Abstract
Objectives
We estimate the prevalence of malnutrition among older patients presenting to an emergency department (ED) in the southeastern United States and identify subgroups at increased risk.
Methods
We conducted a cross-sectional study with random time block sampling of cognitively intact patients aged 65 years and older. Nutrition was assessed using the Mini Nutritional Assessment Short-Form (0–14 scale) with malnutrition defined as a score of 7 or less and at-risk for malnutrition defined as a score of 8–11. The presence of depressive symptoms was defined as a Center for Epidemiological Studies Depression-10 score of 4 or more (0–10 scale).
Results
Among 138 older adults, 16% (95% Confidence Interval [CI], 10%–22%) were malnourished and 60% (95% CI, 52%–69%) were either malnourished or at-risk for malnutrition. Seventeen of the 22 malnourished patients (77%) denied previously being diagnosed with malnutrition. The prevalence of malnutrition was not appreciably different between males and females, across levels of patient education, or between those living in urban and rural areas. However, the prevalence of malnutrition was higher among patients with depressive symptoms 52%, those residing in assisted living 50%, those with difficulty eating 38%, and those reporting difficulty buying groceries 33%.
Conclusion
Among a random sample of cognitively intact older ED patients, more than half were malnourished or at-risk for malnutrition, and the majority of malnourished patients had not previously been diagnosed. Higher rates of malnutrition among those with depression, difficulty eating, and difficulty buying groceries suggest the need to explore multifaceted interventions.
Keywords: Geriatrics, Emergency Medicine, Malnutrition
INTRODUCTION
Malnutrition is a common but under-diagnosed condition in older adults that is associated with physical and cognitive decline,1,2 decreased quality of life,3 and mortality.4 Malnutrition disproportionately affects older adults,5,6 and results from a combination of changes related to aging, comorbidities, medications, and environmental factors influencing the availability and desirability of food and the ability to eat and absorb nutrients.7 Pooled estimates report the prevalence of malnutrition among community-dwelling older adults of 6% and among hospitalized older adults of 39%.8 In developed countries, treatment of malnutrition is relatively inexpensive and effective: energy and protein supplementation using commercial ‘sip feeds’ results in both weight gain and reduced mortality.9 Despite the existence of brief, accurate instruments to screen for malnutrition, implementation of screening protocols across health care settings is inconsistent. Failure to identify malnutrition is a major obstacle to ensuring that malnourished older adults receive optimal nutritional support.10–12
Older adults make more than 20 million visits to United States emergency departments (EDs) each year. EDs provide an important setting for screening for chronic under-diagnosed medical problems because they provide access to patients who do not receive routine medical care.13,14 The value of using the ED as a setting for identifying important health conditions has been demonstrated for HIV, domestic violence, and substance abuse.15–18 Although there is growing awareness of the potential value of screening for health conditions among older adults in the ED, including non-medical conditions, malnutrition was not identified as a screening target in recently published guidelines.19,20 A 2013 study in Australia demonstrated the feasibility of interventions to treat malnutrition among older ED patients,21 but in order to determine the potential impact of such interventions, a better understanding of the epidemiology of malnutrition among older ED patients is needed. We sought to estimate the prevalence of malnutrition and risk for malnutrition among older adults presenting to a single ED and identify subgroups at increased risk.
METHODS
Study Design
This was a cross-sectional study of ED patients aged 65 years and older. Patient recruitment and enrollment by four trained research assistants occurred over a period of 8 weeks in June and July 2013 during 32 four-hour periods randomly selected as follows: first, four distinct days (including weekends) were selected within each week; second, the start time for each period was selected with equal probability from 9 a.m., 1 p.m., or 5 p.m. Consenting participants completed an in-person interview in the ED which assessed sociodemographic characteristics, nutritional status, and medical history. The study was approved by the study site Institutional Review Board and each patient provided written informed consent.
Setting
The study was conducted in a single academic ED in the southeast United States serving a racially and socioeconomically diverse population of older adults. In the calendar year of 2013, the ED had approximately 70,080 visits with 10,464 visits (14.9%) by patients aged 65 years and older.
Selection of Participants
Patients were eligible if aged 65 years or older, not cognitively impaired, not living in a nursing home or skilled nursing facility, and not experiencing an immediate life-threatening illness or injury as determined by an Emergency Severity Index score of 122 or as judged by the treating emergency provider. Cognitive impairment was defined as a Six Item Screener score of 3 or less.23 Patients who were still in the ED but had a hospital bed assigned (i.e. already admitted) or had received discharge papers (i.e. already discharged) were excluded so that the study did not interfere with the flow of patients out of the department. Patients who were not admitted or discharged at the time of screening were eligible regardless of their final disposition. Research assistants (RAs) assessed each patient’s eligibility. In order to prevent selection bias, patients were approach by RAs in an order determined by random number generator. This order was generated at the beginning of each time block. Among eligible, consenting patients, study data were collected via an in-person interview by the RA.
Prior to collecting data, RAs were instructed in how to determine which patients were eligible for screening and how to code possible responses to screening and interview questions. Each RA then observed an interview conducted by an emergency physician with experience in prospective ED research and performed a survey while observed by this emergency physician. Weekly meetings were held to review the screening and enrollment process and address RA questions.
Data Collection and Measures
Consistent with usage by the Academy of Nutrition and Dietetics, the term malnutrition is used here to describe patients who lack “adequate calories, protein, or other nutrients needed for tissue maintenance and repair.”24 Nutritional status was measured using the Mini-Nutritional Assessment Short-Form (MNA-SF), a validated 6-item tool which combines body mass index (BMI) and patient responses to factors previously linked to malnutrition: weight loss, decline in food intake, recent psychological stress or acute disease, mobility, and neuropsychological disorders.25 The results of the MNA-SF are summed to produce a score from 0–14 with malnutrition defined as a score ≤7 and at-risk for malnutrition defined as a score of 8–11.25 Consistent with the instructions for using the MNA-SF, calf-circumference was measured and used to generate the summary score in patients who were unable to stand for the measurement of height and weight. The MNA-SF screening questions and score interpretation are available at http://www.mna-elderly.com/forms/mini/mna_mini_english.pdf. In addition to sociodemographic groupings, subgroups of patients assessed for increased risk for malnutrition were identified based on a review of literature on malnutrition and included patients with difficulty eating,26,27 difficulty buying groceries,28 depression,27,29 lack of transportation,27,30 and difficulty walking.27,24 Patients who reported depression in the MNA-SF or who answered yes to either of two depression screening questions31 were administered the 10-item Center for Epidemiological Studies Depression-10 (CESD-10).32 Depression was then defined as a CESD-10 score of four or more among these individuals.33
In order to determine whether malnutrition was recognized by the emergency provider or emergency nurse, two authors independently reviewed physician and nursing records for all patients with a MNA-SF score of ≤7. These reviews searched explicitly for a positive response to the single-item question regarding malnutrition which is a standard prompt in the triage nursing note or any other information contained elsewhere in the record indicating the diagnosis or provision of treatment for malnutrition. Prior to conducting the search, the following descriptors or variants thereof were considered recognition of malnutrition: malnutrition; cachexia; wasting; failure to thrive; weight loss; inadequate food intake; or the need for nutritional supplementation, improved diet, nutritional counseling, or food stamps. For 10 randomly selected patients, the time to administer the MNA-SF was measured. This measurement included the time to administer the five verbal questions as well as measure BMI or calf-circumference.
Data Analysis
Data are reported as proportions with 95% confidence intervals. The estimated prevalences of a) malnutrition and b) either malnutrition or at-risk for malnutrition are reported for the entire sample and among subgroups of participants stratified by sociodemographic characteristics and comorbidities. Prevalences are compared across subgroups in a descriptive manner without formal statistical testing. Consistent with this, observed differences that appear to be clinically important are identified and presented as generating rather than confirming hypotheses.
Based on the observation of a notably higher rate of malnutrition in patients with depression, a post-hoc sensitivity analysis was conducted to assess for an association between depression and malnutrition using a definition of malnutrition that did not include information about depression. To do this, a new MNA-SF summary score ranging from 0–12 was calculated for all patients excluding the question assessing neuropsychological problems, which yields 2 points for patients without dementia or depression. This new score was dichotomized by defining malnutrition as a score ≤5, and the prevalence of malnutrition using this revised definition is reported for patients with and without depression.
RESULTS
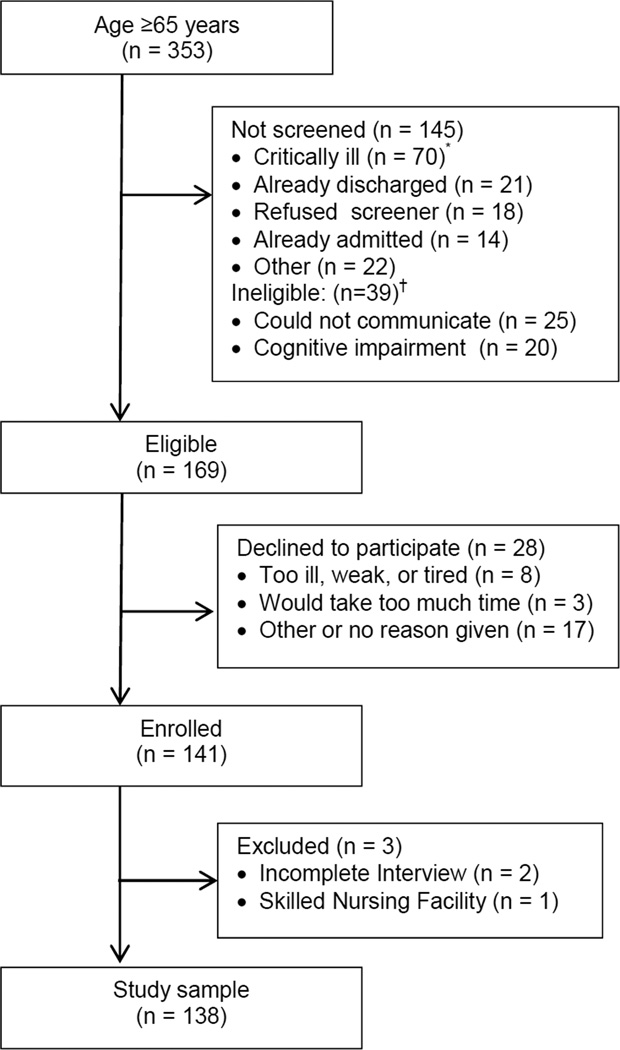
A total of 353 patients aged 65 years or older presented to the ED during the 128 hours of enrollment. Of these patients, 169 were eligible, 141 were enrolled, and 138 (82% of eligible) completed the interview and were included in subsequent analyses (Figure). The most common reasons that patients were not screened were because they were critically ill (n=70), could not communicate (n=25), were cognitively impaired (n=20), or were already discharged (n=21). In our sample, 69% of participants were white and 35% had a college education. By comparison, recent values for individuals aged 65 years and older in the United States are 79% white (2011) and 20% college educated (2009).34,35 Almost all patients had a primary provider (95%), lived in a private residence (94%), and had some health insurance (96%). Four percent had both Medicare and Medicaid coverage (i.e. dual eligible), and 64% had both Medicare as well as some form of secondary insurance.
Figure 1.
Flow diagram of eligibility and enrollment in the emergency department
* Emergency severity index triage score of 1 or too ill as judged by the treating provider
† Not mutually exclusive
Malnutrition as defined by an MNA-SF score ≤7 was identified in 22 patients, corresponding to an overall prevalence of 15.8% (95% confidence interval [CI], 9.7% to 21.9%). Of these 22 patients, only 5 (23%) had been previously diagnosed with malnutrition. The combined prevalence of malnutrition or at-risk for malnutrition was 60.4% (95% CI, 52.2% to 68.6%) and over 50% across all subgroups assessed in this study. The prevalence of malnutrition was not substantially different for females vs. males, across levels of educational attainment, or for those aged 65–74 years vs. 75 years and older (Table).
Table.
Estimated prevalences of a) malnutrition and b) malnutrition or at-risk for malnutrition among patient subgroups.
| %, 95% CI | |||
|---|---|---|---|
| Characteristic | N | Malnourished | Malnourished or At-Risk |
| All | 138 | 15.8 (9.7,21.9) | 60.4 (52.2,68.6) |
| Sex | |||
| Female | 77 | 18.0 (9.5,26.5) | 62.9 (52.1,73.7) |
| Male | 61 | 13.1 (4.6,21.6) | 54.1 (41.6,66.6) |
| Age | |||
| 65–74 | 86 | 17.2 (9.3,25.1) | 63.2 (53.0,73.4) |
| ≥75 | 52 | 13.5 (4.2,22.8) | 52.0 (25.3,51.7) |
| Education | |||
| Not college graduate* | 90 | 17.8 (9.9,25.7) | 62.2 (52.2,72.2) |
| College graduate | 48 | 12.5 (3.1,21.9) | 56.3 (42.3,70.3) |
| Race | |||
| White | 95 | 17.1 (9.6,24.6) | 55.6 (45.6,65.6) |
| Black | 36 | 8.3 (0.0,17.3) | 69.4 (54.4,84.5) |
| Other | 7 | 16.7 (0.0,46.5) | 50.0 (13.0,87.0) |
| Living arrangement | |||
| Private residence | 131 | 13.9 (8.0,19.9) | 58.5 (50.0,67.0) |
| Assisted living facility | 7 | 50.0 (15.4,84.7) | 75.0 (45.0, 100) |
| Population density | |||
| Rural | 90 | 14.6 (7.3,21.9) | 61.8 (51.8,71.8) |
| Urban | 48 | 16.7 (6.2,27.3) | 58.4 (44.4,72.3) |
| Disposition | |||
| Admitted | 72 | 25.4 (15.4,35.5) | 64.8 (53.8,75.8) |
| Discharged | 66 | 6.0 (0.3,11.7) | 56.0 (44.0,68.0) |
| Prescription medications | |||
| ≤5 | 32 | 0.0 (0.0,0.4) | 50.0 (32.7,67.3) |
| >5 | 106 | 20.6 (12.9,28.3) | 63.6 (54.4,72.8) |
| Charlson comorbidity index | |||
| 0–3 | 72 | 6.9 (1.1,12.8) | 59.7 (48.4,71.0) |
| 4 or more | 67 | 25.4 (15.0,35.8) | 61.2 (49.5,72.9) |
| Difficulty buying groceries | |||
| Yes | 12 | 33.3 (6.6,60.0) | 66.6 (39.9,93.3) |
| No | 125 | 14.4 (8.3,20.6) | 59.2 (50.6,67.8) |
| Lack of transportation | |||
| Yes | 17 | 15.8 (12.6,58.0) | 60.4 (37.2,83.7) |
| No | 122 | 13.1 (7.1,19.1) | 59.0 (50.3,67.7) |
| Difficulty walking | |||
| Yes | 66 | 27.2 (16.9,38.5) | 66.6 (55.2,78.0) |
| No | 73 | 5.5 (0.3,10.7) | 54.8 (43.4,66.2) |
| Depression | |||
| Yes | 25 | 52.0 (32.4,71.6) | 84.0 (69.6,98.4) |
| No | 113 | 8.0 (3.0,13.0) | 54.9 (45.7,64.1) |
| Live Alone | |||
| Yes | 35 | 17.1 (4.6,29.6) | 74.3 (59.8,88.8) |
| No | 103 | 15.4 (8.4,22.4) | 55.8 (46.2,65.4) |
| Lack of social support | |||
| Sometimes/often | 20 | 25.0 (6.0, 44.0) | 80.0 (62.5,97.5) |
| Rarely/never | 118 | 14.5 (8.2,20.9) | 55.9 (46.9,64.9) |
| Difficulty eating | |||
| Yes | 16 | 37.5 (13.8,61.2) | 75.0 (53.8,96.2) |
| No | 123 | 13.1 (7.1,19.1) | 58.2 (49.5,66.9) |
The prevalence of malnutrition was notably higher in the following patient subgroups: those residing in assisted living; those reporting difficulty buying groceries sometimes or often in the past year; those with symptoms of depression; and those with difficulty eating. Since the MNA-SF includes an item measuring depression, we conducted a sensitivity analysis excluding that item, and results remained robust. In that analysis, 40.0% (95% CI, 14.2% to 40.2%) of individuals with symptoms of depression were rated as malnourished vs. only 5.3% (95% CI, 2.5% to 11.1%) of individuals without symptoms of depression. Of the 16 patients reporting difficulty eating, 6 reported denture problems, 3 reported dental pain, 3 reported difficulty swallowing, and 4 reported some other problem. Of those participants who were discharged home from the ED (i.e., not hospitalized), 6.0% (95% CI, 0.3% to 11.7%) were malnourished and 56% were either malnourished or at-risk for malnutrition. Among the 22 patients with malnutrition, no information was identified by either reviewer in either the physician or nurse records to indicate recognition of the problem of malnutrition. There was perfect agreement between the two reviewer’s findings. Additionally, for 16 of these 22 patients, the single-item assessment of malnutrition was completed by the triage nurse and indicated no problem with malnutrition. For the 6 remaining patients, the singe-item assessment was not completed. However, 4 of the 22 patients diagnosed with malnutrition had been told in the past that they were malnourished. Among a random sample of 10 participants, the total time to administer the MNA-SF ranged from 3 to 5 minutes. The most variable component and major determinant for the overall time length to complete the MNA-SF was the time it took to measure the patient’s height and weight.
LIMITATIONS
This study has several limitations. The sample size prevents us from providing precise estimates of the prevalence of malnutrition among less prevalent patient subgroups, such as residents of assisted living facilities. RAs were not blinded to the purpose of the study and may have had preconceived ideas regarding which factors would predict malnutrition, creating the possibility of differential misclassification of nutritional status by patient characteristics. We did not perform a test of the inter-rater reliability of the administration of the MNA-SF, and the MNA-SF has not been validated in the ED, although has been validated in older adults across a broad spectrum of settings.25,36
Not all factors that might contribute to malnutrition among older adults were assessed in this study. Medications with anticholinergic properties and several other commonly prescribed medications including metronidazole, sulfamethoxazole, and carbidopa-levadopa either increase constipation, decrease salivation, or suppress appetite and can contribute to decreased food intake and malnutrition.37,38 Modifying medications regimens might be a valuable addition to a program to improve nutritional status among older adults. While eating disorders generally manifest during adolescence, an estimated 70% of community dwelling older women report currently being on a diet and 4% of older women suffer from an eating disorder.39,40 Identification of an eating disorder might be an essential step in improving nutritional health in some older adults. Elder abuse, particularly neglect, might also contribute to the problem of malnutrition among some older adults. Neither the MNA-SF nor any of the additional questions we asked throughout the survey provided insight into whether malnutrition, when present, was an acute or a chronic problem. This distinction might be important in identifying appropriate treatments. A strong relationship between depression and malnutrition was identified, impelling us to perform a post-hoc analysis using a modified version of the MNA-SF which excluded the question about depression. Though the MNA-SF has been validated, our modified version has not.
We excluded older adults who were critically ill, had moderate or severe cognitive impairment, or were living in skilled nursing facilities. These groups comprise important subgroups of older patient receiving care in the ED and are likely to be at higher risk for malnutrition than the cognitively intact, non-critically ill patients included in this study. Patients were enrolled between 9 a.m. and 9 p.m. for an 8-week period in the summer from a single ED in the southeastern US. The prevalence of malnutrition may differ for patients presenting to the ED late at night and in other seasons. Although the patient population cared for in the study site ED is racially and socioeconomically diverse, our sample differed from the US population because it had a greater proportion of minorities and college educated individuals. Sociodemographics of older adults receiving emergency care in other parts of the US vary considerably, limiting the generalizability of these findings. While little is known regarding regional variation in malnutrition among older adults in the US, the Southeast has higher rates of obesity which may result in low rates of malnutrition among older adults than in other regions.41
DISCUSSION
Based on a random sample, we estimated a prevalence of malnutrition among cognitively intact, non-critically ill older adults presenting to a single southeastern academic ED over an 8-week period to be between 10% and 22%. In our sample most of the malnourished patients had not previously been diagnosed. For all of these malnourished patients, the single-item assessment of nutrition currently embedded in the triage nurse assessment either failed to identify malnutrition or was not completed. Further, no other evidence of recognition of the problem of malnutrition was found in the medical record for any of these patients. Our point estimate of the prevalence of malnutrition among older adults discharged from the ED (6%) is similar to that from community samples (5.8%);8 our estimate among admitted patients (25.4%) is lower than prior estimates from hospitalized patients (38.7%).8 We assessed malnutrition using the MNA-SF, which we found could be administered in the ED in less than 5 minutes. The most variable component of the MNA-SF is the time needed to measure height and weight. More liberal use of calf circumference measurement, a valid alternative to BMI in scoring the MNA-SF, would reduce the time to complete assessments.
Our observed trends suggest possible avenues for intervention that could be investigated in subsequent research. Higher rates of malnutrition among those reporting difficulty buying groceries suggest the value of connecting older ED patients with Supplemental Nutrition Assistance Programs (previously known as the Food Stamps Program), Meals on Wheels, Congregate Meal Programs, or community-based food charities which are often available for, but under-utilized by, older adults.42 While the study methods preclude us from inferring the presence or direction of a causal relationship between malnutrition and depression, the substantially higher observed rates of malnutrition among patients with depressive symptoms, even after removing depression from the malnutrition score, suggests that interventions targeting both malnutrition and depression may be appropriate in jointly affected individuals. More than a third of patients reporting difficulty eating were malnourished. Of the problems reported, improper fit of dentures and dental pain were the most common. The relationship between poor dental health and malnutrition among older adults has previously been described,43,44 and add to a large body of literature describing the relationship between dental problems and health outcomes.45,46 At present, Medicare does not cover preventive dental services;47 these findings suggest the need to revise Medicare to ensure access to dental care for all older adults.
In 2004, unplanned rehospitalizations cost Medicare approximately $17.4 billion, and these costs have risen further over the past decade.48 With the increasing numbers of older adults in the US, these costs will continue to rise. The growing role of the ED as a site of care and an entry point into the hospital makes it an essential place for identifying and addressing unmet needs of older adults. Implementation of oral nutritional supplementation is inexpensive and may result in overall cost savings by accelerating recovery from illness and reducing readmissions.49,50 A recent pilot study (N=19) has demonstrated the feasibility of an ED-based intervention to treat malnutrition in older adults;21 further research is needed to characterize the costs and benefits of such a program and, if helpful, develop a scalable version.
CONCLUSION
We observed a high prevalence of malnutrition among older patients presenting to an ED that was not documented in the medical record by the emergency providers or nurses caring for these patients. Our findings suggest that there may be value in ED-based screening and interventions to treat malnutrition among older adults.
Acknowledgments
Funding: This study was supported by National Institute on Aging grant K32AG038548 (Dr. Platts-Mills) and the University of North Carolina’s Summer Undergraduate Research Fellowship (Pereira)
Role of the Sponsors: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the University of North Carolina.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions: GFP and TPM conceived the study and supervised participant enrollment, data management, and data analysis. CMB provided expertise on malnutrition and helped design the questionnaire. MAW created the random block sampling scheme and assisted with data analysis. WCH assisted with the drafting of manuscript. All authors contributed substantially to the revision of the manuscript. TPM takes responsibility for the paper as a whole.
Presentations: None
REFERENCES
- 1.Salvi F, Giorgi R, Grilli A, et al. Mini Nutritional Assessment (short form) and functional decline in older patients admitted to an acute medical ward. Aging Clin Exp Res. 2008;20:322–328. doi: 10.1007/BF03324863. [DOI] [PubMed] [Google Scholar]
- 2.Cereda E, Valzolgher L, Pedrolli C. Mini nutritional assessment is a good predictor of functional status in institutionalised elderly at risk of malnutrition. Clin Nutr. 2008;27:700–705. doi: 10.1016/j.clnu.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Crogan NL, Pasvogel A. The influence of protein-calorie malnutrition on quality of life in nursing homes. The journals of gerontology Series A, Biological sciences and medical sciences. 2003;58:159–164. doi: 10.1093/gerona/58.2.m159. [DOI] [PubMed] [Google Scholar]
- 4.Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22:235–239. doi: 10.1016/s0261-5614(02)00215-7. [DOI] [PubMed] [Google Scholar]
- 5.Guigoz Y, Vellas B, Garry PJ. Mini Nutritional Assessment: a practical assessment tool for grading the nutritional state of elderly patients. In: Vellas BJ, Guigoz Y, Garry PJ, Albarede JL, editors. The mini nutritional assessment: MNA Nutrition in the elderly. Paris: Serdi Publishing Company; 1997. [Google Scholar]
- 6.Stratton RJ, Hackston A, Longmore D, et al. Malnutrition in hospital outpatients and inpatients: prevalence, concurrent validity and ease of use of the 'malnutrition universal screening tool' ('MUST') for adults. The British journal of nutrition. 2004;92:799–808. doi: 10.1079/bjn20041258. [DOI] [PubMed] [Google Scholar]
- 7.Saka B, Kaya O, Ozturk GB, Erten N, Karan MA. Malnutrition in the elderly and its relationship with other geriatric syndromes. Clin Nutr. 2010;29:745–748. doi: 10.1016/j.clnu.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Kaiser MJ, Bauer JM, Ramsch C, et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58:1734–1738. doi: 10.1111/j.1532-5415.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- 9.Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. The Cochrane database of systematic reviews. 2009 doi: 10.1002/14651858.CD003288.pub3. CD003288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson MM, Vaswani S, Liu D, Morley JE, Miller DK. Prevalence and causes of undernutrition in medical outpatients. The American journal of medicine. 1998;104:56–63. doi: 10.1016/s0002-9343(97)00279-9. [DOI] [PubMed] [Google Scholar]
- 11.Guigoz Y, Vellas BJ. Malnutrition in the elderly: the Mini Nutritional Assessment (MNA) Therapeutische Umschau Revue therapeutique. 1997;54:345–350. [PubMed] [Google Scholar]
- 12.Singh H, Watt K, Veitch R, Cantor M, Duerksen DR. Malnutrition is prevalent in hospitalized medical patients: are housestaff identifying the malnourished patient? Nutrition. 2006;22:350–354. doi: 10.1016/j.nut.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 13.Zibulewsky J. The Emergency Medical Treatment and Active Labor Act (EMTALA): what it is and what it means for physicians. Proc (Bayl Univ Med Cent) 2001;14:339–346. doi: 10.1080/08998280.2001.11927785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pane GA, Farner MC, Salness KA. Health care access problems of medically indigent emergency department walk-in patients. Ann Emerg Med. 1991;20:730–733. doi: 10.1016/s0196-0644(05)80832-7. [DOI] [PubMed] [Google Scholar]
- 15.Waller AE, Hohenhaus SM, Shah PJ, Stern EA. Development and validation of an emergency department screening and referral protocol for victims of domestic violence. Ann Emerg Med. 1996;27:754–760. doi: 10.1016/s0196-0644(96)70195-6. [DOI] [PubMed] [Google Scholar]
- 16.Rockett IR, Putnam SL, Jia H, Smith GS. Assessing substance abuse treatment need: a statewide hospital emergency department study. Ann Emerg Med. 2003;41:802–813. doi: 10.1067/mem.2003.189. [DOI] [PubMed] [Google Scholar]
- 17.Haukoos JS, Hopkins E, Conroy AA, et al. Routine opt-out rapid HIV screening and detection of HIV infection in emergency department patients. JAMA : the journal of the American Medical Association. 2010;304:284–292. doi: 10.1001/jama.2010.953. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg WG, Tomlanovich MC. Domestic violence victims in the emergency department. New findings. JAMA : the journal of the American Medical Association. 1984;251:3259–3264. [PubMed] [Google Scholar]
- 19.Carpenter C, Bromley M, Caterino JM, et al. Optimal Older Adult Emergency Care: Introducing Multidisciplinary Geriatric Emergency Department Guidelines from the American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, and Society for Academic Emergency Medicine. Academic Emergency Medicine; 2014. (In Press) [DOI] [PubMed] [Google Scholar]
- 20.Stevens TB, Richmond NL, Pereira GF, Shenvi CL, Platts-Mills TF. Prevalence of Non-Medical Problems Among Older Adults Presenting to the Emergency Department Academic Emergency Medicine. 2014 doi: 10.1111/acem.12395. (In Press) [DOI] [PubMed] [Google Scholar]
- 21.Vivanti A, Isenring E, Baumann S, et al. Emergency department malnutrition screening and support model improves outcomes in a pilot randomised controlled trial. Emerg Med J. 2013 doi: 10.1136/emermed-2013-202965. [DOI] [PubMed] [Google Scholar]
- 22.Tanabe P, Gimbel R, Yarnold PR, Adams JG. The Emergency Severity Index (version 3) 5-level triage system scores predict ED resource consumption. J Emerg Nurs. 2004;30:22–29. doi: 10.1016/j.jen.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 23.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40:771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 24.White JV, Guenter P, Jensen G, Malone A, Schofield M. Consensus statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition) J Acad Nutr Diet. 2012;112:730–738. doi: 10.1016/j.jand.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 25.Kaiser MJ, Bauer JM, Ramsch C, et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13:782–788. doi: 10.1007/s12603-009-0214-7. [DOI] [PubMed] [Google Scholar]
- 26.Serra-Prat M, Palomera M, Gomez C, et al. Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in independently living older persons: a population-based prospective study. Age Ageing. 2012;41:376–381. doi: 10.1093/ageing/afs006. [DOI] [PubMed] [Google Scholar]
- 27.Hickson M. Malnutrition and ageing. Postgrad Med J. 2006;82:2–8. doi: 10.1136/pgmj.2005.037564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wellman NS, Weddle DO, Kranz S, Brain CT. Elder insecurities: poverty, hunger, and malnutrition. J Am Diet Assoc. 1997;97:S120–S122. doi: 10.1016/s0002-8223(97)00744-x. [DOI] [PubMed] [Google Scholar]
- 29.Cabrera MA, Mesas AE, Garcia AR, de Andrade SM. Malnutrition and depression among community-dwelling elderly people. J Am Med Dir Assoc. 2007;8:582–584. doi: 10.1016/j.jamda.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 30.wolfe WS, olson CM, Kendall A, Frongillo EA. Understanding Food Insecurity in the Elderly: A Conceptual Framework. Journal of Nutrition Education. 1996;28:92–100. [Google Scholar]
- 31.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA : the journal of the American Medical Association. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 32.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 33.Irwin M, Artin KH, Oxman MN. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 34.U.S. Department of Health and Human Services. A Profile of Older Americans: 2012. [Accessed June 11, 2014]; at http://www.aoa.gov/Aging_Statistics/Profile/2012/docs/2012profile.pdf.
- 35.United States Census Bureau. Educational Attainment in the United States: 2009. [Accessed June 11, 2014];2012 at http://www.census.gov/prod/2012pubs/p20-566.pdf.
- 36.Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF) The journals of gerontology Series A, Biological sciences and medical sciences. 2001;56:M366–M372. doi: 10.1093/gerona/56.6.m366. [DOI] [PubMed] [Google Scholar]
- 37.Zadak Z, Hyspler R, Ticha A, Vlcek J. Polypharmacy and malnutrition. Curr Opin Clin Nutr Metab Care. 2013;16:50–55. doi: 10.1097/MCO.0b013e32835b612e. [DOI] [PubMed] [Google Scholar]
- 38.Bhatti GK, Howard AC, David EE. inventors; Dosage form for Parkinson's disease, spasticity and muscle spasms. USA. 1992 [Google Scholar]
- 39.Mangweth-Matzek B, Rupp CI, Hausmann A, et al. Never too old for eating disorders or body dissatisfaction: a community study of elderly women. The International journal of eating disorders. 2006;39:583–586. doi: 10.1002/eat.20327. [DOI] [PubMed] [Google Scholar]
- 40.Gagne DA, Von Holle A, Brownley KA, et al. Eating disorder symptoms and weight and shape concerns in a large web-based convenience sample of women ages 50 and above: results of the Gender and Body Image (GABI) study. The International journal of eating disorders. 2012;45:832–844. doi: 10.1002/eat.22030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and metaregression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 42.Omran ML, Morley JE. Assessment of protein energy malnutrition in older persons, part I: History, examination, body composition, and screening tools. Nutrition. 2000;16:50–63. doi: 10.1016/s0899-9007(99)00224-5. [DOI] [PubMed] [Google Scholar]
- 43.Sheiham A, Steele JG, Marcenes W, et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 2001;80:408–413. doi: 10.1177/00220345010800020201. [DOI] [PubMed] [Google Scholar]
- 44.Finch S, Doyle W, Lowe C. In: National diet and national survey People aged 65 years and over; volume 1 report of the diet and nutrition survey. Ministry of Agriculture FaF, editor. London: The Stationary Office; 1998. [Google Scholar]
- 45.Garcia RI, Krall EA, Vokonas PS. Periodontal disease and mortality from all causes in the VA Dental Longitudinal Study. Annals of periodontology / the American Academy of Periodontology. 1998;3:339–349. doi: 10.1902/annals.1998.3.1.339. [DOI] [PubMed] [Google Scholar]
- 46.DeStefano F, Anda RF, Kahn HS, Williamson DF, Russell CM. Dental disease and risk of coronary heart disease and mortality. BMJ. 1993;306:688–691. doi: 10.1136/bmj.306.6879.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Centers for Medicare & Medicaid Services. [Accessed June 20, 2014];Medicare Dental Coverage. at http://cms.hhs.gov/Medicare/Coverage/MedicareDentalCoverage/index.html. [PubMed]
- 48.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 49.Stratton RJ, Hebuterne X, Elia M. A systematic review and meta-analysis of the impact of oral nutritional supplements on hospital readmissions. Ageing Res Rev. 2013;12:884–897. doi: 10.1016/j.arr.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 50.Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012;11:278–296. doi: 10.1016/j.arr.2011.12.008. [DOI] [PubMed] [Google Scholar]