychosocial sequelae of adjusting to chronic medical illness. Subclinical markers of atherosclerosis, such as carotid artery intima-media thickness (IMT) and coronary artery calcification (CAC), are associated with coronary artery atherosclerosis in autopsy samples (9–11) and prospectively associated with risk for future heart attack and stroke (12, 13). Results of studies examining the association between global marital quality and subclinical markers of atherosclerosis are mixed, though, with some indicating no association (14–16) and others indicating significant cross-sectional and longitudinal associations (17). Mixed findings in this literature could be due to traditional measures of marital quality being variably influenced by recall biases. Furthermore, mixed findings could be due to global impressions of marital quality not necessarily being linked with actual moment-to-moment bodily processes and, thus, only indirectly associated with the actual mechanisms by which marital relationships confer health protection.
Studies that assess actual marital interactions may be in a better position to capture the marital dynamics that have direct implications for health behaviors and physiology, and thus cardiovascular health. For example, Smith and colleagues use behavioral coding strategies (18) to examine couple interactions during discussions of conflictual topics. They have shown that individuals whose marital interactions involve high levels of hostility and low levels of warmth are more likely to exhibit CAC (11,13). In contrast, global marital quality reports are not associated with CAC in this sample (14, 16). One limitation of laboratory interaction research is that the samples of marital interaction behavior are based on somewhat narrowly defined circumstances, and may not be broadly representative of marital interactions that occur in the natural environment.
Ecological momentary assessment (EMA) is a method of collecting behavioral and psychosocial data as it occurs in the natural environment, typically using portable devices programmed for recurrent data collection at pre-specified time intervals (19). By obtaining reports of daily life experiences close to the time at which they occur, EMA may allow us to circumvent the recall biases of retrospective report and capture the subtle, momentary marital exchanges more directly linked with momentary autonomic and neurohormonal bodily processes, and thus cardiovascular health (20). Given that marital quality theoretically manifests in two conceptually distinct marital processes important to health, i.e., support and strain (4, 21), EMA should be used to capture both positive and negative aspects of marital interaction. There is evidence that EMA measures of positive and negative marital interactions are moderately correlated with global questionnaire reports of marital quality (22). Furthermore, there is suggestive evidence that having data on daily marital interaction (in addition to global marital quality) is useful in predicting subclinical cardiovascular disease. Specifically, we found an inverse association between frequency of daily marital interactions and 3-year progression of IMT in a previous sample of older adults (50–70 years at baseline), but only among men who reported high quality marital relationships by global report (15). It is possible that interactions in high quality marital relationships are protective because they are more positive and less negative in nature. It was puzzling to us then that we did not find EMA-assessed marital interaction quality to be associated with IMT progression or baseline IMT in this earlier sample. The fact that psychosocial predictors of CVD are frequently stronger among younger when compared to older adults (22, 23) provides grounds for revisiting similar effects in the context of the current study.
The literature demonstrating that marital processes are associated with behavioral and biological factors that also serve as CVD risk factors (e.g., health behaviors, blood pressure, and stress-related cardiovascular reactivity) (21, 23, 24) further supports revisiting the association between marital interaction and IMT. In doing so, it is important to identify the potential effects of personality on this association given that the literature indicates that personality traits like neuroticism influence marital interactions, perceptions of interactions, and health (25, 26).
Primary Aims
We hypothesized that positive and negative marital interactions during daily life, as assessed by EMA, would be associated with carotid artery IMT in a middle-aged sample. In contrast to the existing laboratory-based research in this area, our study design provides a unique opportunity to compare the relative importance of marital and nonmarital interactions. This allows us to rule out the possibility that marital interaction quality is important simply because it reflects social interaction quality in general. Researchers have argued that the positive and negative aspects of marital relationships may be more important for health than similar aspects of other relationships because serious partners more closely share environments, time and resources (4). Therefore, we also hypothesized that the association between marital interaction quality and IMT would be independent of the quality of nonmarital interactions. We also examined whether this association was independent of marital interaction frequency and the Big Five personality dimensions (i.e., neuroticism, extroversion, openness, agreeableness, and conscientiousness).
Pathways
We examined whether traditional CVD risk factors serve as pathways for the marital interaction quality-IMT relationship. We also examined whether blood pressure reactivity to moments of marital interaction varied according to overall marital interaction quality, and whether this reactivity explained the effects of marital interaction quality on subclinical disease processes.
Methods
Participants
Participants were drawn from the Adult Health and Behavior Project – Phase 2 (AHAB-II), a study of psychosocial factors, behavioral and biological risk factors, and subclinical CVD. AHAB-II was approved by the University of Pittsburgh Institutional Review Board. AHAB-II participants were recruited between March 2008 and October 2011 through mass mailings of recruitment letters to individuals randomly selected from voter registration lists and other public domain lists.
To be eligible to participate in AHAB-II, individuals had to be between the ages of 30–55 years and working at least 25 hours per week outside of the home (a substudy involving this cohort was focused on the association between occupational stress and CHD risk). Individuals were excluded from participation if they (a) had a history of cardiovascular disease, schizophrenia or bipolar disorder, chronic hepatitis, renal failure, neurological disorder, lung disease requiring drug treatment, or stage 2 hypertension (SBP/DBP ≥ 160/100); (b) excessively consumed alcohol (≥ 5 portions 3–4 times per week); (c) used fish-oil supplements (because of the requirements for another substudy); (d) were prescribed medications with autonomic effects or used insulin, glucocorticoid, antiarrhythmic, antihypertensive, lipid-lowering, psychotropic, or prescription weight-loss medications; (e) were pregnant; (f) had less than 8th grade reading skills; or (g) were shift workers. Participants signed an informed consent form when enrolled. Participants received compensation up to $410, depending on extent of participation in visits and compliance with the protocol.
The subsample of married or cohabitating participants was used in the current investigation. To be included, participants also had to have completed EMA reports on at least four marital interactions (see elaboration on EMA procedures in Procedure section below). Participants with insufficient marital interaction data did not differ significantly from other participants on important variables, e.g., marital interaction quality, IMT, and biobehavioral CVD risk factor levels (ps > .09). Five additional participants were missing biobehavioral data relevant to the current investigation. Our final analytic sample consisted of 281 participants.
Procedure
Participants completed seven visits, some of which are not relevant to the current report. Demographic variables were assessed at Visit 1. A fasting blood draw was completed at Visit 1 to assess blood levels of physiologic risk factors, e.g., glucose and lipids. Clinic blood pressure was assessed at Visits 2 and 3. Global marital quality was assessed at Visit 3. A carotid artery ultrasound was completed at a separate visit from the other measures.
Ecological momentary assessments (EMA) and ambulatory blood pressure (ABP) assessments were completed between Visits 2 and 3 using a 4-day monitoring protocol (3 working days and 1 nonworking day). The monitoring protocol consisted of two 2-day monitoring periods, usually one period at the beginning of the workweek and another at the end of the workweek, with at least one non-monitoring day in between. During monitoring days, subjects wore an ABP device and carried a PDA (Palm Z22, software: Satellite Forms). They also wore other ambulatory devices not relevant to this investigation. During waking hours on monitoring days, ABP was automatically assessed hourly by inflation of the ABP cuff, which signaled participants to initiate a 43-item EMA questionnaire on the PDA with items that we have used in previous investigations (15, 27). Participants received extensive training and practice on the use of the ABP device and PDA before entering the field for ambulatory monitoring as well as feedback on compliance after completing a practice day. While in the field, participants received four scheduled phone calls from study staff, and staff was always available by cell phone for technical support.
Measures
Marital interaction quality
A measure of positive marital interaction and a measure of negative marital interaction were created using items from the hourly electronic questionnaire. During each assessment, participants were administered several items inquiring about their most recent social interaction, including time of interaction, number of people involved, and types of partners involved, e.g., spouse, coworker, etc.. From each interview, we extracted scores for the current or the most recent interaction. To reduce the possibility of redundancy, we eliminated scores for any interaction occurring more than 45 minutes before each hourly interview. We then separated scores that involved exclusive spousal interactions from those interactions that involved nonspousal partners. Only participants with data on at least four marital interactions were included in the study.
Interaction quality was assessed using four Likert scale items. Item responses [NO! No no yes Yes YES!] were converted to a 1–6 rating scale. Two items assessed positive aspects of interactions (i.e., “agreeable interaction?” and “pleasant interaction?”) and two assessed negative aspects of interactions (i.e., “someone in conflict with you?” and “someone treated you badly?”). Although the positive and negative items were inversely correlated, confirmatory factor analysis (CFA) indicated that they are best treated as indicators of separate constructs, with a two-factor model (Bentler Comparative Fit Index (CFI) = .99) fitting the data significantly better than a one-factor model, χ2(1, N = 281) = 430.65, p <.001. Responses to the two positive items were averaged across observations and days and summed to form a positive marital interaction score (α = .99). Responses to the two negative items were averaged across observations and days and summed to form a negative marital interaction score (α = .96). The positive marital interaction and negative marital interaction scores were moderately correlated, r(281) = −.66, p < .001). The average number of marital interactions rated by participants was 14 (range=4–37).1
The same steps were repeated for calculating positive and negative interaction scores for interactions that involved nonspousal partners, i.e., nonmarital interactions. The average number of nonmarital interactions rated by participants was 29 (range=5–52).
Global marital quality
Global marital quality was assessed using the widely-used Dyadic Adjustment Scale (DAS) (28), a 32-item self-report instrument which has been shown to discriminate between distressed and nondistressed married or cohabitating couples and to have adequate test-retest reliabilities (28, 29).
Personality
Personality traits were assessed using the NEO Personality Inventory-Revised (NEO-PI-R) (30). The NEO-PI-R is a 240-item self-report instrument that measures each of the “big five” personality dimensions using internally consistent, stable scales (31).
Cardiovascular reactivity
We conceptualized reactivity as the association between marital interaction and momentary ABP. As we have done with other psychosocial exposures (32–34), we captured the degree to which marital interaction was associated with momentary fluctuations in ABP using multilevel model analysis (SAS PROC MIXED). This method of capturing reactivity to psychosocial exposures has been validated against laboratory assessments of reactivity (34). For the current study, the primary predictor variable included in the models was a marital interaction indicator variable (i.e., dummy variable indicating marital interaction). Because of the acute nature of the reactivity concept, we designated only the observations associated with spousal partner interactions within the 10 minutes prior to the ABP assessment as involving marital interaction and excluded observations associated with spousal partner interaction more than 10 minutes prior to the ABP assessment. We designated observations that were associated with either no social interaction or interaction with only nonspousal partners within the interval since the last ABP assessment as not involving marital interaction.
Two separate multilevel models were used to estimate momentary systolic and diastolic ABP reactivity to marital interaction, with relevant covariates being specified as fixed effects and a marital interaction indicator variable being specified as a random effect. This multi-level model specification allowed the association between momentary marital interaction and ABP to be estimated overall as well as separately for each participant. The variances and covariances of the intercept and the marital interaction indicator variable were estimated in the model (Gmatrix=UN), and a spatial power autocorrelation matrix was used (REPEATED/sub=subject type=sp(pow) (time) local) (35). The coefficient of interest was the partial regression coefficient for each participant indicating the random effect of marital interaction on ABP adjusted for all relevant participant level and time-varying covariates. Because these coefficients represent the extent of ABP change associated with interacting with the marital partner, each participant’s regression coefficient was considered that participant’s reactivity score for that respective model. Regression coefficients (reactivity scores) were used as predictors in separate analyses as described in the Statistical Analyses section.
Carotid intima-media thickness (IMT)
B-mode ultrasound assessments were conducted at the University of Pittsburgh Ultrasound Research Laboratory using an Acuson Sonoline Antares high resolution duplex scanner (Acuson-Siemens, Malvern, PA). Trained, certified sonographers identified the borders of the intima and medial layers of the left and right carotid arteries, using the intima-lumen interface and the media-adventitial interface as markers. Distances between these interfaces were measured on digitized images across the distal 1 cm (far wall) of the left and right common carotid artery, carotid bulb, and proximal 1 cm of the internal carotid. Studies were read using an automated edge detection algorithm (Artery Measurement System, Goteborg University, Gothenburg, Sweden) (36).
The intraclass correlation coefficient (ICC) for carotid scanning in this sample was .88. The ICC between readers was calculated each year of the study and ranged from .89 to .97.
IMT was operationalized as the average of IMT from the left and right far wall segments of the common carotid artery, carotid artery bulb, and internal carotid artery. One extreme outlier (>4 standard deviations [SDs] above the mean) was eliminated. IMT scores were not normally distributed so they were log transformed to reduce skewness.
Covariates
Demographics
Participants self-reported their age, race/ethnicity, sex, and highest level of education completed.
Behavioral and biological risk factors
Participants self-reported their smoking status (non-smoker, ex-smoker, current smoker, and other tobacco user) and number of drinks of alcohol in the month prior to data collection. Current smoking status (1 vs. 0) was coded. Body mass index (BMI) was calculated based on height and weight measured in the clinic (lbs/inches2 × 703). Clinic blood pressure was assessed at Visits 2 and 3 by trained research assistants using a manual Baumanometer® mercury sphygmomanometer (desk model, W.A. Baum Co. Inc., New York) and a standard protocol (37). At each visit, two readings were taken. Clinic systolic and diastolic blood pressures were calculated as averages of the four readings. A standard lipid panel (total cholesterol, triglyceride, high-density lipoprotein (HDL), and low-density lipoprotein (LDL)) was assessed. Fasting serum glucose was assayed via standard colorimetry.
Statistical Analyses
Analyses were conducted using SAS statistical software (version 9.3; SAS Institute, Cary, NC). Multiple linear regressions (PROC GLM) were used to conduct most analyses and the INDIRECT procedure for SAS (38) was used to test mediation hypotheses. Continuous covariates were centered before being entered into analyses. Race/ethnicity was recoded into a dummy variable representing African American race (1 vs. 0).
Our primary hypothesis was tested by entering the positive marital interaction and negative marital interaction scores into separate regressions with the demographic covariates. In additional regressions, we examined whether demographics modified the main effect by alternating in interaction terms (e.g., sex X positive marital interaction score). To examine whether traditional behavioral and biological CVD risk factors, ABP, or ABP reactivity2 to marital interaction served as mediators, we used the INDIRECT procedure for SAS (38)
We sequentially alternated the following variables into our primary regressions to determine whether they were potential confounders of the main effects of positive and negative marital interactions: number of marital interactions, positive and negative interaction scores derived from interactions with individuals other than the marital partner, and the five personality dimensions.
Lastly, we conducted a series of secondary regression analyses. To explore whether the effects of positive marital interaction and negative marital interaction modified each other, we centered each of these factors and conducted a regression that included these centered factors and a multiplicative interaction term between them. To test the association between global reports of marital quality and IMT, we conducted separate analyses including overall marital quality score.
Results
Select Sample Characteristics
The study sample is described in Table 1. Participants were primarily white (88%), 11% African American, and 1% Asian or other. Participants were middle-aged, educated (76% had at least a bachelor’s degree), and mostly in nondistressed marriages (77% with DAS score > 100; DAS scores ranged from 48–138 with mean DAS score = 109.31). Participants perceived their marital interactions as agreeable (mean positive interaction score = 9.4, SD = 1.4, possible range = 2–12), and low in conflict (mean negative interaction score = 3.4, SD = 1.5, possible range = 2–12). Mean positive and negative interaction scores for non-marital interactions were similar to those for marital interactions (9.5 and 3.3, respectively). If examined by type of interaction partner, friend interactions were rated the most positively (mean positive interaction score = 10.1) and stranger interactions were rated the most negatively (mean negative interaction score = 3.5). Mean IMT was .63 (SD = .12).
Table 1.
Select Characteristics of the Analytic Sample (N = 281)
| Characteristic | Mean (SD) or % (n) |
|---|---|
| Mean (SD) | |
|
| |
| Age (years) | 42.0 (7.3) |
| BMI | 26.7 (5.0) |
| Systolic blood pressure (mm Hg) | 114.8 (10.8) |
| Diastolic blood pressure (mm Hg) | 72.1 (7.8) |
| IMT (mm) | .63 (.12) |
|
| |
| % (n) | |
|
| |
| Male sex | 52.0 (147) |
| African American race | 10.7 (30) |
| Bachelor’s degree or higher | 75.8 (213) |
| Current smoker | 11.0 (31) |
| ≥ 30 drinks per month | 12.5 (35) |
| Distressed marriagea | 22.1 (62) |
Note.
DAS score <100
On average, participants completed 89% of the hourly assessments that they had the opportunity to complete during waking hours on the initial four monitoring days, so overall compliance was excellent. Although individual compliance scores ranged from 41% to 100%, only 8 participants had compliance scores under 60%.
Marital Interaction Quality and IMT
Results of primary analyses are shown in Table 2. Adjusting for demographics, those who rated their marital interactions as more positive demonstrated lower mean IMT, b = −.02, F(1, 275) = 9.18, p = .002, and this association remained significant after adjustment for behavioral and biological risk factors, b = −.02, R2 = .037, F(1, 266) = 10.25, p = .002,. In fact, there were no significant indirect effects of positive marital interaction on IMT through these behavioral and biological risk factors3. Furthermore, none of the interaction terms was significant. To depict the positive marital interaction main effect graphically, we determined adjusted mean IMT at each tertile of the positive marital interaction scores. As Figure 1 demonstrates, the relationship between positive marital interaction and IMT followed a linear pattern in which mean IMT was lower at each subsequent tertile of positive marital interaction; only the top and bottom tertiles were significantly different.
Table 2.
Final Primary Multivariate Linear Regressions Examining Associations of Marital Interaction Quality and IMT
| Positive Marital Interaction | Negative Marital Interaction | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | b | R2 | p | b | R2 | p |
| Age | .011 | .243 | <.001 | .011 | .245 | <.001 |
| Male sex | .059 | .028 | .006 | .051 | .022 | .014 |
| African American race | .053 | .012 | .073 | .054 | .011 | .081 |
| Highest degree | .020 | .014 | .055 | .020 | .013 | .066 |
| Current smoking | −.014 | .001 | .63 | −.017 | .002 | .54 |
| Drinks per month | −.001 | .010 | .10 | −.001 | .005 | .22 |
| BMI | .007 | .034 | .002 | .006 | .028 | .006 |
| Systolic blood pressure | .004 | .035 | .002 | .004 | .034 | .002 |
| Diastolic blood pressure | −.002 | .004 | .28 | −.002 | .004 | .30 |
| Glucose | .001 | .006 | .20 | .001 | .007 | .18 |
| LDL cholesterol | .001 | .021 | .018 | .001 | .025 | .010 |
| HDL cholesterol | −.001 | .009 | .12 | −.001 | .012 | .078 |
| Triglycerides | −.010 | .001 | .62 | −.010 | .000 | .63 |
| Positive marital interaction | −.020 | .037 | .002 | |||
| Negative marital interaction | .020 | .038 | .001 | |||
Note. b = nonstandardized partial regression coefficients.
Figure 1.
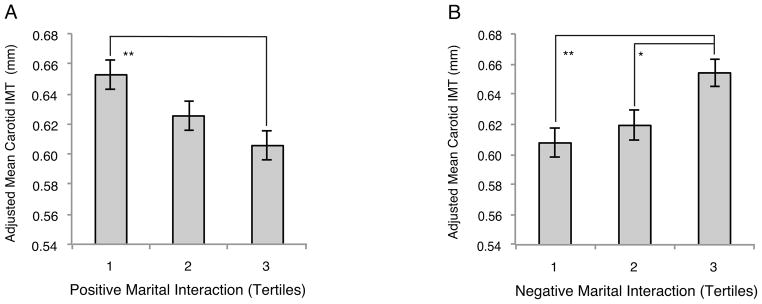
Adjusted mean carotid IMT by positive marital interaction (Panel A) and negative marital interaction (Panel B). Adjusted for all demographic and traditional CVD risk factor covariates. Error bars represent ± 1 standard error. Tertiles used for graphic display although continuous data was used in analyses. Non-transformed IMT data was used in figure for interpretability although log-transformed IMT was used in analyses.
** Groups differ significantly at p < .010. * Groups differ significantly at p < .050.
Adjusting for demographics, those who rated their marital interactions as more negative demonstrated higher mean IMT, [b = .02, F(1, 275) = 10.29, p = .001], and this association remained significant after adjustment for behavioral and biological risk factors, b = .02, R2 = .038, F(1, 266) = 10.33, p = .001. Once again, there were no significant indirect effects of negative marital interaction on IMT through these behavioral and biological risk factors4. None of the interaction terms was significant. To depict the negative marital interaction main effect graphically, we determined adjusted mean IMT at each tertile of the negative marital interaction scores. As Figure 1 demonstrates, those in the top tertile of negative marital interaction had significantly higher IMT than those in the bottom two tertiles, while there was no difference in IMT among those in the bottom two tertiles.
When positive marital interaction and negative marital interaction were tested together in the same model, their separate associations with IMT were reduced in size and significance, b = −.01, p = .16 and b = .01, p = .15, respectively. Furthermore, the interaction between positive and negative marital interaction was not significant, F(1, 265) = .23, p = .63.
Blood Pressure Reactivity as a Potential Pathway
Multilevel models demonstrated that systolic and diastolic blood pressure were lower during moments which involved interaction with the marital partner compared to moments that did not, b = −1.67, p < .001 and b = −1.66, p < .001, respectively and that, with adjustment for demographics, those with higher mean positive marital interaction scores exhibited greater relative reductions in systolic blood pressure during marital interactions, b = −.23, p = .039. However, systolic reactivity to marital interaction was not associated with IMT in multivariate regressions (p = .71). Furthermore, the indirect effects of mean marital interaction quality scores on IMT through mean ABP and ABP reactivity to marital interaction were not significant (p values > .49).
Potential Confounders in the Association between Marital Interaction Quality and IMT
Marital interaction frequency was not significantly associated with IMT, F(1, 266) = 0.69, p = .39, so both positive marital interaction and negative marital interaction remained significant when marital interaction frequency was included in the respective models.
Additionally, the main effects of positive and negative marital interaction remained significant after adjustment for positive and negative nonmarital interaction, respectively. When tested alone, positive nonmarital interaction was significantly associated with IMT (b = −.015, p = .040). However, when positive marital and nonmarital interaction were included together in an analysis, only positive marital interaction was independently associated with IMT (b = −.020, p = .016). When tested alone, negative nonmarital interaction was significantly associated with IMT (b = .013, p = .034). However, when negative marital and nonmarital interaction were included together in an analysis, only negative marital interaction was independently associated with IMT (b =.030, p = .008).
Finally, none of the personality factors was associated with IMT in bivariate or multivariate analyses (p values > .11), and controlling for these factors in respective models did not affect the associations between marital interaction quality and IMT.
Global Marital Quality and IMT
Overall global marital quality, as measured by the DAS, was not significantly associated with IMT, F(1, 266) = 1.14, p = .29.
Discussion
Findings from the current study support the hypothesis that marital interaction quality in daily life is associated with subclinical cardiovascular disease in middle-aged individuals. This is the first study to demonstrate this association and to show that positive and negative interactions contribute to this effect. Associations between marital interaction quality and IMT were independent of marital interaction frequency, nonmarital interaction quality, and major personality factors. We did not find support for behavioral and biological factors as pathways for these associations.
The current study focused on health implications of positive and negative marital interactions whereas more of the literature, primarily laboratory studies, has focused on negative marital interaction alone. Our results suggest that positive and negative marital interactions matter similarly for CVD risk, and that their effects are not independent of each other. This is consistent with laboratory research demonstrating that both low levels of warm behavior and high levels of dominating behavior in laboratory marital interactions are associated with coronary artery calcification (CAC), another subclinical marker of atherosclerosis and CVD risk (14).
Interpretation of the clinical significance of our finding relies on the usefulness of small differences in carotid IMT for predicting future CVD risk. A recent meta-analysis concluded that a .1 mm difference in common carotid IMT is associated with 17% increased risk for myocardial infarction and stroke, with this degree of increased risk evidenced even in studies with only 4 years of follow-up (39). Thus, our finding that the mean IMT of those in the lowest tertile of positive marital interaction quality is .05 mm higher than that of those in the highest tertile suggests that individuals with marital interactions low in positivity may have approximately 8.5% increased risk for myocardial infarction and stroke than those with very positive marital interactions. Similarly, those with marital interaction high in negativity may have approximately 5.5% increased risk for myocardial infarction and stroke than those with marital interactions low in negativity. It is also noteworthy that positive and negative marital interaction each accounted for the same independent proportion of the variance in IMT as the biological risk factors of BMI, systolic blood pressure, and LDL cholesterol. Further discussion of clinical implications must be foregone until additional research designed to demonstrate causality is conducted.
We did not find support for traditional and novel risk factors for cardiovascular disease as mechanisms accounting for the association between marital interaction quality and IMT. Since IMT increases gradually over time, cumulative exposure to behavioral and biological risk factors or risk factor trajectories over the years might better serve as pathways linking marital interactions and IMT than the cross-sectional exposure data that we have available. Longitudinal research suggests that those with differing marital quality tend to exhibit different CVD risk factor profiles and trajectories over time (40). Future research should determine whether differential risk factor trajectories account for the effects of interaction quality. Potential mechanisms other than those presented here (e.g., physical activity, inflammatory markers, and heart rate variability (e.g., see (41)) should be examined longitudinally as well. Additionally, momentary marital interactions and blood pressure may need to be monitored over a longer period to increase precision and stability of reactivity estimates examined as potential pathways.
It is noteworthy that we ruled out personality as a confounding third factor in the association between marital interaction quality and IMT. We did not have data on other potentially confounding factors such as childhood adversity. For example, individuals who have experienced childhood abuse, especially women, are more likely to have less adaptive intimate interactions and be at risk for cardiovascular disease (42–44).
Our finding that marital interaction quality trumps quality of all other social interactions in influencing IMT is consistent with the literature. For example, there is evidence that being married is more important than the size of ones’ entire social network in predicting longevity (45) and that ABP is lower during marital interactions than during nonmarital interactions (27). Taken together, the literature supports the idea that marital interactions and general social interactions have differential importance for health.
It is noteworthy that we found that marital interaction quality was associated with IMT in this sample and not in our previous study, which used the Pittsburgh Healthy Heart Project (PHHP) sample (15). It is likely that substantial differences between the PHHP sample and the current sample explain this differential finding. The PHHP sample was much older (ages 50–70) than the AHAB-II sample (ages 30–55) and had a much higher mean IMT score (.77 mm). Furthermore, the PHHP sample, in addition to being less ethnically diverse and educated, included individuals of various employment statuses whereas AHAB-II only included those working at least 25 hours per week. Workers may be exposed to a wider range of marital interaction experiences that could influence health due to the influence of the work domain on the home domain and relationships. The PHHP sample also reported less marital distress on the DAS than the AHAB-II sample, a fact that may indicate a different distribution of marital interaction quality and, thus, less power to find associations with IMT.
Our finding that global marital quality was not associated with IMT is consistent with the mixed literature on the association between global marital quality and subclinical markers of CVD risk (14–16). EMA measures may be more predictive of physical health outcomes than global measures because, when compared with global retrospective reports, they may more effectively capture experiences directly tied to momentary health processes and variability in these processes (20).
Interestingly, none of our findings differed by sex. A recent meta-analysis found only small, inconsistent sex moderation of the association between marital quality and markers of CVD risk (4). The same may be true of the marital interaction measures examined here.
Limitations
This study is not without limitations. First, it is cross sectional and, thus, a causal relationship between marital interaction quality and IMT cannot be established. There is suggestive evidence that declines in health may lead to declines in marital quality (46), so bidirectional associations are plausible. Nevertheless, given that our sample is healthy and that IMT is a subclinical marker that is generally undetectable, it is unlikely that greater IMT led participants to have less positive or more negative marital interactions.
Relatedly, we do not have data on length of cohabitation or marriage, so it is unclear whether the associations found vary by partnership duration. Marital quality declines over time (47, 48). To the best of our knowledge, no research speaks to whether EMA-assessed marital interaction also becomes less positive or more negative over time. EMA-assessed marital interaction quality seems to at least be stable and reliable over short intervals (22). Of note, we sampled marital interactions from mostly working days. A sampling design based on mostly nonworking days may have resulted in different overall marital interaction scores and possibly different associations with IMT. Nevertheless, our sampling design most closely approximates the lives of working individuals given that they spend more days working than not.
Finally, our sample was primarily white and well educated, so it is unclear whether these associations exist across various ethnic and socioeconomic groups. For example, evidence is less compelling that marriage and marital happiness is cardioprotective for African Americans (3, 49). It is likely that our study was underpowered to detect small to moderate ethnic differences in marital interaction quality effects.
Implications/Future Research
Despite limitations, the current study is the first to demonstrate associations between positive and negative marital interaction during daily life and carotid artery IMT, a subclinical marker of atherosclerosis. This is a compelling finding with implications for future research. Replication in longitudinal and intervention contexts is necessary to delineate more clearly the causal implications of the observed effects. Moreover, additional work is needed to explore the behavioral and biological trajectories by which such interaction patterns might plausibly influence cardiovascular risk. Global and momentary assessments should be used in the service of further understanding the relationship between marital quality and health.
Acknowledgments
Source of Funding: This research was supported by National Institutes of Health Grants P01 HL040962 awarded to Drs. Manuck, Kamarck, and Muldoon and T32 HL007560 (fellowship) awarded to Dr. Joseph. Dr. Joseph is currently supported by the VA Office of Academic Affiliations’ Women’s Health Fellowship Program.
We wish to acknowledge the collaborative efforts of the late Kim Sutton-Tyrrell, director of the Ultrasound Research Laboratory at the University of Pittsburgh, who assisted with this project. She was a wise mentor, a dedicated colleague, and an encouraging collaborator to many of us over the years. Without her efforts, this kind of work, quite simply, would not have been possible.
Glossary
- EMA
Ecological Momentary Assessment
- CVD
cardiovascular disease
- IMT
intima-media thickness
- CHD
Coronary Heart Disease
- ABP
ambulatory blood pressure
- AHAB-II
Adult Health and Behavior Project – Phase 2
- DAS
Dyadic Adjustment Scale
- NEO-PI-R
NEO Personality Inventory-Revised
- ICC
intraclass correlation coefficient
- BMI
body mass index
- LDL
low-density lipoprotein
- HDL
high-density lipoprotein
- PHHP
Pittsburgh Healthy Heart Project
- CAC
coronary artery calcification
Footnotes
We also calculated scores to capture frequency of exposure to positive and negative marital interaction. Specifically, for positive marital interaction frequency and negative marital interaction frequency scores, we calculated proportion of marital interactions rated above the sample means for positive and negative marital interaction scores, respectively. These frequency scores were highly correlated with the respective mean scores, (rs > .89), so we only used mean scores in analyses.
See Methods section for details of the preliminary multilevel analyses that were conducted to derive two separate reactivity terms for each participant.
Results of SAS INDIRECT procedures available upon request.
Results of SAS INDIRECT procedures available upon request.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Contributor Information
Nataria T. Joseph, Department of Psychiatry, University of Pittsburgh.
Thomas W. Kamarck, Departments of Psychology and Psychiatry, University of Pittsburgh.
Matthew F. Muldoon, Department of Medicine, University of Pittsburgh.
Stephen B. Manuck, Department of Psychology, University of Pittsburgh.
References
- 1.Molloy GJ, Stamatakis E, Randall G, Hamer M. Marital status, gender and cardiovascular mortality: behavioural, psychological distress and metabolic explanations. Soc Sci Med. 2009;69(2):223–28. doi: 10.1016/j.socscimed.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ebrahim S, Wannamethee G, McCallum A, Walker M, Shaper AG. Marital status, change in marital status, and mortality in middle-aged British men. Am J Epidemiol. 1995;142(8):834–42. doi: 10.1093/oxfordjournals.aje.a117723. [DOI] [PubMed] [Google Scholar]
- 3.Johnson NJ, Backlund E, Sorlie PD, Loveless CA. Marital status and mortality: the national longitudinal mortality study. Ann Epidemiol. 2000;10(4):224–38. doi: 10.1016/s1047-2797(99)00052-6. [DOI] [PubMed] [Google Scholar]
- 4.Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: a meta-analytic review. Psychol Bull. 2013 doi: 10.1037/a0031859. online first publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Vogli R, Chandola T, Marmot MG. Negative aspects of close relationships and heart disease. Arch Intern Med. 2007;167(18):1951–7. doi: 10.1001/archinte.167.18.1951. Epub 2007/10/10. [DOI] [PubMed] [Google Scholar]
- 6.Orth-Gomer K, Wamala SP, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman MA. Marital stress worsens prognosis in women with coronary heart disease: The Stockholm Female Coronary Risk Study. JAMA. 2000;284(23):3008–14. doi: 10.1001/jama.284.23.3008. Epub 2000/12/21. [DOI] [PubMed] [Google Scholar]
- 7.Rohrbaugh MJ, Shoham V, Coyne JC. Effect of marital quality on eight-year survival of patients with heart failure. Am J Cardiol. 2006;98(8):1069–72. doi: 10.1016/j.amjcard.2006.05.034. Epub 2006/10/10. [DOI] [PubMed] [Google Scholar]
- 8.Wang HX, Leineweber C, Kirkeeide R, Svane B, Schenck-Gustafsson K, Theorell T, et al. Psychosocial stress and atherosclerosis: family and work stress accelerate progression of coronary disease in women. The Stockholm Female Coronary Angiography Study. J Intern Med. 2007;261(3):245–54. doi: 10.1111/j.1365-2796.2006.01759.x. Epub 2007/02/20. [DOI] [PubMed] [Google Scholar]
- 9.Simons DB, Schwartz RS, Edwards WD, Sheedy PF, Breen JF, Rumberger JA. Noninvasive definition of anatomic coronary artery disease by ultrafast computed tomographic scanning: A quantitative pathologic comparison study. J Am Coll Cardiol. 1992;20(5):1118–26. doi: 10.1016/0735-1097(92)90367-v. [DOI] [PubMed] [Google Scholar]
- 10.Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74(6):1399–1406. doi: 10.1161/01.cir.74.6.1399. [DOI] [PubMed] [Google Scholar]
- 11.Wong M, Edelstein J, Wollman J, Bond MG. Ultrasonic-pathological comparison of the human arterial wall. Verification of intima-media thickness. Arterioscler Thromb Vasc Biol. 1993;13(4):482–6. doi: 10.1161/01.atv.13.4.482. [DOI] [PubMed] [Google Scholar]
- 12.O’Leary DH, Polak JF. Intima-media thickness: a tool for atherosclerosis imaging and event prediction. Am J Cardiol. 2002;90(10C):18L–21L. doi: 10.1016/s0002-9149(02)02957-0. [DOI] [PubMed] [Google Scholar]
- 13.Salonen J, Salonen R. Ultrasound B-mode imaging in observational studies of atherosclerotic progression. Circulation. 1993;87(3 Suppl):II56–65. [PubMed] [Google Scholar]
- 14.Smith TW, Uchino BN, Florsheim P, Berg CA, Butner J, Hawkins M, et al. Affiliation and control during marital disagreement, history of divorce, and asymptomatic coronary artery calcification in older couples. Psychosom Med. 2011;73(4):350–7. doi: 10.1097/PSY.0b013e31821188ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Janicki DL, Kamarck TW, Shiffman S, Sutton-Tyrrell K, Gwaltney CJ. Frequency of spousal interaction and 3-year progression of carotid artery intima medial thickness: the Pittsburgh Healthy Heart Project. Psychosom Med. 2005;67(6):889–96. doi: 10.1097/01.psy.0000188476.87869.88. [DOI] [PubMed] [Google Scholar]
- 16.Smith TW, Uchino BN, Berg CA, Florsheim P. Marital discord and coronary artery disease: a comparison of behaviorally defined discrete groups. J Consult Clin Psychol. 2012;80(1):87–92. doi: 10.1037/a0026561. Epub 2011/12/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gallo LC, Troxel WM, Kuller LH, Sutton-Tyrrell K, Edmundowicz D, Matthews KA. Marital status, marital quality, and atherosclerotic burden in postmenopausal women. Psychosom Med. 2003;65(6):952–62. doi: 10.1097/01.psy.0000097350.95305.fe. [DOI] [PubMed] [Google Scholar]
- 18.Smith TW, Berg CA, Florsheim P, Uchino BN, Pearce G, Hawkins M, et al. Conflict and collaboration in middle-aged and older couples: I. Age differences in agency and communion during marital interaction. Psychol Aging. 2009;24(2):259–73. doi: 10.1037/a0015609. Epub 2009/06/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavorial medicine. Ann Behav Med. 1994;16(3):199–202. [Google Scholar]
- 20.Conner TS, Barrett LF. Trends in ambulatory self-report: the role of momentary experience in psychosomatic medicine. Psychosom Med. 2012;74(4):327–37. doi: 10.1097/PSY.0b013e3182546f18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 22.Janicki DL, Kamarck TW, Shiffman S, Gwaltney CJ. Application of ecological momentary assessment to the study of marital adjustment and social interactions during daily life. J Fam Psychol. 2006;20(1):168–72. doi: 10.1037/0893-3200.20.1.168. [DOI] [PubMed] [Google Scholar]
- 23.Robles TF, Kiecolt-Glaser JK. The physiology of marriage: pathways to health. Physiol Behav. 2003;79(3):409–16. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- 24.Kiecolt-Glaser JK, Glaser R, Cacioppo JT, Malarkey WB. Marital stress: immunologic, neuroendocrine, and autonomic correlates. Ann N Y Acad Sci. 1998;840:656–63. doi: 10.1111/j.1749-6632.1998.tb09604.x. Epub 1998/06/18. [DOI] [PubMed] [Google Scholar]
- 25.Pietromonaco PR, Uchino B, Dunkel Schetter C. Close relationship processes and health: Implications of attachment theory for health and disease. Health Psychol. 2013;32(5):499–513. doi: 10.1037/a0029349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGonagle KA, Kessler RC, Schilling EA. The frequency and determinants of marital disagreements in a community sample. J Soc Pers Relat. 1992;9(4):507–24. [Google Scholar]
- 27.Gump BB, Polk DE, Kamarck TW, Shiffman SM. Partner interactions are associated with reduced blood pressure in the natural environment: ambulatory monitoring evidence from a healthy, multiethnic adult sample. Psychosom Med. 2001;63(3):423–33. doi: 10.1097/00006842-200105000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38(1):15–28. [Google Scholar]
- 29.Carey MP, Spector IP, Lantinga LJ, Krauss DJ. Reliability of the Dyadic Adjustment Scale. Psychol Assess. 1993;5(2):238–40. [Google Scholar]
- 30.Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa: Psychological Assessment Resources; 1992. [Google Scholar]
- 31.McCrae RR, John OP. An introduction to the five-factor model and its applications. J Pers. 1992;60(2):175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x. Epub 1992/06/01. [DOI] [PubMed] [Google Scholar]
- 32.Kamarck TW, Shiffman SM, Smithline L, Goodie JL, Paty JA, Gnys M, et al. Effects of task strain, social conflict, and emotional activation on ambulatory cardiovascular activity: Daily life consequences of recurring stress in a multiethnic adult sample. Health Psychol. 1998;17(1):17–29. doi: 10.1037//0278-6133.17.1.17. [DOI] [PubMed] [Google Scholar]
- 33.Kamarck TW, Janicki DL, Shiffman S, Polk DE, Muldoon MF, Liebenauer LL, et al. Psychosocial demands and ambulatory blood pressure: A field assessment approach. Physiol Behav. 2002;77:699–704. doi: 10.1016/s0031-9384(02)00921-6. [DOI] [PubMed] [Google Scholar]
- 34.Kamarck TW, Schwartz JE, Janicki DL, Shiffman S, Raynor DA. Correspondence between laboratory and ambulatory measures of cardiovascular reactivity: a multilevel modeling approach. Psychophysiology. 2003;40(5):675–83. doi: 10.1111/1469-8986.00069. Epub 2003/12/31. [DOI] [PubMed] [Google Scholar]
- 35.Schwartz JE, Stone AA. The analysis of real-time momentary data: A practical guide. In: Stone SS, Shiffman S, Atienza AA, Nebeling L, editors. The science of real-time data capture: Self-reports in health research. New York: Oxford University Press; 2007. pp. 76–113. [Google Scholar]
- 36.Wendelhag I, Liang Q, Gustavsson T, Wikstrand J. A new automated computerized analyzing system simplifies readings and reduces the variability in ultrasound measurement of intima-media thickness. Stroke. 1997;28(11):2195–200. doi: 10.1161/01.str.28.11.2195. Epub 1997/11/22. [DOI] [PubMed] [Google Scholar]
- 37.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45(1):142–61. doi: 10.1161/01.HYP.0000150859.47929.8e. Epub 2004/12/22. [DOI] [PubMed] [Google Scholar]
- 38.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40:879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 39.van den Oord SCH, Sijbrands EJG, ten Kate GL, van Klaveren D, van Domburg RT, van der Steen AFW, et al. Carotid intima-media thickness for cardiovascular risk assessment: systematic review and meta-analysis. Atherosclerosis. 2013;228:1–11. doi: 10.1016/j.atherosclerosis.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 40.Gallo LC, Troxel WM, Matthews KA, Kuller LH. Marital status and quality in middle-aged women: associations with levels and trajectories of cardiovascular risk factors. Health Psychol. 2003;22(5):453–63. doi: 10.1037/0278-6133.22.5.453. [DOI] [PubMed] [Google Scholar]
- 41.Smith TW, Cribbet MR, Nealey-Moore JB, Uchino BN, Williams PG, Mackenzie J, et al. Matters of the variable heart: respiratory sinus arrhythmia response to marital interaction and associations with marital quality. J Pers Soc Psychol. 2011;100(1):103–19. doi: 10.1037/a0021136. Epub 2010/10/20. [DOI] [PubMed] [Google Scholar]
- 42.Hosang GM, Johnson SL, Kiecolt-Glaser J, Di Gregorio MP, Lambert DR, Bechtel MA, et al. Gender specific association of child abuse and adult cardiovascular disease in a sample of patients with Basal Cell Carcinoma. Child Abuse Neglect. 2013;37(6):374–9. doi: 10.1016/j.chiabu.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Batten SV, Aslan M, Maciejewski PK, Mazure CM. Childhood maltreatment as a risk factor for adult cardiovascular disease and depression. J Clin Psychiat. 2004;65(2):249–54. doi: 10.4088/jcp.v65n0217. [DOI] [PubMed] [Google Scholar]
- 44.Scott KM, Von Korff M, Angermeyer MC, Benjet C, Bruffaerts R, de Girolamo G, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiat. 2011;68(8):838–44. doi: 10.1001/archgenpsychiatry.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rutledge T, Matthews K, Lui L-Y, Stone KL, Cauley JA. Social networks and marital status predict mortality in older women: prospective evidence from the Study of Osteoporotic Fractures (SOF) Psychosom Med. 2003;65(4):688–94. doi: 10.1097/01.psy.0000041470.25130.6c. [DOI] [PubMed] [Google Scholar]
- 46.Yorgason JB, Booth A, Johnson D. Health, disability, and marital quality: is the association different for younger versus older cohorts? Res Aging. 2008;30(6):623–48. [Google Scholar]
- 47.Wendorf CA, Lucas T, Imamoğlu EO, Weisfeld CC, Weisfeld GE. Marital satisfaction across three cultures: does the number of children have an impact after accounting for other marital demographics? J Cross Cult Psychol. 2011;42(3):340–54. [Google Scholar]
- 48.VanLaningham J, Johnson DR, Amato P. Marital happiness, marital duration, and the u-shaped curve: evidence from a five-wave panel study. Soc Forces. 2001;79(4):1313–41. [Google Scholar]
- 49.Schwandt HM, Coresh J, Hindin MJ. Marital status, hypertension, coronary heart disease, diabetes, and death among African American women and men: incidence and prevalence in the Atherosclerosis Risk in Communities (ARIC) study participants. J Fam Issues. 2010;31(9):1211–29. doi: 10.1177/0192513X10365487. [DOI] [PMC free article] [PubMed] [Google Scholar]


