Abstract
Background
Gender differences in dyslipidemia are widely documented, but the contributors to these differences are not well understood. This study examines whether differences in quality of care, intensity of lipid- lowering medication regimen and medication adherence can explain this disparity.
Methods
Secondary analysis of medical records data and questionnaires collected from adult patients with type 2 diabetes (n=1,369) from seven outpatient clinics affiliated with an academic medical center as part of the Reducing Racial Disparities in Diabetes: Coached Care (R2D2C2) study. Primary outcome was LDL cholesterol.
Findings
Women had higher LDL cholesterol levels than men (mean[SD]: 101.2[35.2] mg/dl vs. 92.3[33.0] mg/dl, p<0.001), but were no less likely to receive recommended processes of diabetes care, to attain targets for glycemic control and blood pressure, or to be on intensive medication regimens. More women than men reported medication nonadherence due to cost (32.7% vs. 24.2%, p=0.040) and due to side effects (47.2% vs. 36.8%, p=0.024). For all patients, regimen intensity (p<0.05) and nonadherence due to side effects (p<0.01) were each associated with higher LDL cholesterol levels. The addition of a new lipid lowering agent was associated with subsequent nonadherence related to side effects for women (p<0.001), but not for men (p=0.45, test for interaction p=0.048).
Conclusions
Despite comparable quality of diabetes care and regimen intensity for lipid management, women with diabetes experienced poorer lipid control than men. Medication nonadherence appeared to be a major contributor to dyslipidemia, particularly for women, because of side effects associated with intensifying the lipid lowering regimen.
Introduction & Background
Heart disease is the most common cause of death for both men and women with diabetes (Gregg, Gu, Cheng, Venkat Narayan, & Cowie, 2007; Moss, Klein, & Klein, 1991). However, reductions in rates of all-cause and cardiovascular-related mortality observed for men with diabetes since the 1970's have not been observed for women (Dale, Vatten, Nilsen, Midthjell, & Wiseth, 2008; Gregg et al., 2007).
Studies have explored a number of plausible contributors to the apparent gender disparities in cardiovascular disease (CVD) among patients with diabetes (Vaccarino, 2010; Vimalananda, Miller, Palnati, Christiansen, & Fincke, 2011; Wenger, 2007; Xhyheri & Bugiardini, 2010). Such factors have included gender differences in cardiac physiology (Avogaro et al., 2007; Gouni-Berthold, Berthold, Mantzoros, Böhm, & Krone, 2008; Steinberg et al., 2000), presence of multiple chronic conditions (Avogaro et al., 2007), behavioral factors (such as medication nonadherence; Lewey et al., 2013), styles of patient-provider communication (Elderkin-Thompson & Waitzkin, 1999; Hall & Roter, 1995), risk perceptions (Homko et al., 2010; Mosca et al., 2000) and socioeconomic barriers (such as poorer access to care; Brooks et al., 2010; Glied, Jack, & Rachlin, 2008; Ostadal & Ostadal, 2013; Patchias, Waxman, & Fund, 2007; Rustgi, Doty, Collins, & Fund, 2009). Some have hypothesized that women with diabetes may receive poorer quality of care compared to men, suggesting a gender bias among providers (Fisher, Brenner, Cheren, & Stange, 2013; Hvelplund et al., 2010; Tobin et al., 1987; Xhyheri & Bugiardini, 2010).
Gender disparities in lipid management may be a particularly important contributor to suboptimal CVD outcomes in women with diabetes (Gouni-Berthold et al., 2008). Women with diabetes have been shown to have less well-controlled LDL cholesterol levels than men and to be less likely to have received lipid-lowering medications (Gouni-Berthold et al., 2008; Wexler, Grant, Meigs, Nathan, & Cagliero, 2005) even though their risk of developing coronary artery disease is similar to that of men with diabetes (Kalyani et al., 2013).
Evidence for the relative contribution of a number of these factors to gender disparities in cardiovascular outcomes remains controversial (Vaccarino, 2010; Vimalananda et al., 2013; Xhyheri & Bugiardini, 2010). Although the presence of gender differences in adherence to statin therapy is well-supported by a meta-analysis of 53 studies (Lewey et al., 2013), prior studies on gender disparities in dyslipidemia did not explicitly assess the degree to which gender differences in lipid levels can be explained by differences in adherence to intensive lipid-lowering medication regimens (Gouni-Berthold et al., 2008; Wexler et al., 2005). To examine the contribution of quality of care, intensity of the lipid-lowering medication regimen and medication adherence to gender disparities in lipid management we report here analyses of data from the Reducing Racial Disparities in Diabetes with Coached Care study (R2D2C2, ClinicalTrials.gov identifier: NCT01123239; Kaplan, Billimek, Sorkin, Ngo-Metzger, & Greenfield, 2013). The R2D2C2 study employs data from multiple data sources in an ethnically and socioeconomically diverse sample to identify key contributors to disparities in diabetes care.
The present study has three objectives. First, we examine differences between men and women in lipid control, the overall quality of diabetes care they receive, the intensity of medication regimen they are prescribed, and adherence to their medication regimens. Second, we evaluate whether women are more or less likely than men to report medication nonadherence (both nonadherence related to cost and nonadherence related to side effects) following intensification of the lipid lowering regimen. Third, we present a model examining the degree to which gender differences in each of three areas: (1) quality of diabetes care, (2) regimen intensity and (3) medication nonadherence contribute to gender disparities in dyslipidemia.
Methods
Study population
The R2D2C2 study has been described in detail elsewhere (Kaplan et al., 2013). Under the oversight of the University of California, Irvine Institutional Review Board, the study included a cross-sectional observational study component that enrolled a sample of patients from seven outpatient clinics affiliated with an academic medical center. The patient sample was drawn from a diabetes registry representing all adult patients with a diagnosis code for type 2 diabetes who had at least one encounter with a family medicine, internal medicine, or endocrinology provider within a 12 month period and who spoke Spanish, English or Vietnamese. The analytic sample for this study (N=1,369) included 555 men and 814 women with type 2 diabetes, and was similar in demographics and disease-related characteristics to the registry population (Kaplan et al., 2013). Data were collected from May 2006 through June 2011.
Measures
Upon providing informed consent to the study, all study participants completed a baseline questionnaire. Medical records were abstracted for the 12-month period leading up to the date the questionnaire was completed. Participant characteristics, including age, sex, race/ethnicity, insurance type, history of heart disease and body mass index (BMI) were collected from the medical record. Comorbidity was assessed from the patient questionnaire using a 38-item version of the Total Illness Burden Index (TIBI; Malik et al., 2013), which summarizes the presence and severity of the patient's conditions and symptoms comorbid to diabetes and heart disease. Years of education was also collected from patient report. Laboratory values and blood pressure were abstracted from medical records.
Quality of Diabetes Care
Performance of five recommended processes of care (annual assessments for hemoglobin A1c, lipids, and microalbuminuria; annual foot exam and annual dilated eye exam) was assessed from the medical record for the 12 month period preceding the date the patient completed the baseline questionnaire. Attainment of recommended targets defined according to American Heart Association and American Diabetes Association guidelines was also assessed for LDL cholesterol (less than 100 mg/dl), HDL cholesterol (greater than 50 mg/dL for men and greater than 60 mg/dl for women), systolic blood pressure target (less than 140 mmHg) and A1c (less than 8%) using the most recent value prior to the baseline questionnaire date.
Regimen intensity
Regimen intensity for hyperlipidemia, hypertension and hyperglycemia treatment was assessed by determining the number of medication classes prescribed for each cardiovascular risk factor at baseline. Five medication classes were included for hyperlipidemia (statins, bile acid resins, fibrates, niacin and ezetimibe), eight for hypertension (ACE inhibitors, alpha blockers, angiotensin antagonists, beta adrenergic blockers, calcium channel blockers, thiazides/related diuretics, potassium-sparing diuretics, and loop diuretics); and eight for hyperglycemia (biguanides, sulfonylureas, thiazolidinediones, DPP-4 inhibitors, alpha-glucosidase inhibitors, meglitinides, GLP-1 agonists, and insulin). To examine the impact of regimen intensification on subsequent medication adherence, we also identified patients who had a new class of lipid medications added in the 12 month period leading up to the baseline questionnaire date (collected between 2006 and 2011).
Medication nonadherence
Medication nonadherence was measured from the baseline questionnaire using seven items (Safran et al., 2005) that assess both the extent and reasons for nonadherence. Cost-related nonadherence was measured as a composite of three items asking how frequently respondents deviated from their physicians' instructions due to the monetary costs of the regimen. Nonadherence related to side effects was measured as a composite of four items asking how frequently respondents deviated from their physicians' instructions due to side effects or other negative experiences with the medication. Each of these composite scales was scored as dichotomous variables, with patients reporting nonadherence on at least one item coded as “reporting nonadherence” (1), and those reporting no deviations from their prescribed regimen “not reporting nonadherence” (0; Billimek & August, 2013).
Data Analysis
We compared men and women's baseline demographic and disease-related characteristics using independent samples t-tests (for continuous variables) and chi-square tests (for categorical variables). We then used ordinary least squares regression to assess gender differences in lipid levels after adjustment for age, education, race/ethnicity, insurance status, history of coronary heart disease and comorbidities. The proportions of women versus men attaining recommended process and outcome targets for quality diabetes care, taking an intensive medication regimen for glycemic, lipid and blood pressure control, and reporting medication nonadherence were compared using logistic regression models adjusted for the same set of covariates. The association between treatment intensification (the addition of a new lipid medication) and subsequent medication nonadherence was assessed using logistic regression models adjusting for age, education, race/ethnicity, and compared between men and women by testing for a gender by treatment intensification interaction in the model. Finally, the degree to which lipid regimen intensity (number of lipid medications currently prescribed) and medication nonadherence were each associated with LDL cholesterol levels was assessed using a linear regression model, also including the covariates noted above. All analyses were performed using SPSS Statistics version 21.0 (SPSS, Chicago, Illinois, USA).
Results
Compared to men, women in the sample had fewer years of education, more women were of Hispanic race/ethnicity, fewer women had commercial insurance, and women had greater comorbidity as measured by the TIBI (Table 1).
Table 1. Characteristics of the study sample (N=1369)*.
| Participant Characteristics† | Men N=555 | Women N=814 | p |
|---|---|---|---|
| Age, years | 59.6 [11.4] | 58.6 [11.4] | 0.11 |
| Education, years | 11.4 [4.8] | 8.4 [4.9] | <0.001 |
| Duration of diabetes, years | 9.6 [7.9] | 9.3 [6.9] | 0.40 |
| Race/ethnicity | <0.001 | ||
| White, % | 37.7 | 20.0 | |
| Hispanic, % | 44.5 | 62.3 | |
| Vietnamese, % | 17.8 | 17.7 | |
| Health insurance type | <0.001 | ||
| Uninsured, % | 17.7 | 23.5 | |
| Commercial, % | 21.1 | 11.8 | |
| Medicare, % | 33.2 | 28.4 | |
| Medicaid, % | 21.1 | 26.8 | |
| Medicare and Medicaid, % | 7.0 | 9.6 | |
| Comorbidity (Total Illness Burden Index) | 3.2 [2.3] | 3.9 [2.4] | <0.001 |
| Heart disease noted in the medical record, % | 24.1 | 11.4 | <0.001 |
| Body mass index, kg/m2 | 30.7 [16.1] | 30.7 [9.5] | 0.98 |
Values presented as means with standard deviations in parentheses for continuous variables and as percentages for categorical variables. P-values for group comparisons were computed using independent samples t-tests for continuous variables and chi-squared tests for categorical variables.
Age, education, race/ethnicity, duration of diabetes and comorbidity derive from patient questionnaire. All other data derive from medical record abstraction.
Women had higher LDL cholesterol (unadjusted mean [SD]: 101.8 [35.7] mg/dl vs. 92.5 [33.4] mg/dl, adjusted mean difference [95%CI]: 7.4 [3.4, 11.3], p<0.001), higher HDL cholesterol (unadjusted mean [SD]: 47.9 [13.4] mg/dl vs. 41.1 [12.4] mg/dl, adjusted mean difference [95%CI]: 7.6 [6.1, 9.1], p<0.001), and higher total cholesterol (unadjusted mean [SD]: 177.7 [47.1] mg/dl vs. 159.6 [46.8] mg/dl, adjusted mean difference [95%CI]: 15.1 [9.6, 20.5], p<0.001) compared to men (see Table 2). Women also had higher non-HDL cholesterol compared to men (unadjusted mean [SD]: 129.8 [47.0] mg/dl vs. 118.4 [46.1] mg/dl, adjusted mean difference [95%CI]: 7.5 [2.1, 12.9], p=0.006).
Table 2. Lipid profile, by gender (mean [SD])*.
| Men N=555 | Women N=814 | Adjusted mean difference† (95% CI) | p | |
|---|---|---|---|---|
| LDL cholesterol (mg/dl) | 92.5 [33.4] | 101.8 [35.7] | 7.4 (3.4, 11.3) | <0.001 |
| HDL cholesterol (mg/dl) | 41.1 [12.4] | 47.9 [13.4] | 7.6 (6.1, 9.1) | <0.001 |
| Total cholesterol (mg/dl) | 159.6 [46.8] | 177.7 [47.1] | 15.1 (9.6, 20.5) | <0.001 |
| Non-HDL cholesterol (mg/dl) | 118.4 [46.1] | 129.8 [47.0] | 7.5 (2.1, 12.9) | 0.006 |
Values presented as mean [standard deviation] of each laboratory values for patients within each gender, from medical record abstraction.
Adjusted mean difference and p-values were computed using ordinary least squares regression models adjusted for age, education, race/ethnicity, health insurance type and comorbidity.
Overall, quality of diabetes care was comparable for women and men (Table 3), with similar proportions of each gender receiving an A1c test, lipid panel, urinalysis for microalbumin, foot exam and eye exam in the twelve months prior to baseline. In adjusted analyses, women were more likely than men to attain the target for glycemic control of A1c<8% (aOR [95% CI] 1.48 [1.12, 1.95], p=0.005), and as likely as men to attain the target of systolic blood pressure below 140 mmHg. In spite of receiving comparable processes of diabetes care, however, women were less likely than men to have LDL and HDL levels at target. Only 55.0% of women, compared to 69.7% of men had LDL cholesterol levels below 100 mg/dl (aOR [95% CI]: 0.62 [0.48, 0.79], p<0.001). Fewer women than men had HDL cholesterol at recommended levels, with 40.4% of women having HDL cholesterol greater than 50 mg/dl as recommended for women compared to 47.9% of men with HDL cholesterol above the target of 40 mg/dl for men (aOR [95% CI]: 0.77 [0.60, 0.98], p=0.03).
Table 3. Characteristics of diabetes care received and reports of medication nonadherence, by gender*.
| Men | Women | Odds Ratio (95% CI)† | ||||
|---|---|---|---|---|---|---|
| N=555 | N=814 | Unadjusted | p | Adjusted | p | |
| Quality of Care: Processes‡ | ||||||
| Annual A1c test | 97.8 | 96.8 | 0.65 (0.32, 1.31) | 0.23 | 0.69 (0.33, 1.45) | 0.33 |
| Annual lipid panel | 96.0 | 95.9 | 0.73 (0.52, 1.58) | 0.91 | 1.08 (0.60, 1.95) | 0.81 |
| Annual urinalysis for microalbumin | 77.8 | 76.7 | 0.95 (0.73, 1.24) | 0.69 | 0.95 (0.71, 1.27) | 0.71 |
| Annual foot exam | 98.6 | 99.0 | 1.64 (0.59, 4.54) | 0.35 | 1.30 (0.44, 3.86) | 0.63 |
| Annual eye exam | 57.8 | 59.1 | 1.04 (0.83, 1.30) | 0.73 | 1.30 (1.02, 1.66) | 0.04 |
| Quality of Care: Outcomes‡ | ||||||
| A1c <8% | 68.0 | 67.3 | 0.96 (0.76, 1.22) | 0.75 | 1.48 (1.12, 1.95) | 0.006 |
| SBP <140 mmHg | 71.8 | 67.7 | 0.84 (0.66, 1.07) | 0.16 | 0.90 (0.69, 1.17) | 0.42 |
| LDL <100 mg/dl | 69.7 | 55.0 | 0.53 (0.42, 0.67) | <0.001 | 0.62 (0.48, 0.79) | <0.001 |
| HDL > 40 mg/dL (men), or HDL >50 mg/dL (women) | 47.9 | 40.4 | 0.74 (0.59, 0.92) | 0.007 | 0.77 (0.60, 0.98) | 0.03 |
| Regimen Intensity‡ | ||||||
| On 2 or more oral hypoglycemic agents and/or insulin | 69.4 | 67.6 | 0.95 (0.75, 1.20) | 0.66 | 0.77 (0.60, 1.00) | 0.05 |
| On 2 or more blood pressure medications | 53.7 | 51.4 | 0.92 (0.74, 1.15) | 0.46 | 0.98 (0.76, 1.26) | 0.84 |
| On 1 or more lipid lowering medications | 79.7 | 80.8 | 1.02 (0.77, 1.35) | 0.89 | 1.14 (0.84, 1.53) | 0.40 |
| On 2 or more lipid lowering medications | 15.8 | 11.2 | 0.66 (0.47, 0.91) | 0.011 | 0.77 (0.54, 1.10) | 0.15 |
| Reported medication nonadherence§ | ||||||
| related to cost | 24.2 | 32.7 | 1.57 (1.22, 2.01) | 0.001 | 1.34 (1.01, 1.78) | 0.04 |
| related to side effects | 36.8 | 47.2 | 1.61 (1.27, 2.05) | <0.001 | 1.35 (1.04, 1.74) | 0.02 |
Values presented are the percentage of patients within each gender for whom the indicator is present.
Odds ratios and p-values were computed using logistic regression models adjusted for age, education, race/ethnicity, health insurance type and comorbidity.
Derived from medical record abstraction.
From patient report using a seven-item scale in the baseline questionnaire
Similar proportions of women and men were on intensive diabetes regimens including 2 or more oral hypoglycemic agents and/or insulin, and intensive blood pressure regimens including two or more classes of blood pressure medications (see Table 3). However, fewer women (11.2%) than men (15.8%) were prescribed two or more lipid-lowering medications (unadjusted OR [95%CI]: 0.66 [0.47, 0.91], p=0.011), although this difference was not statistically significant after adjustment for race/ethnicity, education, insurance status, history of heart disease and other comorbidities (aOR [95%CI]: 0.77 [0.54, 1.10], p=0.40). More women than men reported nonadherence related to cost (32.7% vs. 24.2%, aOR [95%CI]: 1.34 [1.01, 1.78], p=0.04) and nonadherence related to side effects (47.2% vs. 36.8%, aOR [95%CI]: 1.35 [1.04, 1.74], p=0.02).
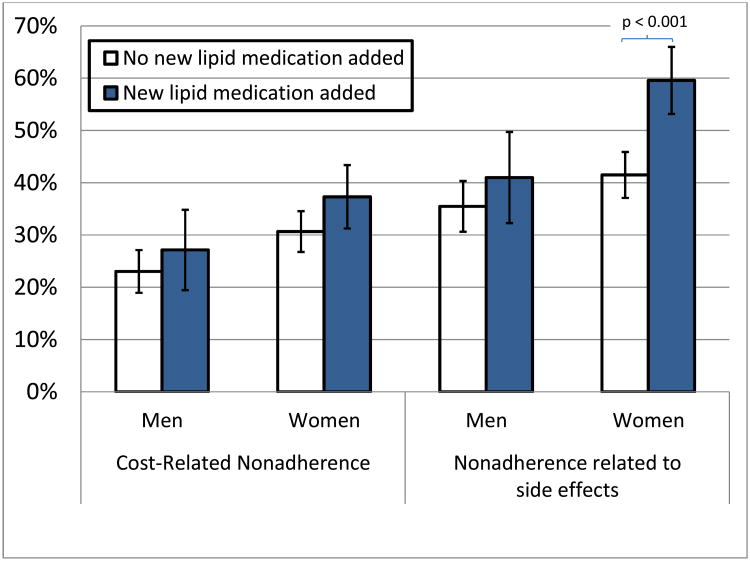
Examination of the reported reasons for nonadherence revealed that intensifying the regimen by adding a new lipid lowering medication was not associated with greater cost-related medication nonadherence for men or for women (Figure 1). However, the addition of a lipid medication was associated with greater medication nonadherence related to side effects of the medication for women but not for men (p-value for the gender by medication intensification interaction = 0.048). Nonadherence related to side effects was reported by 41.0% of men for whom a new lipid lowering drug was added to their regimen compared to 35.5% of men for whom a new medication was not added (aOR [95% CI]: 1.17 [0.76, 1.81], p=0.45). More women for whom a new lipid medication was added (59.6%) reported nonadherence related to side effects of the medication compared to those for whom a new lipid medication was not added (41.5%; aOR [95% CI]: 2.12 [1.52, 2.96], p<0.001). Adding new antihyperglycemic and blood pressure medications carried no association with nonadherence due to cost or due to side effects in either gender (data not shown).
Figure 1.
Comparing the association of treatment intensification with patient-reported cost-related nonadherence and nonadherence related to side-effects of the medication across genders. After adjustment for age, education, race/ethnicity and insurance status, the test for gender by regimen intensification interaction is significant for nonadherence related to side effects (p=0.048). Error bars represent 95% confidence intervals.
In a multivariable regression model that included gender, age, insurance type, race/ethnicity, history of heart disease, comorbidity, regimen intensity (number of classes of lipid lowering medications), nonadherence related to cost and nonadherence related to medication side effects, the adjusted mean LDL cholesterol level for women was 6.5 mg/dl higher (95% CI: 2.1, 10.8; p=0.004) than for men (see Table 4). For both genders, age was associated with lower LDL cholesterol (0.5 mg/dl lower per year of age; 95% CI: -0.7, -0.2; p<0.001), as was Vietnamese race/ethnicity (9.9 mg/dl lower compared to non-Hispanic white patients; 95% CI: -16.9, -2.8; p=0.006), and history of heart disease (8.3 mg/dl lower than patients with no history of heart disease (95% CI: -14.2, -2.5; p=0.005). A more intense regimen of lipid lowering medications was associated with lower LDL cholesterol for both genders (3.8 mg/dl per additional class of lipid lowering medication prescribed; 95% CI: -7.3, -0.3; p=0.033). Patients of either gender who reported medication nonadherence related to side effects, however, had LDL cholesterol levels 6.3 mg/dl higher (95% CI: 2.0, 10.7; p=0.043) compared to patients who did not.
Table 4. Multivariable model predicting LDL cholesterol*.
| Model covariates | Unstandardized beta estimate (95% CI) |
|---|---|
| (Constant) | 127.9 (108.6, 147.3)¶ |
| Female gender† | 6.5 (2.1, 10.8) ‖ |
| Age, yrs† | -0.5 (-0.7, -0.2)¶ |
| Education level, yrs‡ | -0.2 (-0.8, 0.4) |
| Insurance type (ref: commercial insurance)† | |
| Uninsured | 4.6 (-2.9, 12.2) |
| Medicaid | -4.5 (-10.4, 1.4) |
| Medicare | -1.5 (-7.0, 4.0) |
| Race/Ethnicity (ref: non-Hispanic white) ‡ | |
| Hispanic | -1.8 (-8.6, 4.9) |
| Vietnamese | -9.9 (-16.9, -2.8)‖ |
| History of heart disease† | -8.3 (-14.2, -2.5) ‖ |
| Other comorbidity (Total Illness Burden Index score)‡ | 0.2 (-0.8, 1.1) |
| Body mass index† | -0.1 (-0.2, 0.1) |
| Lipid regimen intensity (Number of classes of lipid lowering medications) † | -3.8 (-7.3, -0.3)§ |
| Nonadherence related to cost‡ | 4.6 (-0.3, 9.6) |
| Nonadherence related to side effects‡ | 6.3 (2.0, 10.7) ‖ |
Results from a linear regression model predicting LDL cholesterol level (R2 = .12). Unstandardized beta estimates can be interpreted as the mean difference in LDL cholesterol associated with a one unit change in a given model covariate, adjusted for all other model covariates.
Derived from medical record abstraction.
From patient self-report in the baseline questionnaire.
p<0.05;
p<0.01;
p<0.001
Conclusions & Discussion
Numerous studies have found a gender disparity in cardiovascular risk factors and outcomes and have attempted to illuminate the mechanism behind it (Vaccarino, 2010; Wenger, 2007; Xhyheri & Bugiardini, 2010). In the current study of an ethnically and socioeconomically diverse sample of diabetes patients, women were found to have higher levels of LDL cholesterol than men, despite receiving diabetes care of comparable quality to the care received by men. This finding is consistent with other studies (e.g. Gouni-Berthold et al., 2008; Vimalananda et al., 2011). Also consistent with prior research (e.g. Vimalananda et al., 2011), unadjusted comparisons showed that fewer women than men received intensive treatment for lipids. After adjusting for SES, insurance type and comorbidity in the current study, however, this difference in regimen intensity was not statistically significant, which suggests that factors other than gender bias in prescribing patterns explain the less intensive regimens observed for women.
Although women in this sample were no less likely than men to be put on an intensive lipid-lowering regimen, differences in how women versus men responded to regimen intensification may have contributed to the observed gender disparity in lipid control. Consistent with other studies (e.g. Parris, Lawrence, Mohn, & Long, 2005), results from the multivariable model suggest that, for both genders, the lipid-lowering benefit of being on an intensive regimen was diminished for patients who become nonadherent to the regimen. Women in the current study were more likely than men to be nonadherent to their regimen overall, as reported elsewhere (Lewey et al., 2013; Parris et al., 2005), but were particularly likely to report nonadherence following regimen intensification.
Building on prior work, which relied on medical records data to assess adherence (Parris et al., 2005; Pedan, Varasteh, & Schneeweiss, 2007; Vimalananda et al., 2011), the current study examined reasons for nonadherence obtained from a patient-reported measure. Examination of the reasons reported for nonadherence revealed that adding a new lipid medication was associated with a greater than two-fold increase in the adjusted odds of reporting nonadherence due to side effects in women, but no increase in nonadherence due to side effects in men. Neither women nor men experienced higher rates of nonadherence related to cost following the addition of a new lipid medication. Taken together, these findings suggest that efforts to manage side effects may be particularly helpful to reduce nonadherence and to improve outcomes in women initiating new lipid-lowering medications. To maximize the benefit of regimen intensification to reduce LDL cholesterol, providers should routinely evaluate the side effects of lipid-lowering medications experienced by patients at regular intervals and discuss options to adjust the dosages or classes of medications prescribed until an acceptable option is identified.
Limitations
This study employed secondary analysis of a dataset with a number of strengths, including a diverse sample, the availability of a patient-reported measure of both the extent of and reasons for nonadherence (Billimek & August, 2013), and the assessment of regimen intensity from medical records for a period immediately preceding the collection of patient-reported measures. The dataset also has some important limitations. First, nonadherence is assessed from a single patient-reported measure, which may underestimate the extent of nonadherence among patients in the sample (DiMatteo, 2004). A strength of the specific measure we used, however, is that it assesses the patient's reasons for nonadherence, which are not captured in other types of measures such as medication possession ratios or pill counts (Voils et al., 2012). Second, the dataset includes chart review data indicating the number of classes of antihyperglycemic, lipid and blood pressure medications prescribed and whether a new medication from one of these classes was added in the previous year, but does not indicate the specific classes of medications that were prescribed (e.g. whether the medication was a statin or a fibrate) or the dosage of the medications. Although further study would be required to examine the impact of specific medication classes or dosages on successful lipid management, the data presented here suggest that lipid regimen intensification as it was performed in practice was associated with greater nonadherence due to side effects in women.
Because medication nonadherence was assessed after, but not before, regimen intensification, we cannot determine the temporal direction of the association between these two variables (e.g. whether nonadherence increased after regimen intensification, or if patients with a history of nonadherence were more likely to have their regimens intensified). Finally, given that a significant gender difference in LDL cholesterol is observed in the multivariable model adjusting for nonadherence, regimen intensity and numerous other covariates, and that much of the variation in LDL cholesterol remains unexplained by this model, it is clear that a number of unmeasured factors could contribute to disparities in outcomes between men and women. Future studies may reveal additional important biological and behavioral mechanisms that drive the gender differences observed.
Implications for Practice
Despite receiving diabetes care of comparable overall quality and being prescribed lipid-lowering medication regimens of similar intensity, far fewer women than men achieve adequate lipid control. Although intensive lipid-lowering medication regimens help lower LDL cholesterol, side effects from intensified regimens may lead to nonadherence and diminished benefit for women, more so than for men. This suggests that efforts to improve quality of diabetes care on traditional process measures, and guidelines recommending intensive lipid-lowering therapy for individuals with diabetes may not be adequate to close the gender disparity in lipid management. Efforts to tailor regimens over multiple visits and to help patients effectively manage side effects of intensive therapy may reduce nonadherence following treatment intensification, and lessen the observed gender disparity in LDL cholesterol control.
Acknowledgments
This work was supported by The Robert Wood Johnson Foundation (Grants # 1051084 and #59758), Princeton, New Jersey, The NovoNordisk Foundation, Corporate Diabetes Programmes, Novo Nordisk, Bagsvaerd, Denmark, and the National Institute of Diabetes, Digestive and Kidney Diseases (R18DK69846 and K01DK078939).
Footnotes
All authors have no conflicts of interest to report.
Dr. Billimek had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Avogaro A, Giorda C, Maggini M, Mannucci E, Raschetti R, Lombardo F, et al. Ferrannini E. Incidence of Coronary Heart Disease in Type 2 Diabetic Men and Women Impact of microvascular complications, treatment, and geographic location. Diabetes Care. 2007;30(5):1241–1247. doi: 10.2337/dc06-2558. [DOI] [PubMed] [Google Scholar]
- Billimek J, August KJ. Costs and Beliefs: Understanding Individual- and Neighborhood-Level Correlates of Medication Nonadherence Among Mexican Americans With Type 2 Diabetes. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2013 doi: 10.1037/hea0000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks EL, Preis SR, Hwang SJ, Murabito JM, Benjamin EJ, Kelly-Hayes M, et al. Levy D. Health Insurance and Cardiovascular Disease Risk Factors. The American Journal of Medicine. 2010;123(8):741–747. doi: 10.1016/j.amjmed.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale AC, Vatten LJ, Nilsen TI, Midthjell K, Wiseth R. Secular decline in mortality from coronary heart disease in adults with diabetes mellitus: cohort study. BMJ : British Medical Journal. 2008;337(7661):99–102. doi: 10.1136/bmj.39582.447998.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMatteo M. Variations in patients' adherence to medical recommendations: a quantitative review of 50 years of research. Medical Care. 2004;42(3):200–9. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- Elderkin-Thompson V, Waitzkin H. Differences in Clinical Communication by Gender. Journal of General Internal Medicine. 1999;14(2):112–121. doi: 10.1111/j.1525-1497.1999.tb00006.x. [DOI] [PubMed] [Google Scholar]
- Fisher DM, Brenner CJ, Cheren M, Stange KC. Engagement of groups in family medicine board maintenance of certification. J Am Board Fam Med. 2013;26:149–58. doi: 10.3122/jabfm.2013.02.120262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glied S, Jack K, Rachlin J. Women's Health Insurance Coverage 1980–2005. Women's Health Issues. 2008;18(1):7–16. doi: 10.1016/j.whi.2007.10.002. [DOI] [PubMed] [Google Scholar]
- Gouni-Berthold I, Berthold HK, Mantzoros CS, Böhm M, Krone W. Sex Disparities in the Treatment and Control of Cardiovascular Risk Factors in Type 2 Diabetes. Diabetes Care. 2008;31(7):1389–1391. doi: 10.2337/dc08-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregg EW, Gu Q, Cheng YJ, Venkat Narayan KM, Cowie CC. Mortality Trends in Men and Women with Diabetes, 1971 to 2000. Annals of Internal Medicine. 2007;147(3):149–155. doi: 10.7326/0003-4819-147-3-200708070-00167. [DOI] [PubMed] [Google Scholar]
- Hall JA, Roter DL. Patient gender and communication with physicians: results of a community-based study. Women's Health (Hillsdale, N J) 1995;1(1):77–95. [PubMed] [Google Scholar]
- Homko CJ, Zamora L, Santamore WP, Kashem A, McConnell T, Bove AA. Gender Differences in Cardiovascular Risk Factors and Risk Perception Among Individuals With Diabetes. The Diabetes Educator. 2010;36(3):483–488. doi: 10.1177/0145721710366757. [DOI] [PubMed] [Google Scholar]
- Hvelplund A, Galatius S, Madsen M, Rasmussen JN, Rasmussen S, Madsen JK, et al. Abildstrøm SZ. Women with acute coronary syndrome are less invasively examined and subsequently less treated than men. European Heart Journal. 2010;31(6):684–690. doi: 10.1093/eurheartj/ehp493. [DOI] [PubMed] [Google Scholar]
- Kalyani RR, Lazo M, Ouyang P, Turkbey E, Chevalier K, Brancati F, et al. Vaidya D. Gender Differences in Diabetes and Risk of Incident Coronary Artery Disease in Healthy Young and Middle-Aged Adults. Diabetes Care. 2013 doi: 10.2337/dc13-1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SH, Billimek J, Sorkin DH, Ngo-Metzger Q, Greenfield S. Reducing Racial/Ethnic Disparities in Diabetes: The Coached Care (R2D2C2) Project. Journal of General Internal Medicine. 2013 doi: 10.1007/s11606-013-2452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewey J, Shrank WH, Bowry ADK, Kilabuk E, Brennan TA, Choudhry NK. Gender and racial disparities in adherence to statin therapy: A meta-analysis. American Heart Journal. 2013;165(5):665–678.e1. doi: 10.1016/j.ahj.2013.02.011. [DOI] [PubMed] [Google Scholar]
- Malik S, Billimek J, Greenfield S, Sorkin DH, Ngo-Metzger Q, Kaplan SH. Patient Complexity and Risk Factor Control Among Multimorbid Patients With Type 2 Diabetes: Results From the R2D2C2 Study. Medical Care. 2013;51(2):180–185. doi: 10.1097/MLR.0b013e318273119b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosca L, Jones WK, King KB, Ouyang P, Redberg RF, Hill MN for the American Heart Association Women's Heart Disease and Stroke Campaign Task Force. Awareness, Perception, and Knowledge of Heart Disease Risk and Prevention Among Women in the United States. Archives of Family Medicine. 2000;9(6):506. doi: 10.1001/archfami.9.6.506. [DOI] [PubMed] [Google Scholar]
- Moss SE, Klein R, Klein BE. Cause-specific mortality in a population-based study of diabetes. American Journal of Public Health. 1991;81(9):1158–1162. doi: 10.2105/ajph.81.9.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostadal B, Ostadal P. Sex-based differences in cardiac ischemic injury and protection: Therapeutic implications. British Journal of Pharmacology. 2013:n/a–n/a. doi: 10.1111/bph.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parris ES, Lawrence DB, Mohn LA, Long LB. Adherence to statin therapy and LDL cholesterol goal attainment by patients with diabetes and dyslipidemia. Diabetes Care. 2005;28(3):595–599. doi: 10.2337/diacare.28.3.595. [DOI] [PubMed] [Google Scholar]
- Patchias EM, Waxman J, Fund C. Women and health coverage: The affordability gap. Commonwealth Fund. 2007 Retrieved from http://69.36.173.42/sites/default/files/pdfs/Section%204%20Making%20Health%20Care%20Affordable.pdf. [PubMed]
- Pedan A, Varasteh L, Schneeweiss S. Analysis of factors associated with statin adherence in a hierarchical model considering physician, pharmacy, patient, and prescription characteristics. Journal of Managed Care Pharmacy: JMCP. 2007;13(6):487–496. doi: 10.18553/jmcp.2007.13.6.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rustgi SD, Doty MM, Collins SR, Fund C. Women at risk: Why many women are forgoing needed health care. Commonwealth Fund. 2009 Retrieved from http://thecommonwealthfund.com/∼/media/Files/Publications/Issue%20Brief/2009/May/Women%20at%20Risk/PDF_1262_Rustgi_women_at_risk_issue_brief_Final.pdf. [PubMed]
- Safran DG, Neuman P, Schoen C, Kitchman MS, Wilson IB, Cooper B, et al. Rogers WH. Prescription Drug Coverage And Seniors: Findings From A 2003 National Survey. Health Affairs. 2005;24(Supp):w152–w166. doi: 10.1377/hlthaff.w5.152. [DOI] [PubMed] [Google Scholar]
- Steinberg HO, Paradisi G, Cronin J, Crowde K, Hempfling A, Hook G, Baron AD. Type II Diabetes Abrogates Sex Differences in Endothelial Function in Premenopausal Women. Circulation. 2000;101(17):2040–2046. doi: 10.1161/01.CIR.101.17.2040. [DOI] [PubMed] [Google Scholar]
- Tobin JN, Wassertheil-Smoller S, Wexler JP, Steingart RM, Budner N, Lense L, Wachspress J. Sex bias in considering coronary bypass surgery. Annals of Internal Medicine. 1987;107(1):19–25. doi: 10.7326/0003-4819-107-1-19. [DOI] [PubMed] [Google Scholar]
- Vaccarino V. Ischemic Heart Disease in Women Many Questions, Few Facts. Circulation: Cardiovascular Quality and Outcomes. 2010;3(2):111–115. doi: 10.1161/CIRCOUTCOMES.109.925313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vimalananda VG, Miller DR, Hofer TP, Holleman RG, Klamerus ML, Kerr EA. Accounting for clinical action reduces estimates of gender disparities in lipid management for diabetic veterans. Journal of General Internal Medicine. 2013;28 Suppl 2:S529–535. doi: 10.1007/s11606-013-2340-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vimalananda VG, Miller DR, Palnati M, Christiansen CL, Fincke BG. Gender Disparities in Lipid-Lowering Therapy Among Veterans With Diabetes. Women's Health Issues. 2011;21(4, Supplement):S176–S181. doi: 10.1016/j.whi.2011.04.009. [DOI] [PubMed] [Google Scholar]
- Voils CI, Maciejewski ML, Hoyle RH, Reeve BB, Gallagher P, Bryson CL, Yancy WS. Initial Validation of a Self-Report Measure of the Extent of and Reasons for Medication Nonadherence. Medical Care. 2012;50(12):1013–1019. doi: 10.1097/MLR.0b013e318269e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger NK. Heightened Cardiovascular Risk in Diabetic Women: Can the Tide Be Turned? Annals of Internal Medicine. 2007;147(3):208–210. doi: 10.7326/0003-4819-147-3-200708070-00169. [DOI] [PubMed] [Google Scholar]
- Wexler DJ, Grant RW, Meigs JB, Nathan DM, Cagliero E. Sex Disparities in Treatment of Cardiac Risk Factors in Patients With Type 2 Diabetes. Diabetes Care. 2005;28(3):514–520. doi: 10.2337/diacare.28.3.514. [DOI] [PubMed] [Google Scholar]
- Xhyheri B, Bugiardini R. Diagnosis and Treatment of Heart Disease: Are Women Different From Men? Progress in Cardiovascular Diseases. 2010;53(3):227–236. doi: 10.1016/j.pcad.2010.07.004. [DOI] [PubMed] [Google Scholar]