Abstract
Background:
The prevalence of self-medication is high all over the world, especially in Iran. But there is a paucity of studies to explore self-medication activities among the university students. Therefore, the present study was undertaken to determine the self-medication among student in Isfahan University of Medical Sciences, based on Health Belief Model (HBM).
Materials and Methods:
This cross-sectional study was conducted in 197 medical students of Isfahan University of Medical Sciences who were randomly chosen by a stratified random sampling method in 2009. The data were collected using a validated and reliable questionnaire based on HBM. Statistical analysis was performed using SPSS software (ver. 16). Descriptive and analytical statistics (independent t-test and test) were used. A two-tailed P value lower than 0.05 was considered statistically significant.
Results:
The mean and standard deviation of participants’ age was 22.00 ± 2.77 years. 67.3% of the sample consisted of females. The mean scores of knowledge, perceived susceptibility, perceived severity, perceived benefits, and perceived barrier were 80.36 ± 18.29, 40.92 ± 13.89, 61.48 ± 19.03, 59.11 ± 18.46, and 30.36 ± 12.40, respectively. According to the results, 84.98% of students had experienced self-medication at least for one disease during the past 6 months.
Conclusions:
The prevalence of self-medication in medical students is high and we can consider it as a health problem. So, we need educational interventions for the students, using HBM constructs.
Keywords: Drug, Health Belief Model, knowledge, practice, self-medication, student
INTRODUCTION
Self-medication is defined as the use of medication, whether modern or traditional, without the advice of a physician either for diagnosis, prescription, or surveillance of treatment.[1]
This includes acquiring medicines without a prescription, resubmitting old prescriptions to purchase medicines, sharing medicines with relatives or members of one's social circle, or using leftover medicines stored at home.[2]
The prevalence of self-medication is high all over the world; it is up to 68% in the European countries[3] and much higher in the developing countries,[4] with rates going as high as 92% among the adolescents of Kuwait,[5] 31% in India,[6] and 59% in Nepal.[4]
There is some recent evidence that prevalence of self-medication is increasing in developing and developed countries.[7,8] There are also some reports regarding self-medication and drugs’ storage in Iran.[9,10] Previous studies reveal that the prevalence of self-medication in Iran is 63% in Tabriz, 83% in Yazd, and 94% in Ramhormoz.[11,12,13] Another study reported 86% self-medication for at least in one disease during the past months in women who refer to health centers.[14]
Previous studies in different populations have revealed self-medication is influenced by many factors such as education, family, society, law, availability of drugs, and exposure to advertisements.[9,10,15,16] Also, previous study emphasize on high level of education and professional status as the predictive factors for self-medication.[17]
Because, medical students need to be familiar with diseases and drugs during their education it can be lead to self medication in this group.
The prevalence of self-medication in students in Slovenia and Thailand was 92.3% and 86%, respectively.[18] Some studies reported the prevalence of self-medication as 55% in Egyptian medical students[19] and 98% in Palestinian students.[20]
Few studies regarding students’ self-medication have been conducted in Iran, which have also reported the prevalence rates from 53 to 85%.[21,22]
As mentioned earlier, there is a paucity of studies to explore self-medication activities among the university students in Iran. One of the behavioral models that can be used to describe this matter is Health Belief Model (HBM). This model, which emerged in the late 1950s, was used as an exploratory model to assess why people did not use preventive health services and eventually to understand why people use or fail to use health services.[19] HBM consists of various constructs including perceived susceptibility, severity, barriers and benefits, cues to action, and health action.[19] Many researchers now employ this model to identify the behavior; for example, Sharifirad and Shamsy used this model in two different cities in Iran (Isfahan and Arak) and concluded that this model can describe well the reality of self-medication.[14,22,23]
Despites this, there is paucity of literature to explore self-medication practice among medical students in Iran using appropriate exploratory model. Therefore, the present study was undertaken to determine the self-medication practice among the students in Isfahan University of Medical Sciences, based on HBM.
MATERIALS AND METHODS
This cross-sectional study was conducted in 197 medical students of Isfahan University of Medical Sciences who were randomly chosen by a stratified random sampling method in 2009.
Students who were allowed to prescribe medication were excluded from the study. All participants were informed about the details of the study and were asked to read and sign a consent form.
A self-administered questionnaire was designed by the researchers. The questionnaire was divided into three sections: Demographic data (4 questions), knowledge (10 questions), and HBM constructs (perceived susceptibility, perceived severity, perceived benefits, and perceived barriers) each part (5 questions), cues to action and practice (11 questions). For HBM construct, Likert scoring method was used to assess the answers as follows: (certainly agree = 4, agree = 3, no idea = 2, disagree = 1, and certainly disagree = 0), and the score range for every section was from 0 to 100. For knowledge section, score 1 was given to each correct answer and the score for wrong answers was zero. Finally, practice and behavior of participants was assessed over the past 6 months by questions with yes or no answers. Scores 1 and 0 were given to yes and no answers about practice, respectively.
Content validity of the questionnaire was assessed through view points of an expert panel. The reliability was determined by Cronbach's alpha, and the scores of alpha for the questions were in the range of 0.81–0.88.
Statistical analysis was performed using SPSS software (ver. 16). We used descriptive (mean and frequency) and analytical statistics (independent t-test and test). A two-tailed P value lower than 0.05 was considered statistically significant.
RESULTS
The mean and standard deviation of participants’ age was 22.00 ± 2.77 years. Less than half of the sample were males [n = 65 (32.7%)] and over half of them [n = 132 (67.3%)] were females. Among the participants, 179 (91.3%) were single while 17 (8.7%) were married. Majority of the participants [187 (95.4%)] had medical insurance.
The mean score of knowledge was 80.36 ± 18.29. The data showed that the mean scores of the model variables for perceived susceptibility, perceived severity, perceived benefits, and perceived barrier were 40.92 ± 13.89, 61.48 ± 19.03, 59.11 ± 18.46, and 30.36 ± 12.40, respectively.
The results showed that 84.98% of students had experienced self-medication at least for one disease during the past 6 months.
The most common symptom that led students to engage in self-medication was headache [114 (58.2%)]. The medical conditions that led to self-medication are given in Table 1. The frequency of medicines used is given in Table 2.
Table 1.
Medical conditions that pushed the student to self-medicate
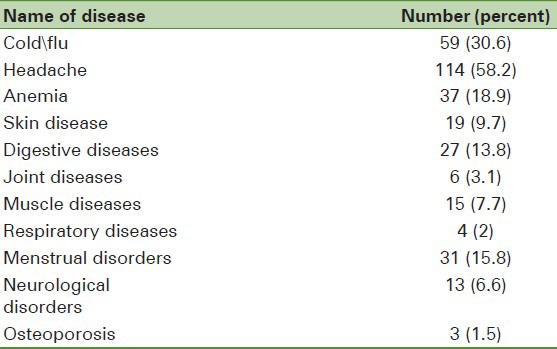
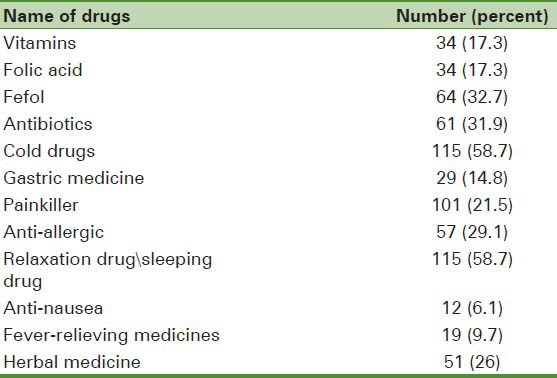
Table 2.
Commonest drugs that were used in self-medication
The most common factors that led to self-medication were previous experience (60.7%), simple availability of the medications (50.5%), mild diseases (45.5%), good result (48.5%), and lack of time (42.3%).
The main resources of information about self-medication were physician (68.37%), books (48.98%), family (20.92%), TV (19.90%), magazine (18.37%), other patients (15.81%), and radio (14.28%).
Moreover, the most important reasons for avoiding self-medication among the students were their fear of getting complications from self-medication [142 (72.9%)], lack of belief [27 (13.8%)], and being in good physical condition [26 (13.3%)].
There was no significant difference between the self-medication practices and age (P = 0.123). Self-medication was significantly different between the two sexes; women took higher self-medication (P < 0.001). Also, there was a significant difference between self-medication and medical insurance; self-medication was higher in people who did not have medical insurance (P = 0.021).
DISCUSSION
Our study demonstrates that about 84.98% of students in Isfahan University of Medical Sciences self-medicate. This result is similar to 83% self-medication reported by Baghianimoghadam.[18] However, one study reported 92% self-medication in Kuwait and 98% in Palestinian students.[24] Also, findings from a literature review of self-medication in physicians and medical students reported 50% self-treatment in 76% of studies.[25] In general, the prevalence of self-medication in students is quite high and needs to be taken seriously.
Based on the findings, despite the high prevalence of self-medication, students’ knowledge is particularly high about self-medication. So, what is the problem? Consistently in various studies related to health education, it is expressed that knowledge does not cause behavior. It is also seen in other studies about self-medication.[24,26]
According to our study findings, the mean of perceived susceptibility was less than 50. This shows students’ low sensitivity to self-medication complications due to their insufficient knowledge regarding drug complications.
In relation to benefits and barriers, we must teach them the benefits of self-treatment and reduce the barriers of access to doctor and provide free medical facilities.
Therefore, the findings of the study suggest the need for focusing on susceptibility structure and improving the perceived benefits in educational programs to reduce the self-medication rate among students. Educational programs should inform the entire student community regarding the side effects of the medications too.
Other studies based on the HBM revealed that HBM could be a suitable model for identifying and improving behaviors.[14,23,27]
In our study, the most frequently reported illness that led to self-medication in students was headache. This is similar to that reported by Abahussain in Kuwait[5] and another study in Karachi.[17] In Thailand also, fever and pain were found to most frequently lead to self-medication.[16]
In the present study, the lowest frequently of self-medication was associated with osteoporosis. It can be attributed to the low risk of osteoporosis in young people.
Most of the drugs used were cold or flu drugs and painkillers. This is comparable to Zafar et al.'s study results that showed painkillers were the most frequent drugs used.[26] In de Aquino et al.'s study, the most frequent drugs used were found to be analgesics and vitamins.[28] Antibiotics were the most frequently used (58.8%) as observed in El Ezz's study, which is not in agreement with the present study.[17]
The rate of using antibiotics in our study was 31.3%, while in Sarahroodi and Arzi's study, it was 53%.[20] In general, Iran can be considered as one of the largest antibiotic consuming countries in the world.
In this study, 26% of the students reported that they used herbal medicines, similar to that reported by Asefzadeh et al.,[28] but 9% of participants in western Nepal reported that they used herbs for self-medication.[33] Thus, using herbal medicines can be associated with culture.
Based on our study findings, the most common factors that led to herbal self-medication were previous experience with similar symptom, simple availability of the medications, mild diseases, good result, and lack of time, while other studies listed reasons such as mild disease, faster and easier access to medicines, and personal beliefs regarding herbal medicine.[4,29,30]
In our study, pharmacy access to nonprescription drugs and existence of a home pharmacy can be the reasons for self-medication, which is consistent with other studies.[16,17,31,33]
We found more female students than male students self-medicating (P = 0.021). This was also seen in other studies,[34,35] but is not consistent with the result of a study conducted by Baghianimoghadam in Yazd city.[20]
There was significant difference between self-medication and medical insurance. This could be reflecting the financial problems faced by the students.
There are a few limitations of this study. The first is that the questionnaire was a self-reported one. The second limitation of this study was that we took a convenience sample and our sample size was small.
CONCLUSION
The prevalence of self-medication in medical students is high and we can consider it as a health problem. So, the findings of the study suggest the need for educational intervention among the students, using HBM constructs, especially perceived susceptibility and perceived barrier, and finally for framing rules limiting the use of drugs stocked at home and also for getting medication from pharmacies without a prescription.
ACKNOWLEDGMENT
The authors would like to thank all the students who willingly participated in the study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Hughes CM, McElnay JC, Fleming GF. Benefits ts and risks of self medication. Drug Saf. 2001;24:1027–37. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- 2.Loyola Filho AI, Lima-Costa MF, Uchôa E. Bambui Project: A qualitative approach to self-medication. Cad Saude Publica. 2004;20:1661–9. doi: 10.1590/s0102-311x2004000600025. [DOI] [PubMed] [Google Scholar]
- 3.Bretagne JF, Richard-Molard B, Honnorat C, Caekaert A, Barthelemy P. Gastroesophageal reflux in the French general population: National survey of 8000 adults. Presse Med. 2006;35:23–31. doi: 10.1016/s0755-4982(06)74515-8. [DOI] [PubMed] [Google Scholar]
- 4.Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: A questionnaire-based study. BMC Fam Pract. 2002;3:17. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abahussain E, Matowe LK, Nicholls PJ. Self-reported medication use among adolescents in Kuwait. Med Princ Pract. 2005;14:161–4. doi: 10.1159/000084633. [DOI] [PubMed] [Google Scholar]
- 6.Deshpande SG, Tiwari R. Self medication--a growing concern. Indian J Med Sci. 1997;51:93–6. [PubMed] [Google Scholar]
- 7.Sahebi L, Vahidi RG. Self-medication and storage of drugs at home among the clients of drugstores in Tabriz. Curr Drug Saf. 2009;4:107–12. doi: 10.2174/157488609788172982. [DOI] [PubMed] [Google Scholar]
- 8.Sedighi B, Ghaderi-Sohi S, Emami S. Evaluation of self-medication prevalence, diagnosis and prescription inmigraine in Kerman, Iran. Saudi Med J. 2006;27:377–80. [PubMed] [Google Scholar]
- 9.Somi MH, Behshid M, Zamanzadeh V, Abbasalizadeh SH, Yavarikia P, Pezeshkian M. Health seeking behavior of residents in northwestern Tabriz. Med J Tabriz Univ Med Sci. 2003;25:77–81. [Google Scholar]
- 10.Haji Seyed Javadi ES. Knowledge of pregnant women on drug use during pregnancy. J Qazvin Univ Med Sci. 2005;9:80–3. [Google Scholar]
- 11.Sereshti M, Azari P, Rafieian M, Kheiri S. Use of herbal medicines by pregnant women in Shahr-e-Kord. J Reprod Infertility. 2006;7:131–25. [Google Scholar]
- 12.Sharifirad G, Pirzadeh A, Azadbakht L. Knowledge and practice in association with self-medication of nutrient supplements, herbal and chemical pills among women based on Health Belief Model. J Res Med Sci. 2011;16:852–3. [PMC free article] [PubMed] [Google Scholar]
- 13.Montastruc JL, Bagheri H, Geraud T, Lapeyre MM. Pharmacovigilance of self-medication. Therapie. 1997;52:105–10. [PubMed] [Google Scholar]
- 14.Hebeeb GE, Gearhart JG. Common patient symptoms: Patterns of self-treatment and prevention. J Miss State Med Assoc. 1993;34:179–81. [PubMed] [Google Scholar]
- 15.Martins AP, Miranda AC, Mendes Z, Soares MA, Ferreira P, Nogueira A. Self-medication in a Portuguese urban population: A prevalence study. Pharmacoepidemiol Drug Saf. 2002;11:409–14. doi: 10.1002/pds.711. [DOI] [PubMed] [Google Scholar]
- 16.Kitikannakorn N, Sitthiworranan C. Self-medication among undergraduate students in Thailand. International Journal on Disability and Human Development. 2009;8:411–6. [Google Scholar]
- 17.El Ezz NF, Ez-Elarab HS. Knowledge, attitude and practice of medical students towards self medication at Ain Shams University, Egypt. J Prev Med Hyg. 2011;52:196–200. [PubMed] [Google Scholar]
- 18.Baghianimoghadam MH, Ehrampoush MH. Evaluation of attitude and practice of students of Yazd University of Medical Sciences to self-medication. Zahedan J Res Med Sci. 2006;8:111–9. [Google Scholar]
- 19.Sawalha AF. A descriptive study of self-medication practices among Palestinian medical and nonmedical university students. Res Soc Adm Pharm. 2008;4:164–72. doi: 10.1016/j.sapharm.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Sarahroodi S, Arzi A. Self medication with antibiotics, is it a problem among Iranian colledge students in Tehran. J Biol Sci. 2009;9:829–32. [Google Scholar]
- 21.Glanz K, Rimer BK, Viswanath K. 4th ed. San Francisco: John Wiley and Sons; 2008. Health Behavior and Health Education: Theory, Research, and Practice. [Google Scholar]
- 22.Shamsi M, Tajik R, Mohammad Beigi A. Effect of education based on Health Belief Model on self-medication in mothers referring to health centers of Arak. Arak Med Univ J. 2009;12:57–66. [Google Scholar]
- 23.Montgomery AJ, Bradley C, Rochfort A, Panagopoulou E. A review of self-medication in physicians and medical students. Occup Med (Lond) 2011;61:490–7. doi: 10.1093/occmed/kqr098. [DOI] [PubMed] [Google Scholar]
- 24.James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med Princ Pract. 2006;15:270–5. doi: 10.1159/000092989. [DOI] [PubMed] [Google Scholar]
- 25.Pirzadeh A, Mazaheri MA. The effect of education on women's practice based on the health belief model about pap smear test. Int J Prev Med. 2012;3:585–90. [PMC free article] [PubMed] [Google Scholar]
- 26.Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. Self-medication amongst university students of Karachi: Prevalence, knowledge and attitudes. J Pak Med Assoc. 2008;58:214–7. [PubMed] [Google Scholar]
- 27.de Aquino DS, de Barros JA, da Silva MD. Self-medication and health academic staff. Cien Saude Colet. 2010;15:2533–8. doi: 10.1590/s1413-81232010000500027. [DOI] [PubMed] [Google Scholar]
- 28.Asefzadeh S, Anbarloei M, Habibi Sh, Rezaei M. Selfmedication among the in-patients of Qazvin teaching hospitals. J Qazvin Univ Med Sci. 2002;5:48–54. [Google Scholar]
- 29.Sepehri Ch, Kohan S, Ghazanfari Z. The knowledge of patients referred to Kerman pharmacies about their dispensed drugs, 1997. J Babol Univ Med Sci. 2001;3:52–8. [Google Scholar]
- 30.Dinarvand R, Nikzard A. Status of prescription and drug usage in Tehran in 1998. Hakim Res J. 2000;3:230–3. [Google Scholar]
- 31.Bonner S, Zimmerman BJ, Evans D, Irigoyen M, Resnick D, Mellins RB. An individualized intervention to improve asthma management among Urban Latino and African –American families. J Asthma. 2002;39:167–79. doi: 10.1081/jas-120002198. [DOI] [PubMed] [Google Scholar]
- 32.Motola G, Russo F, Mazzeo F, Rinaldi B, Capuano A, Rossi F, et al. Over the counter aral non steroidal anti- inflammatory drugs: A pharmaco epidemiologic study in southern Italy. Adv Ther. 2001;18:216–22. doi: 10.1007/BF02853167. [DOI] [PubMed] [Google Scholar]
- 33.Ferris DG, Nyirjesy P, Sobel JD, Soper D, Pavletic A, Litaker MS. Over the counter antifungal drug misuse associated with patient diagnosed vulvovaginal candidiasis. Obstet Gynecol. 2002;99:419–25. doi: 10.1016/s0029-7844(01)01759-8. [DOI] [PubMed] [Google Scholar]
- 34.Klemenc-Ketis Z, Kersnik J. The effect of demographic characteristics on self-medication patterns: A cross-sectional nationwide study from Slovenia. Coll Antropol. 2011;35:1237–42. [PubMed] [Google Scholar]
- 35.Kitikannakorn N, Sitthiworranan C. Self-medication among undergraduate students in Thailand. Int J Disabil Hum Dev. 2009;8:411–6. [Google Scholar]


