Abstract
Objective
The objective of this study was to identify latent variables for neighborhood factors and diabetes self-care and examine the effect of neighborhood factors on diabetes self-care in adults with type 2 diabetes.
Research Design and Methods
615 subjects were recruited from an academic medical center and a Veterans affairs medical center in the southeastern United States. Validated scales were used to assess neighborhood factors and diabetes-related self-care. Confirmatory factor analysis (CFA) was used to determine the latent constructs. Structural equation modeling (SEM) was then used to assess the relationship between neighborhood factors and diabetes self-care.
Results
Based on a theoretical framework, CFA yielded four latent variables for neighborhood factors (neighborhood violence, access to healthy food, social support, and neighborhood aesthetics) and one latent variable diabetes self-care ( including diet, exercise, foot care, blood sugar testing and medication adherence). SEM showed that social support (r=0.28, p<0.001) and access to healthy foods (r=-0.16, p=0.003) were significantly associated with self-care behaviors, while neighborhood violence (r= -0.06, p<0.001) and aesthetics (r=-0.07, p=0.278) were not χ2 (180, N=611)=192, p=0.26, RMSEA=0.01, CFI=0.999). In the final trimmed model, social support (r=0.31, p<0.001) and access to healthy foods (r=-0.20, p<0.001) remained significantly associated with self-care behaviors χ2 (76, N=611)=60, p=0.91, RMSEA=0.00, CFI=1.0).
Conclusion
This study developed latent factors for neighborhood characteristics and diabetes self-care and found that social support and access to healthy foods were significantly associated with diabetes self-care and should be considered as targets for future interventions.
Keywords: diabetes, neighborhood/community, social determinants, self-care behaviors, diabetes outcomes
INTRODUCTION
Type 2 diabetes mellitus is a chronic illness that affects more than 25.3 million people in the United States (US) and 366 million people worldwide (1, 2). To attain optimal type 2 diabetes health outcomes, patients must participate in self-care behaviors, including eating a recommended diet, regular exercise, monitoring blood glucose, medication adherence, and foot care (3, 4). Emphasis has been placed on optimizing these behaviors in adults with type 2 diabetes in order to reduce the risk of type 2 diabetes related complications and to improve health outcomes (5). Additionally, self-care behaviors account for over 90% of the variance in glycemic control, in patients with type 2 diabetes (6). Yet, socio-environmental factors have been shown to contribute to up to 85% of patients’ nonadherence to self-care behaviors in adults with diabetes (5, 7-11). However, there is limited information on which socio-environmental elements have direct effects on self-care behaviors.
Previous studies have shown that socio-environmental factors, specifically neighborhood characteristics, can impact health outcomes of those with chronic illness, including type 2 diabetes (8, 12, 13). Neighborhood characteristics that have been identified as barriers to type 2 diabetes self-care behaviors include, but are not limited to, crime, violence, social cohesion, social support, and lack of resources (7, 8, 12, 14-16). Neighborhood characteristics have been shown to decrease medication adherence by 21.9%, reduce overall physical health, and contribute to poor dietary patterns (7, 19). Thus, identifying which neighborhood characteristics have the most significant impact on type 2 diabetes self-care behaviors can direct future initiatives.
An overview of the literature indicates various elements of the socio-environment are predictors of health outcomes (7, 8, 12-14). However, few studies have examined the structural pathways that link the social environment/neighborhood to self-care behaviors in patients with type 2 diabetes. Structural equation modeling (SEM) is an appropriate methodology to examine these relationships. In SEM, a theoretical framework and existing empirical evidence is tested using an available dataset (20). Predictive paths and covariance are tested to understand how well the hypothesized relationship is supported by goodness-of-fit statistics. SEM also allows testing of relationships among multiple dependent/outcome variables, which is important in understanding the role of neighborhood factors in diabetes.
The previously published theoretical framework by Brown and colleagues (13) examines the relationship between components of socioeconomic position and health outcomes in patients with type 2 diabetes. The framework indicates that an individual’s socioeconomic position, which includes education, income, employment, and community crime rates among other characteristics, can contribute to health outcomes as an adult. Furthermore, the framework hypothesizes that socioeconomic position has an impact on type 2 diabetess health outcomes. Subsequently, socioeconomic position influences proximal and distal moderators/mediators, that take into account health behaviors, access to care, and process of care, an individual’s stress level, provider decision-making style, community availability of health foods, and the health care system. As a result, socioeconomic position and distal and proximal moderators/mediators are thought to impact health outcomes (e.g., health status, quality of life, glycemic control).
Using the aforementioned theoretical framework, this study assessed the relationship between neighborhood characteristics and self-care behaviors using confirmatory factor analysis (CFA) to create latent variables for neighborhood factors and diabetes self-care. We then used SEM to test the structural relationships between neighborhood factors and self-care (21). Based on the aforementioned theoretical framework (13), we hypothesized that neighborhood factors would load under four latent variables (neighborhood violence, neighborhood aesthetics, access to healthy foods and social support), while diet, exercise, blood sugar testing, foot care and medication adherence would load on a type 2 diabetes self-care behavior latent factor. We further hypothesized that the neighborhood latent factors would be significantly associated with diabetes self-care behavior latent factors.
RESEARCH DESIGN AND METHODS
Sample Selection and Setting
Patients with type 2 diabetes (N=615) were recruited from an academic medical center and a Veterans affairs medical center in the southeastern United States. Approvals were obtained from the institutional review board and research and development committee for both institutions prior to study enrollment. Eligible patients had to be 18 years of age or older, a patient at either facility with a diagnosis of type 2 diabetes in their medical record, and able to communicate in English. Subjects were ineligible if they exhibited mental confusion during the screening interview or reported alcohol or drug abuse/dependency, active psychosis or acute mental disorder using validated screening instruments.
Data Collection
Program Coordinators reviewed the electronic clinic roster to identify eligible patients. Eligible patients were approached in the clinic waiting room and provided a description of the study. Those interested and eligible were then consented and given the questionnaire to complete. Patients were able to complete the assessment before or after their scheduled clinic appointments, depending on clinic flow. Six hundred and fifteen participants were consented and completed the study. Study personnel who had direct contact with patients were required to conduct mock study visits with fellow study personnel to insure that the consent process and administration of the study assessment were standardized. Outcome measures were abstracted from each patient’s electronic medical record.
Self-Care Behaviors
Self-Reported Medication Adherence
This was measured with the 8-item self-report Morisky Medication Adherence Scale (MMAS) (22). Each of the 8 items measures a specific medication-taking behavior. The new scale has higher reliability compared with the older 4-item scale (α = 0.83 vs. α = 0.61). The MMAS scores can range from 0 to 8 and was categorized as high adherence (score, 8), medium adherence (score, 6 to <8), and low adherence (score, <6).
Self-Care Behaviors
This was assessed with the Summary of Diabetes Self-Care Activities (SDSCA) scale (3). SCDCA is a brief, validated self-report questionnaire of diabetes self-management that includes items assessing diet, exercise, medication adherence, and self-blood glucose testing. The average inter-item correlations within scales are high; test-retest correlations are moderate; and correlations with other measures of diet and exercise generally support the validity of the SDSCA subscales.
Social Determinants of Health and Neighborhood Factors
Demographics
Previously validated items from the 2002 National Health Interview Survey (23) were used to capture age, gender, race/ethnicity, marital status, household income, and health insurance. Age was categorized as 18-34 years, 35-44 years, 45-64 years, and 65 years and older. Race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, and Hispanic/Other. Marital status was categorized as married or not married. Education was categorized as less than high school graduate, high school graduate, college, or graduate school. Employment was categorized as employed or not employed. Annual personal income was categorized as <$20,000, $20,000-$49,999, $50,000-74,999, and $75,000 and greater. Health insurance was categorized as insured or uninsured.
Social Support/Social Cohesion
A 3-item subscale from the Medical Outcomes Study (MOS) Social Support Survey (24) that measures positive social interaction was used to measure social support. The total scale (α=0.97) and subscales (α=0.91 to 0.96) have high internal consistency, good criterion and discriminant validity, and one-year test-retest reliability (0.72 to 0.76). Social cohesion was measured using the 5-item Sampson Scale (25). This scale measures the respondents’ ability to trust and relate to those in their neighborhood. The answers range from 1 (strongly agree) to 5 (strongly disagree).
Neighborhood Characteristics
Based on evidence from a prior validation study, six scales and four indices were used to assess neighborhood characteristics (26). For each of the scales and indices a higher score indicates more perceived problems in the neighborhood.
Neighborhood problems were measured using the neighborhood violence scale with response options ranging from 1 (often) to 4 (never) (26).
Neighborhood aesthetic quality was measured using a scale consisting of 7 items compiled from several studies that analyzed the impact of neighborhood aesthetics on health behaviors (27-31).
Access to healthy foods used 6-items to measure availability of fresh produce, low-fat products, and overall quality of foods available to the respondent (26), with answers ranging from 1 (strongly agree) to 5 (strongly disagree).
Statistical Analyses
Sample Size Calculation
To calculate the sample size for analysis, the N:q ratio was used, where N is the minimum sample size and q is the number of model parameters that require statistical estimates (32, 33). The recommended ratio for SEM is 20:1, which was used for this analysis (32, 33). Also, maximum likelihood for missing values (MLMV) was used as the model estimation method.
Overview of SEM
The purpose of SEM is to determine the extent to which a theoretical model is supported by sample data (21). In general, SEM tests theoretical models using hypothesis testing to understand the complex relationship where latent and indicator variables are measured with error (21). A latent variable is a construct that can be described as an explanatory variable presumed to reflect a continuum that is not directly observable (34). However, latent variables can be indirectly observed or measured using multiple indicator (or dependent) variables (21). Ultimately, SEM is advantageous because it accounts for measurement error in indicator variables while developing a parsimonious model (21).
Data Analyses
We used confirmatory factor analysis (CFA) as part of structural equation modeling (SEM) to identify latent variables that describe different neighborhood factors (e.g., neighborhood problems, neighborhood aesthetics, access to healthy foods, social support). Prior analysis suggests that type 2 diabetes self-care behaviors, measured by the SDSCA, load onto a single latent construct (see Figure 1) (35). Thus, we used the same latent variable for this analysis. For this study, we conducted five sets of analyses to determine the structural relationships of the data using path coefficients. All analyses were performed using STATA V13 and a two-tailed alpha of 0.05 was used to determine statistical significance.
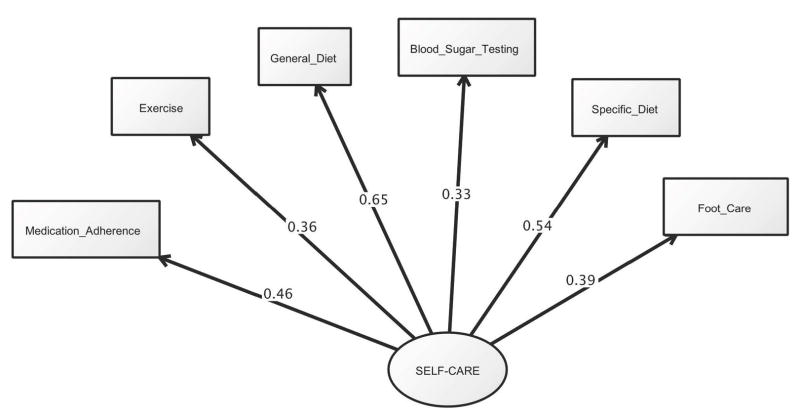
Figure 1.
Confirmatory Factor Analysis of Diabetes Self-Care Behaviors (Measurement Model).
Note: Overall model fit, χ2 (8)=9.94, p=0.27; RSMEA=0.02 and CFI=0.994. For this measurement model, each factor loading had a significance level of p<0.001.
Step 1: Calculating Cronbach’s Alpha
Cronbach’s alpha was calculated for scales used as indicator variables to assess internal consistency of the items (36). We only used a scale if the items loaded with a Cronbach’s alpha equal to or greater than 0.8.
Step 2: Factor Analysis
Factor analysis was used to determine which sets of observed variables share common variance-covariance characteristics that define a theoretical construct, also known as a latent variable (21). Factor analysis was performed for each indicator scale. Scales were kept if they loaded onto one factor, sufficiently explained the variance on the factor, and had a factor loading equal to or greater than 0.6. In line with the theoretical framework for the study (13), we examined factor loadings for the four neighborhood latent variables and the self-care latent variable.
Step 3: CFA to Test Fit for Hypothesized Structural Model
Confirmatory factor analysis (CFA) was used to statistically test the significance of the hypothesized measurement models—neighborhood violence, access to healthy food, neighborhood aesthetics, and social support. For each latent variable we examined factor loadings, goodness-of-fit statistics and used modification indices to build CFA models that were consistent with our conceptual model and had good model fit statistics. Our sample size of 615 cases was sufficient for this analysis.
Step 4: Model Fitting and Structural Models
We ran structural models to test the association between neighborhood latent variables and self-care latent variables. Maximum likelihood for missing variables (MLMV) was used to retrieve as much information possible from observations with missing values. Again, consistent with the theoretical framework, we hypothesized that neighborhood problems, access to healthy food, neighborhood aesthetics, and social support would be significantly associated with type 2 diabetes self-care behaviors. The latent neighborhood variables that had non-significant associations with self-care were removed from the model, resulting in a “trimmed” model.
Step 5: Fit Statistics
Based on guidelines for model fit, we used multiple indicators including likelihood ratio chi-square tests, the comparative fit index (CFI) and the root mean square error of approximation (RSMEA). A non-significant chi-square test suggests the data fits the hypothesized structural model (21). A CFI value can range from 0 to 1, where 1 indicates perfect data fit (21). An RSMEA value can range from 0 to infinity, with a value less than 0.05 indicating a close fit, values equal to or less than 0.08 indicate reasonable fit, and values equal to or greater than 0.1 indicate poor fit (21).
RESULTS
Sample Characteristics
Demographic and sample characteristics for this sample of 615 adults with type 2 diabetes are shown in Table 1. The majority of these patients were men (61.6%), non-Hispanic Black (65.7%), between the ages of 45-64 (53.6%), not employed (65.3%), college educated (47.1%), and had an income less than $20,000 annually (41.6%). In the last 7 days participants reported, on average, adhering to a general diet 4.7 days, specific diet 4 days, exercise 2.6 days, self-monitoring blood glucose 4.6 days and foot care 4.3 days and a Morisky medication adherence score of 4.9.
Table 1.
Sample demographic characteristics
| % | |
|---|---|
|
| |
| Age | |
| 18-34 years | 1.6 |
| 35-44 years | 5.2 |
| 45-64 years | 53.6 |
| 65+ years | 39.6 |
| Gender | |
| Women | 38.4 |
| Men | 61.6 |
| Race/Ethnicity | |
| Non-Hispanic Black | 65.7 |
| Non-Hispanic Whites | 33.0 |
| Hispanic/Other | 1.3 |
| Marital Status | |
| Married | 49.7 |
| Not Married | 50.3 |
| Educational level | |
| Less than high school graduate | 13.0 |
| High school graduate | 28.2 |
| College education | 47.1 |
| More than college | 11.7 |
| Employment status | |
| Employed | 34.7 |
| Not employed | 65.3 |
| Annual income level | |
| <$20,000 | 41.6 |
| $20,000-$49,000 | 38.9 |
| $50,000-$74,999 | 10.1 |
| $75,000+ | 9.4 |
| Self-Care Behaviors (over 7 days) | |
| General Diet | 4.7 (±2.0) |
| Specific Diet | 4.0 (±1.6) |
| Exercise | 2.6 (±2.2) |
| Self-Monitoring Glucose Testing | 4.6 (±2.5) |
| Foot Care | 4.3 (±2.5) |
| Morisky Medication Adherence Scale (score 0-8) | 4.9 (±2.0) |
Diabetes Self-Care Behaviors
The measurement model for self-care behaviors showed good fit (see Figure 1) (χ2 (8)=9.94, p=0.27; RSMEA=0.02 and CFI=0.994. Diabetes self-care (SDSCA) loaded significantly onto the measured variables: general diet (r=0.65, p<0.001), specific diet (r=0.54, p<0.001), exercise (r=0.36, p<0.001), self-monitoring blood glucose testing (r=0.33, p<0.001), foot care (r=0.39, p<0.001), and medication adherence (r=0.46, p<0.001). The alpha statistic for the six items was 0.61. These variables loaded onto factors accounting for 35% of the variance with factor loadings ranging from 0.47 to 0.70.
Neighborhood Problems
The measurement model for neighborhood problems showed good fit (χ2 (1)= 0.78, p<0.38; RSMEA=0.00 and CFI=1.00. The four items related to violence loaded significantly onto and had a significant association with the measured variable: “in the past six months, how often was there a fight in your neighborhood” (r=0.79, p<0.001), “in the past six month, have there been any gang fights” (r=0.77, p<0.001), “in the past six months, has there been sexual assault or rape” (r=0.75, p<0.001), and “in the past six months, has there been a robbing or mugging” (r=0.70, p<0.001). The alpha statistic for these four items was 0.81. These variables account for 66% of the variance with factor loadings ranging from 0.79 to 0.84.
Neighborhood Aesthetics
The measurement model for neighborhood aesthetics showed good fit (χ2 (0)=0.0, no p value; RSMEA=0.00 and CFI=1.00), showing that the model has no additional degrees of freedom. Because the model has no additional degrees of freedom, the model has a perfect fit. Three items loaded significantly onto and had a significant association with the measured variable: “my neighborhood is attractive” (r=0.63, p<0.001), “there are interesting things to do in my neighborhood” (r=0.76, p<0.001), and “there is enjoyable scenery in my neighborhood” (r=0.84, p<0.001). The three measures of neighborhood aesthetics had an alpha statistic of 0.79. These measures accounted for 70% of the variance with factor loadings ranging from 0.79 to 0.87.
Access to Healthy Foods
The measurement model for access to healthy food showed good fit (χ2 (1)=0.20, p<0.65; RSMEA=0.00 and CFI=1.00. Each item on the six-item access to healthy food scale loaded significantly onto and had a significant association with the measured variable: “it is easy to purchase fresh fruits and vegetables in my neighborhood” (r=0.79, p<0.001), “there is a large selection of fresh fruits and vegetables available in my neighborhood” (r=0.85, p<0.001), “the fresh produce in my neighborhood is of high quality” (r=0.87, p<0.001), “is it easy to purchase low fat products in my neighborhood” (r=0.95, p<0.001), “there is a large selection of low fat products available in my neighborhood” (r=0.96, p<0.001), and “the low fat products in my neighborhood are of high quality” (r=0.97, p<0.001). The access to healthy food scale had an alpha statistic of 0.97. These items accounted for 87% of variance with factor loadings ranging from 0.90 to 0.94.
Social Support
The measurement model for social support showed good fit, χ2 (0, N=610)=0.0, RSMEA=0.00, CFI=1.00 (90% CI: 0.00-0.00). There were three items that loaded significantly onto and had a significant association with the measured variable: “someone to have a good time with” (r=0.94, p<0.001), “someone to get together with for relaxation” (r=0.96, p<0.001), and “someone to do something enjoyable with” (r=0.97, p<0.001). The subscale of social support had an alpha statistics of 0.93. These measures explain 95% of variance with factor loadings ranging from 0.97 to 0.98.
Structural Models
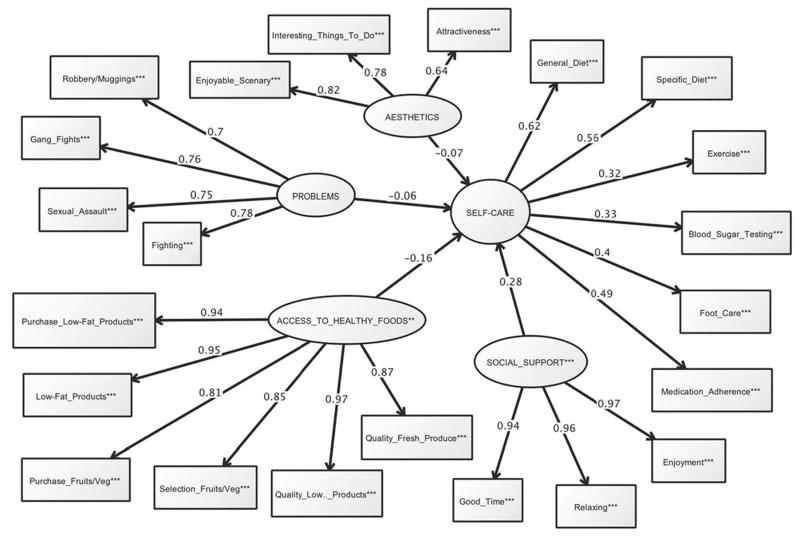
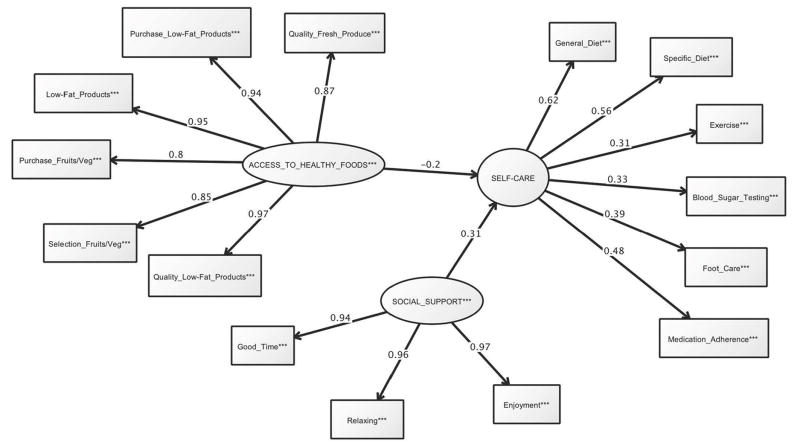
The final model (Figure 2) examined the relationship between neighborhood latent variables and type 2 diabetes self-care behaviors. The model demonstrated a good fit (χ2 (180)=192, p=0.26; CFI=0.99 and RMSEA=0.01. Type 2 diabetes self-care behavior was significantly associated with social support (r=0.28, p<0.001) and access to healthy food (r=-0.16, p=0.003). Neighborhood characteristics and violence did not have statistically significant association with type 2 diabetes self-care behaviors. Items that we found to not have a significant association were omitted to create a trimmed model. These modifications allowed us to generate a more parsimonious model. Figure 3 shows the trimmed model. The trimmed model demonstrates a good fit, χ2 (180, N=611)= 192, p=0.26, CFI=0.99, RMSEA=0.01 (90% CI:0.00-0.02). In the trimmed model, diabetes self-care behavior was significantly associated with social support (r=0.31 p<0.001) and access to healthy food (r=-0.20, p<0.001).
Figure 2.
Estimated Structural Model of Type 2 Diabetes Self-Care and Neighborhood Factors (Full)
Note: Coefficients are standardized path coefficients. Overall model fit, χ2 (180)=192, p=0.26; RSMEA=0.01 and CFI=0.999. For tests of significance of individual paths *p<0.05, **p<0.01, ***p<0.001.
Figure 3.
Estimated Structural Model of T2DM Self-Care and Neighborhood Factors (Trimmed)
Note: Coefficients are standardized path coefficients. Overall model fit, χ2 (76)=59.8, p=0.91 RSMEA=0.00 and CFI=1.00. For tests of significance of individual paths *p<0.05, **p<0.01, ***p<0.001.
CONCLUSION
Using an established theoretical framework (13), we were able to create four latent variables that represent neighborhood characteristics and a latent variable to represent diabetes self-care. Using several indicator scales to measure elements of the neighborhood, we found that a few items were the best indicators for the neighborhood latent variables—neighborhood aesthetics, neighborhood violence, social support and access to healthy foods. Structural equation modeling showed that access to healthy foods and social support latent variables had significant associations with type 2 diabetes self-care behaviors, while neighborhood violence and neighborhood aesthetics latent variables did not have a statistically significant association with type 2 diabetes self-care behaviors.
These results are in line with findings from prior studies (8, 12, 19, 25, 37-40). In addition, these findings support the theoretical framework outlined by Brown and colleagues (13), in that, we found significant associations between neighborhood characteristics, as a function of an individual’s socioeconomic position, and diabetes self-care behaviors. Subsequently, it could be hypothesized that, because diabetes self-care behaviors have been significantly association with health outcomes in the literature, neighborhood characteristics may indirectly influence diabetes health outcomes. However, contrary to the literature (7, 8), neighborhood problems (e.g. safety, crime, perceived problems) and neighborhood aesthetics (e.g., walking environment, recreational facilities, neighborhood activities) did not have significant associations with self-care behaviors in this patient population.
While previous studies have focused on individual aspects of the neighborhood and socio-environment to explain barriers to health outcomes and health behaviors, the findings from the current study hone in on which socio-environmental factors influence health behaviors. Furthermore, this study gives insight into which aspects of the socio-environment could be modified to increase adherence to self-care behaviors in patients with type 2 diabetes.
Moreover, public health initiatives should emphasize and encourage community gardens, farmer’s markets, and opening affordable grocery stores that provide fresh produce and low-fat products in low-income neighborhoods. Together with public health workers, clinicians can be instrumental in facilitating opportunities for social support. Support groups that are held in communities for health specific conditions, peer-to-peer mentoring, community health workers, or community health champions can be a means for social support. However, the type of social support needed by individuals’ may vary. Therefore, clinicians must be able to understand what level of support their respective patient may require.
In conclusion, we found that neighborhood violence and neighborhood aesthetics latent variables did not have a statistically significant association with type 2 diabetes self-care behaviors whereas access to healthy foods and social support latent variables had significant associations with type 2 diabetes self-care behaviors. This suggests that access to healthy food and social support may be important targets for future interventions in individuals with type 2 diabetes when trying to improve patients’ self-care behaviors. In addition, it provides new findings on the effect of neighborhood factors on adherence to type 2 diabetes self-care behaviors and provides further insight on the specific socio-environmental characteristics associated with poor health outcomes in diabetes.
Acknowledgments
Funding Source: This study was supported by Grant K24DK093699-01 from The National Institute of Diabetes and Digestive and Kidney Disease (PI: Leonard Egede).
Footnotes
Author Contributions: LEE obtained funding for the study. BLS and LEE designed the study, acquired, analyzed and interpreted the data. BLS, CMG, JSZ and LEE developed the analysis, contributed to interpretation and critically revised the manuscript for important intellectual content. All authors approved the final manuscript.
Conflict of Interest: The authors report no potential conflicts of interest relevant to this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Institute for Diabetes, Digestion, and Kidney Disease (NIDDK) National Diabetes Statistics, 2011. NIH Publication 11-3892; Feb, 2011. http://diabetes.niddk.nih.gov/DM/PUBS/statistics. [Google Scholar]
- 2.International Diabetes Federation. IDF Diabetes Atlas. 5. Brussels, Belgium: International Diabetes Federation; 2011. http://www.idf.org/diabetesatlas. [Google Scholar]
- 3.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000 Jul;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 4.Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. Journal of Diabetes and Metabolic Disorders. 2013;12:14–19. doi: 10.1186/2251-6581-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asante E. Interventions to promote treatment adherence in type 2 diabetes mellitus. British Journal of Community Nursing. 2013;18(6):267–274. doi: 10.12968/bjcn.2013.18.6.267. [DOI] [PubMed] [Google Scholar]
- 6.Tuerk PW, Mueller M, Egede LE. Estimating physician effects on glycemic control in the treatment of diabetes: methods, effect sizes, and implications for treatment policy. Diabetes Care. 2008;31(5):869–873. doi: 10.2337/dc07-1662. [DOI] [PubMed] [Google Scholar]
- 7.Billimek J, Sorkin DH. Self-reported neighborhood safety and nonadherence to treatment regimens among patients with type 2 diabetes. J Gen Intern Med. 2011;27(3):292–296. doi: 10.1007/s11606-011-1882-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gary TL, Safford MM, Gerzoff RB, Ettner SL, Karter AJ, Beckles GL, Brown AF. Perception of neighborhood problems, health behaviors, and diabetes outcomes among adults with diabetes in managed care: the translating research into action for diabetes (TRIAD) study. Diabetes Care. 2008;31(2):273–278. doi: 10.2337/dc07-1111. [DOI] [PubMed] [Google Scholar]
- 9.Paes AH, Bakker A, Soe-Agnie CJ. Impact of dosage frequency on patient comphance. Diabetes Care. 1997;20(10):1512–7. doi: 10.2337/diacare.20.10.1512. [DOI] [PubMed] [Google Scholar]
- 10.Cramer JA. A systematic review of adherence with medication for diabetes. Diabetes Care. 2004;32:1218–24. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- 11.Yusuf FKB, Obe O, Joseph BY. Adherence to anti-diabetic drug therapy and self-management practices among type-2 diabetics in Nigeria. Pharni World Sd. 2008;30(6):876–83. doi: 10.1007/s11096-008-9243-2. [DOI] [PubMed] [Google Scholar]
- 12.Brown AF, Ang A, Pebley AR. The relationship between neighborhood characteristics and self-rated health for adults with chronic conditions. Am J of Public Health. 2007;97(5):926–932. doi: 10.2105/AJPH.2005.069443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, Karter AJ, Safford M, Waitzfelder B, Prata PA, Beckles GL. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiologic Reviews. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 14.Kollannoor-Samuel G, Vega-López S, Chhabra J, Segura-Pérez S, Damio G, Pérez-Escamilla R. Food insecurity and low self-efficacy are associated with health care access barriers among Puerto-Ricans with type 2 diabetes. J Immigrant Minority Health. 2012;14:552–562. doi: 10.1007/s10903-011-9551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heisler M. Different models to mobilize peer support to improve diabetes self-management and clinical outcomes: evidence, logistics, evaluation considerations and needs for future research. Family Practice. 2010;27:i23–i32. doi: 10.1093/fampra/cmp003. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 16.Zgibor JC, Simmons D. Barriers to blood glucose monitoring in a multiethnic community. Diabetes Care. 2002;25:1772–1777. doi: 10.2337/diacare.25.10.1772. [DOI] [PubMed] [Google Scholar]
- 17.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Research and Clinical Practice. 2011;93:1–9. doi: 10.1016/j.diabres.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Weaver RR, Lemonde M, Payman N, Goodman WM. Health capabilities and diabetes self-management: the impact of economic, social and cultural resources. Social Science & Medicine. 2014;102:58–68. doi: 10.1016/j.socscimed.2013.11.033. [DOI] [PubMed] [Google Scholar]
- 19.Millstein RA, Yeh HC, Brancati FL, Batts-Turner M, Gary TL. Food availability, neighborhood socioeconomic status, and dietary patterns among blacks with type 2 diabetes mellitus. Medscape J Med. 2009;11(1):15. [PMC free article] [PubMed] [Google Scholar]
- 20.Schönberger M, Ponsford J, Olver J, Ponsford M, Wirtz M. Prediction of functional and employment outcome 1 year after traumatic brain injury: a structural equation modeling approach. J Neurol Neurosurg Psychiatry. 2011;82:936–941. doi: 10.1136/jnnp.2010.210021. [DOI] [PubMed] [Google Scholar]
- 21.Schumacker RE, Lomax RG. A beginner’s guide to structural equation modeling. 3. Taylor and Francis Group; New York: 2010. [Google Scholar]
- 22.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. Survey Questionnaire, National Health Interview Survey, 2002. National Center for Health Statistics; Hyattsville, Maryland: 2004. [February 2, 2014]. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2002/ [Google Scholar]
- 24.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Social Science and Medicine. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 25.Sampson RJ, Raudenbush RW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 26.Echeverria SE, Dietz-Roux AV, Link BG. Reliability of self-reported neighborhood characteristics. J Urban Health. 2004;81(4):682–701. doi: 10.1093/jurban/jth151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sallis JF, Johnson MF, Calfas KJ, Caparosa S, Nichols JF. Assessing perceived physical environmental variables that may influence physical activity. Res Q Exerc Sport. 1997;68:345–351. doi: 10.1080/02701367.1997.10608015. [DOI] [PubMed] [Google Scholar]
- 28.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Empidemiol. 2002;155:507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 29.Giles-Corti B, Donovan RJ. Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Prev Med. 2002;35:601–611. doi: 10.1006/pmed.2002.1115. [DOI] [PubMed] [Google Scholar]
- 30.Ball K, Bauman A, Leslie E, Own N. Perceived environmental aesthetics and convenience and company are associated with walking for exercise among Australian adults. Prev Med. 2001;33:434–440. doi: 10.1006/pmed.2001.0912. [DOI] [PubMed] [Google Scholar]
- 31.King AC, Castro C, Wilcox S, Eyler AA, Sallis JF, Brownson RC. Personal and environmental factors associated with physical inactivity among different racial-ethnic groups of US middle-aged and older-aged women. Health Psychol. 2000;19:354–364. doi: 10.1037//0278-6133.19.4.354. [DOI] [PubMed] [Google Scholar]
- 32.Kline RB. Principles and practices of structural equation modeling. 3. Guilford Press; New York, NY: 2011. [Google Scholar]
- 33.Tanaka JS. “How big is big enough?”: sample size and goodness of fit in structural equation models with latent variables. Child Development. 1987;58:134–146. [Google Scholar]
- 34.Kline RB. Principles and Practice of Structural Equation Modeling. 3. Guilford Press; NY: 2011. [Google Scholar]
- 35.Egede LE, Osborn CY. Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. Diabetes Educ. 2010;36(2):276–283. doi: 10.1177/0145721710361389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing clinical research. 3. Philadelphia: Lippincott Williams Wilkins; 2007. [Google Scholar]
- 37.Boardman JD. Stress and physical health: the role of neighborhoods as mediating and moderating mechanisms. Social Science and Medicine. 2004;58:2473–2483. doi: 10.1016/j.socscimed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 38.Browning CP, Cagney KA. Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. Journal of Health and Social Behavior. 2002;43(4):383–399. [PubMed] [Google Scholar]
- 39.Diez Roux AV, Mair C. Neighborhoods and health. Ann NY Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 40.Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among US adults with diabetes. Diabetes Care. 2013;36:3093–3099. doi: 10.2337/dc13-0570. [DOI] [PMC free article] [PubMed] [Google Scholar]