Abstract
Traditional cytogenetic studies of ovarian stromal tumors are few, although trisomy 12 has been frequently documented utilizing fluorescence in-situ hybridization (FISH). In the current study, karyotypic analysis of four ovarian stromal tumors and a review of the literature suggested that numerical abnormalities of chromosomes 4 and 9 might also be important, possibly as secondary changes. To determine the frequency of 4, 9, and 12 aneuploidy in a larger group of ovarian tumors, FISH studies were performed on eight fibromas, three thecomas, one fibrothecoma, and five cellular fibromas. Trisomy 12 was identified in all five cellular fibromas as well as in two fibromas and the fibrothecoma. Gain of chromosome 9 was confined to the cellular fibromas. Loss of chromosomes 4 and/or 9 were prominent in the fibromas. These findings confirm the presence of trisomy 12 as a nonrandom chromosomal abnormality in ovarian stromal tumors. Moreover, these conventional and molecular cytogenetic data indicate that gain of chromosome 9 in addition to gain of chromosome 12 is prominent in cellular fibroma. In contrast, loss of chromosomes 4 and/or 9 are recurrent in fibroma. In summary, imbalances of chromosomes 4 and 9 appear to represent important secondary abnormalities in the thecoma-fibroma ovarian tumor group.
INTRODUCTION
The thecoma-fibroma group of ovarian stromal tumors represent a spectrum of neoplasms composed entirely of lipid-containing cells resembling theca interna cells to those containing predominantly spindle-shaped cells with variable intercellular collagen. This group of neoplasms derived from ovarian mesenchyme accounts for approximately 5-8% of all ovarian neoplasms.[1] The majority of ovarian thecomas arise in postmenopausal women and some may produce considerable quantities of estrogen resulting in abnormal uterine bleeding.[2] Ovarian fibromas are most frequent in middle age women. Notably, ovarian fibromas are also a common feature of Gorlin syndrome [nevoid basal cell carcinoma syndrome (NBCCS)]; approximately 75% of females with Gorlin syndrome (localized to 9q22.3) have ovarian fibromas.[3,4] The fibromas in Gorlin syndrome are usually bilateral, heavily calcified, and are seen in a younger age patient.
Conventional cytogenetic studies of ovarian stromal tumors are few.[5-17] These sparse karyotypic studies, and additional FISH analyses, have revealed extra copies (trisomy and tetrasomy) of chromosome 12 as a recurrent anomaly in this ovarian tumor subset.[1,5-23] In the current study, cytogenetic and molecular cytogenetic evaluation of 17 benign ovarian tumors (eight fibromas, three thecomas, one fibrothecoma, and five cellular fibromas) and a review of the literature [1,5-23], indicate that numerical imbalances of chromosomes 4 and 9 also represent nonrandom alterations in the thecoma-fibroma group of ovarian stromal tumors.
METHODS
Tumor Samples
Sixteen tumors of the ovarian thecoma-fibroma group were obtained from the surgical pathology files of the Department of Pathology and Microbiology, University of Nebraska Medical Center and one was obtained from the Department of Pathology, Creighton Medical Center. All tumors were diagnosed according to the World Health Organization histological criteria for ovarian stromal tumors [4] and included the following: eight fibromas, three thecomas, one fibrothecoma, and five cellular fibromas. The clinicohistopathologic features of the patients and corresponding tumors are listed in Table 1. The patient ages ranged from 12 to 86 years of age; the average age was 53 years. The average age of the patients with thecomas was 65 years, compared to 47 and 54 years of age for the patients with fibromas and cellular fibromas, respectively. The fibroma from Case 6 arose in a patient with Gorlin syndrome; the remaining tumors were sporadic and unilateral.
Table 1.
Clinicopathologic, Cytogenetic and Molecular Cytogenetic Findings of Current Study
| Case # | Age | Diagnosis | Size (cm) | Karyotype | Chromosome Copy Number (FISH Analysis) | Reference | ||
|---|---|---|---|---|---|---|---|---|
| Chrom. 4 | Chrom. 9 | Chrom. 12 | ||||||
| 1 | 28 | Cellular Fibroma | 4 | 64-65,XXX,-1[3],-5[4],+6[2],-7[4],+10[4],-11[4],+12[4],-13[4],-16[4],-17[4],+21[3],-22[4][cp4]/46,XX[19] | N | N | + | Current study |
| 2 | 49 | Cellular Fibroma | 16 | 49,XX+9,+12,+20[20] | - | + | + | Current study |
| 3 | 72 | Cellular Fibroma | 10 | NP | N | + | + | Current study |
| 4 | 37 | Cellular Fibroma | 8.5 | 67,X,-X,-X,-1,+3,-4,-7,+9,-11,+12,+13,+15,-16,+18,-22,[14]/46,XX[6] | - | + | + | Current study |
| 5 | 86 | Cellular Fibroma | 16 | NP | N | N | + | Current study |
| 6 | 12 | Fibroma* | 10 | 46,XX | - | N | N | Current study |
| 7 | 28 | Fibroma | 10.1 | NP | - | - | N | Current study |
| 8 | 84 | Fibroma | N/A | NP | + | N | + | Current study |
| 9 | 60 | Fibroma | 10 | NP | - | N | - | Current study |
| 10 | 51 | Fibroma | 1.5 | NP | - | N | N | Current study |
| 11 | 70 | Fibroma | 1 | NP | - | - | N | Current study |
| 12 | 26 | Fibroma | 5 | NP | - | - | + | Current study |
| 13 | 41 | Fibroma | 7 | NP | - | N | N | Current study |
| 14 | 67 | Fibrothecoma | 7 | NP | + | N | + | Current study |
| 15 | 41 | Thecoma | 6 | NP | NR | NR | NR | Current study |
| 16 | 79 | Thecoma | 0.8 | NP | NR | NR | NR | Current study |
| 17 | 75 | Thecoma | 1 | NP | NR | NR | NR | Current study |
Gorlin syndrome patient; N/A = not available; N = normal; NR = no results; NP = not performed
Cytogenetic analysis
Representative samples of three cellular fibromas and one fibroma (Cases 1, 2, 4, and 6) were submitted for cytogenetic analysis. Standard culture and harvest procedures were performed as described previously. [24] Briefly, the tissue was disaggregated mechanically and enzymatically and cultured in RPMI 1640 media supplemented with 20% fetal bovine serum for 3 to 6 days. Cells were exposed to an overnight treatment of Colcemid (0.02 ųg/ml). After subsequent hypotonic treatment (0.7% sodium citrate for 20 min), the preparations were fixed three times with methanol and glacial acetic acid (3:1). Metaphase cells were banded with Giemsa trypsin. The karyotypes were described according to the International System for Human Cytogenetic Nomenclature. [25]
Molecular cytogenetic analysis
Tricolor interphase FISH studies using chromosome enumeration probes specific for chromosomes 4, 9, and 12 (CEP; Vysis, Des Plaines, IL) were performed on the cytologic touch preparation and the formalin-fixed, paraffin-embedded tissue sections of the 17 benign ovarian stromal tumors. Pretreatment of the slides prior to hybridization included the following: each slide was immersed in Hemo-De three times for 5 minutes, 95% ethanol twice for 1 minute, 0.2N hydrochloric acid for 20 minutes, followed by rinsing in purified water for 3 minutes, immersing in 80°C 1M sodium thiocyanate (NaSCN) solution for 15 minutes, washing in purified water for 3 minutes, and immersing for 10 minutes in a 37°C protease solution composed of 50ml protease buffer (Vysis) with 25mg protease. Subsequently, the slides were dehydrated in 70%, 85%, and 95% ethanol for 1 minute each and allowed to air dry.
Hybridization was performed according to the manufacturer’s instructions. Briefly, for each slide the following probe mixture was used: 1μl CEP 4, 1μl CEP 12, 0.5μl CEP 9, 0.5μl distilled water, and 7μl LSI/WCP hybridization buffer (Vysis). The slides were placed on a pre-warmed HYBrite, for a 5 minute denaturation period at 80°C followed by a 14-18 hour hybridization period at 37°C. Posthybridization, the slides were washed in 72°C 0.4 × SSC/0.3% NP40 for 2 minutes, followed by a second 2 minute wash in 2 × SSC/0.1% NP40 at ambient temperature. Following air-dyring, 10μl of 4,6-diamidino-2-phenylindole (DAPI II) counterstain was added to each slide and sealed with a 22×50mm glass coverslip. The hybridized slides were stored at -20°C.
Analysis of the CEP probes was performed using an Olympus BX51 fluorescent microscope. Strong, well-delineated aqua, orange, and green hybridization signals were assessed in 200 interphase nuclei per case by two different individuals. An interphase cell specimen was interpreted as abnormal if the copy number for a chromosome 4, 9, and/or 12 CEP probe signal(s) was greater than two signals per probe in more than 20% of the cells evaluated or less than two signals per probe in 30% of the cells evaluated (more than two standard deviations above the average false-positive rate). Histopathologically normal paraffin-embedded ovarian tissue was used as a normal control.
RESULTS
Traditional karyotypic analysis revealed clonal abnormalities in three of the four specimens analyzed. FISH studies were successfully performed on all but 3 cases. Prolonged exposure to formalin may be responsible for the three failed hybridizations despite repeated efforts.
The cytogenetic and molecular cytogenetic findings are summarized in Table 1. Aneuploidies of chromosomes 4, 9, and 12 were detected cytogenetically in three of the five cellular fibromas (Figures 1 and 2). Molecular cytogenetic studies revealed extra copies of chromosome 12 in all five cellular fibromas (Figure 3A), two of 8 fibromas and the fibrothecoma (Figure 3B). Extra copies of chromosome 9 were observed only in the cellular fibromas (Figure 3A). In contrast, loss of chromosomes 4 and 9 were prominent in the fibromas, with seven of eight fibromas showing loss of chromosome 4 and three of eight showing a loss of chromosome 9 (Figures 3C and D).
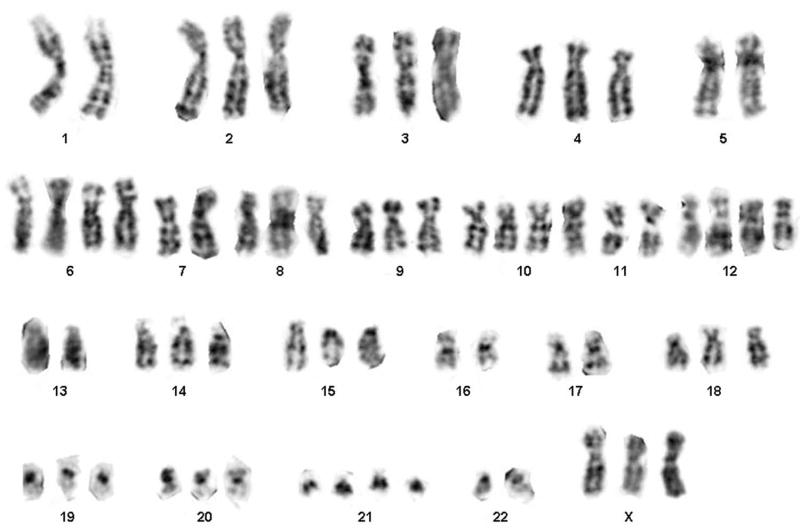
Figure 1.
Representative karyotype of Case 1 exhibiting the following abnormal complement: 64-65,XXX,-1,-5,+6,-7,+10,-11,+12,-13,-16,-17,+21,-22.
Figure 2.
Representative karyotype of Case 4 exhibiting the following abnormal complement: 67,X,-X,-X,-1,+3,-4,-7,+9,-11,+12,+13,+15,-16, +18,-22.
Figure 3.
FISH analyses on representative paraffin-embedded tissue sections with chromosome 4 (aqua), 9 (orange), and 12 (green) CEP probes reveals: (A) gain of chromosomes 9 and 12 in Case 3 (cellular fibroma); (B) gain of chromosomes 4 and 12 in Case 14 (fibrothecoma); (C) loss of chromosomes 4 and 9 (arrow) in Case 7 (fibroma); and, (D) loss of chromosomes 4 and 9 (single aqua and orange signal in abnormal cells indicated by arrows) and gain of chromosome 12 (3-4 green signals in abnormal cells indicated by arrows) in Case 12 (fibroma).
DISCUSSION
Conventional cytogenetic and molecular cytogenetic studies have shown that the most consistent and often sole anomaly in benign ovarian stromal tumors is the presence of extra copies of chromosome 12. [1,5-23] In this study, karyotypic analysis of four ovarian stromal tumors of the thecoma-fibroma group and a review of the literature suggested that aneuploidy for chromosomes 4 and 9 might also be recurrent and represent secondary events in these neoplasms. [6,8,10,14,17] These findings prompted our evaluation of a larger and more histologically diverse cohort of the thecoma-fibroma group of ovarian tumors by fluorescence in situ hybridization. FISH analysis, using centromeric probes, is a valuable approach for detection of numerical chromosomal abnormalities in archival tissue (formalin-fixed, paraffin-embedded tissue).
In the current report, the presence of extra copies of chromosome 12 was confirmed as a nonrandom chromosomal abnormality in 8 (57%) of 14 benign ovarian stromal tumors by cytogenetic and/or FISH analyses. In addition, loss of chromosome 4 and gain of chromosome 9 was identified in two (40%) and three (60%) of five cellular fibromas respectively. Loss of chromosome 4 was also prominent in fibroma [7 (88%) of 8 specimens], but in contrast to cellular fibromas, loss not gain of chromosome 9 [3 (38%) of 8 specimens] was observed.
Karyotypic data from previous studies, presented in Table 2, show only one cellular fibroma has previously been subjected to cytogenetic analysis and this case showed tetrasomy 12 as the sole anomaly. [16] Trisomy 12 has also been observed as the sole anomaly in prior cytogenetic reports of thirteen ovarian fibromas, fibrothecomas and thecomas. [5-9,11,12] Gain of chromosomes 4 and/or 9 have also been documented in six fibromas, fibrothecomas and thecomas in addition to two cellular fibromas of the present study. [6,8,10,14,17] Overall, most abnormal karyotypes in benign ovarian stromal tumors have been hyperdiploid, but a few (including two in the current study) have exhibited near triploid complements.
Table 2.
Clinicopathologic and Cytogenetic Findings of Previously Reported Cases
| Case # | Age | Diagnosis | Size (cm) | Karyotype | Reference |
|---|---|---|---|---|---|
| 1 | 44 | Cellular Fibroma | N/A | 48,XX,+12,+12 | Liang, et al (2001)[12] |
| 2 | N/A | Fibroma | 14 | 47,XX,+12 | Pejovic, et al (1990) [2] |
| 3 | N/A | Fibroma | 28 | 47,XX,+12 | Pejovic, et al (1990) [2] |
| 4 | N/A | Fibroma | N/A | 47,XX,+12 | Samuelson, et al (1988) [1] |
| 5 | 40 | Fibroma | 2 | 47,XX,+12 | Fletcher, et al (1991) [4] |
| 6 | 60 | Fibroma | 10.5 | 47,XX,+12 | Fletcher, et al (1991) [4] |
| 7 | 12 | Fibroma* | 20 | 73,XXX,-2,del(2)(q31),+4,-11,?inv(11)(p15q21)x2,+12,+13,+14,+14,-16,-16,+18,+21,+21 | Smith, et al (2002) [13] |
| 8 | 77 | Fibroma | 6.5 | 47,XX,+12 | Leung, et al (1990) [3] |
| 9 | 56 | Fibroma | 8 | 47,XX,+12 | Leung, et al (1990) [3] |
| 10 | 48 | Fibroma | N/A | 47,XX,+12 | Gancberg, et al (2001) [5] |
| 11 | 85 | Fibrothecoma | 5.3 | 44,XX,dup(1)(p13p31),del(3)(p14),add(10p),-16,-22 | Izutsu, et al (1995) [9] |
| 12 | N/A | Fibrothecoma | 8 | 49,XX,+4,+9,+12 | Pejovic, et al (1990) [2] |
| 13 | 56 | Fibrothecoma | 6 | 53,XX,+6,+7,+9,+12,+14,+18,+19 | Fletcher, et al (1991) [4] |
| 14 | 47 | Fibrothecoma | 16 | 50,XX,+X,+4,+12,+12(6/12 w/additional trisomy 6) | Fletcher, et al (1991) [4] |
| 15 | 65 | Fibrothecoma | 7 | 46,XX | Fletcher, et al (1991) [4] |
| 16 | 66 | Fibrothecoma | 4 | 46,XX | Fletcher, et al (1991) [4] |
| 17 | 59 | Fibrothecoma | 3.3 | 47,XX,+12 | Fletcher, et al (1991) [4] |
| 18 | 70 | Fibrothecoma | 17.5 | 47,XX,+12 | Fletcher, et al (1991) [4] |
| 19 | 67 | Fibrothecoma | N/A | 45,XX,-22 | Dal Cin, et al (1997) [11] |
| 20 | N/A | Fibrothecoma | N/A | 57,XX,+4,+5,+6,+10,+12,+12,+14,+17,+18,+19,+20 | Dal Cin, et al (1992) [10] |
| 21 | 42 | Thecoma | 10 | 47,XX,+12 | Walter, et al (1993) [8] |
| 22 | 57 | Thecoma | 22 | 48,XX,+4,+12 | Mrozek, et al (1992) [6] |
Gorlin syndrome patient; N/A = not available; N = normal; NR = no results; NP = not performed
Loss of chromosome 9 copy number in a subset of the fibromas analyzed in this study is noteworthy because of the association of ovarian fibromas and Gorlin syndrome or nevoid basal cell carcinoma (NBCC). Gorlin syndrome is an autosomal dominant disorder featuring distinctive congenital malformations and a predisposition to a variety of benign and malignant neoplasms, including ovarian fibroma. [26-29] The gene for Gorlin syndrome, PTCH1, has been localized to 9q22.3 and is characterized as a tumor suppressor gene encoding for a transmembrane protein that functions as a receptor for sonic hedgehog. [30,31] To the best of our knowledge, only one other syndromic ovarian fibroma in addition to Case 6 of the current study has been subjected to cytogenetic analysis.[17] Interestingly, neither of these Gorlin syndrome ovarian fibromas exhibited loss of chromosome 9 cytogenetically, nor was chromosome 9 loss detected by FISH analysis in the current case. Notably however, three sporadically occurring ovarian fibromas did show loss of chromosome 9 by FISH analysis in the present series. In addition, a recent study examining loss of heterozygosity (LOH) using polymerase chain reaction (PCR) amplification at 9q22.3 revealed LOH at this locus in 4 of 6 sporadic cellular fibromas and 2 of 9 sporadic thecomas. [26] Contrary to our data, this same study also analyzed 8 fibromas all of which were found to be negative for LOH at 9q22.3. An additional study of LOH using PCR analysis, performed by Byrom and colleagues, of region of 9q22-31 showed LOH (either complete or sporadic) in 70.3% of 111ovarian tumors analyzed, revealing 6 of 9 fibromas to have LOH in this region. [32]
In summary, these data indicate that imbalances of chromosomes 4 and 9 represent important secondary changes in addition to trisomy 12 as the recurrent primary abnormality in the thecoma-fibroma group of ovarian stromal tumors. Moreover, heterozygous loss of one chromosome 9 homologue in three nonsyndromic ovarian fibromas suggests a somatic role of the PTCH1 tumor suppressor gene in these neoplasms. Additional studies of sporadic and syndromic ovarian tumors of the thecoma-fibroma group to include other technical approaches may expose an even higher frequency of PTCH1 loss or mutation.
Acknowledgments
The authors would like to thank Ms. Patti Cattano and Ming Zhou for their technical assistance and Ms. Kimberly Christian for her assistance in preparing the manuscript. This study was supported in part by NIH/NCI P30 CA 3672 and State of Nebraska LB595.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shashi V, Golden WL, von Kap-Herr C, Andersen WA, Gaffey MJ. Interphase fluorescence in situ hybridization for trisomy 12 on archival ovarian sex cord-stromal tumors. Gynecol Oncol. 1994;55:349–54. doi: 10.1006/gyno.1994.1305. [DOI] [PubMed] [Google Scholar]
- 2.Zhang J, Young RH, Arseneau I, Scully RE. Ovarian stromal tumors containing lutein or Leydig cells (luteinized thecomas and stromal Leydig cells)-a clinicopathological analysis of fifty cases. Int J Gynecol Pathol. 1982;1:270–85. doi: 10.1097/00004347-198203000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Gorlin RJ. Nevoid basal-cell carcinoma syndrome. Medicine(Baltimore) 1987;66:98–113. doi: 10.1097/00005792-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Tavassoli FA, Devilee P, editors. WHO Classification of Tumours: Pathology & Genetics of Tumours of the Breast and Female Genital Organs. IARC Press; Lyon, France: 2003. Tumours of the ovary and peritoneum; pp. 149–151. [Google Scholar]
- 5.Samuelson J, Katz S, Schwatz PE, Yang-Feng TI. Chromosomal evolution through tumor progression in ovarian cancer. Am J Hum Genet Suppl. 1988:A33. [Google Scholar]
- 6.Pejovic T, Heim S, Mandahl N, Elmfors B, Floderus UM, Furgyik S, Helm G, Willen H, Mitelman F. Trisomy 12 is a consistent chromosomal aberration in benign ovarian tumors. Genes Chromosome Cancer. 1990;2:48–52. doi: 10.1002/gcc.2870020109. [DOI] [PubMed] [Google Scholar]
- 7.Leung WY, Schwartz PE, Ng HT, Yang-Feng TL. Trisomy 12 in benign fibroma and granulose cell tumor of the ovary. Gynecol Oncol. 1990;38:28–31. doi: 10.1016/0090-8258(90)90006-7. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher JA, Gibas Z, Donovan K, Perez-Atayde A, Genest D, Morton CC, Lage JM. Ovarian granulose-stromal cell tumors are characterized by trisomy 12. Am J Pathol. 1991;138:515–20. [PMC free article] [PubMed] [Google Scholar]
- 9.Gancberg D, Scourneau M, Verdebout JM, Larsimont D, Verhest A. Detection of extra chromosomes 12 by fluorescent in situ hybridization (FISH) in ovarian stromal tumors. Study of 12 cases and review of the literature. Ann Pathol. 2001;21:393–8. [PubMed] [Google Scholar]
- 10.Mrozek K, Limon J, Debniak J, Mrozek Emerich J. Trisomy 12 and 4 in a thecoma of the ovary. Gynecol Oncol. 1992;45:66–8. doi: 10.1016/0090-8258(92)90493-3. [DOI] [PubMed] [Google Scholar]
- 11.Mrozek K, Nedoszytko B, Babinska M, Mrozek E, Hrabowska M, Emerich J, Limon J. Trisomy of chromosome 12 in a case of thecoma of the ovary. Gynecol Oncol. 1990;36:413–6. doi: 10.1016/0090-8258(90)90154-d. [DOI] [PubMed] [Google Scholar]
- 12.Walter TA, Rieck J, Hossfeld DK, Walter Loning T. An ovarian thecoma with a single numerical aberration: +12. Cancer Genet Cytogenet. 1993;71:180–2. doi: 10.1016/0165-4608(93)90029-l. [DOI] [PubMed] [Google Scholar]
- 13.Izutsu T, Kudo T, Miura F, Nishiya I. Numerical and structural chromosome abnormalities in an ovarian fibrothecoma. Cancer Genet Cytogenet. 1995;83:84–6. doi: 10.1016/s0165-4608(94)00307-6. [DOI] [PubMed] [Google Scholar]
- 14.Dal Cin P, Moerman P, De Wever I, Van den Berghe H. Numerical chromosome aberrations in fibrothecoma. Tumori. 1992;78:140–2. doi: 10.1177/030089169207800216. [DOI] [PubMed] [Google Scholar]
- 15.Dal Cin P, Qi H, Pauwels P, Backx C, Van den Berghe H. Monosomy 22 in a fibrothecoma. Cancer Genet Cytogenet. 1997;99:129–31. doi: 10.1016/s0165-4608(97)00210-0. [DOI] [PubMed] [Google Scholar]
- 16.Liang SB, Sonobe H, Taguchi T, Takeuchi T, Furihata M, Yuri K, Ohtsuki Y. Tetrasomy 12 in ovarian tumors of thecoma-fibroma group: A fluorescence in situ hybridization analysis using paraffin sections. Pathol Int. 2001;51:37–42. doi: 10.1046/j.1440-1827.2001.01168.x. [DOI] [PubMed] [Google Scholar]
- 17.Smith LM, Hu P, Meyer LJ, Coffin CM. Complex karyotpic abnormality in ovarian fibroma associated with Gorlin syndrome. Am J Med Genet. 2002;112:61–4. doi: 10.1002/ajmg.10607. [DOI] [PubMed] [Google Scholar]
- 18.Kiechle-Schwarz M, Pfleiderer A, Sreekantaiah C, Berger CS, Medchill MT, Sandberg AA. Cluster of trisomy 12 to tumors of the female genitourinary tract. Cancer Genet Cytogenet. 1991;54:273–5. doi: 10.1016/0165-4608(91)90223-h. [DOI] [PubMed] [Google Scholar]
- 19.Schofield DE, Fletcher JA. Trisomy 12 in pediatric granulose-stromal cell tumors. demonstration by a modified method of fluorescence in situ hybridization on paraffin-embedded material. Am J Pathol. 1992;141:1265–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Taruscio D, Carcangiu ML, Ward DC. Detection of trisomy12 on ovarian sex cord stromal tumors by fluorescence in situ hybridization. Diagn Mol Pathol. 1993;2:94–8. [PubMed] [Google Scholar]
- 21.Persons DL, Hartmann LC, Herath JF, Keeney GL, Jenkins RB. Fluorescence in situ hybridization analysis of trisomy 12 in ovarian tumors. Am J Clin Pathol. 1994;102:775–9. doi: 10.1093/ajcp/102.6.775. [DOI] [PubMed] [Google Scholar]
- 22.Halperin D, Visscher DW, Wallis T, Lawrence WD. Evaluation of chromosome 12 copy number in ovarian granulose cell tumors using interphase cytogenetics. Int J Gynecol Pathol. 1995;14:319–23. doi: 10.1097/00004347-199510000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Tsuji T, Kawauchi S, Utsunomiya T, Nagata Y, Tsuneyoshi M. Fibrosarcoma versus cellular fibroma of the ovary: A comparative study of their proliferative activity and chromosome aberrations using MIB-1 immunostaining, DNA flow cytometry, and fluorescence in situ hybridization. Am J Surg Pathol. 1997;21:52–9. doi: 10.1097/00000478-199701000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Althof PA, Ohmori K, Zhou M, Bailey JM, Bridge RS, Nelson M, Neff JR, Bridge JA. Cytogenetic and molecular cytogenetic findings in 43 aneurysmal bone cysts: aberrations of 17p mapped to 17p13.2 by fluorescence in situ hybridization. Mod Pathol. 2004;17:518–25. doi: 10.1038/modpathol.3800090. [DOI] [PubMed] [Google Scholar]
- 25.Shaffer L, Tommerup N, editors. ISCN. An international system for human cytogenetic nomenclature. Basel: S. Karger; 2005. [Google Scholar]
- 26.Tsuji T, Catasus L, Tsuji Prat J. Is loss of heterozygosity at 9q22.3 (PTCH gene) and 19p13.3 (STK11 gene) involved in the pathogenesis of ovarian stromal tumors? Hum Pathol. 2005;36:792–6. doi: 10.1016/j.humpath.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Gorlin RJ, Goltz RW. Multiple nevoid basal cell epithelioma, jaw cysts and bifid rib syndrome. N Engl J Med. 1960;262:908–12. doi: 10.1056/NEJM196005052621803. [DOI] [PubMed] [Google Scholar]
- 28.Shanley S, Ratcliffe J, Hockey A, Haan E, Oley C, Ravine D, Martin N, Wicking C, Chenevix-Trench G. Nevoid basal cell carcinoma syndrome: review of 118 affected individuals. Am J Med Genet. 1994;50:282–90. doi: 10.1002/ajmg.1320500312. [DOI] [PubMed] [Google Scholar]
- 29.Kimonis VE, Goldstein AM, Pastakia B, Yang ML, Kase R, DiGiovanna JJ, Bale AE, Bale SJ. Clinical manifestations in 105 persons with nevoid basal cell carcinoma syndrome. Am J Med Genet. 1997;69:299–308. [PubMed] [Google Scholar]
- 30.Farndon PA, Del Mastro RG, Evans DGR, Kilpatrick MW. Location of gene for Gorlin syndrome. Lancet. 1992;339:581–2. doi: 10.1016/0140-6736(92)90868-4. [DOI] [PubMed] [Google Scholar]
- 31.Chen Y, Struhl G. Dual roles for Patched in sequestering and transducing Hedgehog. Cell. 1996;87:553–63. doi: 10.1016/s0092-8674(00)81374-4. [DOI] [PubMed] [Google Scholar]
- 32.Byrom J, Mudaliar V, Redman CW, Jones P, Strange RC, Hoban PR. Loss of heterozygosity at chromosome 9q22-31 is a frequent and early event in ovarian tumors. Int J Oncol. 2004;24(5):1271. [PubMed] [Google Scholar]