Abstract
Background
The International Union Against Cancer/American Joint Committee on Cancer (UICC/AJCC) TNM staging system of nasopharyngeal carcinoma (NPC) is the most important system for survival prediction. The TNM 7th edition UICC/AJCC TNM staging system for NPC was adopted in January 2009, and is now internationally recommended. In comparison with the TNM 6th edition, there were several revisions in the new edition staging system. This study aims to evaluate the prognostic value of the TNM 7th edition for NPC patients in comparison with the TNM 6th edition.
Method
Clinical data of 2,629 NPC patients from the Sun Yat-sen University Cancer Center between January 2006 and December 2010 were retrospectively collected and all the patients were restaged according to the criteria of the TNM 6th edition and TNM 7th edition UICC/AJCC staging manual. Univariate and multivariate COX proportional hazards analyses were applied to evaluate the prognostic values between adjacent stage categories of the TNM 6th edition and TNM 7th edition.
Results
In comparison with the TNM 6th edition, a significant alteration of the distribution of N categories was observed when the TNM 7th edition was applied (χ2 = 20.589, P<0.001), with 119 (119/670, 17.8%) patients up-staging from N0 to N1. With regard to T and overall stage, 37 (37/561, 6.6%) patients were down-staged from T2a with the TNM 6th edition to T1 with the TNM 7th edition, and finally two patients were up-staged to overall stage II (2/118, 1.7%). Moreover, the survival curves were significantly segregated (P<0.05) between T1 and T2 as well as N1 and N2 with the TNM 7th edition.
Conclusions
The TNM 7th edition led to a significant alteration in the distribution of N categories and it is superior to the TNM 6th edition in predicting the frequency of overall survival and distant metastasis-free survival.
Introduction
Nasopharyngeal carcinoma (NPC) is a non-lymphomatous and squamous-cell carcinoma, which is commonly associated with Epstein-Barr virus infection [1]. The annual incidence of NPC reaches about 25 per 100,000 individuals among the Cantonese people that inhabit Guangdong province in Southern China, which is 25-fold higher than that in the Western world [1], [2]. During the past decades, the overall 5-year survival rate has improved substantially from 60% to 80%. However, 20–30% patients finally progress with distant metastasis and/or loco-regional recurrence [3], [4]. Therefore, better treatment approaches and rational planning are urgently required for NPC patients.
As outlined by the UICC/AJCC, the TNM staging system is the most important prognosticator for survival prediction and contributes largely to the treatment planning of NPC patients [5], [6]. To date, there have been four editions of TNM staging systems for NPC that have been updated in association with the development of imaging and treatment technologies. The TNM 6th edition has been commonly used since its release in 2002 [7]; however, there are still some controversies: firstly, accumulative studies revealed that nasal and/or oropharyngeal invasion (T2a by TNM 6th edition) without parapharyngeal extension had a similar prognosis compared to T1; secondly, retropharyngeal lymph node (RLN) involvement, regardless of laterality, had an inferior prognosis compared to node-negative disease[8], [9], [10]; thirdly, masticator space invasiveness including the medial and lateral pterygoid muscles had a similar prognosis to T4 [11], [12]. In 2009, the TNM 7th edition UICC/AJCC staging system for NPC was released [13] and revised the corresponding criteria based on the previous findings except for the definition of the masticator space. In fact, there was no instruction about the definition of masticator space in the TNM 6th edition and TNM 7th edition AJCC cancer staging handbook [14], [15]. Therefore, there was no obvious change regarding T4. Here, in order to evaluate the prognostic value of the TNM 7th edition, we compared the prognostic performance of the TNM 7th edition with the TNM 6th edition, in a large retrospective cohort of 2,629 NPC patients.
Materials and Method
Patient characteristics
We retrospectively reviewed the medical records of 2,671 consecutive patients with biopsy-proven hospitalization at Sun Yat-sen University Cancer Center (SYSUCC) between January 2006 and December 2010. One patient without radiation therapy and 41 patients without a complete medical history of clinical and follow-up data were excluded from the study. Finally, 2,629 patients remained for further analyses (Table 1 and S1 Table). This study was approved by the Institutional Review Board of the Sun Yat-sen University Cancer Center. All patients signed an informed consent form prior to participating in the study. All 2,629 patients had undergone fiberoptic endoscopic biopsy of the nasopharynx and contrast-enhanced CT/MRI of the nasopharynx and neck during staging work-up. Almost all individuals (2,625/2,629, 99.8%) received magnetic resonance imaging (MRI) of the head and neck to evaluate the primary tumor and the frequency of LN metastases, and the other four patients received CT. All included patients underwent other pretreatment evaluations, including physical and neurologic examinations, hematology and biochemistry profiling, chest radiography, abdominal ultrasonography and emission CT scan. In addition, a total of 287 (10.9% of 2,629) patients underwent 18F-fluorodeoxyglucose positron emission tomography and computed tomography (PET/CT) examination to help evaluate distant metastatic disease. Cranial nervepalsy was assessed clinically. Two clinicians independently reviewed all of the images based on the MRI/CT diagnosis criteria and re-staged all the patients according to the criteria of the TNM 6th edition and TNM 7th edition for NPC (Table 2). Any disagreements were resolved by consensus.
Table 1. Distribution and characteristics of 2,629 patients with nasopharyngeal carcinoma.
| Characteristic | TNM 6th edition | TNM 7th edition | ||||
| N | % | N | % | ?2 | P | |
| Gender | ||||||
| Female | 673 | 25.6 | 673 | 25.6 | ||
| Male | 1,956 | 74.4 | 1,956 | 74.4 | ||
| Age (year) | ||||||
| Median | 50 | 50 | ||||
| Range | 6–98 | 6–98 | ||||
| Histology | ||||||
| WHO I+II | 142 | 5.4 | 142 | 5.4 | ||
| WHO III | 2,487 | 94.6 | 2,487 | 94.6 | ||
| Treatment | ||||||
| RT | 673 | 25.6 | 673 | 25.6 | ||
| CRT | 1,956 | 74.4 | 1,956 | 74.4 | ||
| Radiotherapy techniques | ||||||
| 2D-CRT | 1,863 | 70.9 | 1,863 | 70.9 | ||
| 3D-CRT | 85 | 3.2 | 85 | 3.2 | ||
| IMRT | 681 | 25.9 | 681 | 25.9 | ||
| T-classification | 3.467 | 0.325 | ||||
| T1 | 292 | 11.1 | 329 | 12.5 | ||
| T2 | 561 | 21.3 | 524 | 19.9 | ||
| T3 | 1,247 | 47.5 | 1,247 | 47.5 | ||
| T4 | 529 | 20.1 | 529 | 20.1 | ||
| N-classification | 20.589 | <0.001 | ||||
| N0 | 670 | 25.5 | 551 | 21 | ||
| N1 | 728 | 27.7 | 847 | 32.2 | ||
| N2 | 1,042 | 39.6 | 1,042 | 39.6 | ||
| N3 | 189 | 7.2 | 189 | 7.2 | ||
| M-classification | ||||||
| M0 | 2,553 | 97.1 | 2,553 | 97.1 | ||
| M1 | 76 | 2.9 | 76 | 2.9 | ||
| Overall Stage | 0.22 | 0.999 | ||||
| I | 118 | 4.5 | 120 | 4.6 | ||
| II | 389 | 14.8 | 387 | 14.7 | ||
| III | 1,400 | 53.3 | 1,400 | 53.2 | ||
| IV | 722 | 27.5 | 722 | 27.5 | ||
Abbreviations: AJCC = American Joint Committee on Cancer; WHO = World Health Organization; RT = Radiotherapy; CRT = Chemoradiotherapy; 2D-CRT = conventional 2-dimensional radiotherapy; 3D-CRT = 3-dimensional conformal radiotherapy; IMRT = Intensity-modulated radiation therapy
Table 2. Classification criteria of TNM 6th and TNM 7th staging system for nasopharyngeal carcinoma.
| TM6th | TNM7th | |
| T classification | ||
| T1 | nasopharynx | nasopharynx, oropharynx or nasal cavity |
| T2 | ||
| T2a | oropharynx and/or nasal cavity | pharapharyneal extension |
| T2b | parapharyneal extension | |
| T3 | bony structures and/or paranasal sinuses | bony structures and/or paranasal sinuses |
| T4 | intracranial extension and/or cranial nerves, infratemporal fossa hypophaynx, orbit or masticatory spacea | intracranial extension and/or cranial nerves, hypopharynx, orbit or infratemporal fossa/masticatory spaceb |
| N classification | ||
| N0 | none | none |
| N1 | unilateral node(s), ≤6cm in greatest dimension, above the supraclavicular fossa | unilateral cervical and/or unilateral or bilateral retropharyngeal node(s),≤6cm in greatest dimension, above the supraclavicular fossa |
| N2 | bilateral node(s),≤6cm in greatest dimension, above the supraclavicular fossa | bilateral cervical node(s),≤6cm in greatest dimension, above the supraclavicular fossa |
| N3a | >6cm, or in supraclavical fossa | >6cm, or in supraclavical fossa |
| stage group | ||
| I | T1N0M0 | T1N0M0 |
| II | T1N1M0, T2N0-1M0 | |
| IIA | T2aN0M0 | |
| IIB | T1-2aN1M0, T2bN0-1M0 | |
| III | T1-2bN2M0, T3N0-2M0 | T1-2N2M0, T3N0-2M0 |
| IVA | T4N0-2M0 | T4N0-2M0 |
| IVB | any T N3M0 | any T N3M0 |
| IVC | any T any N 3M1 | any T any N 3M1 |
Abbreviations: UICC = the International Union Against Cancer; AJCC = American Joint Committee on Cancer
Masticator space involvement denotes extension of tumor beyond the anterior surface of the lateral pterygoid muscle or lateral extension beyond the posterolateral wall of the maxillary antrum and the pterygomaxillary fissrue.
Masticator space primarily consists of the muscles of mastication. Anatomically, the superficial layer of the deep cervical fascia splits to enclose the muscles of mastication to enclose this space. These muscles are the medial and lateral pterygoid, masseter and temporalis.
With regard to non-distant metastatic cancer, it was defined as a primary tumor with or without local regional lymphocyte node metastases, including stage I, II, III, IVa and IVb subgroups. With respect to distant metastasis, it was defined as a tumor spreading from the original (primary) tumor to distant organs or distant lymph nodes. Among a total of 2,629 individuals recruited, 542 patients had a primary tumor without regional lymphatic metastases, 2,011 patients had local regional lymphatic metastases, and the remaining 76 patients had distant metastases.
Determination of nasal and/or oropharyngeal cavity invasion for the T category
Diagnostic MRI/CT criteria for nasal invasion included nasal structure (turbinates and nasal septum) involvement, and extension to the line of bilateral pterygopalatine fossa. Oropharyngeal invasion was determined as the tumor margin accessing the gap of the first and second cervical intervertebra [16]. Patients with nasal cavity and/or oropharynx involvement were classified as T2a by the TNM 6th edition but T1 by the TNM 7th edition [17].
Determination of lymph node metastasis for N classification
Metastatic lymphadenopathy was determined by using MRI/CT with any of the following: 1) lateral RLNs with a minimal axial dimension (MID) of 6 mm [18] and any lymph node observed in the median retropharyngeal group, or cervical lymph nodes with a MID of 11 mm in the digastric region, and MID of 10 mm for all other cervical lymph nodes except the retropharyngeal group; 2) lymph nodes of any size with central necrosis or a contrast-enhancing rim; and 3) lymph node cluster, meaning the presence of 3 contiguous and confluent lymph nodes, each of which should have a MID of 8–10 mm [16], [19]. Patients with RLN metastasis but no positive cervical lymph nodes (N0RLN+) were staged as a N0 subset in the 6th edition but an N1 subset in the 7th edition. Patients with neither RLN nor cervical lymph node metastasis (N0RLN-) remained in the N0 subset in both editions [17].
Treatment and follow-up
Radiotherapy with or without chemotherapy remained as standard care for NPC patients [20]. For non-distant metastatic NPC, all patients were treated with standard curative radical radiotherapy, including conventional 2-dimensional radiotherapy (2D-CRT) or intensity-modulated radiation therapy (IMRT), as described previously [20]. Briefly, all target volumes were outlined slice by slice in the treatment planning system based on enhanced CT scans. The radiation dose was 60∼72 Gy at the nasopharyngeal region and 50∼66 Gy at the regional lymph nodes. Part of the patients with stage II and all patients with stage III to stage IV disease were commonly combined with sequential chemotherapy with a platinum-based regimen. Salvage treatments (including surgery, brachytherapy, and chemotherapy) were provided in the event of documented disease recurrence or persistence.
For distant metastatic NPC, loco-regional radiotherapy with cisplatin-based systemic chemotherapy was provided to the patients [21]. Local treatment of metastatic sites, including radiation therapy, surgical resection or ablation, or other treatments were provided to the metastatic patients based on the discretion of the attending radiation oncologists.
The patients were followed up every three months in the first three years, and every six months thereafter or until death. The last follow-up date was May 30, 2013 for all available patients. Local recurrence was confirmed by fiberoptic endoscopy, MRI and biopsy. Distant metastases were diagnosed based on clinical symptoms, physical examination, and imaging methods including CT-scan, bone scan, and abdominal sonography or PET-CT.
Statistical Analysis
The differences in T, N and overall stage distributions between the TNM 6th and TNM 7th editions were compared using chi-square tests. The following endpoints were assessed: overall survival (OS), loco-regional recurrence-free survival (LRRFS), and distant metastasis-free survival (DMFS). The survival rate of OS, LRRFS and DMFS at 3 years and 5 years in percent are supplied in S2 Table.
The event for OS was defined as the duration from diagnosis until the date of death from any causes, or date of the last follow-up. LRRFS was the duration between the date of being diagnosed and the date of having event of loco-regional recurrence or date of the last follow-up. DMFS was defined as the duration from diagnosis until the date of metastasis, or date of the last follow-up. These endpoints were analyzed with a Kaplan-Meier method and a log-rank test. Multivariate analyses with the Cox proportional hazards model were used to test independence, significance, and hazard discrimination. Additionally, survival curves were plotted using the Cox multivariate model in addition to the Kaplan-Meier method. A two-tailed P value <0.05 was considered statistically significant. Above analyses were carried out using SPSS software (version 16.0, SPSS Inc., Chicago, IL, USA).
Results
Distributions and characteristics of NPC patients according to the TNM 6th edition and TNM 7th edition
The patients' distributions and characteristics are summarized in Table 1. The median age of the 2,629 patients was 50 years old (6–81 years old) and 1,956 (74.4%) were male. The median follow-up was 54.40 months (range; 1.23–87.20 months). The patients were treated with 2D-CRT (70.9% or 1,863 individuals), 3D-CRT (3.2% or 85 individuals), or IMRT (25.9% or 681 individuals) radiation therapies. The majority of the patients (1,956/2,629, 74.4%) were treated with combination chemoradiation therapy. Also, 622 (23.7%) patients were given induction chemotherapy (IC); 703 (26.7%) patients were given concurrent chemotherapy (CC); 16 (0.6%) patients were treated with adjuvant therapies. Furthermore, 545 (20.7%) patients were given IC and CC treatments and 28 (1.1%) patients were treated with CC and adjuvant chemotherapy. By comparing the distributions of the TNM 6th edition and TNM 7th edition, 37 (37/561, 6.6%) patients were down-staged from T2a with the TNM 6th edition to T1 with TNM 7th edition and 119 (119/670, 17.8%) patients were up-staged from N0 with the TNM 6th edition to N1 with the TNM 7th edition. Eventually, because of the presence of positive lymph nodes (N1-3) and T2-4 subsets, 2 patients were up-staged from stage I to II (2/118, 1.7%). Significant differences in the distribution between the TNM 6th edition and TNM 7th edition were found in N classification (χ2 = 20.589, p<0.001) but not in T classification (χ2 = 3.476, p = 0.325) or overall stage (χ2 = 0.220, p = 0.999; Table1).
Survival analyses of T categories according to the TNM 6th edition and TNM 7th edition
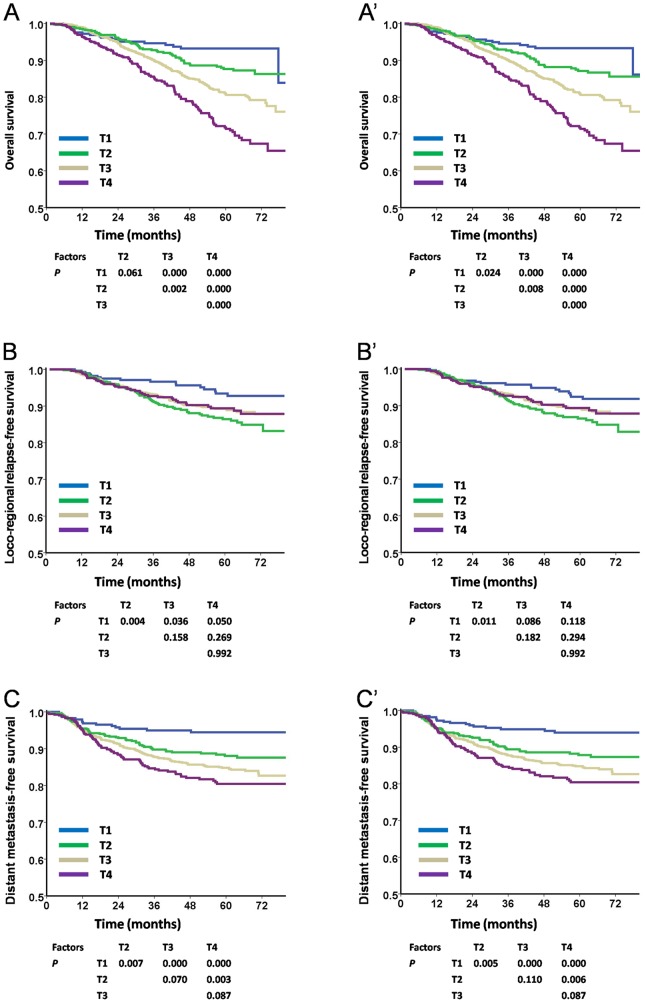
For OS, significant separations between adjacent stage categories were observed with the TNM 7th edition. However, the differences between T1 and T2 categories were not significant (P = 0.061) with the TNM 6th edition (Fig. 1A, and Fig. 1A′). With regard to LRRFS, there were nonsignificant survival curve segregations between adjacent stage categories of T2-T4 by both editions of the staging system (Figs. 1B and1B′). For DMFS, survival curves could be significantly segregated among each category of T classification (P<0.05) with both the TNM 6th edition and TNM 7th edition except for T2 vs. T3 and T3 vs. T4 (P>0.05; Figs. 1C and 1C′).
Figure 1. Survival analyses of T categories using the TNM 6th and the TNM 7th editions staging systems.
Panels A, B, and C were staged according to the TNM 6th edition, while panels A′, B′, and C′ were staged using the TNM 7th edition. In OS analysis, there were significant differences for each stage of T categories except for T1 vs. T2 in the TNM 6th edition (Panel 1A), which became significant in the TNM 7th edition (Panel 1A′). With regard to LRRFS, no significant differences were observed for each stage of T2-T4 subsets in both editions (Panels 1B and1B′). With regard to DMFS, both TNM 6th and TNM 7th editions showed distinct differences in survival among each stages of T categories except for T2 vs. T3 and T3 vs. T4 (Panels 1C and 1C′). UICC/AJCC: International Union Against Cancer stage system/American Joint Committee on Cancer; OS, overall survival; DMFS, distant metastasis-free survival; LRRFS, loco-regional recurrence-free survival.
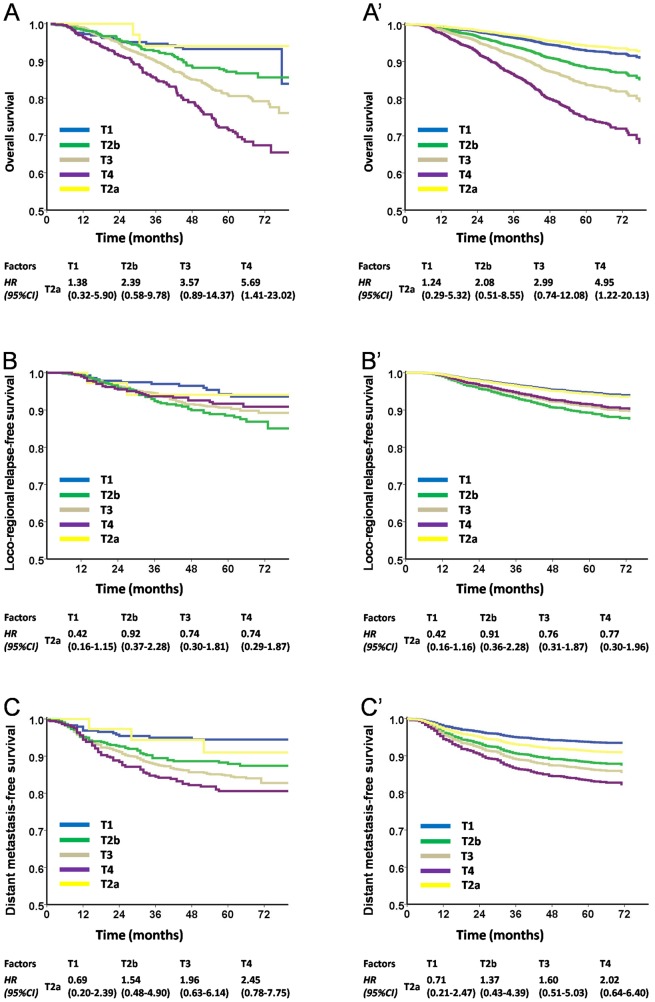
Further, we classified patients with nasal and/or oropharyngeal cavity invasion (T2a by the TNM 6th edition) as a separate subgroup. Our results showed that the hazard ratios (HRs) of T2a were similar to T1 (nasopharyngx invasion) in OS (before adjusted: HR = 1.38; after adjusted: HR = 1.24; Figs. 2A and 2A′), LRRFS (before adjusted: HR = 0.9; after adjusted: HR = 0.71; Figs. 2B and 2B′) and DMFS (before adjusted: HR = 0.69; after adjusted: HR = 0.71; Figs. 2C and 2C′), but differed significantly from T2b (parapharyngeal space invasion).
Figure 2. Survival analyses of the HRs of the T2a subset compared with other subsets using the TNM 6th edition staging system.
Panels A, B, and C were staged according to the TNM 6th edition staging system, while panels A′, B′, and C′ were plotted as estimated from the Cox multivariate model with adjustments for sex, age, histology, treatment modality, and radiotherapy techniques. In both statistical model, the hazard ratios (HRs) of T2a were similar to T1 in OS (Panels A and A′), LRRFS (Panels 2B and 2B′) and DMFS (Panels C and C′) but were significantly different from the T2b subset (parapharyngeal space invasion). HR: hazard ratio.
Survival analyses of N categories according to the TNM 6th edition and TNM 7th edition
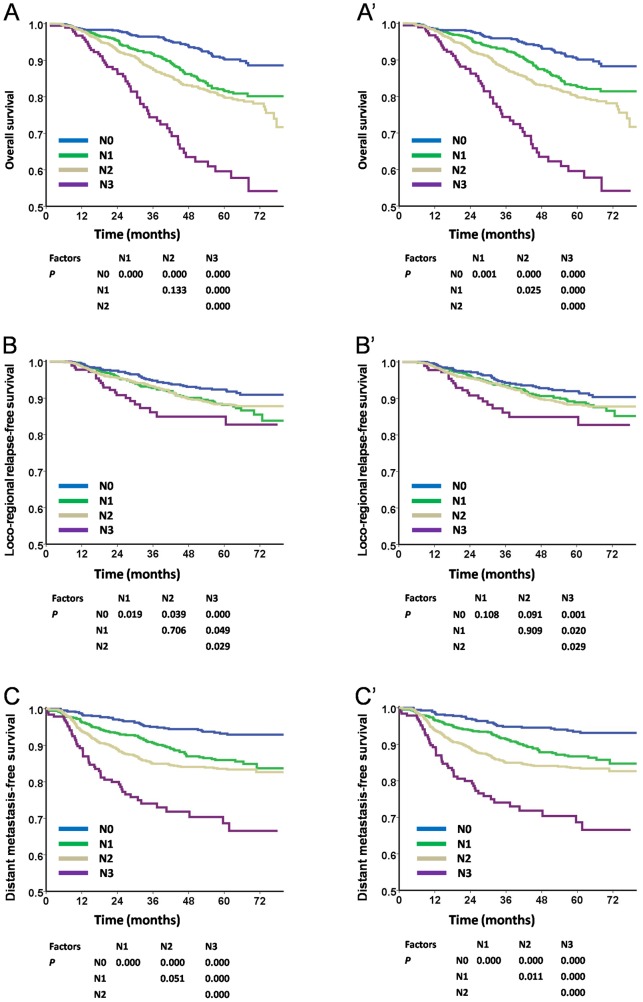
Significant survival curve separations were obtained between N1 and N2 with the TNM 7th edition in OS (P = 0.025) and DMFS (P = 0.011; Figs. 3A′ and 3C′). However, these differences were not significant with the TNM 6th edition. With respect to LRRFS, there was a non-significant survival difference between N1 and N2 according to the criteria of the TNM 6th edition and TNM 7th edition (Figs. 3B and 3B′).
Figure 3. Survival analyses of N categories using the TNM 6th and the TNM 7th editions staging systems.
Panels A, B, and C were staged according to the TNM 6th edition staging system, while panels A′, B′, and C′ were followed according to the TNM 7th edition. There were significant differences among each stage of N categories except for N1 vs. N2 in either OS or DMFS (Panels 3A and 3C) in the TNM 6th edition, while such differences became significant in the TNM 7th edition (Panels 3A′ and 3C′). However, neither the TNM 6th nor TNM 7th edition could distinguish the LRFFS between N1 and N2 (Panels 3B and 3B′).
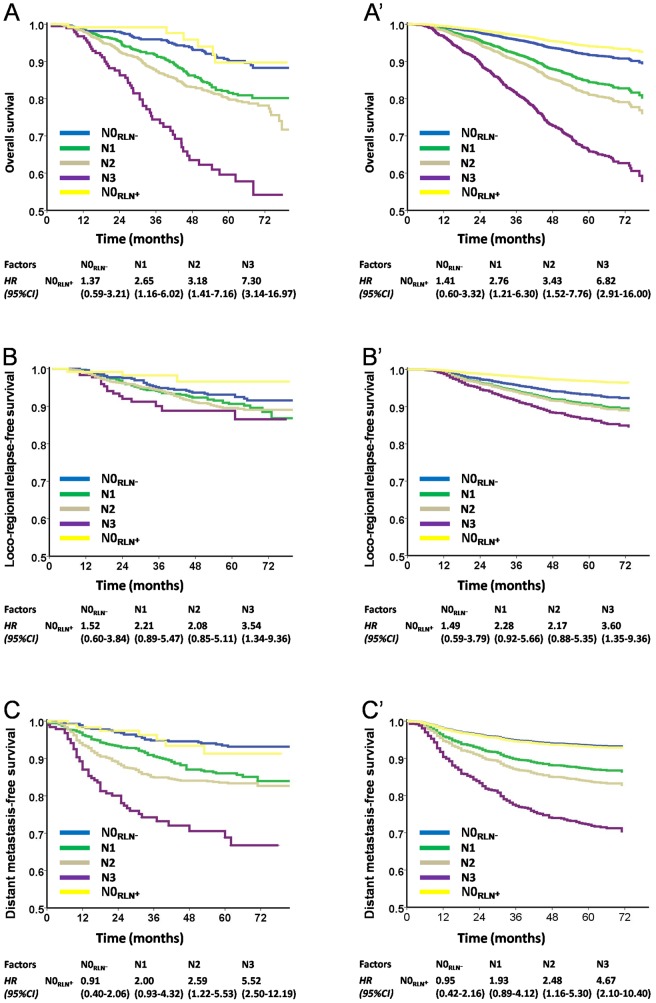
Further, we classified N0 patients with RLN metastasis (N0RLN+ by the TNM 6th edition) as a subgroup. The HRs of N0RLN+ were found to be similar to N0 without RLN metastasis (N0RLN-; before adjusted: OS, HR = 1.37, LRRFS, HR = 1.52 and DMFS, HR = 0.91; after adjusted: OS, HR = 1.41, LRRFS, HR = 1.49 and DMFS, HR = 0.95) but significantly different from the N1 category (before adjusted: OS, HR = 2.65, LRRFS, HR = 2.21 and DMFS, HR = 2.00; after adjusted: OS, HR = 2.76, LRRFS, HR = 2.28 and DMFS, HR = 1.93; Figs. 4A–4C′).
Figure 4. Survival analyses of the HRs of N0RLN+ subset comparing with other subsets using the TNM 6th staging system.
Panels A, B, and C were staged as the TNM 6th edition staging system, while panels A′, B′, and C′ were plotted as estimated from the Cox multivariate model with adjustments for sex, age, histology, treatment modality, and radiotherapy techniques. Patients with N0RLN+ were divided into a subgroup alone, the HRs of N0RLN+ was similar to N0RLN- in OS (Panels A and A′), LRRFS (Panels B and B′) and DMFS (Panels C and C′).
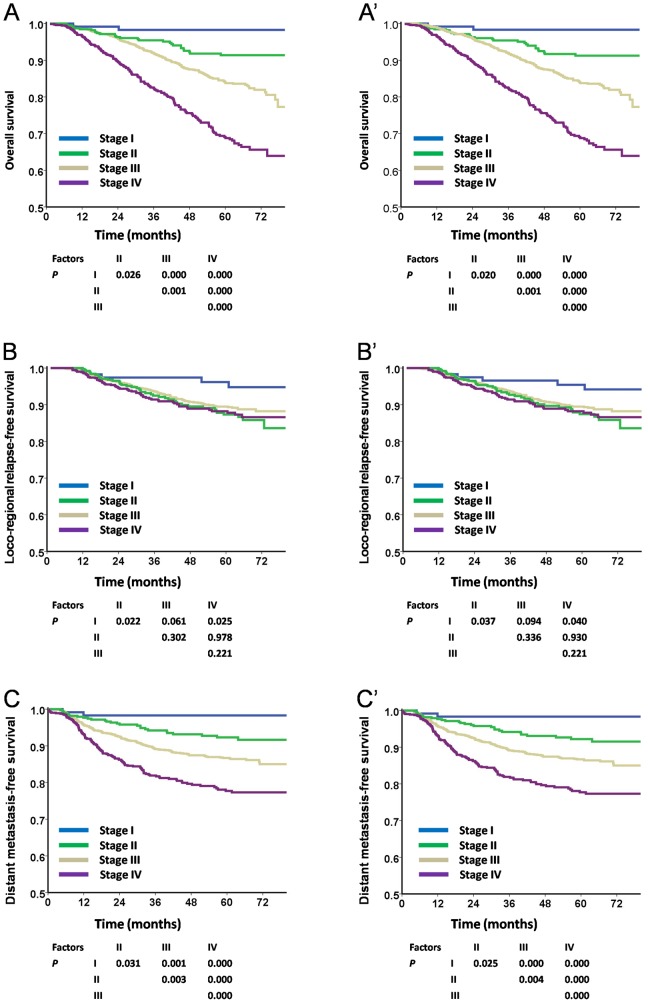
Survival analyses of overall stages according to the TNM 6th edition and TNM 7th edition
For OS and DMFS, significant separations were achieved between adjacent stage categories with the TNM 6th edition and TNM 7th edition (P<0.05; Figs. 5A and 5A′, 5C and 5C′, respectively). With respect to LRRFS, the differences were only observed between stage I and stage II (P = 0.022, P = 0.037, respectively) as well as stage I and stage IV (P = 0.025, P = 0.040, respectively) with the two editions of staging systems (Figs. 5B and 5B′).
Figure 5. Survival analyses of overall stage using the TNM 6th and the TNM 7th staging systems.
Panels A, B, and C were staged with the TNM 6th edition staging system, while panels A′, B′, and C′ followed the TNM 7th edition. Both 6th and 7th editions could distinctly separate the survival curves of each overall stage in OS and DMFS (Panels 5A and 5A′, 5C and 5C′). With regard to LRRFS, no significant differences were noted among each overall stage except that stage I showed significantly better survival than stage II and stage IV (Panels 5B and 5B′).
Multivariate analysis of T, N, and M categories according to the TNM 6th edition and TNM 7th edition
We conducted a Cox model multivariate analysis after adjusting for gender, age, and treatments and the results revealed that T, N, and M classifications were independent prognostic factors for OS and DMFS by both the TNM 6th edition and TNM 7th edition (P<0.05), but not for LRRFS (P>0.05; Table 3 and S3 Table).
Table 3. Multivariate analysis of independent prognostic factors in NPC patients.
| TNM6th | TNM7th | ||||||||
| End point | Variable | Univariate analysis | Multivariate analysis | Univariate analysis | Multivariate analysis | ||||
| HR(95% CI) | P value | HR(95% CI) | P value | HR(95% CI) | P value | HR(95% CI) | P value | ||
| Distant failure | T Classification | <0.001 | 0.002 | <0.001 | 0.002 | ||||
| T1 | reference | reference | reference | reference | |||||
| T2 | 2.157(1.225–3.797) | 0.008 | 1.905(1.079–3.366) | 0.026 | 2.099(1.236–3.566) | 0.006 | 1.840(1.080–3.136) | 0.025 | |
| T3 | 2.839(1.675–4.813) | <0.001 | 2.280(1.333–3.901) | 0.003 | 2.693(1.657–4.377) | <0.001 | 2.148(1.310–3.521) | 0.002 | |
| T4 | 3.526(2.037–6.103) | <0.001 | 2.822(1.611–4.943) | <0.001 | 3.344(2.012–5.559) | <0.001 | 2.634(1.565–4.431) | <0.001 | |
| N Classification | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| N0 | 0.464(0.318–0.677) | <0.001 | 0.502(0.342–0.736) | <0.001 | 0.491(0.329–0.734) | 0.001 | 4.679(2.947–7.431) | <0.001 | |
| N1 | reference | reference | reference | reference | |||||
| N2 | 1.305(1.004–1.698) | 0.047 | 1.275(0.978–1.663) | 0.073 | 1.404(1.086–1.814) | 0.009 | 1.358(1.047–1.760) | 0.021 | |
| N3 | 2.741(1.929–3.896) | <0.001 | 2.378(1.661–3.405) | <0.001 | 2.948(2.885–4.169) | <0.001 | 2.530(1.774–3.607) | <0.001 | |
| M Classification | |||||||||
| M0 | reference | reference | reference | reference | |||||
| M1 | 4.611(3.105–6.846) | <0.001 | 3.343(2.228–5.015) | <0.001 | 4.611(3.105–6.846) | <0.001 | 3.421(2.281–5.132) | <0.001 | |
| Death | T Classification | <0.001 | <0.001 | <0.001 | <0.001 | ||||
| T1 | reference | reference | reference | reference | |||||
| T2 | 1.656(0.986–2.780) | 0.056 | 1.641(0.974–2.764) | 0.063 | 1.797(1.088–2.967) | 0.022 | 1.737(1.048–2.877) | 0.032 | |
| T3 | 2.595(1.620–4.156) | <0.001 | 2.459(1.520–3.977) | <0.001 | 2.687(1.713–4.216) | <0.001 | 2.489(1.572–3.942) | <0.001 | |
| T4 | 4.135(2.549–6.706) | <0.001 | 4.017(2.442–6.608) | <0.001 | 4.283(2.695–6.806) | <0.001 | 4.038(2.503–6.513) | <0.001 | |
| N Classification | <0.001 | <0.001 | <0.001 | <0.001 | |||||
| N0 | 0.497(0.357–0.691) | <0.001 | 0.488(0.349–0.682) | <0.001 | 0.563(0.400–0.792) | 0.001 | 0.563(0.398–0.796) | 0.001 | |
| N1 | reference | reference | reference | reference | |||||
| N2 | 1.200(0.944–1.526) | 0.136 | 1.246(0.977–1.589) | 0.076 | 1.307(1.032–1.655) | 0.026 | 1.359(1.070–1.727) | 0.012 | |
| N3 | 2.761(1.986–3.836) | <0.001 | 2.478(1.766–3.478) | <0.001 | 3.007(2.170–4.166) | <0.001 | 2.696(1.925–3.776) | <0.001 | |
| M Classification | |||||||||
| M0 | reference | reference | reference | reference | |||||
| M1 | 5.098(3.524–7.374) | <0.001 | 3.576(2.443–5.234) | <0.001 | 5.098(3.524–7.374) | <0.001 | 3.653(2.496–5.345) | <0.001 | |
| Loco-regional relapse | T Classification | 0.114 | 0.135 | 0.071 | 0.079 | ||||
| T1 | reference | reference | reference | reference | |||||
| T2 | 2.053(1.138–3.705) | 0.017 | 2.026(1.118–3.674) | 0.02 | 2.110(1.202–3.706) | 0.009 | 2.100(1.189–3.707) | 0.011 | |
| T3 | 1.718(0.980–3.011) | 0.059 | 1.747(0.982–3.109) | 0.058 | 1.702(1.002–2.891) | 0.049 | 1.736(1.006–2.998) | 0.048 | |
| T4 | 1.590(0.855–2.955) | 0.143 | 1.629(0.857–3.098) | 0.137 | 1.575(0.871–2.846) | 0.133 | 1.604(0.866–2.972) | 0.133 | |
| N Classification | 0.035 | 0.056 | 0.087 | 0.169 | |||||
| N0 | 0.691(0.459–1.040) | 0.077 | 0.673(0.442–1.023) | 0.064 | 0.831(0.549–1.258) | 0.381 | 0.823(0.538–1.260) | 0.37 | |
| N1 | reference | reference | reference | reference | |||||
| N2 | 1.043(0.744–1.463) | 0.807 | 1.035(0.735–1.456) | 0.845 | 1.146(0.821–1.599) | 0.423 | 1.129(0.806–1.582) | 0.481 | |
| N3 | 1.547(0.898–2.664) | 0.116 | 1.479(0.849–2.578) | 0.167 | 1.699(0.990–2.917) | 0.054 | 1.606(0.924–2.792) | 0.093 | |
| M Classification | |||||||||
| M0 | reference | reference | reference | reference | |||||
| M1 | 2.084(0.978–4.441) | 0.057 | 1.695(0.783–3.667) | 0.18 | 2.084(0.978–4.441) | 0.057 | 1.714(0.793–3.706) | 0.171 | |
Abbreviation: HR = Hazard Ratio, derived from COX proportional hazard model.
Discussion
Recently, several studies have compared the TNM 6th edition with the TNM 7th edition. Unfortunately, the results have been heterogeneous. In a panel of 903 Chinese NPC patients, Sun et al. observed non-significant differences in prognosis prediction between T2a and T1 categories using the two editions of the UICC/AJCC staging system [12]. Another recent study by OuYang et al. assessed the prognostic value of the two editions of the TNM staging system by combining analyses of the Akaike information criterion (AIC) and Harrell's concordance index (c-index). They concluded that the TNM 6th edition T-classification had superior prognostic value to the TNM 7th edition. However, FFS was the only factor evaluated following end points [22]. Since clearly elucidating the superiority of the current staging system is critical for treatment choice and prognosis prediction [23], [24], we performed a retrospective study with a large sample size of 2,629 NPC patients. In this study, we compared the prognostic value of the TNM 6th edition and TNM 7th edition based on the significant separations of survival curves for OS, LRRFS and DMFS, which were the most widely used practices in cancer research. Our study revealed that there was a significant difference and better survival curve segregations between T1 and T2 (for OS), N1and N2 (for OS and DMFS) according to the TNM 7th edition.
Considering suggestions from previous studies regarding the prognosis of certain features in TNM 6th edition staging criteria [25], [26], [27], it was not unexpected to observe improvement with the TNM 7th edition, and our aim was to validate these results.
For the T-classification, our study revealed that with the TNM 7th edition, a significant difference and better survival curve segregation between T1 and T2 were obtained in OS analysis. Moreover, the rationality of the TNM 7th edition was reconfirmed based on the findings of the proportional hazards analyses. These observations were consistent with a series of previous studies, where they found no significant differences between T2a and T1 categories in the risks of disease failures and survival rates, and proposed that T2a should be categorized as T1 [25], [26], [27], [28], [29]. On the contrary, Sun et al. did not find significant differences between T2a and T1 in either of the two editions. The discordance might be partly due to the different sample sizes, where a total of 2,629 patients were recruited in our study but only 903 patients participated in their study. Interestingly, reverse results were obtained by OuYang et al. As different following end points and statistical models were used between the two studies, further research using the data of patients from other centers is required.
With regard to N-classification, subsequent retrospective studies revealed that RLN metastasis, regardless of laterality, had a poorer prognosis than node-negative disease [30], [31], [32], [33]. However, reverse evidence showed that RLN metastases did not influence OS and DMFS [12], [34], [35]. Because of the uncertain prognostic value of RLN metastasis, we classified patients with positive RLN as a subgroup alone, and found the similarity of risks of disease failure between N0RLN+ and N0RLN- , but different from N1. In addition, our results also revealed that classifying RLN metastasis to N1 obtained better survival curve separations between N1 and N2 in OS and DMFS according to the TNM 7th edition. The following reasons may explain the heterogeneous results regarding the prognostic value of RLN metastasis between our model and previous studies. On the one hand, cumulative studies have reported that the use of MRI was associated with improved tumor control and survival of NPC patients because a higher radiation dose could be delivered to the tumor by the external beam, which led to better tumor control [36], [37]. On the other hand, the visible RLNs were outlined with the primary tumor as GTV and received higher dose irradiation than cervical lymph nodes using either IMRT or 2D-CRT techniques, which eventually led to satisfactory control of RLN. Therefore, it is acceptable that RLN involvement did not significantly influence the prognosis of NPC patients due to the improvement of tumor extent visualization. Further validations with data from multiple centers are required and we are currently planning these studies.
With respect to overall stage, both editions had distinct survival curves in OS and DMFS, which is consistent with the previous findings by Rui et al. [38]. However, with regard to LRRFS, neither edition had significant survival curves separations. An important reason might be the increased local control rates with benefits from the improvement of imaging and radiotherapy modalities and the widespread use of combined chemo-radiotherapy. It has been suggested that MRI had an influence on local tumor control, with around a 20% improvement in the local control rate for NPC [39]. 3D-CRT and IMRT had remarkable advantages in providing better tumor target coverage and allowed the delivery of a high dose to the gross tumor while significantly reducing the dose to the surrounding normal tissues [40], [41]. Therefore, it is urgent to search for a marker to improve the prognostic predication of LRRFS, which is what we are currently planning.
Conclusion
The TNM 7th staging system had superior performance to the TNM 6th edition in predicting OS and DMFS, and significant alterations in the distribution of N classification. As these findings were limited due to being a retrospective study in a single center, further studies in multicenters or employing a prospective method are needed to validate these findings.
Supporting Information
Baseline clinical characteristics of the 2,671 nasopharyngeal carcinoma patients.
(DOC)
Comparison of the survival rate by TNM 6th and TNM 7th staging system.
(DOC)
Multivariate analysis of independent prognostic factors in NPC patients.
(DOC)
Acknowledgments
We thank You-Yuan Yao, Li-Na Feng, Rou Jiang and Tong-Tong Liu for their assistance in this study.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Program for New Century Excellent Talents in University (NCET-12-0562), Sun Yat-Sen University Clinical Research 5010 Program (201310), National Natural Science Foundation of China (Grants No. 81071890), Guangdong Provincial Natural Science Foundation of China (S2013020012726), and National High Technology Research and Development Program of China (863 Program, No. 2012AA02A501). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Wei WI, Sham JS (2005) Nasopharyngeal carcinoma. Lancet 365:2041–2054. [DOI] [PubMed] [Google Scholar]
- 2. Yu MC, Yuan JM (2002) Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol 12:421–429. [DOI] [PubMed] [Google Scholar]
- 3. Lee AW, Lau WH, Tung SY, Chua DT, Chappell R, et al. (2005) Preliminary results of a randomized study on therapeutic gain by concurrent chemotherapy for regionally-advanced nasopharyngeal carcinoma: NPC-9901 Trial by the Hong Kong Nasopharyngeal Cancer Study Group. J Clin Oncol 23:6966–6975. [DOI] [PubMed] [Google Scholar]
- 4. Ma J, Mai HQ, Hong MH, Cui NJ, Lu TX, et al. (2001) Is the 1997 AJCC staging system for nasopharyngeal carcinoma prognostically useful for Chinese patient populations? Int J Radiat Oncol Biol Phys 50:1181–1189. [DOI] [PubMed] [Google Scholar]
- 5. Gospodarowicz MK, Miller D, Groome PA, Greene FL, Logan PA, et al. (2004) The process for continuous improvement of the TNM classification. Cancer 100:1–5. [DOI] [PubMed] [Google Scholar]
- 6. Greene FL, Sobin LH (2008) The staging of cancer: a retrospective and prospective appraisal. CA Cancer J Clin 58:180–190. [DOI] [PubMed] [Google Scholar]
- 7. Kalogera-Fountzila A, Karanikolas D, Katodritis N, Samantas E, Sarafopoulos A, et al. (2006) Prognostic factors and significance of the revised 6th edition of the AJCC classification in patients with locally advanced nasopharyngeal carcinoma. Strahlenther Onkol 182:458–466. [DOI] [PubMed] [Google Scholar]
- 8. Casselman JW (1994) The value of MRI in the diagnosis and staging of nasopharynx tumors. J Belge Radiol 77:67–71. [PubMed] [Google Scholar]
- 9. Ho HC, Lee MS, Hsiao SH, Hwang JH, Hung SK, et al. (2008) Prognostic influence of parapharyngeal extension in nasopharyngeal carcinoma. Acta Otolaryngol 128:790–798. [DOI] [PubMed] [Google Scholar]
- 10. Neel HR, Taylor WF, Pearson GR (1985) Prognostic determinants and a new view of staging for patients with nasopharyngeal carcinoma. Ann Otol Rhinol Laryngol 94:529–537. [DOI] [PubMed] [Google Scholar]
- 11. Tang LL, Li WF, Chen L, Sun Y, Chen Y, et al. (2010) Prognostic value and staging categories of anatomic masticator space involvement in nasopharyngeal carcinoma: a study of 924 cases with MR imaging. Radiology 257:151–157. [DOI] [PubMed] [Google Scholar]
- 12. Sun R, Qiu HZ, Mai HQ, Zhang Q, Hong MH, et al. (2013) Prognostic value and differences of the sixth and seventh editions of the UICC/AJCC staging systems in nasopharyngeal carcinoma. J Cancer Res Clin Oncol 139:307–314. [DOI] [PubMed] [Google Scholar]
- 13. Lai SZ, Li WF, Chen L, Luo W, Chen YY, et al. (2011) How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys 80:661–668. [DOI] [PubMed] [Google Scholar]
- 14. Kalogera-Fountzila A, Karanikolas D, Katodritis N, Samantas E, Sarafopoulos A, et al. (2006) Prognostic factors and significance of the revised 6th edition of the AJCC classification in patients with locally advanced nasopharyngeal carcinoma. Strahlenther Onkol 182:458–466. [DOI] [PubMed] [Google Scholar]
- 15. Lai SZ, Li WF, Chen L, Luo W, Chen YY, et al. (2011) How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys 80:661–668. [DOI] [PubMed] [Google Scholar]
- 16. Li WF, Sun Y, Chen M, Tang LL, Liu LZ, et al. (2012) Locoregional extension patterns of nasopharyngeal carcinoma and suggestions for clinical target volume delineation. Chin J Cancer 31:579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edge S, Byrd DR, Compton CC, Fritz AG, Greene FL, et al. (2010) AJCC cancer staging handbook from the AJCC cancer stagnig manual, 7th edn. New York. pp. p63–p79.
- 18. Zhang GY, Liu LZ, Wei WH, Deng YM, Li YZ, et al. (2010) Radiologic criteria of retropharyngeal lymph node metastasis in nasopharyngeal carcinoma treated with radiation therapy. Radiology 255:605–612. [DOI] [PubMed] [Google Scholar]
- 19. Ma J, Liu L, Tang L, Zong J, Lin A, et al. (2007) Retropharyngeal lymph node metastasis in nasopharyngeal carcinoma: prognostic value and staging categories. Clin Cancer Res 13:1445–1452. [DOI] [PubMed] [Google Scholar]
- 20. Spratt DE, Lee N (2012) Current and emerging treatment options for nasopharyngeal carcinoma. Onco Targets Ther 5:297–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen MY, Jiang R, Guo L, Zou X, Liu Q, et al. (2013) Locoregional radiotherapy in patients with distant metastases of nasopharyngeal carcinoma at diagnosis. Chin J Cancer 32:604–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. OuYang PY, Su Z, Ma XH, Mao YP, Liu MZ, et al. (2013) Comparison of TNM staging systems for nasopharyngeal carcinoma, and proposal of a new staging system. Br J Cancer 109:2987–2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Groome PA, Schulze K, Boysen M, Hall SF, Mackillop WJ (2001) A comparison of published head and neck stage groupings in carcinomas of the oral cavity. Head Neck 23:613–624. [DOI] [PubMed] [Google Scholar]
- 24. Sayegh ME, Sano T, Dexter S, Katai H, Fukagawa T, et al. (2004) TNM and Japanese staging systems for gastric cancer: how do they coexist? Gastric Cancer 7:140–148. [DOI] [PubMed] [Google Scholar]
- 25. Lee AW, Au JS, Teo PM, Leung TW, Chua DT, et al. (2004) Staging of nasopharyngeal carcinoma: suggestions for improving the current UICC/AJCC Staging System. Clin Oncol (R Coll Radiol) 16:269–276. [DOI] [PubMed] [Google Scholar]
- 26. Mao YP, Xie FY, Liu LZ, Sun Y, Li L, et al. (2009) Re-evaluation of 6th edition of AJCC staging system for nasopharyngeal carcinoma and proposed improvement based on magnetic resonance imaging. Int J Radiat Oncol Biol Phys 73:1326–1334. [DOI] [PubMed] [Google Scholar]
- 27. Liu MZ, Tang LL, Zong JF, Huang Y, Sun Y, et al. (2008) Evaluation of sixth edition of AJCC staging system for nasopharyngeal carcinoma and proposed improvement. Int J Radiat Oncol Biol Phys 70:1115–1123. [DOI] [PubMed] [Google Scholar]
- 28. Hong MH, Mai HQ, Min HQ, Ma J, Zhang EP, et al. (2000) A comparison of the Chinese 1992 and fifth-edition International Union Against Cancer staging systems for staging nasopharyngeal carcinoma. Cancer 89:242–247. [DOI] [PubMed] [Google Scholar]
- 29. Au JS, Law CK, Foo W, Lau WH (2003) In-depth evaluation of the AJCC/UICC 1997 staging system of nasopharyngeal carcinoma: prognostic homogeneity and proposed refinements. Int J Radiat Oncol Biol Phys 56:413–426. [DOI] [PubMed] [Google Scholar]
- 30. Ma J, Liu L, Tang L, Zong J, Lin A, et al. (2007) Retropharyngeal lymph node metastasis in nasopharyngeal carcinoma: prognostic value and staging categories. Clin Cancer Res 13:1445–1452. [DOI] [PubMed] [Google Scholar]
- 31. Chong VF, Fan YF, Khoo JB (1995) Retropharyngeal lymphadenopathy in nasopharyngeal carcinoma. Eur J Radiol 21:100–105. [DOI] [PubMed] [Google Scholar]
- 32. Tang L, Li L, Mao Y, Liu L, Liang S, et al. (2008) Retropharyngeal lymph node metastasis in nasopharyngeal carcinoma detected by magnetic resonance imaging : prognostic value and staging categories. Cancer 113:347–354. [DOI] [PubMed] [Google Scholar]
- 33. Tham IW, Hee SW, Yap SP, Tuan JK, Wee J (2009) Retropharyngeal nodal metastasis related to higher rate of distant metastasis in patients with N0 and N1 nasopharyngeal cancer. Head Neck 31:468–474. [DOI] [PubMed] [Google Scholar]
- 34. Chua DT, Sham JS, Kwong DL, Au GK, Choy DT (1997) Retropharyngeal lymphadenopathy in patients with nasopharyngeal carcinoma: a computed tomography-based study. Cancer 79:869–877. [PubMed] [Google Scholar]
- 35. Ng WT, Lee AW, Kan WK, Chan J, Pang ES, et al. (2007) N-staging by magnetic resonance imaging for patients with nasopharyngeal carcinoma: pattern of nodal involvement by radiological levels. Radiother Oncol 82:70–75. [DOI] [PubMed] [Google Scholar]
- 36. Chang JT, Lin CY, Chen TM, Kang CJ, Ng SH, et al. (2005) Nasopharyngeal carcinoma with cranial nerve palsy: the importance of MRI for radiotherapy. Int J Radiat Oncol Biol Phys 63:1354–1360. [DOI] [PubMed] [Google Scholar]
- 37. Liao XB, Mao YP, Liu LZ, Tang LL, Sun Y, et al. (2008) How does magnetic resonance imaging influence staging according to AJCC staging system for nasopharyngeal carcinoma compared with computed tomography? Int J Radiat Oncol Biol Phys 72:1368–1377. [DOI] [PubMed] [Google Scholar]
- 38. Sun R, Qiu HZ, Mai HQ, Zhang Q, Hong MH, et al. (2013) Prognostic value and differences of the sixth and seventh editions of the UICC/AJCC staging systems in nasopharyngeal carcinoma. J Cancer Res Clin Oncol 139:307–314. [DOI] [PubMed] [Google Scholar]
- 39. Chang JT, Lin CY, Chen TM, Kang CJ, Ng SH, et al. (2005) Nasopharyngeal carcinoma with cranial nerve palsy: the importance of MRI for radiotherapy. Int J Radiat Oncol Biol Phys 63:1354–1360. [DOI] [PubMed] [Google Scholar]
- 40.(2001) Intensity-modulated radiotherapy: current status and issues of interest. Int J Radiat Oncol Biol Phys 51:880–914. [DOI] [PubMed] [Google Scholar]
- 41. Sultanem K, Shu HK, Xia P, Akazawa C, Quivey JM, et al. (2000) Three-dimensional intensity-modulated radiotherapy in the treatment of nasopharyngeal carcinoma: the University of California-San Francisco experience. Int J Radiat Oncol Biol Phys 48:711–722. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Baseline clinical characteristics of the 2,671 nasopharyngeal carcinoma patients.
(DOC)
Comparison of the survival rate by TNM 6th and TNM 7th staging system.
(DOC)
Multivariate analysis of independent prognostic factors in NPC patients.
(DOC)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.