Abstract
Introduction and Objectives:
Health system reforms are the most strategic issue that has been seriously considered in healthcare systems in order to reduce costs and increase efficiency and effectiveness. The costs of health system finance in our country, lack of universal coverage in health insurance, and related issues necessitate reforms in our health system financing. The aim of this research was to prepare a structure of framework for social health insurance in Iran and conducting a comparative study in selected countries with social health insurance.
Materials and Methods:
This comparative descriptive study was conducted in three phases. The first phase of the study examined the structure of health social insurance in four countries – Germany, South Korea, Egypt, and Australia. The second phase was to develop an initial model, which was designed to determine the shared and distinguishing points of the investigated structures, for health insurance in Iran. The third phase was to validate the final research model. The developed model by the Delphi method was given to 20 professionals in financing of the health system, health economics and management of healthcare services. Their comments were collected in two stages and its validity was confirmed.
Findings:
The study of the structure of health insurance in the selected countries shows that health social insurance in different countries have different structures. Based on the findings of the present study, the current situation of the health system, and the conducted surveys, the following framework is suitable for the health social insurance system in Iran. The Health Social Insurance Organization has a unique service by having five funds of governmental employees, companies and NGOs, self-insured, villagers, and others, which serves as a nongovernmental organization under the supervision of public law and by decision- and policy-making of the Health Insurance Supreme Council. Membership in this organization is based on the nationality or residence, which the insured by paying the insurance premiums within 6-10% of their income and employment status, are entitled to use the services. Providing services to the insured are performed by indirect forms. Payments to the service providers for the fee of inpatient and outpatient services are conservative and the related diagnostic groups system.
Conclusions:
Paying attention to the importance of modification of the fragmented health insurance system and financing the country's healthcare can reduce much of the failure of the health system, including the access of the public to health services. The countries according to the degree of development, governmental, and private insurance companies and existing rules must use the appropriate structure, comprehensive approach to the structure, and financing of the health social insurance on the investigated basis and careful attention to the intersections and differentiation. Studied structures, using them in the proposed approach and taking advantages of the perspectives of different beneficiaries about discussed topics can be important and efficient in order to achieve the goals of the health social insurance.
Keywords: Health insurance, health insurance structure, insurance, selected countries
INTRODUCTION
Structure and financing system of health insurance is a very important component of a health system. The mechanisms, which transfer and organize money for financing the health sector activities and the mechanisms of how to use this money, are very essential for the efficient and effective allocation.[1] Financing has a significant impact on the followings: Performance of the health system, determining the amount of inventory of money, who will bear the financial burden?, who controls the funds?, how the risks will be cumulative?, is it possible to control the cost of healthcare?, direct and indirect effects on the two main objectives of health systems, equitable financing system and meeting the expectations of other people.[2] The goal of an efficient financial system is typically providing adequate resources for the access of people to healthcare services and personal care. Therefore, the people due to the inability for payment would not be denied in accessing to health services or would not be driven to poverty due to health costs.[3] Meanwhile, we can say that the issue is the fundamental philosophy in the existence of healthcare services insurance. Due to the mentioned content, the most effective mechanism, which can be against the diseases and threatening factors for the human health and ensuring the safety of all members of society is the public health insurance system.[4] Health insurances with bilateral performance in the realm of health and social welfare have had an important role. They are known as the tool of governance and accountability in the healthcare system.[5] Therefore, in terms of changing pattern of diseases, emerging diseases, providing equality and accessing to healthcare and justice in the distribution of the financial burden of healthcare costs will be achieved only with the establishment of adequate, comprehensive, and integrity of health insurance.[6] The other benefits of health insurance are: Strengthening and mobilizing financial resources from low to higher priority sectors of health, treatment and social security, reducing the overhead costs, and controlling the growth of healthcare costs.[7] Futurism, based on scientific basis, is an indicator and a necessity in both developed and developing societies. In a society, that feels this need should link the present to the future by using the updated ideas and knowledge with safe and reliable infrastructure.[8] The insurance will cause the development and growth process to move efficiently and safely. Anyhow, it is better for health insurance to be associated with the correct programs and using applied economics and management professionals. The method of organizing the insurance is more important, because, the correct structure by the precise definition of outsourcing relationships will lead to the stability and survival of the insurance organization. In our country, the need to establish a social security institution has been felt for years and the social security organization was established with the main activity of covering the population of the society. Nevertheless, there is a huge gap between the current arrangements of this organization in the country and the philosophy of social health insurance. There are several people who do not have sufficient knowledge of the activities of the social insurance.[9] Thus, only on the interaction of this, they cannot benefit from the advantages and services efficiently. In contrast, large numbers of people are not covered by any insurance yet and are positioned at a low level in terms of economic and social welfare.[10] Lack of separate funding and provision of services in the Ministry of Health and social security organizations comparing with current trends in many developed and developing countries conflict and undermine the performance.[11] In addition to the raised points about the weaknesses in financing of the health system of the country, existence of various health insurance funds with different rules and regulations has caused significant problems and challenges. The most important issue in this regard is the lack of social justice, which specifically means a lack of equity in health.[10] Despite such challenges, the need for reform in this area and theoretical and practical efforts in this regard are discussed. The most important policy initiatives in this area are the laws relating to health insurance in the fifth development plan of the country. However, so far, needed actions have not been implemented in this area. In this regard, there is a need to develop a model to organize the state of financing in health insurance and preventing the loss of capital in the country. Therefore, in addition to reducing the challenges in the health insurance, it will be possible to access to health promotion and customer satisfaction, which is the ultimate goal and philosophy of the healthcare system. Due to this fact that the employed approaches for reform in different countries were not always successful and for accessing to the health system reform, we cannot follow a specific formula or even regional. Therefore, it should be noted that history, capacity, values, and the national culture with enough information and the right tools are essential to design the modifications.[12] The present study has been developed in this direction, in line with the Health Insurance Law and research priorities of the Ministry of Health based on increasing quality and quantity of health insurance. First, social health insurance structure is described and analyzed in selected countries. Finally, by studying the experiences of the selected countries and using the Delphi technique, a suitable model has been suggested for the health and social insurance in Iran.
MATERIALS AND METHODS
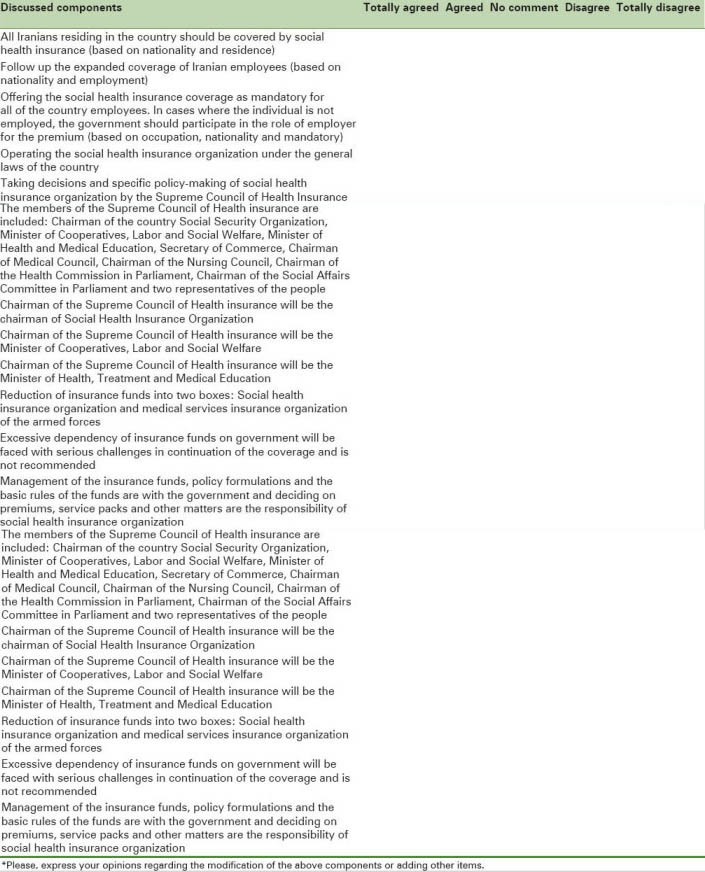
This study was an applied research, which examined the structures of social health insurance in the selected countries as a descriptive-adaptive study in 2011-2012. The study population in the section of the comparative study consisted of the selected countries: Germany, Australia, South Korea, and Egypt. The countries were selected based on the fact that these countries have been able to perform the social health insurance systems successfully. Therefore, the effective use of their positive experiences can be helpful. The mentioned combination was from developed and developing countries. The availability of the needed information in these countries was more in comparison with other countries. The participants in the survey proposed model were experts in the fields of financing the health system, insurance, health insurance, health economics, and healthcare services management. The subjects were classified into three groups. The first group consisted of university professors due to their impartial judicial views and a deep insight into the subject of the study. The second group employed individuals in healthcare organizations and the third group included the employees of the governmental healthcare organizations and policy-making in the country. In this study, the social health insurance structure was evaluated at four bases including: Management and organization of social health insurance, financial flows, purchase services, and its position in the health system. In order to collect data in the first phase of the study, the followings were used as a base of reliable information: Valid informing databases, reference textbooks, World Health Organization published reports, databases of Medline, Elsevier, and Pop Med, and electronic correspondence with people who were aware of the case in the studied countries. Adaptive tables were used for data analysis in the second phase of the study. Then, the initial model was designed by using the common and differentiation points included in the comparative tables for the structure of social health insurance in Iran. Delphi method was used to determine its validity. In the third phase of the study, the basic pattern in the form of questionnaires describing all of the components was distributed among 20 professionals in this field and they were asked to state whether they agree or disagree to the above mentioned aspects. Based on the Likert scale, the option of open answers was also considered for them. The components rated less than 50% agree or completely agree were rejected and other components with their mean scores were entered into the second round of the Delphi questionnaire. Finally, the significant components in the second round of Delphi were listed in the final model.
Findings
This study has examined the four-basis structure of social health insurance. In this section, first, the findings from a comparative study would be provided, and then, the extracted patterns from the perspective of experts will be discussed.
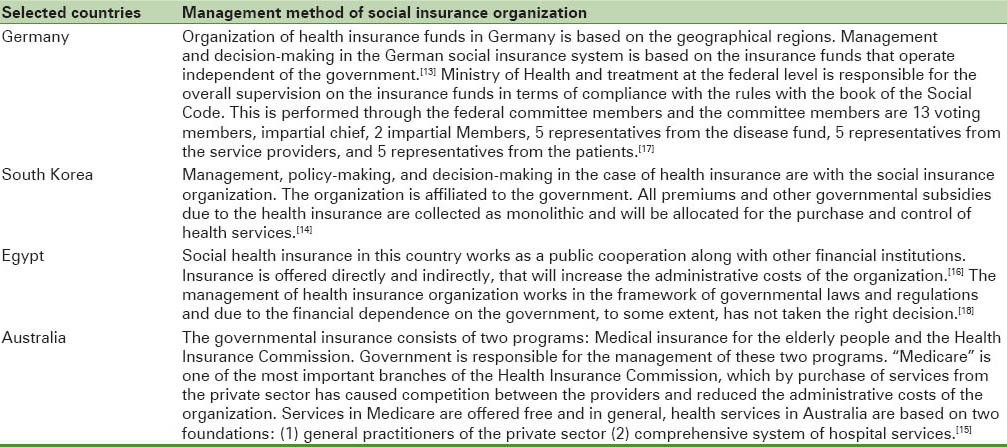
Management method of social health insurance
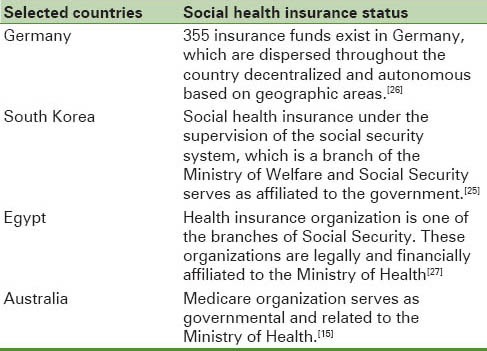
One of the features of social health insurance system is its governmental management, the same as in Germany.[13] In Korea and Australia, it is governmental and in Egypt, due to financial dependence on the government, it is semi-governmental.[14,15,16] Department of Health Insurance in Australia as governmental consists of two programs: The elderly health insurance, which offers the health and hospital services, and Health Insurance Commission, which is responsible for providing medical care [Table 1].[15]
Table 1.
Method of social health insurance organization management in selected countries
Financial flows of social health insurance organization
State-funded of healthcare system through taxes, social insurance, governmental subsidies, private insurance, paid out of pocket by patients, and method of financial flows in social health insurance organization are summarized in Tables 2 and 3.[18,19,20,21,22]
Table 2.
Financing of the healthcare system through the taxes, social insurance, governmental subsidies, private insurance, and paid out of pocket by patients
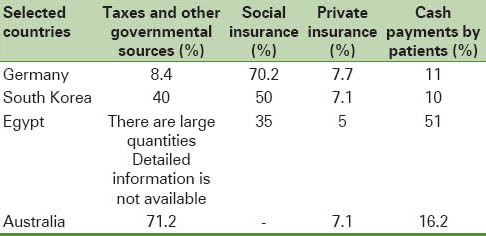
Table 3.
Financial flows in social health insurance organization in selected countries
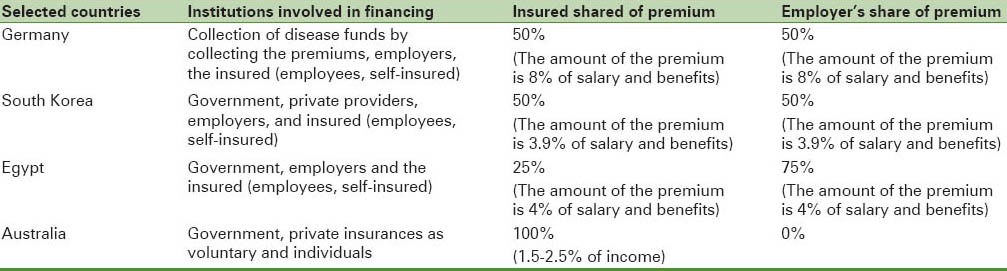
Policies of purchasing the services
Insurance funds in Germany contract with the service providers in three levels in order to provide healthcare services to the insured, outpatient care, secondary, and social healthcare.[19] Service providing in South Korea is consisted of three levels: First, second, and the third.[23,25] In Australia, it is performed through referral system in both primary and secondary healthcare [Table 4].[15]
Table 4.
Policies of purchasing services in social health insurance organization in selected countries
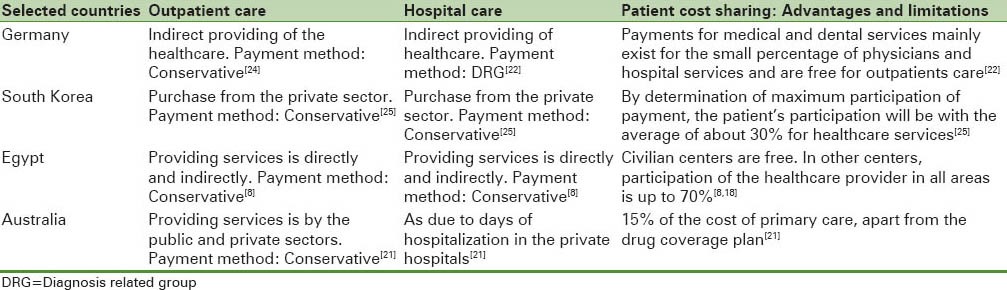
Social health insurance status
The number, variety, and connections of health insurance organizations in the surveyed countries are different. Meanwhile, 355 insurance funds are scattered throughout Germany as autonomous based on geographical areas.[26] Health insurance organization in South Korea serves as a unit under the supervision of social insurance.[25] In Egypt, social health insurance serves as public cooperative alongside other methods of financing[27] [Table 5].
Table 5.
Social health insurance status in selected countries
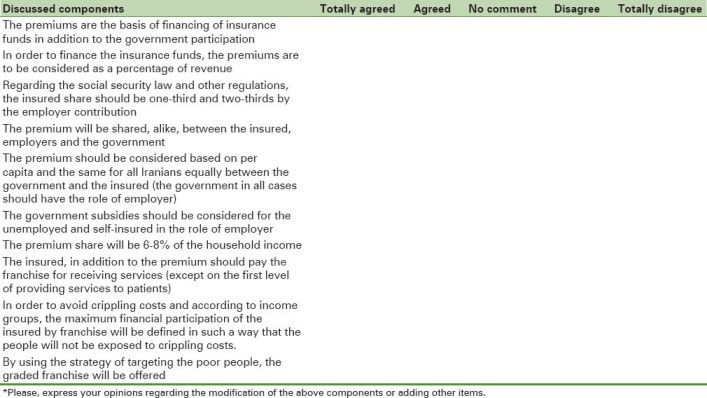
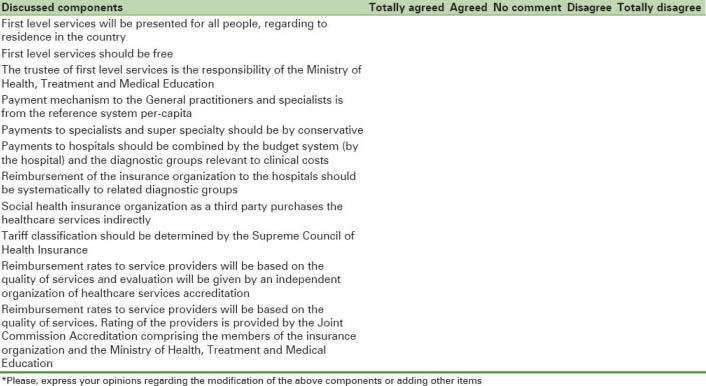
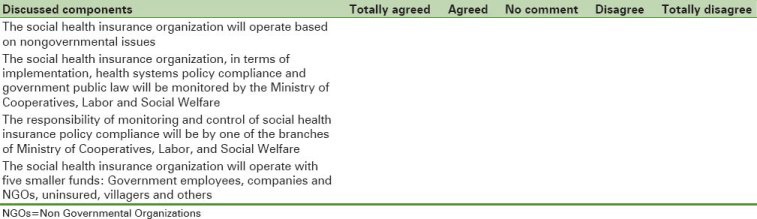
The final model derived from expert opinions in Delphi technique
As mentioned in the “Methods” section of the study, the information related to investigations and studies, which were obtained about the integration of health insurance by using the questionnaires were given to the professionals and experts. In this section, the final model derived from the survey is presented [Table 6 and Figure 1].
Table 6.
Final model of social health insurance structure for Iran has been extracted from the perspectives of the experts in the Delphi Technique
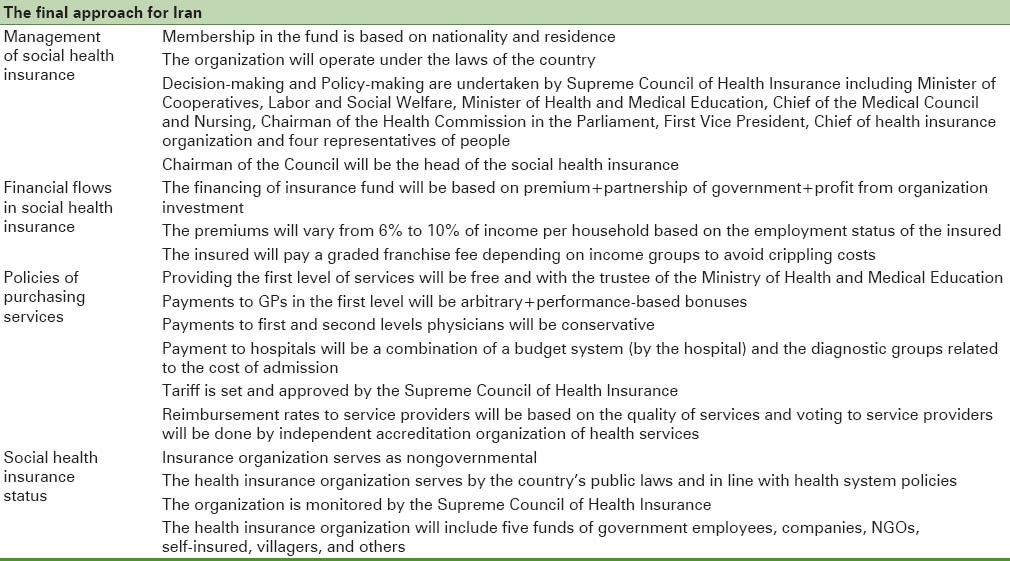
Figure 1.
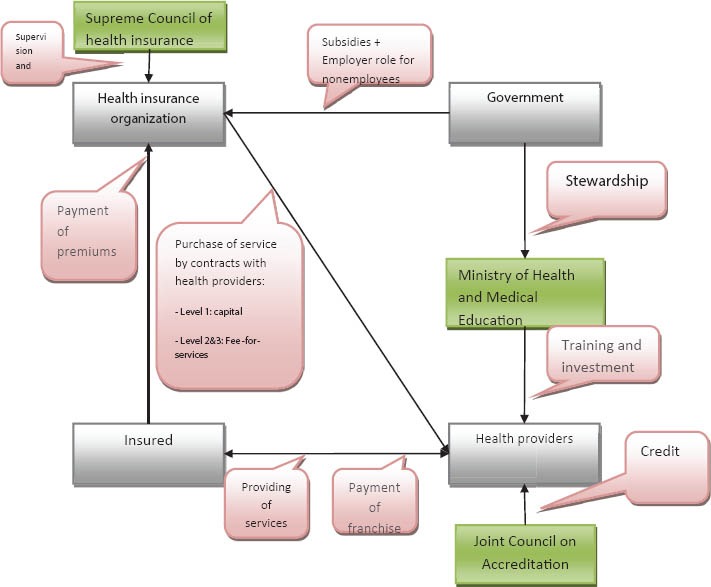
Schematic view of the final model for the social health insurance structure in Iran derived from expert perspectives by the Delphi technique
DISCUSSION AND CONCLUSION
One of the most important Millennium Development Goals is poverty reduction. World Health Organization introduces the social health insurance as an effective strategy for reducing financial barriers in access to health. For this purpose, in many countries, this method of financing has helped considerably to overcome the poverty trap of diseases, improving the quality and quantity of health, creating incentives for economic activity and growth in the health sector.[28] The World Health Organization reports show that health status, satisfaction and accountability, waiting time and equity of financing in countries with social health insurance systems are significantly better than other forms of health financing in countries with tax-based system.[29] The article of “social health insurance in comparison with system of financing based on taxes”, which was conducted in the Organization for Economic Cooperation and Development (OECD) countries, examined the differences between the two systems. The findings stated that social health insurance per capita in comparison with the tax increased about 3-4%. Employee participation has declined voluntarily from 8% to 10% and there was no significant difference observed in the social health insurance in other cases compared with tax.[30] “Health insurance reform in Vietnam; Reviewing recent developments and future challenges” was an article that was studied in 2008 in order to evaluate new health system of financing. This study provided three factors of financial stability, services performance and equity in health financing and knew the result of social health insurance in the country.[31] Several studies have confirmed necessary reforms in health financing system in Iran. Among these studies, the article of Alireza Vafaei can be entitled as health insurance. This article stated that the heaviness of an insurance structure with performing unnecessary parallel actions and inevitable increase in implementing and running costs would be a major loss. This leads in preventing scientific and practical development in an efficient healthcare insurance industry and wasting the limited current resources.[32] Moghadasi et al., in their study, stated that the biggest challenge to the country's health insurance system is to overcome the existing problems in the path of health insurance integration. These problems can be classified such as dimensions of policy-making, laws and regulations, organizational structure, and financing.[33] The Eqbali article entitled “The structure of health insurance” stated that in many countries, due to management insecurity and unstable governments, the allocated resources by the governments do not have continuity.[34] Nongovernmental social insurance confirms the health in the provided model. Perhaps the most important result of the idea of being autonomous of social health insurance system is that such systems appear to be stable, especially in terms of organization and financing. In fact, by considering the chaos in Western Europe and the number of imposed governmental new systems in France and Germany cannot exceed the stability and survival of social health insurance system. Taiwan's experience in integrating the insurance funds entitled as National Health Insurance and the coverage of 96%[35] is consistent with the unity of Social Insurance Organization in the proposed structure. This feature can reduce many of the administrative and management costs. Lessons and doctrines drawn from the study of “180 years of German health insurance and comparing with low-income and middle-income countries”[17] could be the provided solutions in the proposed model. In the section about the management of social health insurance and method of receiving the premiums, it has been shown that different kinds of financing practices are used in different countries. Countries according to their degree of development, public and private insurance companies, and current laws use the appropriate structure of a comprehensive approach to the health and social insurance in the four-basis: Management, cash flow, purchasing policies, and insurance status. Careful attention to the intersection and differentiation points of insurance structures of the studied countries, their usage from the proposed model and enjoying the viewpoints of various beneficiaries in this study are the strength points of this study. The limitations of this research were the lack of access to information and statistics of developing countries. For instance, some statistics related to the study variables were hardly collected and took a long time. Lack of easy access to some of the participants in the survey, the difficulty of justifying the insurance authorities in explaining the research title, method of cooperation, and their late feedback were other limitations of the present study.
In order to create public coverage and implementation of social health insurance system, conducting the following studies are suggested
Review of barriers to implementation of an integrated health insurance and lack of enforcement of laws in the country
More detailed investigation to determine premiums and the insured franchise
Clarification of the relationship between insurance organization, service providers and government
Supplementary studies in the four-reviewed basis in this study more specifically.
APPENDICES
Delphi technique questionnaires
Basis 1.
How to manage Social health insurance Organization
Basis 2.
Method of financial flow in Social health insurance Organization
Basis 3.
Method of purchasing the services of Social health insurance Organization
Basis 4.
The position and status of Social health insurance Organization
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Marks RC, Rich MW. “Health Care Reform: A Guide to Equity and Efficiency.” Translated: Ahmadv AR, and Tofighy. Sh Ibn Sina Largest Publisher of Scientific and Cultural Institutions. Printing. SUMMER 1384. :297–71. [Google Scholar]
- 2.Normand C, Weber A. Geneva: World Health Organization/ILO; 1994. Social health insurance: A guidebook for planning. [Google Scholar]
- 3.Knaul F, Arreola-Ornelas H, Mendez O, Martínez A. Fair health financing and catastrophic health expenditures: Potential impact of the coverage extension of the popular health insurance in Mexico. Salud publica de Mexico. 47(2005):S54–65. [PubMed] [Google Scholar]
- 4.Social health insurance: A contribution to the international development policy debate universal systems of social protection. Federal Ministry for Economic Cooperation and Development. 2005 Nov [Google Scholar]
- 5.Carrin G, James C. Social health insurance: Key factors affecting the transition towards universal coverage. Int Soc Secur Rev. 2005;58:45–64. [Google Scholar]
- 6.Chisholm D, Evans DB. Improving health system efficiency as a means of moving towards universal coverage. World Health Report 2010 background paper, no. 28. [Last accessed on 2012 Jan 04]. Available from: http://www.who.int/healthsystems/topics/financing/healthreport/whr_background/en .
- 7.Principles of Management and the Social Security system. Social Security Research Institute, Tehran. :1376. [Google Scholar]
- 8.WHO, 2000. Geneva: World Health Organization; 2000. World Health Report 2000-Health Systems: Improving Performance. [Google Scholar]
- 9.Mohammed A, Hosseini R. The health insurance system. Jihad in Tehran University Publications. Printing. Winter. :1389. [Google Scholar]
- 10.Hajizadeh, Mohammad Healthy economy. Tehran, Publishing community. 1378:95–83. [Google Scholar]
- 11.The World Health Organization reported in 2000. Why health systems are important? Translation: Ahmadvand AR, Ibn Sina largest publisher of scientific and cultural institutions. Printing. SUMMER. 1382:50–33. [Google Scholar]
- 12.WHO. Geneva: WHO; 2001. Management effectiveness program (Map Guide) [Google Scholar]
- 13.Schut FT, Gress S, Wasem J. Consumer price sensitivity and social health insurer choice in Germany and the Netherlands. Int J Health Care Finance Econ. 2003;3:117–38. doi: 10.1023/a:1023369231291. [DOI] [PubMed] [Google Scholar]
- 14.Mishra R. Social security in South Korea and Singapore: Explaining the differences. Soc Policy Adm. 2007;29:228–40. [Google Scholar]
- 15.Cat. no. AUS 142. Canberra: AIHW; Australian Institute of Health and Welfare 2011. Australia's welfare 2011. Australia's welfare series no. 10. [Google Scholar]
- 16.Yip W, Berman P. Targeted health insurance in a low income country and its impact on access and equity in access: Egypt's school health insurance. Health Econ. 2001;10:207–20. doi: 10.1002/hec.589. [DOI] [PubMed] [Google Scholar]
- 17.Bärnighausen T, Sauerborn R. One hundred and eighteen years of the German health insurance system: Are there any lessons for middle-and low-income countries? Soc Sci Med. 2002;54:1559–87. doi: 10.1016/s0277-9536(01)00137-x. [DOI] [PubMed] [Google Scholar]
- 18.Gericke, Christian A. Financing health care in Egypt: Current issues and options for reform. No.2004/5. Diskussions papiere Technische Universität Berlin, Fakultät Wirtschaft und Management. 2004 [Google Scholar]
- 19.Jacobs, Rowena, Maria Goddard. “Social health insurance systems in European countries” The role of the insurer in the health care system: A comparative study of four European countries, University of York. 2000 [Google Scholar]
- 20.Kwon S. Thirty years of national health insurance in South Korea: Lessons for achieving universal health care coverage. Health Policy Plann. 2009;24:63–71. doi: 10.1093/heapol/czn037. [DOI] [PubMed] [Google Scholar]
- 21.Smith J. Tax expenditures and public health financing in Australia. Australia Institute. 2000 [Google Scholar]
- 22.Busse R, Dixon A, Healy J, Krasnik A, Leon S, Paris V, et al. health care system in eight countries: Trends and challenges: European observatory on health care system. [Last accessed on 2014 Nov 09]. Available from: http://www.cimca.ca/i/m/Health-Care-Systems-in-Eight-Countries-European-Observatory.pdf .
- 23.Lee J. Health care reform in South Korea: Success or failure? Am JPublic Health. 2003;93:48–51. doi: 10.2105/ajph.93.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Busse R, Riesberg A. Health care system in transition (Germany) [Last accessed on 2014 Nov 09]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0018/80703/E85472.pdf .
- 25.Kwon S. Healthcare financing reform and the new single payer system in the Republic of Korea: Social solidarity or efficiency? International Social Security Review. 2003;56:75–94. [Google Scholar]
- 26.Ali Zadeh Murad. Overview of the health and welfare. Special Issue on Medical Insurance. 2002;6:45. [Google Scholar]
- 27.Schwefel D. Health financing in Egypt. National health accounts, health insurance and family health funds. Lessons for the Health Sector Modernisation Programme of Syria. [Last accessed on 2014 Nov 09]. Available from: http://detlef-schwefel.de/232-Schwefel-Egypt.pdf .
- 28.World Health Organization. The world health report 2003: Shaping the future. World Health Organization. 2003. [Last accessed on 2014 Nov 09]. Available from: http://www.who.int/whr/2003/en/whr03_en.pdf .
- 29.Evans D, Etienne C. Health systems financing and the path to universal coverage. Bulletin of the World Health Organization. 2010;88:402. doi: 10.2471/BLT.10.078741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wagstaff A. Social Health Insurance vs. Tax-Financed Health Systems–Evidence from the OECD. [Last accessed on 2014 Nov 09]. Available from: http://elibrary.worldbank.org/doi/pdf/10.1596/1813-9450-4821 .
- 31.Ekman B, Liem NT, Duc HA, Axelson H. Health insurance reform in Vietnam: A review of recent developments and future challenges. Health Policy Plan. 2008;23:252–63. doi: 10.1093/heapol/czn009. [DOI] [PubMed] [Google Scholar]
- 32.Najjar A. Process packets of information systems in selected countries, and provide complementary health insurance services model for Iran. Journal of Health Information Management. 2006;3:0. [Google Scholar]
- 33.Moghadasi H. The health insurance system problems and urgency of corrective approach. Journal of Management. 2001:14–0. [Google Scholar]
- 34.Eqbali M. Health insurance structure. Journal of national Medical council of the Islamic Republic of Iran. 2001 [Google Scholar]
- 35.Cheng TM. Taiwan's new national health insurance program: Genesis and experience so far. Health Aff (Millwood) 2003;22:61–76. doi: 10.1377/hlthaff.22.3.61. [DOI] [PubMed] [Google Scholar]


