Abstract
In July 2012 the IFCPC adopted a revised terminology for colposcopic examinations of the uterine cervix. In 2012, the Boards of the Arbeitsgemeinschaft Kolposkopie (AGK – Austrian Society of Colposcopy), the Arbeitsgemeinschaft für Kolposkopie und Zervixpathologie (AGKOL – Swiss Society of Colposcopy and Cervical Pathology) and the Arbeitsgemeinschaft für Kolposkopie und Zervixpathologie (AGCPC – German Society of Colposcopy and Cervical Pathology) accepted the validity of the 2011 IFCPC nomenclature and recommended its use in general clinical practice across German-speaking countries. The revised nomenclature was devised so that examiners can evaluate colposcopic criteria according to a specific scheme. At the start of the examination, the examiner must assess whether the colposcopy is representative or not. 1. Can the examination be classed as adequate or inadequate (reasons must be given)? 2. How would you describe the visibility of the squamocolumnar junction and categorize the transformation zone? Below we discuss some aspects of this general assessment as outlined in the nomenclature which were found to require further clarification for general practice.
Key words: colposcopy, cervix uteri, nomenclature, IFCPC Rio de Janeiro 2011, transformation zone, adequate colposcopy, inadequate colposcopy
Abstract
Zusammenfassung
Im Juli 2012 wurde eine überarbeitete Nomenklatur zur kolposkopischen Untersuchung der Cervix uteri durch die IFCPC verabschiedet. 2012 erfolgte eine durch die Vorstände der Arbeitsgemeinschaft Kolposkopie (AGK, Österreich), der Arbeitsgemeinschaft für Kolposkopie und Zervixpathologie (AGKOL, Schweiz) und der Arbeitsgemeinschaft für Kolposkopie und Zervixpathologie (AGCPC, Deutschland) anerkannte Darstellung mit Empfehlung zur Nutzung für den deutschsprachigen Raum. Die Nomenklatur ist so aufgebaut, dass der Untersucher nach einem bestimmten Schema kolposkopische Kriterien beurteilen soll. Zu Beginn der kolposkopischen Untersuchung wird geprüft, ob die Kolposkopie repräsentativ ist: 1. Ist die Untersuchung als adäquat oder inadäquat (mit Begründung) einzuschätzen? 2. Wie sind die Einsehbarkeit der Plattenepithel-Zylinderepithelgrenze und der Typus der Transformationszone zu bewerten? Im Folgenden wird auf einige Aspekte dieser grundsätzlichen Vorbemerkungen der Nomenklatur eingegangen, die sich im praktischen Gebrauch als klärungsbedürftig erwiesen haben.
Schlüsselwörter: Kolposkopie, Cervix uteri, Nomenklatur, IFCPC Rio de Janeiro 2011, Transformationszone, adäquate Kolposkopie, inadäquate Kolposkopie
Introduction
The current colposcopic nomenclature was published on July 1, 2012 in Obstetrics & Gynecology 1.
In Frauenarzt 2012 2 and Geburtshilfe & Frauenheilkunde 2013 8, the Boards of the Arbeitsgemeinschaft Kolposkopie (AGK – Austrian Society of Colposcopy), the Arbeitsgemeinschaft für Kolposkopie und Zervixpathologie (AGKOL – Swiss Society of Colposcopy and Cervical Pathology) and the Arbeitsgemeinschaft für Kolposkopie und Zervixpathologie (AGCPC – German Society of Colposcopy and Cervical Pathology) accepted the validity of the revised nomenclature and recommended its use in general clinical practice across German-speaking countries.
It must be emphasized that one of the primary aims of the new IFCPC nomenclature was to create a closer association between terminology and therapeutic procedures. Examples for this include the introduction of a grading to describe the visibility of the squamocolumnar junction and the types of excision outlined in the Addendum.
In the authorsʼ opinion, this is a welcome step as it simplifies individualized planning and implementation of treatment. See also various publications on this point (e.g. Kühn 2011 7, Reich & Fritsch 2014 9). Overall, the new colposcopy nomenclature emphasizes the significance of colposcopic investigations more than the preceding version did.
It is particularly gratifying that two recent publications from Germany (Scheungraber et al. 3, 4) were also incorporated in the revised nomenclature.
It should be noted that the distinction between lesions located inside and those located outside the transformation zone described in the nomenclature (an important distinction in clinical practice) as well as the significance of superficial expansion of abnormal colposcopic findings in the uterine cervix were scientifically confirmed by publications from German-speaking countries 5, 6.
Some aspects, which were found to require further clarification for general practice, are discussed below.
Adequate or Inadequate
The colposcopy nomenclature for the uterine cervix and the vagina begins with a basic but fundamentally important distinction: Is the colposcopic examination “adequate” (doable) or “inadequate” (not doable); if it is inadequate, the reason why it is unfeasible must be stated. These terms have replaced the former terminology “satisfactory/unsatisfactory colposcopy”. This change aimed to emphasize that in cases where colposcopy was inadequate, e.g. due to inflammation, a control examination must be performed after treatment (Fig. 1). Shifting the questions whether an assessment is doable and whether the colposcopic examination is valid to the beginning of the nomenclature emphasizes the significance of these criteria.
Fig. 1.
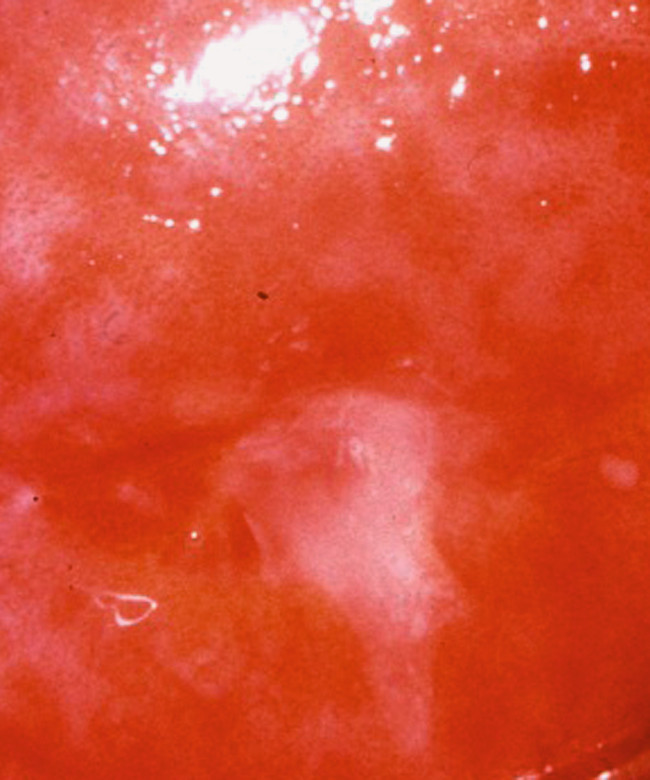
Inadequate conditions for colposcopic assessment, inflammation.
It is important to emphasize that even if the border between squamous and columnar epithelium is not entirely visible (transformation zone type 3), it may still be possible to carry out an adequate colposcopic examination, and this is usually the case (Fig. 4). Adequate colposcopic examination thus refers to the general condition under which a colposcopic examination is carried out. Assessment of the type of transformation zone is virtually only possible in adequate conditions (Fig. 2).
Fig. 4.

Adequate conditions for colposcopic assessment, transformation zone type 3; only limited assessment of the transformation zone is possible.
Fig. 2.

Adequate conditions for colposcopic assessment, transformation zone type 1.
Border between Squamous and Columnar Epithelium and Transformation Zone
Basically, assessment of the transformation zone and classification into the respective transformation zones type 1, 2 or 3 is done after the application of acetic acid.
The transformation zone in its native state is usually gray to red. After cleaning with a dry swab, colposcopic observation will usually show a network of regular branching vessels (an indication that the vessels are unremarkable), openings of the cervical glands, and the nabothian glands. With the exception of the vessels, all of these structures are more clearly visible after the application of acetic acid. The border between squamous and columnar epithelium is a sharp, often demarcated border between the grape-like columnar epithelium and the metaplastic squamous epithelium and is more or less visible on colposcopy.
Localizing the border between squamous and columnar epithelium is the prerequisite for classifying the transformation zone as type 1, 2 or 3.
The two terms (border between squamous and columnar epithelium, transformation zone) describe two different but overlapping aspects. The border between squamous and columnar epithelium constitutes the “inner” margin of the transformation zone. It can be “completely visible”, “partially visible” or even “not visible”. If a transformation zone 1 or 2 is present, the border between squamous and columnar epithelium will be entirely visible.
A transformation zone is classified as type 1 when it is entirely ectocervical (without any endocervical portion) (Fig. 2). Transformation zones type 2 and 3 always have an endocervical portion, meaning that the border between squamous and columnar epithelium extends into the cervical canal. If the border is completely visible, it is referred to as a type 2 transformation zone. Visualization of the border can be done with or without additional instruments (endospeculum) (Fig. 3 a and b). The transformation zone is only classified as type 3 if the border between squamous and columnar epithelium is not completely visible (even with the help of additional instruments) (Fig. 4). If this is the case, colposcopy can only provide information about the visible part of the transformation zone; however, if the conditions for colposcopic examination are otherwise optimal, this examination must still be classified as adequate.
Fig. 3 a.
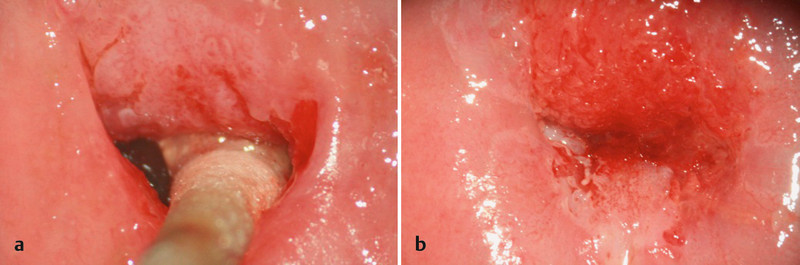
and b Adequate conditions for colposcopic assessment, transformation zone type 2.
As mentioned above, one of the aims of the nomenclature commission of the IFCPC was to improve the planning of potentially necessary therapeutic options. Evaluation of these two aspects makes this easier, for example, when planning the targeted excision of the lesion (type of excision).
Three different types of excision are mentioned in the addendum to the nomenclature, which also included for the first time the dimensions of excision specimens. The excision types link the different transformation types to clinical practice; the aim is to replace the continued use of a wide range of excision terms by descriptions of the types of excision performed and not the methods used for excision.
Supporting Information
German supporting information for this article
References
- 1.Bornstein J, Bentley J, Bösze P. et al. 2011 colposcopic terminology of the International Federation for Cervical Pathology and Colposcopy. Obstet Gynecol. 2012;120:166–172. doi: 10.1097/AOG.0b013e318254f90c. [DOI] [PubMed] [Google Scholar]
- 2.Girardi F, Frey Tirri B, Küppers V. et al. Neue kolposkopische IFCPC-Nomenklatur der Cervix uteri (Rio de Janeiro 2011) Frauenarzt. 2012;53:1064–1065. [Google Scholar]
- 3.Scheungraber C, Glutig K, Fechtel B. et al. Inner border—a specific and significant colposcopic sign for moderate or severe dysplasia (cervical intraepithelial neoplasia 2 or 3) J Low Genit Tract Dis. 2009;13:1–4. doi: 10.1097/LGT.0b013e31817ff92a. [DOI] [PubMed] [Google Scholar]
- 4.Scheungraber C, Koenig U, Fechtel B. et al. The colposcopic feature ridge sign is associated with the presence of cervical intraepithelial neoplasia 2/3 and human papillomavirus 16 in young women. J Low Genit Tract Dis. 2009;13:13–16. doi: 10.1097/LGT.0b013e318180438a. [DOI] [PubMed] [Google Scholar]
- 5.Girardi F, Reich O, Tamussino K. Stuttgart: Thieme; 2014. Burghardtʼs Colposcopy and cervical Pathology. 4th ed. [Google Scholar]
- 6.Fritsch H, Hoermann R, Bitsche M. et al. Development of epithelial and mesenchymal regionalization of the human fetal utero-vaginal anlagen. J Anat. 2013;222:462–472. doi: 10.1111/joa.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kühn W. Kolposkopie zur Früherkennung des Zervixkarzinoms. Pathologe. 2011;32:497–504. doi: 10.1007/s00292-011-1480-9. [DOI] [PubMed] [Google Scholar]
- 8.Quaas J, Reich O, Frey Tirri B. et al. Explanation and use of the colposcopy terminology of the IFCPC (International Federation for Cervical Pathology and Colposcopy) Rio 2011. Geburtsh Frauenheilk. 2013;73:904–907. doi: 10.1055/s-0033-1350824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Reich O, Fritsch H. The developmental origin of cervical and vaginal epithelium and their clinical consequences: a systematic review. J Low Genit Tract Dis. 2014;18:358–360. doi: 10.1097/LGT.0000000000000023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
German supporting information for this article


