Abstract
Objectives
To evaluate the impact of doula support on first trimester abortion care.
Study Design
Women were randomized to receive doula support or routine care during first trimester surgical abortion. We examined the effect of doula support on pain during abortion using a 100-mm visual analog scale. The study had statistical power to detect 20% difference in mean pain scores. Secondary measures included satisfaction, procedure duration, and patient recommendations regarding doula support.
Results
Two hundred and fourteen women completed the study: 106 received doula support, 108 received routine care. The groups did not differ regarding demographics, gestational age, or medical history. Pain scores in the doula and control groups did not differ at speculum insertion (38.6mm [±26.3mm] vs. 43.6mm [±25.9mm], p=0.18) or procedure completion (68.2mm [±28.0mm] vs. 70.6mm [±23.5mm], p=0.52). Procedure duration (3.39min [±2.83min] vs. 3.18min [±2.36min], p=0.55) and patient satisfaction (75.2mm [±28.6mm] vs. 74.6mm [±27.4mm], p=0.89) did not differ between doula and control groups. Among women who received doula support, 96.2% recommended routine doula support for abortion and 60.4% indicated interest in training as doulas. Among women who did not receive doula support, 71.6% of women would have wanted it. Additional clinical staff was needed to provide support for 2.9% of women in the doula group and 14.7% of controls (p<0.01).
Conclusions
Although doula support did not have a measurable effect on pain or satisfaction, women overwhelmingly recommended it for routine care. Women receiving doula support were less likely to require additional clinic support resources. Doula support, therefore, may address patient psychosocial needs.
Keywords: abortion, doula, lay health worker, pregnancy termination
INTRODUCTION
Full spectrum doulas are lay people who provide support to women across a variety of reproductive experiences, including birth, miscarriage, adoption, and abortion (1). Doula support during labor and delivery is associated with improved pain control, shorter labor, decreased rates of cesarean delivery, and breastfeeding (2–10).
In abortion care, doulas may serve as an important source of emotional and social support. Additionally, many women who undergo abortion are unlikely to have adequate pain control. In a survey of National Abortion Federation member sites, 46% of clinics provide local anesthesia with or without oral pre-medication, 33% local anesthesia with intravenous sedation, and 21% deep sedation or general anesthesia for first trimester abortions (11). A 2010 literature review concluded that many patients who do not receive general anesthesia find first trimester surgical abortion uncomfortable (12).
During abortion procedures, doulas adopt techniques and skills used in birth settings that may aid in pain management (1). Although, to date, no studies have assessed doulas at the time of abortion, one study evaluating “support people” in an abortion clinic recovery room reported overwhelmingly positive experiences (13). We conducted a non-blinded, randomized controlled trial (RCT) to assess the effect of doula support on pain during first trimester abortion. We hypothesized that women randomized to doula support would have statistically significant less pain compared to women randomized to usual care.
MATERIALS AND METHODS
Women seeking a first trimester surgical abortion at the John H. Stroger, Jr. Hospital of Cook County were recruited between May 2013 and July 2013. The institutional review boards of both the John H. Stroger, Jr. Hospital of Cook County and The University of Chicago approved the study protocol and procedures.
Prior to the start of the study, a family planning fellowship-trained obstetrician gynecologist and two doulas with 5 years of combined experience providing labor and delivery and abortion support (doula trainers) designed and conducted a two-day doula training. The curriculum consisted of 6 lectures, group discussions, and role-playing, including the following topics: medical and psychosocial aspects of abortion care, pregnancy options counseling, clinic logistics, and team building. Trainees learned and practiced doula techniques such as verbal support, handholding, massage, breathing guidance, and relaxation techniques. After completing the training session and prior to functioning independently as a doula in the clinic, trainees shadowed, and were subsequently proctored by one of the two doula trainers.
Researchers recruited women for study participation after obtaining ultrasound confirmation of pregnancy, routine clinic pre-procedure counseling, and completion of the consent process for first trimester surgical abortion. Inclusion criteria included: gestational age less than 14 0/7 weeks, age 18 years or older, English speaking, and able to read and understand the study consent forms. Researchers excluded women who declined participation or who did not meet inclusion criteria.
Women were randomized to doula support or usual care. A research team member not involved in participant recruitment or enrollment generated the allocation scheme using a computer-generated random number sequence. An allocation ratio of one-to-one was used in block sizes of ten for group assignment. Researchers ensured concealment by placing group assignments in sequentially-numbered, opaque sealed envelopes. We revealed allocation to participants at the time of the procedure.
Six attending physicians performed abortion procedures according to clinic protocol. Clinic protocol includes receiving 400 mcg of buccal misoprostol and 800 mg of ibuprofen pre-procedure. Procedures are routinely performed using paracervical block, although administration of local anesthesia is at the discretion of the provider. Physicians perform procedures under ultrasound guidance. Standard protocol includes having at least one physician, one surgical technician, and an ultrasound technician in the room during the procedure. Should a patient need additional support for pain or anxiety during the procedure, an additional clinic staff member is asked to come to the room to assist. Per clinic protocol, patient’s friends, family members and/or partners are not allowed in the procedure room and remain in the waiting area.
Three doulas provided support during the study period: one experienced doula and two women who completed abortion doula training and subsequent proctoring. Doulas introduced themselves to participants upon entry into the procedure room and explained their role at that time. Doulas briefly described the techniques that they commonly used and encouraged women to communicate their preferences regarding which techniques to use. Doulas were present prior to the start of the procedure, through completion of the procedure, and assisted women in returning to the recovery area.
Research assessment points occurred before, during and after the procedure. After providing informed consent, women were asked to complete a brief demographic survey and a 100-mm visual analog scale (VAS) on baseline anxiety about the procedure (anchors: 0-mm=no anxiety, 100-mm=extremely anxious) and anticipated procedure pain (anchors: 0-mm=no pain, 100-mm=worst pain imaginable). Pain was assessed using a 100-mm VAS (anchors: 0-mm=no pain, 100-mm=worst pain imaginable) at the time of speculum insertion, upon completion of the procedure, and in the recovery room roughly 9 minutes (median 8.0 min) minutes after the procedure. Following the procedure, all participants rated their satisfaction in response to the question “How satisfied were you with your experience?” using a 100-mm VAS (anchors: 0-mm=completely unsatisfied, 100-mm=completely satisfied). Women who received doula support completed additional “yes”/“no” questions: “Would you recommend that support people be routinely used during abortion procedures?” and “Would you be interested in training to become an abortion support person?”. Women who did not receive doula support were asked, “Do you wish that you had had someone to provide support during your abortion procedure?”. In addition, we documented procedure time from speculum insertion to removal, as well as procedure difficulty as rated by the provider using a 4-point Likert scale (anchors: “not difficult” and “very difficult”). Providers additionally documented: whether a trainee was involved in the procedure, whether participants required additional pain medication, whether participants required additional support from other clinic staff, and whether an adverse event occurred.
We based sample size on the primary outcome of pain at completion of aspiration. Based on previous studies, we assumed that the mean pain score at completion of aspiration would be 55-mm (14). We determined our sample size based on our consideration that a 20% difference in mean pain scores would be clinically relevant. In order to obtain 80% power with an alpha of 0.05 using a two-tailed hypothesis, 95 participants were needed in each arm. A total of 220 participants, 110 were enrolled in order in each arm, to allow for study attrition and incomplete data (pre-/post-procedure questions).
We entered all baseline, pre-, and post-procedure questionnaire items into IBM SPSS (version 21.0) for analyses. We conducted analyses according to intention-to-treat design and used descriptive statistics to describe the characteristics of the two groups. To compare the study groups with respect to baseline characteristics and outcomes, we used independent group t-tests and Wilcoxon signed-rank tests for continuous variables and Chi-square (X2) and Fisher’s exact tests for categorical variables. We considered P-values <0.05 to be statistically significant.
RESULTS
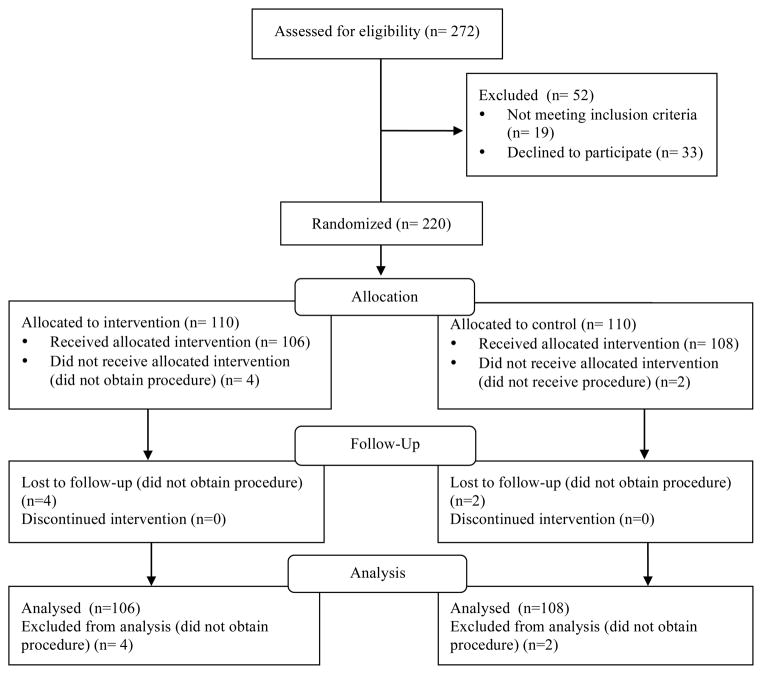
A total of 272 women were approached for enrollment in the study; 33 declined to participate and 19 did not meet eligibility criteria (17 due to age requirements and 2 due to language requirements). We enrolled 220 in the study, including six women who did not ultimately undergo an abortion procedure, with a total of 214 completing study procedures; 106 were randomized to the doula group and 108 were randomized to the control group (i.e. women who did not receive doula support). The mean age of participants was 24.5 years, with the majority of women (87.7%) identifying as African-American (Table 1). The mean gestational age was 62.5 days and women had an average of 3.6 previous pregnancies: with an average of 1.6 living children, 0.99 previous elective abortion, and 0.22 previous miscarriages. Groups did not differ significantly on demographic and baseline obstetric and gynecologic variables (Table 1).
Table 1.
Demographic Variables
| Characteristic | Doula Group (n=106) | Control Group (n=108) | Significance (p) |
|---|---|---|---|
| Age (years) | 24.8 ± 4.96 | 24.3 ± 4.99 | 0.48 |
| Race/Ethnicity | 84.9% African American | 90.8% African American | 0.18 |
| Marital Status | 86.8% single | 90.8% single | 0.69 |
| BMI (kg/m2) | 29.3 | 28.5 | 0.44 |
| Gestational age (days) | 62.4 ± 15.5 | 62.5 ± 15.3 | 0.96 |
| Gravidity | 3.5 ± 1.8 | 3.6 ± 2.2 | 0.89 |
| Previous vaginal deliveries | 1.3 ± 1.2 | 1.3 ± 1.3 | 0.79 |
| Previous elective abortions | 0.94 ± 1.0) | 1.0 ± 1.8) | 0.77 |
| Previous dilation and curettage | 1.9% | 4.6% | 0.27 |
| Previous LEEP | 3.8% | 3.7% | 0.97 |
| Previous Cervical conization | 0.9% | 0.9% | 0.98 |
| Previous cervical laser ablation | 0.9% | 0% | 0.31 |
Values are mean ± standard deviation or n (%).
Measures of pain and anxiety did not differ between the two groups at any of the assessment points. At baseline, there were no significant differences in VAS scores on anticipated pain (mean 51.9mm compared with 55.0mm, p=0.43) and anxiety (mean 60.3mm compared with 54.9mm, p=0.23) (Table 2). Additionally, the doula and control groups did not differ with regards to pain at the time of speculum insertion (mean 38.6mm compared with 43.6mm, p=0.18) or pain with the abortion procedure (mean 68.2mm compared with 70.6mm, p=0.52). No differences were found for procedure duration between women randomized to doula care and those randomized to routine care (mean 3.4 min, median 3.0 min compared with 3.2 min, median 3.0 min p=0.55).
Table 2.
Anticipated and Procedural Pain and Anxiety
| Doula Group | Control Group | Significance (p) | |
|---|---|---|---|
| Pre-procedure anticipated pain (mm) | 51.9 ± 27.2 | 55.0 ± 30.0 | 0.43 |
| Pre-procedure anxiety (mm) | 60.3 ± 31.2 | 54.9 ± 34.3 | 0.23 |
| Duration of procedure (minutes) | 3.39 ± 2.83 | 3.18 ± 2.36 | 0.55 |
| Pain with speculum insertion (mm) | 38.6 ± 26.3 | 43.6 ± 25.9 | 0.18 |
| Pain with abortion procedure (mm) | 68.2 ± 28.0 | 70.6 ± 23.5 | 0.52 |
Values are mean ± standard deviation.
Post-procedure, the majority of women in both arms reported being satisfied with the procedure (mean 75.2mm compared with 74.6mm, p=0.89). Recalled pain did not differ between women randomized to doula care compared to those randomized to usual care (mean 63.5mm compared with 65.0mm, p=0.697). When asked about their experiences, 96.2% of women who received doula support would recommend that doula support be routinely used during procedures and 60.4% expressed interest in training to become a doula. A large proportion (71.6%) of women who did not receive doula support reported that they would have wanted someone present to provide support during their procedure.
Providers gave favorable ratings to both groups regarding ease of procedures. Responses included: “Not difficult” (95.3% compared with 90.8%, p=0.32) (Table 3). The majority of women in the doula and control groups (72.6% compared with 73.4%, p= 0.90) received paracervical blocks and trainees were involved in less than 10% of procedures in both groups. No adverse events were reported for either group. The need for additional support from clinic staff normally assigned to other clinical tasks, was significantly different between the two groups, with 2.9% of women in the doula group requiring additional support, such as handholding, from a clinic staff member compared to 14.7% in the control group (p=0.002).
Table 3.
Provider and procedural descriptives
| Doula Group | Control Group | Significance (p) | |
|---|---|---|---|
| Difficulty of procedure | 95.3% Not difficult | 90.8% Not difficult | 0.31 |
| Trainee involvement | 9 (8.5) | 9 (8.3) | 0.95 |
| Received paracervical block | 77 (72.6) | 88 (73.4) | 0.90 |
| Need for additional support | 3 (2.9) | 16 (14.7) | 0.002 |
Values are n (%).
COMMENT
This paper evaluates the effect of doula support at the time of abortion on a range of clinical outcomes. Overall, we found that women randomized to doula support almost universally felt that it should become part of routine care. Similarly, women not randomized to doula care also endorsed routine support. We also found that the need for additional clinic staff to provide supplemental support was significantly higher among procedures for control women. Therefore, while not alleviating perceived and experienced pain, the incorporation of a volunteer doula program in this busy abortion clinic did help to decrease the re-direction of clinic staff resources. However, despite the overwhelming positive endorsement for “support during procedures” from all women, our study did not find a statistically significant effect on any of the major outcomes that we considered including pain and satisfaction. Additionally, women in both arms were equally satisfied. This likely reflects the fact that all respondents received the care that they intended to receive – a safe termination of pregnancy. Finally, the majority of women who experienced doula care actually expressed interest in training to become a doula themselves. This interest may reflect admiration or gratitude for the service.
This study has a number of strengths. First, there are limited studies on doula support at the time of first trimester abortion and we provide quantitative information in a randomized study. The high-volume of our research setting allowed for rapid recruitment and enrollment and ensured that we reached adequate statistical power to assess primary outcomes. The comparable demographic data between both groups reflects our success in randomization procedures.
Yet, we must also note limitations. First, we enrolled both primiparous and multiparous women and women who had and had not had previous abortions. Additionally, a small minority of participants in both arms did not receive a paracervical block. Although we did not have adequate statistical power to conduct sub-group analyses to evaluate the possible effects of obstetric history or lack of paracervical block on women’s experiences with pain or satisfaction at the time of abortion, our study groups were comparable with regards to obstetric and gynecologic factors and presence or absence of paracervical block. Second, as our sample was not demographically diverse, consisting primarily African-American women of low socioeconomic status presenting to a public hospital, our findings may not be generalizable to all practice settings. The generalizability of our findings may also be limited by the fact that all participants received misoprostol prior to their procedure, a practice that may not be common to all clinical sites and may impact the level of pain that women experienced during their procedure. All of the doulas participating in this study were white, which may have impacted the interaction between doulas and largely African-American study participants. While literature on lay health workers (LHW) explores the value of shared backgrounds between LHWs and their clients, we did not explore the role of race/ethnicity concordance or discordance in this study (15). Lastly, doulas provided individualized support depending on each patient’s needs and preferences. Thus, the intervention was necessarily heterogeneous and we were unable to examine the effects of specific techniques (breathing guidance, handholding, etc.).
Pain control at the time of abortion is an important problem. Although most first trimester surgical abortions in this country are performed using local anesthesia, with or without pre-medication, there are conflicting data regarding the effectiveness of this method in reducing pain at the time of abortion (11, 12, 16). It is reasonable to believe that doula support may reduce pain. A variety of psychosocial and emotional factors such as anxiety, depression, and anticipation of pain, influence women’s experiences with pain at the time of abortion (17–20). Finally, there is ample literature demonstrating the impact of doula support on pain during labor and delivery (3, 7, 10). Nevertheless, we did not find a significant difference in pain scores.
Prior non-pharmacologic interventions may provide insight into why doula support may not change perception of pain. Previous studies evaluating the effects of non-pharmacologic auxiliary interventions (such as music) on pain during abortion have demonstrated mixed results (1, 21, 22). While these types of interventions likely address emotional components of pain, they may have limited benefits in addressing physiologic components of pain. Additionally, different approaches to measuring pain are able to capture different components of pain management. Several studies of doula support at the time of labor and delivery demonstrate that doula support is associated with delayed epidural use and/or lower epidural rates (3, 7, 10). Although doula support in this context may decrease physical pain, an alternative interpretation of these data is that that doula support helps women cope with pain. Our study results may potentially reflect a similar phenomenon: that a resounding majority of women valued doula support despite a lack of measureable improvement in pain may indicate that doula support helps women cope with aspects of the abortion procedure that were not specifically assessed in this study. Similarly, high rates of reported satisfaction among all women most likely reflect their feelings about the outcome of the procedure itself, not the process.
Ultimately, this study demonstrates that doula support is highly valued by women who receive it, but is not perceived as a solution for pain. Fortunately, there are very good pharmacologic approaches to pain management in the form of deep sedation or general anesthesia. Although exploring alternative modes of pain control is still warranted, perhaps barriers to adequate pain management at the time of abortion are financial and logistical rather than scientific. Nevertheless, despite not necessarily receiving a direct benefit in pain reduction, women in this study liked doula support, wished it for a fellow patient, and would have liked to be trained to be a doula themselves. Our study’s findings are relevant and timely, as volunteer abortion doula groups are organizing across the country and increasingly being used in clinics (1). Therefore, fully understanding the potential benefits and limitations of doula care is important for providers considering incorporating this service into their practice setting.
Figure 1.
CONSORT Flowchart. This chart demonstrates the number of women recruited, excluded, randomized, and analyzed during the study period.
Acknowledgments
Funding: Funding for this study was provided through a grant from the Society of Family Planning. Research reported in this publication was supported by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Number KL2TR000431.
Kate Palmer: Hektoen Institute, Chicago, IL. Assisted in intervention development. Not compensated for this work.
Alicia Roston: Hektoen Institute, Chicago, IL. Assisted in data collection. Not compensated for this work.
Kelly Stempinski: Hektoen Institute, Chicago, IL. Assisted in data collection. Not compensated for this work.
Footnotes
Conflict of Interest: All authors have no conflict of interest.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Findings reported in this manuscript were presented as an oral presentation at the National Abortion Federation Annual Meeting, San Francisco, CA, April 5–8, 2014.
ClinicalTrials.gov Identifier: NCT01937988
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chor J, Goyal V, Roston A, Keith L, Patel A. Doulas as Facilitators: The Role of Doulas in Abortion Care. Journal of Family Planning and Reproductive Health Care. 2012;38(2):123–4. doi: 10.1136/jfprhc-2011-100278. [DOI] [PubMed] [Google Scholar]
- 2.Klaus MH, Kennell JH. The doula: an essential ingredient of childbirth rediscovered. Acta Paediatr. 1997;86:1034–6. doi: 10.1111/j.1651-2227.1997.tb14800.x. [DOI] [PubMed] [Google Scholar]
- 3.Scott K, Klaus P, Klaus M. The Obstetrical and Postpartum Benefits of Continuous Support during Childbirth. Journal of Women’s Health & Gender Based Medicine. 1999;8(10):1257–1265. doi: 10.1089/jwh.1.1999.8.1257. [DOI] [PubMed] [Google Scholar]
- 4.Campbell D, Lake M, Falk M, Backstrand J. A Randomized Control Trial of Continuous Support in Labor by a Lay Doula. JOGNN. 2006;35:456–464. doi: 10.1111/j.1552-6909.2006.00067.x. [DOI] [PubMed] [Google Scholar]
- 5.Nommsen_Rivers L, Mestergeorge A, Hansen R, Cullum A, Dewey K. Doula Care, Early Breastfeeding Outcomes, and Breastfeeding Status at 6 Weeks Postpartum Among Low-Income Primiparae. JOGNN. 2009;38:157–173. doi: 10.1111/j.1552-6909.2009.01005.x. [DOI] [PubMed] [Google Scholar]
- 6.Hodnett ED, Osborn RW. Effects of Continuous Intrapartum Professional Support on Childbirth Outcomes. Research in Nursing & Health. 1989;12:289–97. doi: 10.1002/nur.4770120504. [DOI] [PubMed] [Google Scholar]
- 7.Gordon NP, Walton D, McAdam E, Derman J, Gallitero G, Garrett L. Effects of Providing Hospital-Based Doulas in Health Maintenance Organization Hospitals. Obstet Gynecol. 1999;93:422–6. doi: 10.1016/s0029-7844(98)00430-x. [DOI] [PubMed] [Google Scholar]
- 8.Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Continuous Emotional Support During Labor in a US Hospital. JAMA. 1991;265(17):2197–2201. [PubMed] [Google Scholar]
- 9.Scott K, Klaus P, Klaus M. The Obstetrical and Postpartum Benefits of Continuous Support during Childbirth. Journal of Women’s Health & Gender based Medicine. 1999;8(10):1257–1265. doi: 10.1089/jwh.1.1999.8.1257. [DOI] [PubMed] [Google Scholar]
- 10.McGrath SK, Kennell JH. Continuous labor support for middle-class couples: effect on cesarean section rates. BIRTH. 2008;35(2):92–7. doi: 10.1111/j.1523-536X.2008.00221.x. [DOI] [PubMed] [Google Scholar]
- 11.O’Connell K, Jones HE, Simon M, Saporta V, Paul M, Lichtenberg ES. First-trimester surgical abortion practices: a survey of National Abortion Federation members. Contraception. 2009;79:385–392. doi: 10.1016/j.contraception.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Renner R-M, Jensen JT, Nichols MD, Edelman A. Pain control in first-trimester surgical abortion: a systematic review of randomized controlled trials. Contraception. 2010;81:372–388. doi: 10.1016/j.contraception.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Veiga MB, Lam M, Gemeinhardt C, Houlihan E, Fitzsimmons BP, Hodgson ZG. Social support in the post-abortion recovery room: evidence from patients, support persons and nurses in a Vancouver clinic. Contraception. 2011;83:268–273. doi: 10.1016/j.contraception.2010.07.019. [DOI] [PubMed] [Google Scholar]
- 14.Edelman A, Nichols MD, Jensen J. Comparison of pain and time of procedures with two first-trimester abortion techniques performed by residents and faculty. Am J Obstet Gynecol. 2001;184:1564–7. doi: 10.1067/mob.2001.114858. [DOI] [PubMed] [Google Scholar]
- 15.Hans S, Korfmacher J. The professional development of paraprofessionals. Zero to Three. 2002;23(2):4–8. [Google Scholar]
- 16.Renner R-M, Nichols MD, Jensen JT, Li H, Edelman AB. Paracervical block for pain control in first-trimester surgical abortion: a randomized controlled trial. Contraception. 2012;119:1030–7. doi: 10.1097/AOG.0b013e318250b13e. [DOI] [PubMed] [Google Scholar]
- 17.Smith GM, Stubblefield PG, Chirchirillo L, McCarthy MJ. Pain of first-trimester abortion: its quantification and relations with other variables. Am J Obstet Gynecol. 1979;133:489–98. doi: 10.1016/0002-9378(79)90282-5. [DOI] [PubMed] [Google Scholar]
- 18.Pud D, Amit A. Anxiety as a predictor of pain magnitude following termination of first-trimester pregnancy. Pain Med. 2005;6:143–148. doi: 10.1111/j.1526-4637.2005.05030.x. [DOI] [PubMed] [Google Scholar]
- 19.Belanger E, Melzack R, Lauzon P. Pain of first-trimester abortion: a study of psychosocial and medical predictors. Pain. 1989;36:339–350. doi: 10.1016/0304-3959(89)90094-8. [DOI] [PubMed] [Google Scholar]
- 20.Singh RH, Ghanem KG, Burke AE, Nichols MD, Rogers K, Blumenthal PD. Predictors and perception of pain in women undergoing first trimester surgical abortion. Contraception. 2008;78:155–61. doi: 10.1016/j.contraception.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Guerrero JM, Castano PM, Schmidt EO, Rosario L, Westhoff CL. Music as an auxiliary analgesic during first trimester surgical pain: a randomized controlled trial. Contraception. 2012;86:157–62. doi: 10.1016/j.contraception.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro AG, Cohen H. Auxiliary pain relief during suction curettage. Contraception. 1975;11:25–30. doi: 10.1016/0010-7824(75)90047-5. [DOI] [PubMed] [Google Scholar]