Abstract
Background:
Health literacy is a measure of individual's ability to read, comprehend, and act on medical instructions. Older adults are one of the most important at risk groups affected by the impact of inadequate health literacy. Health promoting behaviors in older adults have potential impact on their health and quality of life and reduce the costs incurred to health care. Given the paucity of information health literacy and health promoting behavior, the purpose of this study was to examine health literacy level in older adults and the relationship between health literacy and health promoting behaviors.
Materials and Method:
A cross-sectional survey of 354 older adults was conducted in Isfahan. The method of sampling was clustering. Health literacy was measured using the Test of Functional Health Literacy in Adults (TOFHLA). Data were collected via home interviewing. Health promoting behaviors were measured based on self-reported smoking status, exercise, and consumption of fruit and vegetables. The collected data were analyzed using descriptive statistics and one-way ANOVA and χ2 tests under SPSS 18 software.
Results:
The sample group averaged 67 ± 6.97 years in age. Approximately 79.6% of adults were found to have inadequate health literacy. They tended to be older, have fewer years of schooling, lower household income, and being female Individuals with inadequate health literacy were more likely to report limitations in activity and lower consumption of fruit and vegetables (P < 0.001). No significant association was found between health literacy and smoking status.
Conclusion:
Considering high prevalence of inadequate health literacy among older adults, and its inverse relationship with some health promoting behaviors. Simple educational materials and effective interventions for low health literacy people can improve health promotion in society and mitigate the adverse health effects of low health literacy.
Keywords: Health literacy, health promoting behaviors, older adults
INTRODUCTION
The effect of low health literacy on the public health has been the subject of much attention during last decade, causing a complex association for education and health.[1] Inadequate health literacy is defined as limited ability to receive, interpret, and understand the primary health services and information necessary for proper decision making about health.[2] Inadequate health literacy is associated with issues such as inadequate understanding of health information, medical instructions and implementing them,[3,4,5,6] less resort to preventive measures,[7] delayed diagnosis of diseases,[8] inability in self-care skills,[9] and not leading a healthy lifestyle.[10] Furthermore, epidemics of chronic diseases[1] and the rate of report to doctor and hospitalization[11] are higher among individuals with inadequate health literacy, generally incurring higher medical bills.[12]
According to findings of a survey in 2006 and data about 31 129 participants, about a quarter suffered from inadequate health literacy.[13] In a study in Iran, 56.6% of the participants had inadequate health literacy and only 28.1% had high and adequate health literacy.[14] The other study that conducted in Isfahan, Iran, only 15.5% of adults had adequate health literacy based on S-TOFHLA questionnaire.[15]
Inadequate health literacy is more rampant among senile cohort, immigrant communities, illiterate individuals, lower-income families, individuals with lower psychological health, and patients of chronic diseases. These groups probably would be affected by the more harmful impact of inadequate health literacy than other groups would.[9,16,17,18,19]
In an IRNA (Iranian News Agency; Iran's state-run news agency) report, it was said that currently older adults above 60 comprised 6% of total population of the country, accounting for 4 562 000 people. According to age pyramid, it is estimated that this figure will soar to 26 393 000 people, about 26% of total population by 2050.[20] Other reports reveal that 60% of health care expenses; 35% of hospitalization bills, and 47% of days in hospital incur to older adults. Given the rapid surge of the number of older adults, the issues of provision of health and welfare for this group has displayed increasingly new dimensions.[21]
Health promoting behaviors are among the main criteria of health, identified as a background contributor to avoiding diseases, and health promotion and prevention of diseases are directly related to these behaviors.[22] These behaviors in older adult would significantly effect on promotion of health and living quality and subsequently, would cut health care costs.[23]
Mortality rate statistics on major causes of death indicates that 53% of major causes of death are associated withunhealthy life style and behavior.[24,25] The US Department of Health and Human Services has emphasized upon the regular physical activity, avoiding cigarette, alcohol, good nutritional habits, and building age-appropriate immunity for improving health among older adults.[23] These behaviors can be assumed as health-promoting behaviors. Given the importance of health literacy and health promoting behavior among older adults andreport prepared by Agency for Healthcare Research and Quality, which highlights the necessity of further research on the health literacy and impacts on individuals’ health, and also a research[10] on health literacy and healthy behaviors, the present study, we examined the links between health literacy and health promoting behaviors among older adults as one of the most vulnerable age groups in Isfahan.
MATERIALS AND METHODS
A descriptive–analytical study was carried out in Isfahan with participants over 60. The data werecollected through homeinterviewing. The sampling was cluster samples appropriate to the volume of the population. Health Centers were assumed as cluster heads. With the larger population covered by the services provided by these Health Centers in Isfahan second health network, eightcenters from second network and sixcenters from first network were taken randomly. Then, moving to the right-hand side of (in the exit door of any health center) the health center, 28 individuals were selected from each cluster and assigned to research groups. Given that interview was our main data collecting tool, the participants were briefed about the research objectives in clear way as possible, and finally, from within older adults willing to participate, were incorporated into study. Some of participants were illiterate, hence, were unable to read the questionnaire and fill in them, and they felt being mortified,[26,27,28] a sample written text was given to individuals to be read aloud by them. This way, the illiterate individuals were sort out, and other literate individuals helped the illiterate cohort fill the questionnaires. Because of the number of questions, which was quite many, questionnaires were filled in two stages. Individuals with acute auditory and visual problems, or cognitive and psychological disorders, and thus incapable of filling in the questionnaire were eliminated.
To evaluate the health literacy among the participants, we used Test of Functional Health Literacy in Adults (TOFHLA). This is one of the most applied and valid questionnaires to measure health literacy worldwide and validity of its translated form has been examined in many languages. To measure the validity of the questionnaire, Cronbach's alpha test with assurance of 95% and significance of 0.05 was used. The reliability was 0.79 for calculation and 0.88 for reading comprehension. The questionnaire comprised of twosections of calculation and reading comprehension. Calculation measured the individual's ability to understand and act according to doctors’ and health educators’ instructions thatneeded calculating capabilities. This section included 10 health instructions or prescription of medications, report time to doctors, steps to use financial aids, and an example from the result of a clinical test. These comments were provided to subjects as flash cards. Questions were asked and individual scores ranged from 0 to 50.
In reading comprehension section, the participants’ ability to understand threetexts, namely (instructions for preparation for an X-ray imaging of upper gastronomical tract, patients’ rights and obligations in insurance form sheets, and the hospital consent forms) were measured and assigned scores ranging from 0 to 50. Summing the two scores would give a total of 100 score for health literacy. Ultimately, participants’ health literacy scores were divided into three categories of inadequate (0-59); border (60-74), and adequate (75-100). The questionnaire also included personal items such as age, gender, marital status, education, and income level. To examine the health promoting behavior, threeitems in health promoting behavior checklist were evaluated. These included smoking, which was answered with ‘yes,’ ‘quitted,’ and ‘never smoked’; sport as walking, which was answered with ‘never do,’ ‘onesession a week,’ ‘two to three sessions a week,’ and ‘fouror more sessions a week’; fruit consumption, which was answered with ‘less than twounits per week,’ ‘two to four units per week,’ and ‘more than fourunits per week’; vegetable intake thatwas answered with ‘less than threeunits per week,’ ‘three to five units per week,’ and ‘more than fiveunits per week’. The collected data wereanalyzed in SPSS 18 via descriptive statistics (to determine mean, standard deviation, and the percentage of personal data and health literacy levels) and one-way ANOVA and χ2 tests for establishing a relationship between health literacy levels and personal characteristics and health promoting behaviors.
Findings
We collected the data on 354 individuals above 60 in Isfahan. The sample averaged 67 ± 6.97 years in age, with 60 being the least age, and 91 being the highest. The majority of participants were males (57.3%), married (77.7%), and illiterate (46.9%). Generally, about 46% of participants reported their economic status as moderate, 43% reported it as poor, and only 9.3% reported it as good and very good condition [Table 1].
Table 1.
Personal characteristics and health literacy levels among older adults in Isfahan
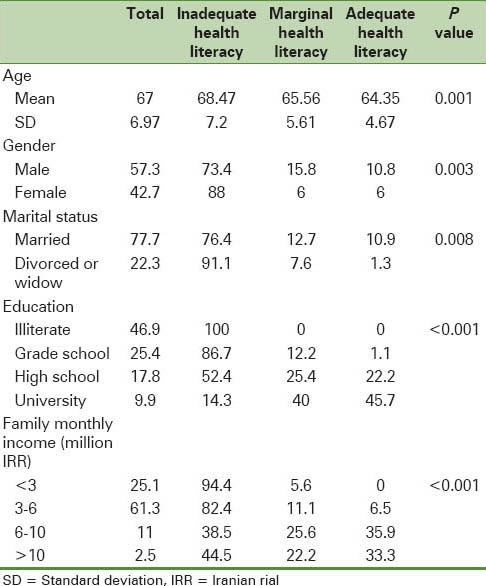
The mean score of health literacy was 29.07 ± 30.45 out of possible 100. Health literacy of 79.7% of older adults evaluated as inadequate, 11.6% were in border condition, and 8.8% of them had adequate health literacy. One-way ANOVA test set a significant relationship between health literacy and age, and χ2 test set a significant relationship between health literacy with gender, marital status, education, and household income level. Inadequate health literacy was more prevalent among individuals in higher ages, lower education and income, divorced and widowed, and also among women.
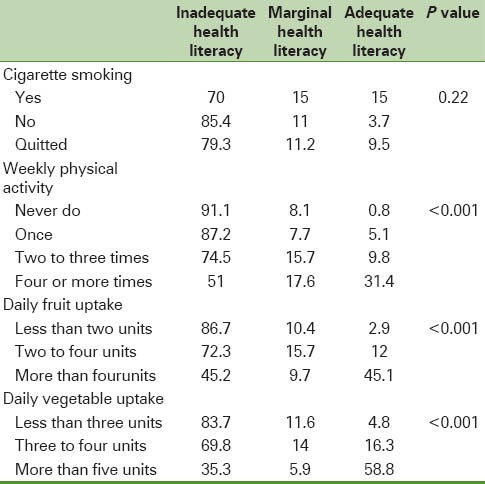
Results for health promoting behaviors, our findings indicated that about 65% of participants did not smoke; 34.7% of them did no physical activity; 67% consumed less than twounits of fruits daily and about 83% eat less than threeunits of vegetables daily. X2 test indicated that there was a significant relationship between health literacy level and physical activity, fruits, and vegetables consumption (P < 0.001), such that older adults with higher health literacy reported more physical excises, fruits, and vegetables consumption [Table 2].
Table 2.
Health promoting behavior and health literacy levels among older adults in Isfahan
DISCUSSION AND CONCLUSION
Our results indicated that the level of health literacy was quite low among older adults and 79% of them lacked adequate health literacy. Because of the epidemics of chronic diseases and subsequent need for older adults to capability in self-care skills, and also special needs such as screening tests and leading healthy life among older adults, the issue of health literacy gains importance, since much research indicated that health literacy research wielded direct impact on these factors. Such lower health literacy among older adults would wring the bells for authorities and policy-making agents in the domain of public health.
Research from around the world also indicated larger scope of inadequate health literacy. An NAAL (National Assessment of Adult Literacy) study by Kutner et al., in 2003 found that only 3% of older adults possessed adequate health literacy.[29] In Wagner et al., 30% of older adults (above 60) lacked adequate health literacy.[10] Baker et al. reported inadequate health literacy for 24.5% of the older adults.[30] Wolf et al. found inadequate health literacy for 22.2% of the older adults.[26] In their systematic study of 80 research, Paasche-Orlow et al. reported 20% of participants as having border level health literacy and 26% of participants as having inadequate health literacy.[13] Tehrani et al. reported an overall inadequate health literacy level for 56.6% of the participants.[14]
We found a significant relationship between health literacy and age, gender, education, and income levels, with higher ages and lower incomes having the lower health literacy, a fact confirmed by other authors.[3,10,29,31] Married individuals enjoyed higher health literacy, consistent with findings of Tehrani et al.,[14] Our findings indicated inadequate health literacy more rampant among women than among men. Le et al. also found higher health literacy scores for man compared to women.[32] In contrast to our study, Wagner et al. reported a higher health literacy score for women compared to men.[10] Other studies found no association for health literacy level and gender.[14,30,32] In our studies, lower scores for health literacy among women is probably accounted for by their lower education.
The present study also indicated that physical exercises were higher among individuals with higher health literacy score. Other studies found similar results.[1,26] Given the physiological changes in older adults, physical exercise gains importance among this cohort, since regular exercises as an important preventive measure against health risks, cuts significantly the cardiovascular diseases, diabetes, hollow bones, and deaths and debilitations related to chronic diseases.[33] Therefore, health literacy, as improving factor of physical performance among older adults should found attention in health promoting programs more than ever.
Consistent with Wagner et al., working in Britain, our findings also indicated that individuals with higher health literacy reported higher consumption of fruits and vegetables.[10] This can be attributed to higher education level, since higher education contribute to individuals’ information about benefits of consuming fruits and vegetables. Having the privilege of more financial sources and belonging to higher socioeconomic classes could overcome the effect of economic factor as one of barriers on affording to consume fruits and vegetables.[34]
Contrary to other research, we did not find any significant relationship between health literacy level and smoking habits. Wolfe et al. found that individuals with higher health literacy smoked more than others[26] and Wagner et al. reported lower smoking for individuals with higher health literacy.[10] It should be noted that since smoking could be left unreported for cultural reasons, and due to the self-report nature of answers, this could be counted as a limitation to the present study.
The findings of this study indicated significant relationship between health literacy level and health promoting behavior, emphasizing upon the key role of health literacy in improving health. Since health promoting behaviors displayed potential effect on health improvement and quality of life in older adults, and hence cutting the incurring health care costs, health literacy should find great attention among the public for its role in improvement of quality of life and healthy life style.
It should be noted that contrary to many studies in other countries, to enhance the quality of assessment, we used a long questionnaire rather than a short questionnaire to examine the health literacy. And since this was a population-based research, the possibility of selection bias is quite low compared to that in other studies, since they often examined individuals going to health care centers to receive services.
Given the age group of the participants (above 60), our results could not be generalized to other cohorts. Thus, further research should be carried out to examine the effects of health literacy on different aspects of health. Among the limitations to our study is its self-report nature of the collected data. Since consent by the participants was a criterion for inclusion, it is possible that those older adults with higher education would be more eager to participate, this can pose another limitation.
A recurring problem related to using questionnaire to measure health literacy in this study is that it focused more on reading and calculation capabilities, while it underestimate the effect of speech ability, the ability to listen, the ability and information necessary to ask support from the health system, which are important components of health literacy. Given the emphasis upon clinical behavior, and the fact that health literacy also was related to issues beyond these behaviors, it is recommended that more extensive aspects of health literacy to measure it be emphasized.
Finally, our findings, as the first ever research in Iran on the relationship between health literacy and many aspects of health, can be drawn upon in micro and macroenvironments, with considerable effect on health status and ultimately on public health. Our results indicated the health literacy among older adults quite inadequate, a fact which invites more attention to the issue of health literacy in health promoting programs. This is an objective achievable only with the cooperation of different factors such as mass media as one of major sources of health-related information for the people and health system; since health system also wielded direct impact on the quality of health care provision and information to service receptors. Overall, through building comprehensive programs and establishing media and simple and easy-to-understand educational material for individuals with inadequate health literacy, regular communications between health authorities and serviceseekers, and effective educational interferences, important steps can be taken to develop the health literacy skills across society.
ACKNOWLEDGEMENT
The authors would thank the teaching staff of Health Education and Promotion department, Isfahan University of Medical Sciences for their kind cooperation and help doing this research. Special thanks also go to all older adults who helped filling in questionnaires as participants.
Footnotes
Source of Support: Isfahan University of medical sciences (IUMS) No: 389480
Conflict of Interest: None declared
REFERENCES
- 1.Wolf MS, Gazmararian JA, Baker DW. Health Literacy and Functional Health Status among Older Adults. Arch Intern Med. 2005;165:1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 2.Selden C, Zorn M, Ratzan S, Parker R. Bethesda, Md: National Library of Medicine; 2000. Current bibliographies in medicine: Health literacy. [Google Scholar]
- 3.Cho YI, Lee SY, Arozullah AM, Crittenden KS. Effects of health literacy onhealth status and health service utilization amongst the elderly. SocSci Med. 2008;66:1809–16. doi: 10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Davis TC, Wolf MS, Bass PF, Middlebrooks M, Kennen E, Baker DW, et al. Low literacy impairs comprehension of prescription drug warning labels. J Gen Intern Med. 2006;21:847–51. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient EducCouns. 2003;51:267–75. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 6.Parker RM, Ratzan SC, Lurie N. Health literacy: A policy challenge for advancing high-quality health care. Health Aff. 2003;22:147–53. doi: 10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]
- 7.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Bennett CL, Ferreira MR, Davis TC, Kaplan J, Weinberger M, Kuzel T, et al. Relation between literacy, race, and stage of presentation among low-income patients with prostate cancer. J ClinOncol. 1998;16:3101–4. doi: 10.1200/JCO.1998.16.9.3101. [DOI] [PubMed] [Google Scholar]
- 9.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetesoutcomes. JAMA. 2002;288:475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 10.Wagner C, Knight K, Steptoe A, Wardle J. Functional health literacy and health-promoting behavior in a national sample of British adults. J Epidemiol Community Health. 2007;61:1086–90. doi: 10.1136/jech.2006.053967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, et al. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health. 2002;92:1278–83. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiss BD, Palmer R. Relationship between health care costs and very low literacy skills in a medically needy and indigent Medicaid population. J Am Board FamPract. 2004;17:44–7. doi: 10.3122/jabfm.17.1.44. [DOI] [PubMed] [Google Scholar]
- 13.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–84. doi: 10.1111/j.1525-1497.2005.40245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tehrani Banihashemi S, Amir Khani A, Haghdoust A, Alavian M, Asghari Fard H, Baradaran H. Health literacy in five province and relative effective factors. Strides in Development of Medical Education. 2007;4:1–9. [Google Scholar]
- 15.Javadzadeh H, SharifiradGh, Reisi M, Tavassoli E, Radjati F. Health literacy among adults population of Isfahan. J Health Syst Res. 2013;9:540–9. [Google Scholar]
- 16.Institute of Medicine. Washington DC: National Academies Press; 2004. Health literacy: A prescription to end confusion. [PubMed] [Google Scholar]
- 17.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients knowledge of their chronic disease: A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 18.Kalichman SC, Rompa D. Functional health literacy is associated with health status and health related knowledge in people living with HIV-AIDS. J Acquir Immune DeficSyndr. 2000;25:337–44. doi: 10.1097/00042560-200012010-00007. [DOI] [PubMed] [Google Scholar]
- 19.Kalichman SC, Benotsch E, Suarez T, Catz S, Miller J, Rompa D. Health literacy and health- related knowledge among persons living with HIV/AIDS. Am J Prev Med. 2000;18:325–31. doi: 10.1016/s0749-3797(00)00121-5. [DOI] [PubMed] [Google Scholar]
- 20.Islamic Republic News Agency. Social; Elderly. [On-line] [Last accessed on 2007 June 03]. Available from: http://www. irna.com/en/news/line-8.html .
- 21.Barry PP. An overview of special considerations in the evaluation and management of thegeriatric patient. Am J Gastroenterol. 2000;95:8–10. doi: 10.1111/j.1572-0241.2000.01697.x. [DOI] [PubMed] [Google Scholar]
- 22.Andrews GA. Promoting health and functioning in an aging population. BMJ. 2001;322:728–9. doi: 10.1136/bmj.322.7288.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee TW, Ko IS, Lee KJ. Health promotion behaviors and quality of life among community-dwelling elderly in Korea: A cross-sectional survey. Int J Nurs Stud. 2006;43:293–300. doi: 10.1016/j.ijnurstu.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 24.Stanhop MY, Lancaster J. 5th ed. United States: Mosby Publisher; 2000. Community health nursing; pp. 569–685. [Google Scholar]
- 25.Phipps J. 6th ed. Louis: Mosby; 1999. Medical – surgical nursing; pp. 66–7. [Google Scholar]
- 26.Wolf MS, Gazmararian JA, Baker DW. Health literacy and health risk behaviors among older adults. Am J Prev Med. 2007:32, 19–24. doi: 10.1016/j.amepre.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 27.Parikh NS, Parker RM, Nurss JR, Baker DW, Williams MV. Shame and health literacy: The unspoken connection. Patient EducCouns. 1996;27:33–9. doi: 10.1016/0738-3991(95)00787-3. [DOI] [PubMed] [Google Scholar]
- 28.Wolf MS, Williams MV, Parker RM, Parikh NS, Nowlan AW, Baker DW. Patients’ shame and attitudes toward discussing the results of literacy screening. J Health Commun. 2007;12:721–32. doi: 10.1080/10810730701672173. [DOI] [PubMed] [Google Scholar]
- 29.Kutner M, Greenberg E, Yin J, Paulsen C, White S. Washington, DC: US Department of Education; 2006. The health literacy of America's adults: Results from the 2003 national assessment of adult literacy. [Google Scholar]
- 30.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among Elderly Person. Arch Intern Med. 2007;167:1503–9. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 31.Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, et al. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–51. doi: 10.1001/jama.281.6.545. [DOI] [PubMed] [Google Scholar]
- 32.Lee SY, Tsai TI, Tsai YW, Kuo KN. Health literacy, health status, and healthcare utilization of taiwanese adults: Results from a national survey. BMC Public Health. 2010;10:614. doi: 10.1186/1471-2458-10-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salehi L, Taghdisi MH, Ghasemi H, Shokervash B. To Identify the facilitator and barrier factors of physical activity among elderly people in tehran. Iran J Epidemiol. 2010;6:7–15. [Google Scholar]
- 34.Salehi L, Ardebili HE, Mohammad K, Taghdisi MH, Davoud S. Some factors affecting consumption of fruit and vegetable by elderly people in Tehran. Iran J Ageing. 2010;4:34–44. [Google Scholar]


