Abstract
Background
Racial misclassification of American Indian and Alaska Native (AI/AN) individuals as non-AI/AN in cancer registries presents problems for cancer surveillance, research, and public health practice. The aim of this study was to investigate the efficiency of tribal linkages in enhancing the quality of racial information in state cancer registries.
Methods
Registry Plus™ Link Plus 2.0 probabilistic record linkage software was used to link the Michigan state cancer registry data (1985–2004; 1,031,168 cancer cases) to the tribal membership roster (40,340 individuals) in July of 2007. A data set was created containing AI/AN cancer cases identified by the state registry, Indian Health Service (IHS) linkages, and tribal linkage. The differences between these three groups of individuals were compared by distribution of demographic, diagnostic, and county-level characteristics using multilevel analysis (conducted in 2007–2008).
Results
From 1995 to 2004, the tribal enrollment file showed linkages to 670 cancer cases (583 individuals) and the tribal linkage led to the identification of 190 AI/AN cancer cases (168 individuals) that were classified as non-AI/AN in the registry. More than 80% of tribal members were reported as non-AI/AN to the registry. Individuals identified by IHS or tribal linkages were different from those reported to be AI/AN in terms of stage at diagnosis, tumor confirmation, and characteristics of the county of diagnosis, including contract health services availability, tribal health services availability, and proportion of AI/AN residents.
Conclusions
The data linkage between tribal and state cancer registry data sets improved racial classification validity of AI/AN Michigan cancer cases. Assessing tribal linkages is a simple, noninvasive way to improve the accuracy of state cancer data for AI/AN populations and to generate tribe-specific cancer information.
Background
According to national cancer registries, the overall cancer incidence rate for American Indian and Alaska Native (AI/AN) individuals is nearly half that for all races combined.1 However, when cancer data are linked with more accurate sources of race, such as Indian Health Service (IHS) patient registration records, the cancer incidence rate for AI/AN individuals can more than double.2
Misclassification of AI/AN cancer cases as non- AI/AN often occurs because of lack of racial identity information in medical records used for cancer registry reporting. Agreement of medical record and selfreported race/ethnicity is particularly low for American Indians but varies widely, with three recent studies3–5 reporting 5%, 16%, and 98% agreement, respectively. Misclassification on death certificates may result in an underestimation by more than 20% of death rates for AI/AN individuals.6
Data linkages aim to identify two records in two data sets that represent the same person. For example, a data linkage between a cancer registry and an IHS patient registration looks for records in the two files that are for the same person. Because the IHS patient registration file includes tribal members only, any individual in the cancer registry who is also in the IHS file is assumed to self-identify as AI/AN. The effectiveness of IHS linkages in identifying misclassified AI/AN individuals has made data linkage a standard tool used by most state cancer registries to improve the quality of AI/AN race data.
The IHS Division of Epidemiology in Albuquerque NM conducts annual linkages with the Michigan state cancer registry. Although these linkages have greatly improved the quality of race data in the registry, IHS provides primary health care to only 58% of the estimated 3.1 million AI/AN population in the U.S.7 Health services are provided both directly at IHS facilities and indirectly, through contract health services (CHS) at non-IHS facilities. The Indian Health Service has one urban health center in Michigan; therefore, the vast majority of IHS services in Michigan are provided through CHS. In 2006, nearly 40% of Michigan counties were non-CHS areas.8 In addition, many AI/AN individuals may not be included in IHS patient files because of eligibility requirements, lack of knowledge, or because they have private insurance. The main objective of the current study was to investigate the capability of tribe linkage to enhance the quality of racial information in the Michigan cancer registry.
Methods
To protect the identity of the participating tribe, it is not referred to by name. This study was approved by the participating Tribal Council, the Michigan Department of Community Health (MDCH), and the University of Michigan Institutional Review Board.
Data on incident cancers from the Detroit area are collected by the Surveillance Epidemiology and End Results (SEER) Program. Data for the rest of the state are collected through the National Program of Cancer Registries (NPCR). Reports to NPCR and SEER are made by hospitals, laboratories, physicians, dentists, clinics, and other state registries, and via death certificates. For this study, a data set containing all reported cancers diagnosed in Michigan from 1985 to 2004 was prepared in the standard North American Association of Central Cancer Registries format. The state data set contained 1,031,168 cancer diagnoses, representing 923,391 individuals. Less than 0.1% of registry cases had missing date of birth, last name, first name, or gender; 3.6% were missing social security number.
Tribal enrollment information is collected passively from all individuals claiming tribal ancestry. There are no quantum requirements for ancestry; individuals need to have only proof of an ancestor who was a member of the tribe. The tribe began collecting electronic information on its members in 1998. For the current study, a data set containing all tribal members enrolled from 1998 to 2007 was prepared, containing 40,340 individuals. Less than 0.1% of the tribe members had missing date of birth, last name, first name, gender, or social security number.
The linkage was conducted on July 20, 2007, at the tribe’s administration building on the tribe’s computer, accessing the state cancer data from a password-protected external hard drive. The data linkages were conducted using Registry Plus™ Link Plus 2.0, a free probabilistic linkage software program developed by the CDC. Below, the technical details used in this linkage are described. Blocking variables included social security number (SSN; method: New York State Identification and Intelligence System [NYSIIS], Phonetic Encoder); date of birth (DOB; method: NYSIIS); first name; and last name. Matching variables included SSN (method: SSN); DOB (method: date); first name (method: first name); last name (method: last name); middle name (method: middle name); and gender (method: exact). Some of the fields included for manual review were street address, city, state, and ZIP from both the registry and the tribe, as well as year of death, year of diagnosis, and cancer site from the registry alone.
Four people, representing state, tribe, and study personnel, conducted manual review of all possible linkages, called clericals. Registry Plus Link Plus assigns a score to each clerical, generated by the probability of matching variable agreement given a true match, reduced by the probability of agreement given a false match,9 aggregated across all the matching variables used. A higher score indicates a higher probability of a true match. The reviewers set upper and lower clerical cutoffs at 17.0 and 11.6, respectively, accepting all clericals above 17.0 as matches and rejecting all clericals below 11.6. Clericals with scores in the range 11.6–17.0 were manually reviewed by four reviewers, who unanimously agreed on all decisions about matches. A recent study10 recommended an upper clerical cutoff of 16.0, which conferred a positive predictive value of 94.6%. By comparison, the cutoff of 17.0 for this analysis is conservative.
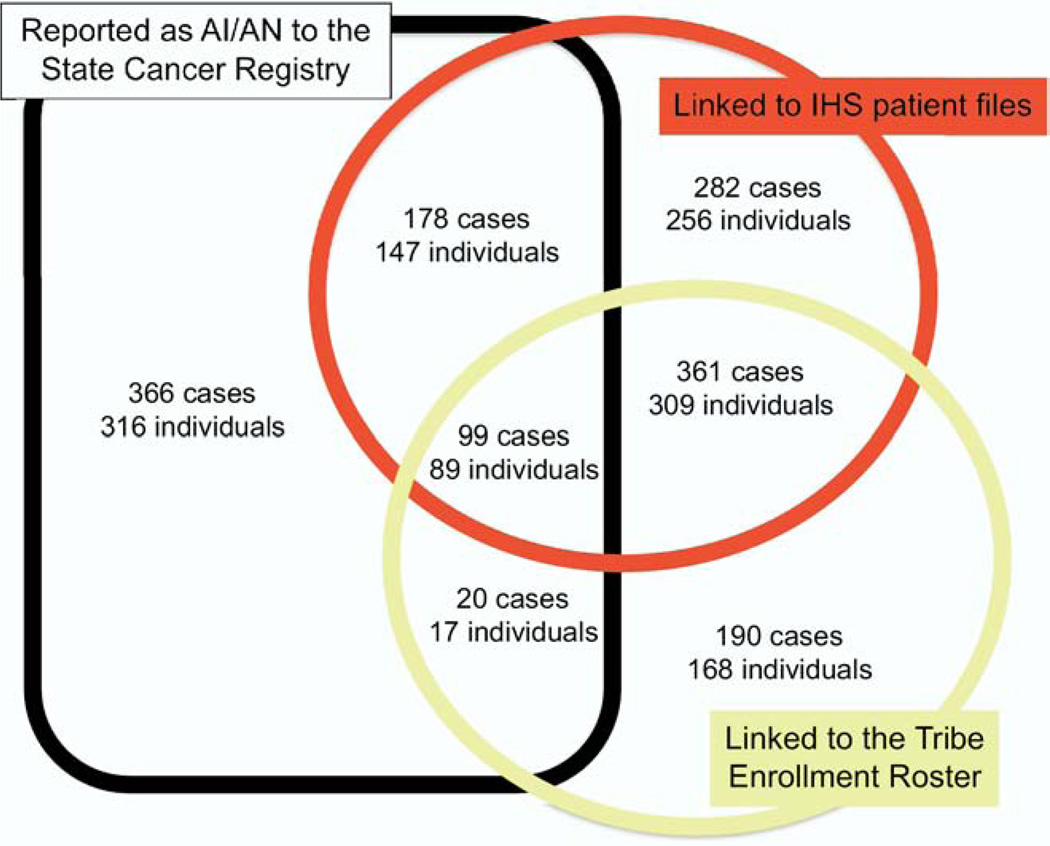
The only field output for all true matches was cancer registry patient identification. After merging this field back with the cancer registry, a data set was created containing all individuals originally reported as AI/AN, those who linked with IHS, and those who linked with the tribe (Figure 1). Lastly, a unique identifier was created as a substitute for patient identification, and all personal identifiers were dropped. The tribe and MDCH each have a copy of the de-identified data set produced by this linkage.
Figure 1.
American Indian/Alaska Native (AI/AN) malignant cancer cases and individuals by reported race and linkage status, 1995–2004
IHS, Indian Health Service
Racial misclassification may be a product of both individual characteristics and the ecologic makeup of the area where the diagnosis is made. For this reason, county-level characteristics were included in the analysis. All county-level characteristics were pulled from the SEER*Stat county attributes file.8 To protect confidentiality, county attributes were merged to the linkage data set, and the county variable was then dropped. Consistent with SEER and MDCH,11,12 an invasive cancer case was defined as any newly diagnosed cancer with a behavior code of 3 (malignant primary site); all urinary bladder cancer cases are included.
The U.S. Census American Factfinder was used to obtain the number of individuals identifying as “AI/AN Alone” living in Michigan by gender and age for the Year 2000 (Decennial Census). Individuals were grouped into 5-year age intervals from 0 to 85. Age-adjusted annual cancer incidence rates were externally standardized to the Year 2000 U.S. standard population,13 using Poisson regression to obtain 95% CIs around estimates. For comparison, the Michigan All Races rate was obtained from the Michigan Resident Cancer Incidence File and the U.S. All Races rate from a SEER report from 1975 to 2004.14
Demographic variables used for analysis included gender and age. Diagnostic variables included tumor confirmation type, cancer report source, and stage at diagnosis. Variables related to the county of diagnosis included urbanicity, the tribe’s service area, county CHS status, and quintile of percentage of AI/AN residents.
All statistical analyses were conducted using SAS 9.1.3, in 2007–2008. Separate models were fitted comparing (1) individuals reported as non-AI/AN but identified through IHS linkage to those reported as AI/AN and (2) individuals reported as non-AI/AN but identified through the tribe link to those reported as AI/AN. Model 1 contains individual-level predictors only. Model 2 contains county-level predictors only. Using the parameter estimates and t- and F-test statistics, predictors that contributed to Models 1 and 2 were included in the multilevel analysis (Model 3).
Results
Summary
Of the 1496 AI/AN cancer cases (1302 individuals) reported from 1995 to 2004, a total of 663 cases (569 individuals) were reported to the registry as AI/AN; 920 cases (801 individuals) linked with the IHS patient files; and 670 cases (583 individuals) linked to the tribe enrollment roster (Figure 1). Of 583 tribe members in the cancer registry, 574 were reported as uniracial (98.5%); two as biracial (0.3%); and seven as having an unknown race (1.2%). For those who reported one race only, 467 were reported as white (81.4%); 104 as AI/AN (18.1%); and three as Asian, Indian, Pakistani, other, or unknown race (0.5%). Of the 801 IHS patients, 792 individuals were reported as uniracial (98.9%); one as biracial (0.1%); and eight as having an unknown race (1.0%). For those who reported one race only, 544 were reported as white (68.7%); 235 as AI/AN (29.7%); and 14 (1.8%) as black, Chinese, Japanese, Asian, Indian, Pakistani, or other race.
Linkage Diagnostics
For tribe-registry links, the mean score was 31.22, with a range from 14.40 to 36.50. The score increased as the diagnosis year increased (B=0.122, p<0.001). Because the tribe’s data set was dated 2007, the tribe’s information was expected to be more similar to the registry information in more recent years.
Incidence
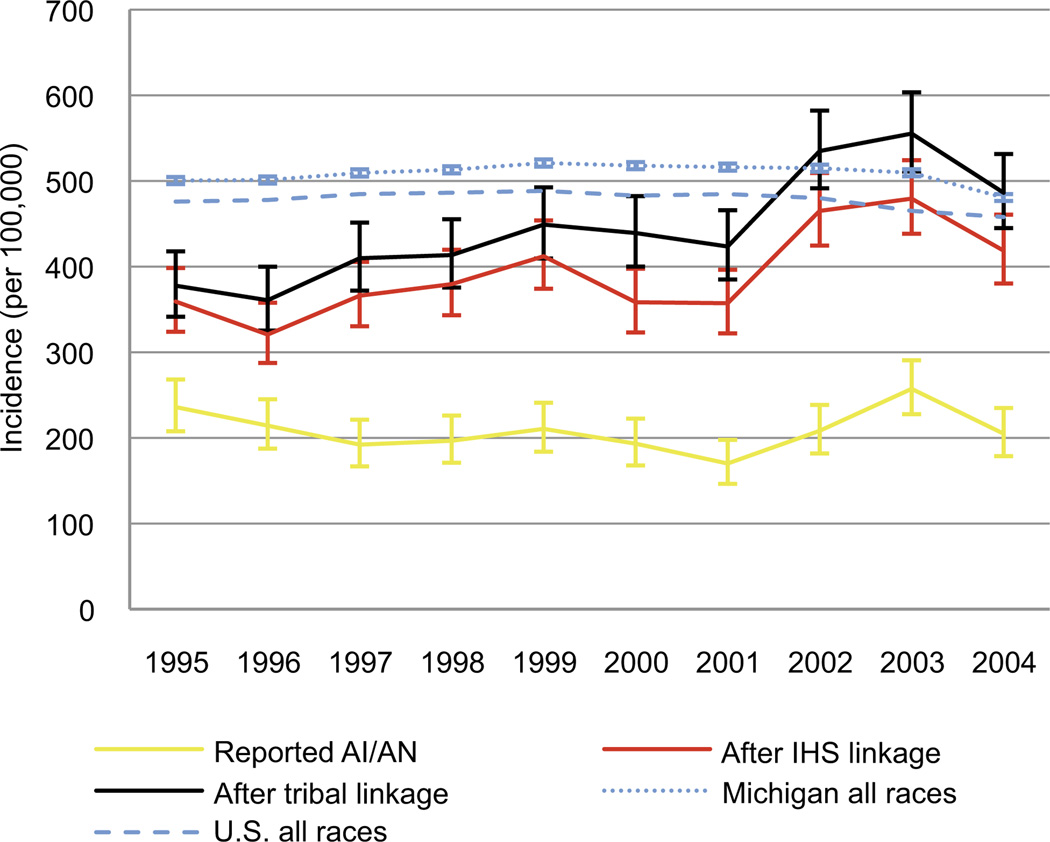
Figure 2 shows the age-adjusted annual incidence rate of invasive cancer from 1995 to 2004. For each diagnosis year, both IHS and tribal linkage result in the identification of racially misclassified individuals. Including only individuals reported as AI/AN, the incidence rate for the Michigan AI/AN population is <60% the incidence rate for Michigan All Races rate for each year, 1995–2004.
Figure 2.
Age-adjusted annual invasive cancer incidence rate by identification type
AI/AN, American Indian/Alaska Native; IHS, Indian Health Service
Models
Table 1 describes the association between outcomes and predictors of interest. Including individual-level predictors only (Model 1), those identified by IHS linkage were less likely than those reported as AI/AN to have regional tumor extension and more likely to have histologic tumor confirmation or to have been reported by hospital inpatient medical records or a managed healthcare organization with unified medical records. Including county-level predictors only (Model 2), those identified by IHS linkage were more likely than those reported as AI/AN to be reported in a CHS county and in the tribe’s service area. These findings remained relatively unchanged, in terms of direction and magnitude in the multilevel model (Model 3).
Table 1.
Multivariate models for AI/AN individuals reported as non-AI/AN, compared to those reported as AI/AN (1995–2004)
| Linked to IHS patient files (n=565) | Linked to tribal roll (n=168) | |||||
|---|---|---|---|---|---|---|
| Model 1 OR pa |
Model 2 OR pa |
Model 3 OR pa |
Model 1 OR pa |
Model 2 OR pa |
Model 3 OR pa |
|
| Individual-level variables | ||||||
| Male | 0.90 (p=0.511) |
0.70 (p=0.112) |
||||
| Aged >65 years | 0.88 (p=0.886) |
0.74 (p=0.196) |
||||
| Regional tumor extensionb |
0.26 (p=0.003) |
0.25 (p=0.029) |
0.53 (p=0.023) |
0.70 (p=0.029) |
||
| Distant tumor extensionb |
0.45 (p<0.001) |
0.42 (p<0.001) |
0.71 (p=0.204) |
0.54 (p=0.190) |
||
| Histologic tumor confirmationc |
2.01 (p=0.025) |
1.94 (p=0.032) |
2.71 (p=0.041) |
3.09 (p=0.020) |
||
| Report by hospital inpatient medical records or managed healthcare organization with unified medical recordsd | 1.87 (p=0.068) |
1.85 (p=0.072) |
0.99 (p=0.985) |
|||
| County-level variables | ||||||
| Diagnosed in an urban, nonmetropolitan areae | 0.97 (p=0.930) |
0.72 (p=0.328) |
||||
| Diagnosed in a completely rural areae | 0.71 (p=0.452) |
0.82 (p=0.712) |
||||
| Diagnosed in a CHSDA countyf |
2.41 (p=0.005) |
2.31 (p=0.004) |
0.51 (p=0.052) |
0.37 (p=0.007) |
||
| Diagnosed in the tribe’s service area |
3.05 (p=0.002) |
2.41 (p=0.023) |
6.32 (p=0.003) |
5.98 (p=0.008) |
||
| Diagnosed in a county with 0.54%–0.75% AI/AN residents (second quintile)6 | 1.60 (p=0.214) |
1.24 (p=0.581) |
1.24 (p=0.605) |
|||
| Diagnosed in a county with 0.75%–2.28% AI/AN residents (third quintile)g | 1.73 (p=0.162) |
1.05 (p=0.908) |
1.01 (p=0.989) |
|||
| Diagnosed in a county with 2.28%–13.04% AI/AN residents (fourth quintile)g | 1.38 (p=0.503) |
0.13 (p=0.099) |
0.27 (p=0.0436) |
|||
| Diagnosed in a county with >13.04% AI/AN residents (highest quintile)g | 0.85 (p=0.829) |
0.04 (p=0.001) |
0.05 (p=0.003) |
|||
t/F-test Pr> |t/F|
Compared to localized or in situ
Compared to positive cytology without histology; positive microscopic confirmation, unspecified; direct visualization or radiography/imaging without microscopic diagnosis; and clinical diagnosis only
Compared to report by lab only, physician’s office, nursing home, or hospice, or death certificate only
Compared to being diagnosed in an urban, nonmetropolitan area
Compared to non-CHSDA
Quintiles; compared to the lowest quintile: counties with <0.54% AI/AN residents
AI/AN, American Indian or Alaska Native; CHSDA, Indian Health Service Contract Health Services Delivery Area; IHS, Indian Health Services
Including individual-level predictors only (Model 1), those identified by the 2007 tribal linkage were less likely than those reported as AI/AN to have regional tumor extension and more likely to have histologic tumor confirmation. Including county-level predictors only (Model 2), those identified by the 2007 tribal linkage were more likely than those reported as AI/AN to be diagnosed in the tribe’s service area and less likely to be diagnosed in a CHS county or in a county with the highest quintile of AI/AN residents. These findings remained relatively unchanged, in terms of direction and magnitude, in the multilevel model (Model 3).
Because the parameters in Model 3 were similar in direction and magnitude to the parameters in Models 1 and 2, there was no evidence for cross-level confounding by any of the variables measured. This fact does not preclude the effects of modifying variables (not evaluated) or unmeasured confounders.
Discussion
Incidence
The most important finding of this study is that link-ages are effective at enhancing the quality of race data in this cancer registry. The IHS linkages from 1995 to 2004 led to the identification of 643 racially misclassified AI/AN cancer cases, a 97% increase. The 2007 tribe link led to the identification of an additional 190 racially misclassified AI/AN cancer cases, a 15% increase. A similar linkage between the Washington State cancer registry, IHS patient files, and 19 tribal rolls in the early 1990s resulted in a greatly increased AI/AN incidence rate; however, very few AI/AN cancer cases were identified through tribal linkage that were not also included in IHS patient files.15 The current study is the first the authors have seen to show that linkage with large tribal rolls can improve identification of AI/AN individuals, above and beyond annual IHS linkages. With each data linkage, the Michigan AI/AN cancer incidence rate verges on, and even outpaces, national and state averages.
The utility of race in medicine has been questioned of late, largely because of its ambiguity and lack of validity as a biological construct.13,16 The classification of race into a handful of standard categories conceals the considerable heterogeneity within races17,18 and among individuals reporting one or multiple races.19,20 The development of American-Indian self-identity is exceedingly complex and is likely influenced by a number of factors, including tribal culture, age, and social support.21 Nonetheless, race remains an important social construct, which makes it of great interest to researchers of population health. Moreover, race-specific incidence patterns are used to allocate support for cancer-prevention and detection programs. For these reasons, the validity of race-specific incidence data, albeit imperfect, is of great import.
Description
The diagnostic and ecologic characteristics of individuals identified via linkages are different than those reported as AI/AN by the registry. Individuals identified by data linkages had earlier-stage cancer and were more likely to have histologic tumor confirmation than individuals who were reported as AI/AN. These differences have clear implications for mortality data. Related research has found that demographic factors, such as education, employment, and marital status, are predictive of disagreement between medical records and selfreported race/ethnicity in other populations.4,22
Limitations
There are several limitations to this research. First, data collection methods for cancer registry reports and the Census are very different. Although both are populationbased estimates, individuals reported to the cancer registry are not actually responding on their own behalf, whereas those reporting to the Census are. The goal of these data linkages is to more closely approximate a self-reported race for AI/AN cancer patients than do medical reports, which have been shown to have little agreement with self-reported AI/AN race.3,4
A major problem with differences in data collection is related to the number of races reported. The 2000 Census allowed respondents to identify with up to six races. Although the cancer registry allows reports to contain up to five races, less than 2% of reports used these extra categories. Incidence rate calculations used the Census group identifying as AI/AN Alone as the denominator, making the assumption that those individuals identified as AI/AN by their report source or linkage are from the same base population that identifies as AI/AN Alone on the Census. Because member-ship in an American Indian tribe has certain incentives, some individuals who do not identify as American Indian Alone may, in fact, be tribe members.
The validity of incidence rate calculations was assessed by comparing results to that of a recent report to the nation. Espey and colleagues23 found that the average age-adjusted annual cancer incidence rate from 1999 to 2004 for AI/AN in the Northern Plains was 611.4 per 100,000 men and 468.1 per 100,000 women. These estimates are comparable to the estimates from this study, often contained in 95% CIs. Lastly, this data linkage included only one Michigan tribe; there are 11 other federally recognized tribes in Michigan.24 Even with these linkages, members of non-Michigan tribes would still be missed.
Strengths
This research study shows that tribal linkages are not only possible but also easy to accomplish when members from tribe, state, and academic institutions collaborate. The link itself takes hours to days to complete, depending on computing resources and the size of the files used. The linkage software is user-friendly and free. In addition to improving data quality for AI/AN individuals in the cancer registry, data linkages can provide tribe-specific cancer statistics, an invaluable resource for tribal health-services planning. Although the numbers contained in this data set are small, it will help inform the leaders of the tribe in their efforts to improve the health of their people. Lastly, the incidence calculations presented in this report can be used to more accurately allocate cancer prevention resources in Michigan.
Confidentiality of data is a high priority for all parties involved. Those involved on both sides agreed on data management and storage practices at the outset of this project. Data linkages such as these help build trust between administrators of tribe and state and, when done properly, promote future collaboration.
Undercounting of AI/AN in disease registries poses a serious problem for resource allocation and prioritization of public health efforts. In order to truly understand cancer in minority populations, data quality on race is critical. Administrators at tribe, state, and academic institutions must collaborate to improve data quality and capability to control cancer in special populations.
Acknowledgments
We want to especially thank Dr. David Espey and Melissa Jim of the CDC and Indian Health Service for their training, support, and technical assistance on this project. Jennifer Johnson was supported by the Cancer Epidemiology Education in Special Populations Program of the University of Michigan (R25-CA 12383). We express our gratitude to the Network for Cancer Control Research Among American Indian and Alaska Native Populations and the Mayo Clinic for their mentorship, and to Kathy Welch at the University of Michigan Center for Statistical Research and Consultation, for statistical assistance. We thank Dr. Hal Morgenstern and Dr. Sandro Galea at the University of Michigan School of Public Health for their comments on an earlier version of the manuscript.
Footnotes
No financial disclosures were reported by the authors of this paper.
References
- 1.Swan J, Edwards K. Cancer rates among American Indians and Alaska Natives: is there a national perspective? Cancer. 2003;98:1262–1272. doi: 10.1002/cncr.11633. [DOI] [PubMed] [Google Scholar]
- 2.Puukka E, Stehr-Green P, Becker TM. Measuring the health status gap for American Indians/Alaska Natives: getting closer to the truth. Am J Public Health. 2005;95:838–843. doi: 10.2105/AJPH.2004.053769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boehmer U, Kressin NR, Berlowitz DR, Christiansen CL, Kazis LE, Jones JA. Self-reported vs administrative race/ethnicity data and study results. Am J Public Health. 2002;92:1471–1472. doi: 10.2105/ajph.92.9.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kressin NR, Chang BH, Hendricks A, Kazis LE. Agreement between administrative data and patients’ self-reports of race/ethnicity. Am J Public Health. 2003;93:1734–1739. doi: 10.2105/ajph.93.10.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McAlpine DD, Beebe TJ, Davern M, Call KT. Agreement between selfreported and administrative race and ethnicity data among Medicaid enrollees in Minnesota. Health Serv Res. 2007;42:2373–2388. doi: 10.1111/j.1475-6773.2007.00771.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat 2. 1999;128:1–13. [PubMed] [Google Scholar]
- 7.USDHHS, Indian Health Service. Indian Health Service Fact Sheet. 2006 www.ihs.gov/PublicInfo/PublicAffairs/Welcome_Info/ThisFacts.asp.
- 8.National Cancer Institute, Surveillance Epidemiology and End Results, County attributes. 2008 www.seer.cancer.gov/seerstat/variables/countyattribs/.
- 9.Fellegi IP, Sunter AB. A theory for record linkage. J Am Stat Assoc. 1969;64:1183–1210. [Google Scholar]
- 10.Campbell KM, Deck D, Krupski A. Record linkage software in the public domain: a comparison of Link Plus, the Link King, and a ‘basic’ deterministic algorithm. Health Informatics J. 2008;14:5–15. doi: 10.1177/1460458208088855. [DOI] [PubMed] [Google Scholar]
- 11.National Cancer Institute, Surveillance Epidemiology and End Results. Accessing datasets and tools: SEER behavior recode for analysis. seer.cancer.gov/behavrecode/index.html.
- 12.Michigan Department of Community Health. Invasive cancer incidence and mortality trends, Michigan residents, 1985–2006. www.mdch.state.mi.us/pha/osr/cancer/stateinc.asp?cdxid=inctrendstotal. [Google Scholar]
- 13.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47:1–17. [PubMed] [Google Scholar]
- 14.Ries LAG, Melbert D, Krapcho M, et al., editors. SEER cancer statistics review, 1975–2004. National Cancer Institute. 2007 seer.cancer.gov/csr/1975_2004/.
- 15.Sugarman J, Holliday M, Ross A, Castorina J, Hui Y. Improving American Indian cancer data in the Washington State cancer registry using linkages with the Indian Health Service and tribal records. Cancer Suppl. 1996;78:1564–1568. [PubMed] [Google Scholar]
- 16.Witzig R. The medicalization of race: scientific legitimization of a flawed social construct. Ann Intern Med. 1996;125:675–679. doi: 10.7326/0003-4819-125-8-199610150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Becker TM, Espey DK, Lawson HW, Saraiya M, Jim MA, Waxman AG. Regional differences in cervical cancer incidence among American Indians and Alaska Natives, 1999–2004. Cancer. 2008;113:1234–1243. doi: 10.1002/cncr.23736. [DOI] [PubMed] [Google Scholar]
- 18.Wallace DC, Torroni A. American Indian prehistory as written in the mitochondrial DNA: a review. Hum Biol. 1992;64:403–416. [PubMed] [Google Scholar]
- 19.Pleis JR, Barnes PM. A comparison of respiratory conditions between multiple race adults and their single race counterparts: an analysis based on American Indian/Alaska Native and white adults. Ethn Health. 2008;13:399–415. doi: 10.1080/13557850801994839. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton BE, Ventura SJ. Characteristics of births to single- and multiple-race women: California, Hawaii, Pennsylvania, Utah, and Washington, 2003. Natl Vital Stat Rep. 2007;55:1–20. [PubMed] [Google Scholar]
- 21.Whitesell NR, Mitchell CM, Kaufman CE, Spicer P the Voices of Indian Teens Project Team. Developmental trajectories of personal and collective self-concept among American Indian adolescents. Child Dev. 2006;77:1487–1503. doi: 10.1111/j.1467-8624.2006.00949.x. [DOI] [PubMed] [Google Scholar]
- 22.Swallen KC, West DW, Stewart SL, Glaser SL, Horn-Ross PL. Predictors of misclassification of Hispanic ethnicity in a population-based cancer registry. Ann Epidemiol. 1997;7:200–206. doi: 10.1016/s1047-2797(96)00154-8. [DOI] [PubMed] [Google Scholar]
- 23.Espey DK, Wu X, Swan J, et al. Annual report to the nation on the status of cancer, 1975–2004, featuring cancer in American Indians and Alaska Natives. Cancer. 2007;110:2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- 24.Kushman C. Michigan’s federally recognized tribes. Sault Ste Marie MI: Inter-Tribal Council of Michigan, Inc.; 2007. [Google Scholar]