Abstract
Levamisole is an immunomodulatory and antihelminthic drug, previously removed from the United States market, and now estimated to be present in the vast majority of cocaine distributed in the United States. Levamisole-adulterated cocaine (LAC) exposure can result in neutropenia, thrombocytopenia, and vasculitis with a predilection for subsites of the face. The objective of this review is to increase awareness among otolaryngologists of the manifestations of LAC exposure. We present the case of a 33-year-old woman with a history of cocaine use, consulted for purpuric, necrotic lesions of the nose, cheeks, and ears, with accompanying leukopenia, thrombocytopenia, and positive antineutrophil cytoplasmic antibodies (ANCA). The effects of levamisole are immune mediated, with antibodies directed against neutrophils causing neutropenia, and vasculitis caused by antibody deposition or secondary to induction of antiphospholipid antibodies causing thrombosis. LAC exposure can be differentiated from other similar appearing pathologies by evaluating serology for specific ANCA. The most important treatment is cessation of cocaine use, which most often results in complete resolution of symptoms. Awareness of the presentation, complications, and treatment of LAC exposure may be especially important for otolaryngologists, who may be one of the firsts to evaluate an affected patient.
Keywords: Levamisole, levamisole-adulterated cocaine, vasculitis, thrombotic vasculopathy, immunomodulatory, purpura, skin necrosis
Levamisole is a synthetic imidazothiazole derivative with antihelminthic and immunomodulatory properties. In the United States, it is currently used primarily as an antihelminthic drug in veterinary medicine. Levamisole was used in the past to treat inflammatory conditions such as rheumatoid arthritis, Crohn's disease, and nephrotic syndrome. It also played a role in the treatment of malignancies, such as leukemia, and as an adjuvant therapy to 5-fluorouracil for colorectal cancer. Levamisole was discontinued for human use in the United States in 2000 due to side effects, most notably neutropenia, agranulocytosis, and vasculitis. Additional less common side effects include multifocal leukoencephalopathy, arthritis, type I and III hypersensitivity reactions, ulcers of the mouth and skin, and gastrointestinal symptoms.1–3
Currently, exposure to levamisole occurs most commonly with cocaine use. It is estimated that approximately 70%–88% of cocaine is contaminated with levamisole and that around 20 million people a year are using cocaine, making levamisole-adulterated cocaine (LAC) a significant public health issue.1,4 In addition to its immunomodulatory and antihelminthic effects, levamisole also has mood stimulatory effects through a few possible mechanisms. Levamisole may enhance noradrenergic transmission and augment sympathomimetic effects of cocaine by inhibiting reuptake of norepinephrine, by inhibiting monoamine oxidase and/or catechol-o-methyl transferase, by acting on postganglionic nicotinic receptors, and by being partially metabolized into an amphetamine-like compound. It could also inhibit acetylcholinesterase activity, increase endogenous opioids, and increase dopamine concentration in the cerebral reward pathway.1,3
With ingestion of LAC, patients often present with a tender, purpuric rash in a retiform distribution with erythematous borders and necrotic centers. Lesions have a predilection for the lower extremities, ears, and malar regions of the cheeks, with pathologic specimens showing a pure thrombotic vasculopathy, small vessel vasculitis, or a combination of both. Laboratory investigations often reveal neutropenia, high-titer antineutrophil cytoplasmic antibodies (ANCA), and evidence of hypercoagulability with positive antiphospholipid antibodies.1,5–7 Our patient presented with painful skin lesions on the face and bilateral upper and lower extremities, thrombocytopenia, leukopenia, positive ANCA, and a hospital course complicated by bacteremia secondary to pyelonephritis.
CASE PRESENTATION
A 33-year-old woman presented to the emergency department complaining of painful skin lesions on her cheeks, nose, back, and bilateral upper and lower extremities that had been developing for the past week. She admitted to recent heroin and cocaine use. The patient reported smoking cocaine obtained from her normal supplier twice in the week before admission, most recently the day before admission. She also reported fever, chills, nausea, decreased appetite, nonproductive cough, chest tightness, and loose stools but denied chest pain, vomiting, trauma, and dysuria. Physical exam revealed ecchymotic lesions on the malar eminences (left greater than right) and on the nasal tip, supratip, nasal ala, nasal sill, and columella (Fig. 1). Nasal mucosa was erythematous and edematous with left septal deviation and left anterior septal mucosa excoriation without perforation. Purpuric and ecchymotic lesions were also noted on the left scapular region, right triceps region (Fig. 2), and bilateral lower extremities. The patient had a past medical history significant for previous episodes of levamisole-induced skin necrosis and reported prostitution as her source of income. In the emergency department, she was started on 60-mg oral prednisone for her skin lesions before being admitted.
Figure 1.
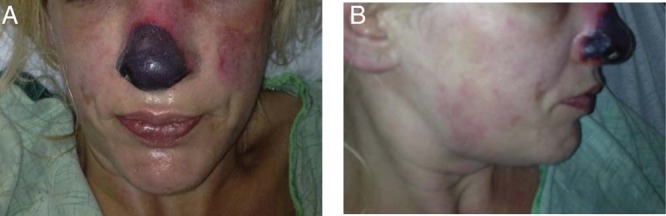
Necrotic lesion of the nose and ecchymotic lesions of the malar eminences.
Figure 2.

Solid purpuric patch of the lateral right arm, necrotic lesion of the nose, and retiform purpuric patches of the medial left arm.
Initial laboratory investigations revealed thrombocytopenia with a platelet count of 125,000 per mm3 and a white blood cell count within normal limits at 4100 per mm3. Absolute neutrophil count was 2600 per mm3. Antinuclear antibodies were weakly positive with a titer of 1:80, and ANCA were positive with a titer of 1:1280. Antimyeloperoxidase antibodies (anti-MPO) were within normal limits, and antiserine protease 3 antibodies (anti-PR3) were elevated at 31 (0–20). Hepatitis B core antibodies were positive, and HIV antibodies were negative. Gas chromatography mass spectrometry analysis was positive for cocaine, levamisole, and nicotine. Toxicology screen was positive for cocaine and opiates. Urinalysis was suggestive of a urinary tract infection, and blood culture was positive for Escherichia coli.
On the second day of admission the patient was started on cefepime, had fevers with a max temperature of 38.7°C, and was tachypneic. She also had an episode of hypotension and elevated lactic acid, which improved after a two liter bolus of normal saline. Her skin lesions appeared lighter, except for lesions on the right triceps and nasal area, which appeared necrotic. She was continued on 50-mg oral prednisone.
Over the course of the rest of her hospital stay, the patient developed additional necrotic lesions on the left helix (Fig. 3), right anterior thigh, and left triceps region. Using a recently proposed staging system for delineating the severity of levamisole-induced vasculopathy dependent on the confluency of purpura and degree of skin necrosis,8 our patient had lesions ranging from mild (stage I) to severe (stage III). Lesions of the malar regions were stage I, lesions of the helix were stage II (moderate), and lesions of the nose and right triceps were stage III. Her platelet count decreased to 74,000 per mm3, and her white blood cell decreased to 3400 per mm3. Her antibiotics were switched from cefepime to ceftriaxone once sensitivities were available. The patient was discharged on hospital day five on 20-mg oral prednisone for 10 days and oral ciprofloxacin after improvement of her skin lesions and multiple negative blood cultures. She returned to the emergency department four weeks later after continued cocaine use and autoamputation of the tip of her nose.
Figure 3.

Purpuric patches of the left ear.
DISCUSSION
The first case reports of complications related to levamisole exposure in cocaine users were published in 2009.1 Before that, most knowledge of levamisole came from its use in treating autoimmune conditions and cancers. The exact mechanism by which levamisole affects the immune system is unclear, but it might increase neutrophil chemotaxis and activity, enhance T-cell immune responses, stimulate antibody production, up-regulate Toll-like receptors, or regulate other cytokine and intracellular signaling networks.2,3,7,9
Levamisole is no longer available for human use due to side effects, most notably neutropenia, agranulocytosis, and vasculitis. It is still used in veterinary medicine for its antihelminthic properties, which are due to agonistic actions on species-specific nicotinic acetylcholine like receptors on the muscle cells of nematodes. Currently, levamisole is only available in the United States for antihelminthic use in veterinary medicine, although other more efficacious antihelminthics are available, creating the possibility that the use of levamisole could be eliminated entirely.10
There appear to be three syndromes associated with LAC exposure: cocaine-induced midline destructive lesion (CIMDL), cutaneous vasculopathy, and agranulocytosis. Characteristic serology can help distinguish these syndromes from each other and from other pathologies that would be part of the differential diagnosis. There are specific patterns of ANCA: cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA) are almost exclusively a result of antibodies against PR3, whereas perinuclear antineutrophil cytoplasmic antibodies (p-ANCA) may target multiple different neutrophil granule components, including MPO, human neutrophil elastase (HNE), and PR3.1
Hard palate perforation is pathognomonic for CIMDL. Characteristic serology for CIMDL is p-ANCA with anti-HNE, anti-PR3, and absence of anti-MPO.1,11 CIMDL is distinct from vasculopathy associated with LAC and is thought to be from vasoconstrictive effects of cocaine, whereas vasculopathy associated with LAC is thought to be related to immune effects.2,3
Cutaneous vasculopathy associated with levamisole presents with a painful, dusky purple rash with erythematous borders and necrotic centers in a netlike, stellate, or angular configuration. Lesions are most common on the lower extremities, face, and ears. Biopsies show leukocytoclastic vasculitis, occlusive thrombotic vasculopathy, or vasculitis with thrombosis. This particular vasculopathy is thought to be due to immune complex deposition or antiphospholipid antibodies causing hypercoagulability leading to tissue thrombosis and skin necrosis.2,3,11
Patients with agranulocytosis associated with levamisole exposure have positive antineutrophil antibodies. Serology with levamisole is more complex than with cocaine. With levamisole, p-ANCA are more common than c-ANCA, but either can be present. Anti-PR3, anti-MPO, and anti-HNE may all be present.1,11 Anti-MPO with anti-HNE distinguishes levamisole pathology from CIMDL. Anti-HNE may be present with CIMDL and after LAC but is specific for CIMDL when anti-MPO is absent. With CIMDL, other autoantibodies, such as antinuclear antibodies or antiphospholipid antibodies, are less likely to be present.2,7
Other pathologies to consider in a patient presenting with a tender, purpuric rash characteristic of LAC exposure include autoimmune connective tissue disorders, Wegener's granulomatosis, microscopic polyangiitis, idiopathic thrombocytopenic purpura, cryoglobulinemia, and warfarin or heparin-induced skin necrosis.1,2,12 Serology can distinguish some of these. Wegener's granulomatosis typically presents with c-ANCA directed against PR3, and microscopic polyangiitis typically displays a pattern of p-ANCA targeting MPO.1
Testing for levamisole directly can be difficult, because levamisole has a half-life of approximately 5.6 hours, and testing is not available through routine toxicology screening.4 In conjunction with the characteristic clinical presentation, this had led some authors to conclude that a positive test for levamisole is not a necessary component of the diagnosis of LAC-induced cutaneous vasculitis.4,7,13 Notably, our patient did test positive for levamisole on gas chromatography mass spectrometry, providing further evidence for the attribution of her symptomatology to levamisole exposure.
Expression of human leukocyte antigen B27 (HLA B27) has been proposed as a risk factor for development of complications after exposure to LAC.2,7,9,11 Patients with an HLA B27 genotype are more susceptible to agranulocytosis after drug exposure, including exposure to levamisole.6 This process may be either multifactorial or dose dependent, because many cases of leukopenia and agranulocytosis have been observed in patients lacking HLA B27.1,2 Additionally, it has been proposed that levamisole in combination with an HLA genotype may induce autoantibody formation, increase metabolism of levamisole to a thiazole derivative, or cause an immune-mediated delayed type hypersensitivity reaction, where levamisole or its metabolites form a hapten with a self-antigen and induce T-cell activation.14 Due to its immunomodulatory effects, levamisole may also unmask an autoimmune disease.5,13
The route of cocaine ingestion does not appear to play a role in the development of LAC-induced pathology. In a review that included information about the route of administration of cocaine in 81 patients with complications secondary to LAC, 35 had snorted it and 41 had smoked it, although specific symptoms experienced by each group were not delineated.1 Further investigations may reveal whether LAC ingested through one route versus another induces a higher frequency of cutaneous, hematologic, or other complications.
The most important treatment of LAC dermatologic or hematologic manifestations is cessation of cocaine use.1,15 Steroids are commonly used as treatment; one review reported treatment with steroids in over 50% of patients, but it is unclear whether or not they are beneficial. Steroids should be used with caution due to the increased susceptibility of infection and other systemic side effects.5 Other therapies include granulocyte colony-stimulating factor, nonsteroidal antiinflammatory drugs, and colchicine.3 Granulocyte colony-stimulating factor should be used for agranulocytosis in patients with evidence of an infection or with an immune compromising condition.2,11 Phentolamine has also been injected into lesions in a case of bilateral ear necrosis, with no improvement.16 The majority of patients with LAC skin lesions heal after cessation of cocaine use without sequelae, but for some, wound care may be important. Necrotic tissue may need to debrided, skin grafts may be needed, and amputation may be required. Consideration of the healing of a surgical site is also important when planning reconstruction.14
Our patient had a clinical course complicated by infection and the eventual autoamputation of the tip of her nose, which is unlike the typical clinical scenario where lesions heal without any permanent damage. This has been reported with other patients, most commonly those with infections. One patient who presented with bullae, diffuse purpura with necrotic centers, and streptococcal toxic shock syndrome ended up requiring several appendage amputations.3 Another patient with septicemia had levamisole-induced necrosis of the skin, soft tissue, and cartilage resulting in nasal amputation, earlobe necrosis, and bilateral above knee amputations.1 Because of potential agranulocytosis, patients with LAC can present with fulminate and opportunistic infections. Many patients with infections have lesions that heal without sequelae, but septicemia or pressors used in treatment may contribute to the pathology.3,10,17
CONCLUSION
Reports of complications related to LAC exposure have been increasing but are difficult to diagnose because of the variability in clinical manifestations. Clinicians should be suspicious of levamisole ingestion in patients with purpuric or necrotic lesions who admit to illicit drug use. Diagnosis is important so that cessation of cocaine use can be stressed to the patient, to prevent the use of other unnecessary and potentially harmful treatments such as immunosuppressive therapy, and to monitor for potentially dangerous and disfiguring complications, including agranulocytosis, infections secondary to agranulocytosis, and skin necrosis that may require surgical intervention.
Footnotes
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Larocque A, Hoffman RS. Levamisole in cocaine: unexpected news from an old acquaintance. Clin Toxicol (Phila) 50:231–241, 2012. [DOI] [PubMed] [Google Scholar]
- 2. Magliocca KR, Coker NA, Parker SR. The head, neck, and systemic manifestations of levamisole-adulterated cocaine use. J Oral Maxillofac Surg 71:487–492, 2013. [DOI] [PubMed] [Google Scholar]
- 3. Freyer CW, Peters M. Palpable purpura complicated by streptococcal toxic shock syndrome resulting in limb necrosis and amputation: a case of levamisole and cocaine coingestion. Pharmacotherapy 32:e17–e23, 2012. [DOI] [PubMed] [Google Scholar]
- 4. Tran H, Tan D, Marnejon TP. Cutaneous vasculopathy associated with levamisole-adulterated cocaine. Clin Med Res 11:26–30, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Arora NP. Cutaneous vasculopathy and neutropenia associated with levamisole-adulterated cocaine. Am J Med Sci 345:45–51, 2013. [DOI] [PubMed] [Google Scholar]
- 6. de la Hera I, Sanz V, Cullen D, et al. Necrosis of ears after use of cocaine probably adulterated with levamisole. Dermatology 223:25–28, 2011. [DOI] [PubMed] [Google Scholar]
- 7. Ullrich K, Koval R, Koval E, et al. Five consecutive cases of a cutaneous vasculopathy in users of levamisole-adulterated cocaine. J Clin Rheumatol 17:193–196, 2011. [DOI] [PubMed] [Google Scholar]
- 8. Gillis JA, Green P, Williams J. Levamisole-induced vasculopathy: staging and management. J Plast Reconstr Aesthet Surg 67:e29–e31, 2014. [DOI] [PubMed] [Google Scholar]
- 9. Lee KC, Ladizinski B, Federman DG. Complications associated with use of levamisole-contaminated cocaine: an emerging public health challenge. Mayo Clin Proc 87:581–586, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arora NP, Jain T, Bhanot R, Natesan SK. Levamisole-induced leukocytoclastic vasculitis and neutropenia in a patient with cocaine use: an extensive case with necrosis of skin, soft tissue, and cartilage. Addict Sci Clin Pract 7:19, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Specks U. The growing complexity of the pathology associated with cocaine use. J Clin Rheumatol 17:167–168, 2011. [DOI] [PubMed] [Google Scholar]
- 12. Chung C, Tumeh PC, Birnbaum R, et al. Characteristic purpura of the ears, vasculitis, and neutropenia–a potential public health epidemic associated with levamisole-adulterated cocaine. J Am Acad Dermatol 65:722–725, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gross RL, Brucker J, Bahce-Altuntas A, et al. A novel cutaneous vasculitis syndrome induced by levamisole-contaminated cocaine. Clin Rheumatol 30:1385–1392, 2011. [DOI] [PubMed] [Google Scholar]
- 14. Belfonte CD, Shanmugam VK, Kieffer N, et al. Levamisole-induced occlusive necrotising vasculitis in cocaine abusers: an unusual cause of skin necrosis and neutropenia. Int Wound J 10:590–596, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Poon SH, Baliog CR, Jr, Sams RN, et al. Syndrome of cocaine-levamisole-induced cutaneous vasculitis and immune-mediated leukopenia. Semin Arthritis Rheum 41:434–444, 2011. [DOI] [PubMed] [Google Scholar]
- 16. Buchanan JA, Vogel JA, Eberhardt AM. Levamisole-induced occlusive necrotizing vasculitis of the ears after use of cocaine contaminated with levamisole. J Med Toxicol 7:83–84, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Muirhead TT, Eide MJ. Images in clinical medicine. Toxic effects of levamisole in a cocaine user. N Engl J Med 364:e52, 2011. [DOI] [PubMed] [Google Scholar]


