Abstract
BACKGROUND
This study examined gender differences in the impact of warfare exposure on self-reported physical health.
METHODS
Data are from the 2010 National Survey of Veterans, a nationally representative survey of veterans from multiple eras of service. Regression analyses assessed gender differences in the association between warfare exposure (deployment to a war zone, exposure to casualties) and health status and functional impairment, adjusting for sociodemographics.
FINDINGS
Women reported better health status but greater functional impairment than men. In men, those who experienced casualties only or both casualties and deployment to a war zone had worse health compared to those who experienced neither stressor or deployment to a war zone only. In women, those who experienced casualties only or both stressors reported worse health than those who experienced war zone only, who did not differ from the unexposed. No association was found between warfare exposure and functional impairment in women, but in men, those who experienced exposure to casualties or both stressors had greater odds of functional impairment compared to those who experienced war zone only or neither stressor.
CONCLUSIONS
Exposure to casualties may be more predictive of health than deployment to a war zone, especially for men. We did not find a stronger association between warfare exposure and health for women than men. Given that the expansion of women's military roles has allowed them to serve in direct combat, their degree and scope of warfare exposure is likely to increase in the future.
Keywords: veterans, gender, health, functional impairment, casualties, deployment
A wealth of evidence exists regarding the negative effects of military service on long-term health. Components of military service such as direct experience in combat and the more general stress of being deployed to a war zone can be conceptualized as examples of warfare exposure, which has been linked to worse health in veterans (Elder, Shanahan, & Clipp, 1997; Hoge et al., 2004; King, King, Gudanowski, & Vreven, 1995). Typically, research on the health consequences of warfare exposure among veterans has focused on mental health outcomes such as posttraumatic-stress disorder (PTSD), but other negative outcomes include higher rates of physician-diagnosed chronic conditions, worse self-reported health, and lower health functioning compared to civilians (Lehavot, Hoerster, Nelson, Jakupcak, & Simpson, 2012; Schnurr & Spiro, 1999; Schnurr, Spiro, & Paris, 2000). This study focuses on the association between warfare exposure and post-deployment self-rated health, and how this association might differ between men and women.
The negative health consequences of warfare have been demonstrated in samples of veterans across a range of service eras, from Vietnam veterans (Kulka et al., 1990), to the more recent cohorts deployed to the Persian Gulf (Proctor et al., 1998) or to Iraq and Afghanistan (Hoge et al., 2004). Generally, compared to veterans without PTSD, veterans with more PTSD symptoms or who were diagnosed with PTSD as a result of combat exposure exhibited worse physical health outcomes such as higher rates of coronary heart disease, more self-reported medical symptoms and conditions, and lower scores on the Medical Outcomes Study Short Form-36 (SF-36) and veteran's version (SF36-V) (Barrett et al., 2002; Beckham et al., 1998; Boscarino, 2004; Dobie et al., 2004; Kubzansky, Koenan, Spiro, Vokonas, & Sparrow, 2007). Veterans using VA health services report lower scores on the SF36-V compared to the general population, as well as more limitations in performing activities of daily living (ADLs) as a measure of functional status (Singh, 2005).
Assessment of warfare exposure has generally focused on traditional notions of combat, such as firing a weapon, being fired upon, and witnessing the death or injury of others (King et al., 1995). However, definitions of warfare that focus on prototypical combat roles may be less applicable in contemporary warfare, which is characterized by irregular and uncertain operations (Burrelli, 2012; Miller, Kavanagh, Lytell, Jennings, & Martin, 2012; Sternke, 2011; Street, Vogt, & Dutra, 2009). This also has implications for defining women's war zone experiences, as women have historically been excluded from units whose primary mission was direct combat. Because military occupations are classified into broad categories of combat arms, combat support, and combat service support, women have generally not served within combat arms. Yet female veterans who served in combat support capacities may still experience the substantive risks of warfare exposure when traveling alongside combat arms units, and when exposed to the aftermath of battle, such as dealing with casualties (Murdoch et al., 2006, Street et al., 2009). Including more general aspects of warfare exposure, such as deployment to a war zone or dealing with casualties, may help encapsulate a wider range of possible stressors.
Most studies examining the relation between warfare exposure and health have sampled male veterans (Frayne et al., 2006). While some studies have focused on the health consequences of deployment among female veterans of a specific cohort (Kang et al., 2014; Pierce, Lewandowski-Romps, & Silverschanz, 2011), few comprehensive studies have examined the range of deployment stressors faced by women from multiple eras of service (Bond, 2004; Sternke, 2011). More generally, given the different prevalence of PTSD in men and women in the general population, there may be gender differences in exposure to trauma (Olff, Langeland, Draijer, & Gersons, 2007; Tolin & Foa, 2006). Military sexual trauma (MST) is one deployment-related stressor more commonly experienced by women than men (Frayne et al., 2006). It is associated with worse post-deployment physical health, as well as mental health problems such as PTSD and depression (Sadler, Booth, Mengeling, & Doebbling, 2004; Smith et al., 2011, Street et al., 2009). One of the most powerful protective factors against developing PTSD is perceived social support, especially in military samples (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003). Female service members generally report lower levels of perceived social support from other military personnel, and also report fewer indicators of social support compared to their male peers (Frayne et al., 2006; Street et al., 2009).
Research on women veterans has been limited by the fact that much of the literature has focused on women using Veterans Health Administration (VHA) services. Although these studies demonstrate the need for care among women enrollees, samples drawn from health care users are not representative of the overall veteran population, as women who seek services have disproportionately higher rates of service-connected disabilities and worse physical and mental health. Therefore, non-treatment-seeking samples are more representative of the overall veteran population, especially in women veterans (Friedman et al., 2011; Ouimette, Wolfe, Daley, & Gima, 2003).
Some studies utilizing national samples, such as the 2010 Behavioral Risk Factor Surveillance Survey (BRFSS), indicate that veterans have worse health and greater health care needs compared to civilians. Veterans from all eras of service consistently demonstrate poorer physical and mental health and higher rates of risky health behaviors compared to their civilian counterparts. Veteran men are more likely than civilian men to report fair or poor health status, worse functional health, such as limited activities due to health problems, and more chronic conditions such as cardiovascular disease, cancer, arthritis, depression, and anxiety (Hoerster et al., 2012). Veteran women are also more likely to report worse health status compared to civilian women, as well as more limited functional health and increased mental distress (Levahot et al., 2012). These disparities between veterans and civilians highlight the importance of addressing the health and health care needs of veterans.
Warfare clearly has a deleterious effect on health, but whether and how this effect differs for male and female veterans remains unclear. The association is complicated by the broader demographic differences between men and women veterans. Women veterans of today are generally younger, have higher levels of education, and are more likely to be ethnic or racial minorities than male veterans (Frayne et al., 2006). Thus, when examining gender differences in the association between warfare exposure and health, it is important to account for these sociodemographic differences. In the present study, it was hypothesized that higher levels of warfare exposure would be associated with worse self-reported health, as defined by both health status and functional impairment, adjusting for sociodemographic characteristics. Regarding gender differences, it was hypothesized that a stronger association between warfare exposure and health would be observed in women than men, given women's greater risk for stressors such as MST, and lower access to resources such as social support.
Methods
Sample
The 2010 National Survey of Veterans (NSV) is the sixth in a series of surveys commissioned by the Department of Veterans Affairs (VA) to assess needs for veteran programs and services, as well as beneficiaries’ awareness of these services (Westat, 2010). The 2010 NSV was mandated by Congress as part of the Veterans Benefits Improvement Act (2004). Veterans were recruited using an address-based sampling approach, which matched U.S. Postal Service residential addresses with VA health care and beneficiary data and Department of Defense data on military retirees and those separated from active duty. This population included all non-institutionalized veteran residents of the 50 states and District of Columbia, and was recruited in 2009-2010. Veterans from all eras of service were sampled, from World War II to September 2001 or later. A prenotification letter was sent, followed by a screening survey to determine eligibility. Households with any veteran were eligible; they received an extended questionnaire with an option to fill out the survey online. A reminder postcard and follow-up survey were also sent. The total number of surveys distributed was 14,163, with 8,710 returned, for a response rate of 61.5%. After excluding 931 veterans with missing gender data, the present study included 500 female veterans and 7,279 male veterans. Because the purpose of the survey was to assess needs and access to VA services among the veteran population in general, a representative sample was drawn; specific groups such as women or ethnic/racial minorities were not over-sampled.
Measures
The key independent variable was a veteran's level of warfare exposure. This was assessed by two dichotomous items: 1) “Did you ever serve in a combat or war zone? [NOTE: Persons serving in a combat or war zone usually receive combat zone tax exclusion, imminent danger pay, or hostile fire pay.]” and, 2) “During your military service, were you ever exposed to dead, dying, or wounded people?” The two variables were multiplied to yield an overall warfare exposure term with four categories: neither war zone/casualties, war zone only, casualties only, and both war zone/casualties. Those who experienced neither war zone/casualties may have included veterans who served during peacetime, while those who experienced war zone only may have included veterans who did not serve directly on the front line, such as those deployed to the Persian Gulf as part of the Navy. Veterans who did not serve in a war zone but did experience exposure to casualties may have included medical personnel who served outside of a war zone but dealt with the wounded or dying. Finally, those who experienced both stressors were deployed to a war zone and also experienced casualties.
Sociodemographic covariates of interest included age, minority status, education, and income. Respondents were coded as minority if they endorsed being of Hispanic, Latino, or Spanish origin, or of a non-white race. Education was assessed by the highest degree or level of school completed by the participant (from less than high school to a doctoral degree; 9 levels), and total income was indicated by a categorical variable ranging from less than <$5,000 to over $150,000 (16 levels).
The first outcome was health status, which was ascertained by the item “In general, would you say your health is...”, with a 5-level response ranging from 1=Poor to 5=Excellent. This is the same measure of general health used in other national surveys, such as the BRFSS and National Health Interview Survey (NHIS). The second outcome, a measure of functional impairment, was created by summing the number of ADLs with which a veteran currently needed assistance, out of six activities (bathing, eating, transferring from a bed to a chair, using a toilet, walking around your home, dressing), which was also used in the NHIS to assess disability. Because of the low endorsement of help needed, this variable was dichotomized into 1=those who needed assistance with at least 1 ADL (8.5%), and 0=those who did not need any assistance.
Analyses
Given the substantial differences in sample size and distribution of variables between men and women (Table 1), all analyses were conducted separately by gender. The chi-squared statistic was used to assess gender differences on categorical variables (minority status, warfare exposure, functional impairment), and t tests were used for continuous variables (age, education, income, health status).
Table 1.
Study Variables by Gender
| Characteristic | Women | Men | χ2/ t (df) |
|---|---|---|---|
| N | 500 | 7279 | |
| Sociodemographic covariates | |||
| Age (M, SD) | 52.1 (17.1) | 65.7 (14.0) | t (7711) = 17.3*** |
| Minority (%) | 26.1 | 11.8 | χ2(1) = 84.7*** |
| Education (median level) | ≥1 year college | <1 year college | t (7702) = −7.54*** |
| Income (median bracket) | 40-50k | 40-50k | t (7270) = 1.0 |
| Warfare exposure (%) | χ2(3) = 59.0*** | ||
| Neither stressor | 61.4 | 52.7 | |
| War zone only | 8.9 | 10.5 | |
| Casualties only | 16.3 | 9.8 | |
| Both stressors | 13.4 | 27.1 | |
| Health status (%) | |||
| Mean (SD) | 3.1 (1.0) | 3.0 (1.1) | t (7656) = −2.5* |
| Poor (1) | 7.3 | 8.7 | |
| Fair (2) | 16.8 | 21.9 | |
| Good (3) | 37.7 | 36.2 | |
| Very good (4) | 31.4 | 25.8 | |
| Excellent (5) | 6.7 | 7.3 | |
| Functional impairment | |||
| Endorsed ≥ 1 ADL (%) | 10.9 | 8.0 | χ2(1) = 4.6* |
Note
p < .05
** p < .01
p < .001
Next, multiple linear regression analyses were conducted to assess the impact of warfare exposure on health status, adjusting for sociodemographic covariates (minority status, education, income, and age). Statistically significant effect of the warfare exposure variable was followed up with post-hoc analysis involving pairwise comparisons of health status between warfare exposure categories. Logistic regression analyses were conducted with the same predictor variables, with functional impairment as the outcome. All analyses were conducted with SAS (version 9.2, SAS Institute, Cary, NC).
Results
Male and female veterans differed across most study variables (Table 1). Women were younger (t (7711) = 17.3, p < .001), better-educated (t (7702)= −7.54, p < .001), and more likely to be of minority status (χ2(1) = 84.7, p < .001) compared to men. Median income did not differ significantly between men and women (t (7270) = 1.0, p = 0.32). Regarding warfare exposure, men and women endorsed significantly different categories of exposure (χ2(3) = 59.0, p < .001). The majority of veterans experienced neither deployment to a war zone nor exposure to casualties (61.4% in women, 52.7% in men). Men were more likely to experience both kinds of stressors (27.1%) compared to either war zone only (10.5%) or casualties only (9.8%). Women were more likely to be exposed to casualties only (16.3%), followed by both kinds of stressors (13.4%) and war zone only (8.9%). Women had slightly better health status compared to men, with a mean self-rated health of 3.1 vs 3.0 for men (where good=3 and very good=4), (t (7656) = -2.5, p < .05). However, women were more likely to endorse functional impairment, or needing ADL assistance (χ2(1) = 4.6, p < .05), with 10.9% of women needing assistance compared to 8.0% of men. The Pearson correlation between health status and functional impairment was 0.34 (p < .001) in men and 0.40 (p < .001) in women.
Although our findings are not directly comparable to civilian samples, given the differing demographic characteristics of veteran and civilian populations, similar questions on health status and functional impairment have been used in national surveys. In the National Health Interview Survey, 2012, 1.9% of those aged 45-64 and 3.3% of those aged 65-74 had an ADL limitation. Using an identical measure of health status that ranged from 1=poor to 5=excellent, in the NHIS those aged 45-64 had a mean self-rated health status of 3.6, compared to 3.4 in those aged 65-74 (Adams, 2013). In the 2010 BRFSS, 13.8% of civilian men and 17.5% of civilian women reported fair or poor health, compared to 30.6% and 24.1% in our sample respectively (Hoerster et al., 2012; Levahot et al., 2012).
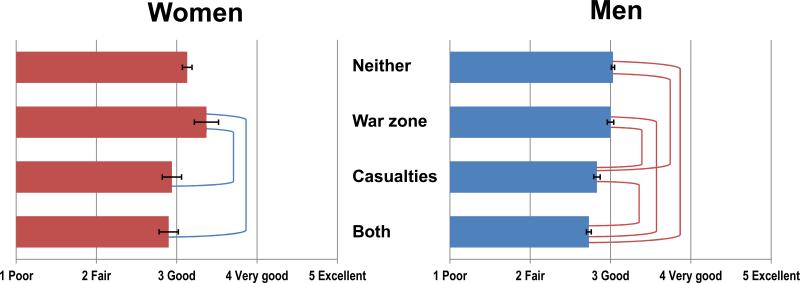
The linear regression analyses demonstrated that warfare exposure, as defined by the combination of deployment to a war zone and exposure to casualties, was associated with health status after adjusting for sociodemographic variables in both men and women (Table 2). In men, using neither stressor as the reference category, exposure to casualties only was negatively associated with health status (B = −0.20, SE = .04, p < .001), as was exposure to both stressors (B = −0.31, SE = 0.03, p < .001). Because the overall warfare exposure term was significant in both men (F(3,6384) = 41.79, p < .0001) and women (F(3,439) = 2.83, p = 0.04), we conducted post-hoc analyses involving pairwise comparisons on health status between exposure categories, adjusting for sociodemographic covariates. Among women, those who experienced exposure to casualties only, or exposure to both casualties and deployment to a war zone, had worse health status compared to those who served in a war zone only (Figure 1). Among men, when comparing adjusted health status among exposure categories, those who experienced both stressors had significantly worse health status compared to all other categories of warfare exposure, while those exposed to casualties only demonstrated worse health status compared to those who were deployed to a war zone only, and those who were exposed to neither stressor. Male veterans who were deployed to a war zone only, and those who experienced neither type of stressor, did not differ significantly in health status (Figure 1). While exposure to casualties or to both stressors influenced health status in men, these factors were not associated with health status in women when compared to the unexposed. For both genders, the effect of war zone-only exposure on health status was not significant.
Table 2.
Effects of Warfare Exposure on Health Status
| Women (n=447) | Men (n=6392) | |||
|---|---|---|---|---|
| B | SE | B | SE | |
| Intercept | 2.21*** | .21 | 2.43*** | .08 |
| Age | −0.01* | .00 | −0.01*** | .00 |
| Minority status | −0.29** | .10 | −0.26*** | .04 |
| Education | 0.06* | .03 | 0.09*** | .01 |
| Income | 0.07*** | .01 | 0.07*** | .00 |
| Warfare exposure | ||||
| Neither war zone/casualties (ref) | - | - | - | - |
| War zone only | 0.24 | 0.16 | −0.03 | .04 |
| Casualties only | −0.18 | 0.12 | −0.20*** | .04 |
| Both war zone/casualties | −0.22 | 0.13 | −0.31*** | .03 |
| F(7,439)=13.23*** | F(7,6384)=178.12*** | |||
| R2 = .17* | R2 = .16* | |||
Note
p < .05
p < .01
p < .001
Figure 1.
Health status by gender and warfare exposure (adjusted for sociodemographics). Brackets illustrate significant differences in health status (p<.05) between exposure categories.
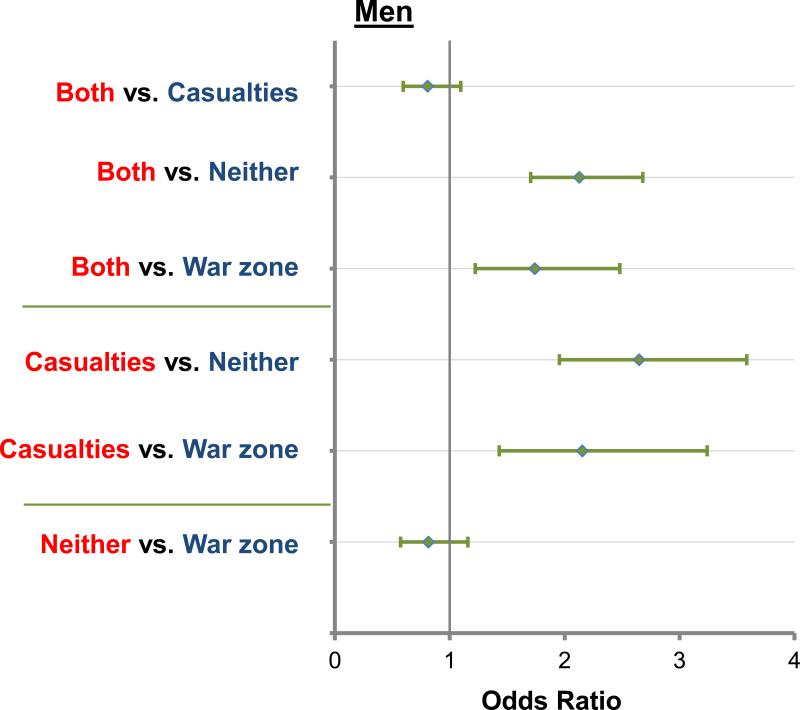
Logistic regression analyses were used to examine the association between warfare exposure and odds of functional impairment, defined by needing help with at least one ADL. In women, warfare exposure was not associated with increased odds of functional impairment; thus, we did not compare specific exposure categories on the outcome (Table 3). Among male veterans, there was a significant association between warfare exposure and increased odds of functional impairment. Compared to the unexposed, those exposed to casualties only had 2.65 times (95% CI: 1.95, 3.59) greater odds of functional impairment, while those who experienced both deployment to a war zone and exposure to casualties had 2.14 times (95% CI: 1.71, 2.68) greater odds of functional impairment, compared to the unexposed (Table 3). In post-hoc follow-up pairwise comparisons, several contrasts were significant: exposure to both stressors compared to neither, exposure to both stressors compared to war zone only, as well as casualties only compared to neither, and casualties only compared to war zone only (Figure 2). In men, these associations provide evidence of the importance of exposure to casualties on functional impairment, given the similarly negative impact of experiencing both types of stressors and exposure to casualties alone. Additionally, exposure to neither stressor and exposure to war zone only demonstrated similar associations with other exposure categories. This suggests that the main differences in impact on health were between the two higher-impact exposure groups (both stressors, casualties only) and the lower-impact/unexposed groups (neither stressors, war zone only).
Table 3.
Effects of Warfare Exposure on Functional Impairment
| Women (n=424) | Men (n=5920) | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age | 1.02 | (1.00, 1.04) | 1.02 | (1.01, 1.02) |
| Minority status | 0.97 | (0.42, 2.21) | 1.74 | (1.33, 2.29) |
| Education | 0.93 | (0.75, 1.14) | 0.93 | (0.88, 0.95) |
| Income | 0.87 | (0.80, 0.95) | 0.87 | (0.85, 0.89) |
| Warfare exposure | Wald χ2(3)=0.756, p=.860 | Wald χ2(3)=63.06, p<.0001 | ||
| Neither war zone/casualties (ref) | - | - | - | - |
| War zone only | 1.67 | (0.37, 3.44) | 1.23 | (0.86, 1.75) |
| Casualties only | 1.21 | (0.48, 3.09) | 2.65 | (1.95, 3.59) |
| Both war zone/casualties | 1.13 | (0.50, 5.60) | 2.14 | (1.71, 2.68) |
Figure 2.
Functional impairment by warfare exposure in men (adjusted for sociodemographics). Odds ratios illustrate associations between exposure categories.
Discussion
Overall, we found that warfare exposure was associated with worse health status in both men and women, and greater functional impairment in men. Findings suggest the relative importance of exposure to casualties compared to deployment to a war zone when predicting self-reported health status and functional impairment, especially for men. Deployment to a war zone only did not have a significant impact on health. Contrary to our hypothesis, we did not find stronger associations between warfare exposure and health in women.
In another study based on the National Survey of Veterans 2010, Edwards (2012) examined the impact of OEF/OIF deployment on veterans’ socioeconomic outcomes. After restricting his analyses to those who endorsed being deployed post-9/11, he found that there was a greater detrimental effect of exposure to casualties compared to deployment to a war zone. This provides converging evidence that exposure to casualties has a stronger impact on multiple indices of overall functioning (health status, functional impairment, socioeconomic status) than deployment to war zone. Perhaps exposure to dead, dying, or wounded bodies was a more reliable marker of consistently traumatic or stressful military experiences, compared to being deployed to a war zone only.
Results demonstrating the importance of exposure to casualties were especially salient among male veterans. In both linear and logistic regression analyses, two distinct groups emerged from our four exposure categories: A higher-impact group consisting of those who experienced both types of stressors or casualties only, and a lower-impact group consisting of those who experienced neither type of stressor and war zone only. These findings suggest that in male veterans, the negative impact of warfare exposure on health status and functional impairment is strongest when exposure includes casualties, whether defined as exposure to casualties only or both exposure to casualties and deployment to a war zone. Considering functional impairment, only men who experienced these higher-impact stressors had significantly greater odds of impairment. Similarly, only men in the higher-impact group had significantly worse health status. Especially for health status, there appears to be an additive effect of experiencing both exposure to casualties and deployment to a warzone when predicting health status. Men who experienced both stressors reported worse health compared to those who experienced one type of exposure only.
In women, the results are less conclusive. As in men, women who experienced higher-impact stressors reported worse health status compared to women who experienced war zone only. Women who experienced war zone only did not differ from their counterparts who experienced neither type of stressor with regard to their health status. No association with warfare exposure was found using functional impairment. Overall, for both outcomes, the magnitude of the regression coefficients and odds ratios suggests that the effect of warfare exposure is smaller in women than in men. The smaller sample of women than men also limited our ability to detect small effects in this group.
Despite the less conclusive results with female veterans, it is noteworthy that women endorsed a significantly higher prevalence of functional impairment compared to men, despite their younger age and slightly better health status. Thus, when considering health across the lifespan for male and female veterans, the impact of functional health may be an especially important issue for aging women. Bean-Mayberry et al. (2011) have suggested that in examining post-deployment health of female veterans, it is important to focus on non-mental health care needs, such as chronic conditions, which may have the greatest impact on functional impairment. In addition, the measure of functional impairment used in this study indicated a more severe level of impairment, in needing assistance with at least one ADL. Other measures of health functioning that included role limitations in a broader range of activities might have provided more insight into functional health, especially in women.
Limitations of this study include the cross-sectional nature of the data, as well as the use of self-report measures. The nature of the data precluded us from adjusting for pre-deployment baseline health and more directly examining health changes related to deployment. Additionally, given the large overall sample size, relatively few women were sampled in comparison to men, which may have hindered our ability to detect associations. Our sample size for women was also too small to stratify by era of service, but we did adjust for age in analyses, which helped address concerns about specific effects of era. More detailed outcome variables could have provided a more substantial assessment of health status and functioning.
Strengths of this study include the large representative sample drawn from a range of service eras. In addition, the sample was not restricted to those enrolled in VHA services, but was instead a more representative sample of the veteran population, which is especially important in research on women veterans. Another strength of this study includes its focus on general health, as considerable research on the impact of military experiences focuses on mental health outcomes of deployment.
Our findings of the small effects of warfare exposure on women's health, and the higher level of functional impairment in women than men, suggest that we may not be accounting for the full range of stressors experienced by women during deployment. As discussed by Sternke (2011), most instruments measuring combat experience were developed and validated with previous generation of male veterans, and may not fully capture female veterans’ experiences. Since a wide range of factors influence women's health in the years following deployment, a complete assessment of all warfare-related exposure variables is critical in understanding and addressing the health consequences of warfare exposure. It is recommended that future studies adopt a more thorough assessment of warfare exposure that is tailored to the multiple aspects (e.g., combat experience, degree of exposure to casualties, work and living conditions, duration and number of deployments) of the deployment experience, as well as additional stressors such as MST, levels of deployment social support, or exposure to prior trauma, which may not be directly related to warfare, but have been associated with post-deployment health and functioning (Dutra et al., 2010; Reger, Gahm, Swanson, & Duma, 2009; Vogt, Proctor, King, King, & Vasterling, 2008).
Implications for Practice and Policy
In considering the implications of this research on veterans’ health, another development to keep in mind is that the level of warfare exposure faced by women will likely increase in the future. The recent Pentagon decision allowing women to serve officially in units whose primary mission is direct combat will expand the range of stressors that define women's war zone experiences (Bumiller & Shanker, 2013; Burrelli, 2012). Our sample, which was drawn from veterans of all cohorts, reflects demographic changes in the composition of the military. Not only are younger veterans more likely to be women than older veterans, but younger men and women face more comparable levels of warfare exposure. Among veterans older than 40, only 5% are women, while among those younger than 40, 22% are women. Comparably, among veterans older than 40, 34% of women and 46% of men experienced warfare exposure, while in veterans younger than 40, 53% of women experienced warfare exposure compared to 65% of men.
Recent studies focusing on mental health outcomes in veterans deployed to Iraq and Afghanistan have provided evidence that women are not necessarily more vulnerable than men to the effects of warfare exposure (Macera, Aralis, Highfill-McRoy, & Rauh 2014; Street, Gradus, Giasson, Vogt, & Resick 2013). For instance, Vogt et al. (2011) found women exhibited modestly lower levels of combat-related stressors compared to men, but comparable levels of perceived threat, perhaps due to their higher prevalence of prior life stressors and increased risk of deployment-related stressors such as sexual harassment. Moreover, there were no significant interactions between gender and combat-related stressors for most mental health outcomes, indicating that women may have comparable levels of risk – and resilience. High levels of combat exposure may actually serve as a risk equalizer for men and women, especially when the reference trauma is very intense with a persistent level of threat (Hoge, Clark, & Castro, 2007). Although the current study examined general health and not mental health as an outcome, and included women from all eras of service, we found a similar lack of evidence for stronger associations between warfare exposure and health.
As policy changes regarding women's ability to officially serve in combat roles are implemented in the coming years, furthering the demographic shift already seen in younger veterans in our sample, it is likely that the number of women experiencing similarly high levels of warfare exposure as men will only increase. Findings regarding female and male veterans’ post-deployment health, in which women demonstrate comparable levels of risk and resilience as men, indicate that these policies actually align with current research. Although future studies should compare the deployment experience for men and women in greater detail, with careful attention to long-term health effects, the evidence thus far bodes well for reducing restrictions on women's roles in the military.
Acknowledgments
This research was supported by a VA Clinical Science Research and Development Service Senior Research Career Scientist Award and National Institutes of Health grant R24-AG039343. The views expressed in this paper are those of the authors and do not necessarily represent the views of the US Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Joyce M. Wang, Massachusetts Veterans Epidemiology Research and Information Center, VA Boston Healthcare System and the Department of Epidemiology, Boston University School of Public Health.
Lewina O. Lee, National Center for PTSD, VA Boston Healthcare System, the Department of Epidemiology, Boston University School of Public Health, and the Department of Psychiatry, Boston University School of Medicine.
Avron Spiro, III, Massachusetts Veterans Epidemiology Research and Information Center, VA Boston Healthcare System, and with the Department of Epidemiology, Boston University School of Public Health, the Department of Psychiatry, Boston University School of Medicine, and the Department of Health Policy and Health Services Research, Boston University Goldman School of Dental Medicine..
References
- Adams PF, Kirzinger WK, Martinez ME. Summary health statistics for the U.S. population: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Statistics Series. 2013;10(259) [PubMed] [Google Scholar]
- Barrett DH, Doebbeling CC, Schwartz DA, Voelker MD, Falter KH, Woolson RF, Doebbeling BN. Posttraumatic stress disorder and self-reported physical health status among U.S. military personnel serving during the Gulf War period: A population-based study. Psychosomatics. 2002;43(3):195–205. doi: 10.1176/appi.psy.43.3.195. doi:10.1176/appi.psy.43.3.195. [DOI] [PubMed] [Google Scholar]
- Bean-Mayberry B, Yano EM, Washington DL, Goldzweig C, Batuman F, Huang C, Shekelle PG. Systematic review of women veterans’ health: Update on successes and gaps. Women's Health Issues. 2011;21(4):S84–S97. doi: 10.1016/j.whi.2011.04.022. doi:10.1016/j.whi.2011.04.022. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Moore SD, Feldman ME, Hertzberg MA, Kirby AC, Fairbank JA. Health status, somatization, and severity of posttraumatic stress disorder in Vietnam combat veterans with posttraumatic stress disorder. American Journal of Psychiatry. 1998;155(11):1565–1569. doi: 10.1176/ajp.155.11.1565. [DOI] [PubMed] [Google Scholar]
- Bond EF. Women's physical and mental health sequellae of wartime service. Nursing Clinics of North America. 2004;39(1):53–68. doi: 10.1016/j.cnur.2003.11.004. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Posttraumatic stress disorder and physical illness: Results from clinical and epidemiologic studies. Annals of the New York Academy of Sciences. 2004;1032(1):141–153. doi: 10.1196/annals.1314.011. doi:10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000;68(5):748–766. doi: 10.1037//0022-006x.68.5.748. doi:10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Bumiller E, Shanker T. Pentagon set to lift ban on women in combat roles. The New York Times. 2013 Jan 23; Retrieved from http://www.nytimes.com/2013/01/24/us/pentagon-says-itis-lifting-ban-on-women-in-combat.html.
- Burrelli DF. Women in combat: Issues for Congress. 2012 Apr 5; Retrieved from http://digital.library.unt.edu/ark:/67531/metadc83997/
- Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: Association with self-reported health problems and functional impairment. Archives of Internal Medicine. 2004;164(4):394–400. doi: 10.1001/archinte.164.4.394. doi:10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- Dutra L, Grubbs K, Greene C, Trego LL, McCartin TL, Kloezeman K, Morland L. Women at war: Implications for mental health. Journal of Trauma & Dissociation. 2010;12(1):25–37. doi: 10.1080/15299732.2010.496141. [DOI] [PubMed] [Google Scholar]
- Edwards RD. Overseas deployment, combat exposure, and well-being in the 2010 National Survey of Veterans. 2012 Retrieved from http://www.nber.org/papers/w18227.
- Elder GH, Jr., Shanahan MJ, Clipp CE. Linking combat and physical health: The legacy of World War II in men's lives. American Journal of Psychiatry. 1997;154(3):330–336. doi: 10.1176/ajp.154.3.330. [DOI] [PubMed] [Google Scholar]
- Frayne SM, Parker VA, Christiansen CL, Loveland S, Seaver MR, Kazis LE, Skinner KM. Health status among 28,000 women veterans: The VA women's health program evaluation project. Journal of General Internal Medicine. 2006;21(S3):S40–S46. doi: 10.1111/j.1525-1497.2006.00373.x. doi:10.1111/j.1525-1497.2006.00373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SA, Phibbs CS, Schmitt SK, Hayes PM, Herrera L, Frayne SM. New women veterans in the VHA: A longitudinal profile. Women's Health Issues. 2011;21(4):S103–S111. doi: 10.1016/j.whi.2011.04.025. doi:10.1016/j.whi.2011.04.025. [DOI] [PubMed] [Google Scholar]
- Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: U.S. military, veteran, and civilian men. American Journal of Preventive Medicine. 2012;43(5):483–489. doi: 10.1016/j.amepre.2012.07.029. doi:10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Clark JC, Castro CA. Commentary: Women in combat and the risk of post-traumatic stress disorder and depression. International Journal of Epidemiology. 2007;36(2):327–329. doi: 10.1093/ije/dym013. doi:10.1093/ije/dym013. [DOI] [PubMed] [Google Scholar]
- Kang HK, Cypel Y, Kilbourne AM, Magruder KM, Serpi T, Collins JF, Spiro A. HealthViEWS: Mortality Study of Female US Vietnam Era Veterans, 1965–2010. American Journal of Epidemiology. 2014:kwt319. doi: 10.1093/aje/kwt319. [DOI] [PubMed] [Google Scholar]
- King DW, King LA, Gudanowski DM, Vreven DL. Alternative representations of war zone stressors: Relationships to posttraumatic stress disorder in male and female Vietnam veterans. Journal of Abnormal Psychology. 1995;104(1):184. doi: 10.1037//0021-843x.104.1.184. [DOI] [PubMed] [Google Scholar]
- Kubzansky LD, Koenen KC, Spiro A, III, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Archives of General Psychiatry. 2007;64(1):109–116. doi: 10.1001/archpsyc.64.1.109. doi:10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam war generation: Report of findings from the National Vietnam Veterans Readjustment Study. Brunner/Mazel; Philadelphia, PA: 1990. [Google Scholar]
- Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. American Journal of Preventive Medicine. 2012;42(5):473–480. doi: 10.1016/j.amepre.2012.01.006. doi:10.1016/j.amepre.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Macera CA, Aralis HJ, Highfill-McRoy R, Rauh MJ. Posttraumatic stress disorder after combat zone deployment in Navy and Marine Corps men and women. Journal of Women's Health. 2014;23(6):499–505. doi: 10.1089/jwh.2013.4302. [DOI] [PubMed] [Google Scholar]
- Miller LL, Kavanagh J, Lytell MC, Jennings K, Martin C. The extent of restrictions on the service of active-component military women. 2012 Retrieved from http://www.rand.org/pubs/monographs/MG1175.html.
- Murdoch M, Bradley A, Mather SH, Klein RE, Turner CL, Yano EM. Women and war: What physicians should know. Journal of General Internal Medicine. 2006;21(S3):S5–S10. doi: 10.1111/j.1525-1497.2006.00368.x. doi:10.1111/j.1525-1497.2006.00368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychological Bulletin. 2007;133(2):183–204. doi: 10.1037/0033-2909.133.2.183. doi:10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Ouimette P, Wolfe J, Daley J, Gima K. Use of VA health care services by women veterans: Findings from a national sample. Women & Health. 2003;38(2):77–91. doi: 10.1300/J013v38n02_06. doi:10.1300/J013v38n02_06. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129(1):52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Pierce PF, Lewandowski-Romps L, Silverschanz P. War-related stressors as predictors of post-deployment health of Air Force women. Women's Health Issues. 2011;21(4):S152–S159. doi: 10.1016/j.whi.2011.04.017. [DOI] [PubMed] [Google Scholar]
- Proctor SP, Heeren T, White RF, Wolfe J, Borgos MS, Davis JD, Vasterling JJ. Health status of Persian Gulf War veterans: Self-reported symptoms, environmental exposures and the effect of stress. International Journal of Epidemiology. 1998;27(6):1000–1010. doi: 10.1093/ije/27.6.1000. [DOI] [PubMed] [Google Scholar]
- Reger MA, Gahm GA, Swanson RD, Duma SJ. Association between number of deployments to Iraq and mental health screening outcomes in US Army soldiers. The Journal of Clinical Psychiatry. 2009;70(9):1266–1272. doi: 10.4088/JCP.08m04361. [DOI] [PubMed] [Google Scholar]
- Sadler AG, Booth BM, Mengeling MA, Doebbeling BN. Life span and repeated violence against women during military service: Effects on health status and outpatient utilization. Journal of Women's Health. 2004;13(7):799–811. doi: 10.1089/jwh.2004.13.799. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Spiro A., III Combat exposure, posttraumatic stress disorder symptoms, and health behaviors as predictors of self-reported physical health in older veterans. The Journal of Nervous and Mental Disease. 1999;187(6):353–359. doi: 10.1097/00005053-199906000-00004. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Spiro A, III, Paris AH. Physician-diagnosed medical disorders in relation to PTSD symptoms in older male military veterans. Health Psychology. 2000;19(1):91–97. doi: 10.1037//0278-6133.19.1.91. doi:10.1037//0278-6133.19.1.91. [DOI] [PubMed] [Google Scholar]
- Singh JA, Borowsky SJ, Nugent S, Murdoch M, Zhao Y, Nelson DB, Nichol KL. Health-Related quality of life, functional impairment, and healthcare utilization by veterans: Veterans' quality of life study. Journal of the American Geriatrics Society. 2005;53(1):108–113. doi: 10.1111/j.1532-5415.2005.53020.x. [DOI] [PubMed] [Google Scholar]
- Smith BN, Shipherd JC, Schuster JL, Vogt DS, King LA, King DW. Posttraumatic stress symptomatology as a mediator of the association between military sexual trauma and post-deployment physical health in women. Journal of Trauma & Dissociation. 2011;12(3):275–289. doi: 10.1080/15299732.2011.551508. doi:10.1080/15299732.2011.551508. [DOI] [PubMed] [Google Scholar]
- Sternke LM. Measurement of military combat exposure among women: Analysis and implications. Women's Health Issues. 2011;21(4):S160–S168. doi: 10.1016/j.whi.2011.04.020. doi:10.1016/j.whi.2011.04.020. [DOI] [PubMed] [Google Scholar]
- Street AE, Gradus JL, Giasson HL, Vogt D, Resick PA. Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. Journal of General Internal Medicine. 2013;28(Suppl 2):S556–S562. doi: 10.1007/s11606-013-2333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street AE, Vogt D, Dutra L. A new generation of women veterans: Stressors faced by women deployed to Iraq and Afghanistan. Clinical Psychology Review. 2009;29(8):685–694. doi: 10.1016/j.cpr.2009.08.007. doi:10.1016/j.cpr.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. doi:10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Veterans Benefits Improvement Act of 2004, Pub. L. No. 108-454.
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15(4):391–403. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]
- Vogt D, Vaughn R, Glickman ME, Schultz M, Drainoni ML, Elwy R, Eisen S. Gender differences in combat-related stressors and their association with postdeployment mental health in a nationally representative sample of U.S. OEF/OIF veterans. Journal of Abnormal Psychology. 2011;120(4):797–806. doi: 10.1037/a0023452. doi:10.1037/a0023452. [DOI] [PubMed] [Google Scholar]
- Westat National survey of veterans, active duty service members, demobilized national guard and reserve members, family members, and surviving spouses. 2010 Oct 18; Retrieved from http://www.va.gov/SURVIVORS/docs/NVSSurveyFinalWeightedReport.pdf.