Abstract
Background:
The intensity and duration of speech difficulty inherently associated with lingual therapy is a significant issue of concern in orthodontics. This study was designed to evaluate and to compare the duration of changes in speech between labial and lingual orthodontics.
Materials and Methods:
A prospective longitudinal clinical study was designed to assess speech of 24 patients undergoing labial or lingual orthodontic treatment. An objective spectrographic evaluation of/s/sound was done using software PRAAT version 5.0.47, a semiobjective auditive evaluation of articulation was done by four speech pathologists and a subjective assessment of speech was done by four laypersons. The tests were performed before (T1), within 24 h (T2), after 1 week (T3) and after 1 month (T4) of the start of therapy. The Mann-Whitney U-test for independent samples was used to assess the significance difference between the labial and lingual appliances. A speech alteration with P < 0.05 was considered to be significant.
Results:
The objective method showed a significant difference to be present between the two groups for the/s/sound in the middle position (P < 0.001) at T3. The semiobjective assessment showed worst speech performance in the lingual group to be present at T3 for vowels and blends (P < 0.01) and at T3 and T4 for alveolar and palatal consonants (P < 0.01). The subjective assessment also showed a significant difference between the two groups at T3 (P < 0.01) and T4 (P < 0.05).
Conclusion:
Both appliance systems caused a comparable speech difficulty immediately after bonding (T2). Although the speech recovered within a week in the labial group (T3), the lingual group continued to experience discomfort even after a month (T4).
Keywords: Articulation, labial orthodontics, lingual orthodontics, spectrography, speech
INTRODUCTION
The esthetic revolution in dentistry has not left orthodontics untouched. The quest of esthetics has expanded the inventory at the orthodontist's disposition-brackets made of plastic and porcelain, coated arch wires, plastic aligners-all with the sole aim to make the braces less visible. However, the only true solution to the poor esthetics of the conventional fixed orthodontic appliances is to attach the appliances to the lingual surfaces of the teeth. The lingual technique offers the most esthetic orthodontic treatment option at present. This outstanding advantage over other therapies is, however, eclipsed by the drawback that the bracket placement on the lingual surface entails a substantial, albeit temporary, change in the morphology of the lingual tooth surface due to the brackets and thus of the second articulation zone. Lingual placement of the brackets, hence, appears problematic in terms of articulation.[1] Lingual orthodontic patients are usually informed that there may be some speech difficulty and tongue discomfort associated with the insertion of the appliance whose intensity and duration is not yet clearly documented in orthodontic literature.[2,3] If parameters are available to predict the level of inconvenience caused by lingual appliance system, they would help the orthodontist in counselling the patient about the associated difficulties with this treatment modality, thus, helping the patient in decision making when opting for it.[4]
This study was designed with the following objectives:
To prospectively evaluate and compare the speech changes between the patients treated with labial and lingual fixed orthodontic appliance.
To provide guidelines to the orthodontist to help them in counselling their patients about the speech difficulties that may be encountered during the course of treatment.
The null hypothesis being tested was “there is no difference in speech changes observed between patients treated with lingual or labial appliance”.
MATERIALS AND METHODS
24 (12 per group) individuals were assigned to two different groups (LA [labial]-5 males and 7 females; mean age of 22.4 years, and LI [lingual]-6 males and 6 females; mean age of 23.5 years) in a prospective longitudinal study that was conducted in Department of Orthodontics, S.D.M. College of Dental Sciences, Dharwad, Karnataka, India. The ethical clearance for this study was obtained from Institutional Ethical Committee, SDM College of Dental Sciences, Dharwad. The subjects were included based on the following criteria:
Inclusion criteria
Language: Native Kannada speakers (regional language)
Age range: Between 18 and 35 years of age
Method of selection: Convenience and judgment sampling. Sample selection was done from patients who reported to the department from August 2008 to January 2010.
Malocclusion type: Cases with minimum to moderate crowding where treatment involved mainly arch alignment were included as subjects.
All possible inclusions were first examined by a speech language hearing pathologist and audiologist and were included only after obtaining their clearance.
Exclusion criteria
Individuals with impaired stereognostic ability that might be speakers with articulatory problems.[5] Hence, the exclusion criteria was the presence of cleft lip, cleft palate or velar cleft.
A history of speech and hearing disorders.
A history of previous elocution training or speech therapy.
Note on age, gender, sample size and sampling method:
Sex and age related effects were not checked in this study, since a previous study had shown that sex and age did not have any effect on the stereognostic ability (the ability to recognize and discriminate forms) of an individual up to the age of 80 years.[1]
Sample size was limited to 12 per group since at the time of study the lingual technique was relatively new to the place of study; hence, only near ideal cases were included.
A convenience and judgement sampling method was used in the study since the lingual technique was new leading to the lack of expertise and the high cost of treatment limited the number of patients opting for it.
The subjects were allocated to two different groups-LI (lingual) and LA (labial).
The brackets used for lingual orthodontics were STb™ (Ormco CA, USA) brackets, indirectly bonded to the tooth surface. The positioning on the models was done using torque angulation device and bracket positioning device (TAD and BPD, Chiang Mai, Thailand). A Memosil™ tray was used to transfer the brackets from the model to the mouth. Bracket base thickness had been reported to affect the level of discomfort among the patients.[6] TAD is advancement over TARG and is similar to TOP wherein the composite on bracket base compensates for the in out difference between the teeth. Hence, the effect caused by TOP as reported by Hohoff et al.[6] may be valid for TAD also. However, no literature comparing the level of discomfort caused to the patient by bracket positioning done using TAD and BPD with that caused by the other positioning techniques was available in the knowledge of the authors.
The patients undergoing labial orthodontics were treated with pre-adjusted edgewise system using MBT Versatile+ (3M Unitek) prescription. These brackets were directly bonded onto the tooth surface. Direct bonding was chosen since this is the most common method used for bracket positioning in labial orthodontics.[7] A Goshgarian Transpalatal arch was used to reinforce anchorage in the labial group, which was custom fabricated. TPA was used to re-enforce anchorage for three reasons being, economical, common mean to re-enforce anchorage and it brought the labial appliance as close to the lingual group whereas comparisons were being made.
Steps in fabrication of transpalatal arch:
Maxillary molar bands were fitted and palatal sheath alginate impression was made.
The bands were carefully placed in the impression and a thin layer of wax was applied to the inner surface of bands and the impressions were poured in plaster.
A TPA was fabricated on the cast obtained using 0.9 mm stainless steel wire with a distal loop and maintaining a clearance of 1 mm from the tissue, for which a thickness of modelling wax was used as a spacer.
The wax was then melted away and the passivity of the TPA was verified with it being loose from the plaster cast. The bands were then cleaned and sandblasted.
The TPA was finally placed in the mouth after band cementation and secured in place with ligature ties.
Bonding in both groups was done using Transbond XT™ light cure adhesive paste (3M Unitek).
Speech recording was done at following recording sessions:
Immediately before bonding – T1.
24 h after bonding – T2.
1 week after bonding – T3.
1 month after bonding – T4.
The recording was done in a soundproof room in the Department of Speech, Hearing and Audiology in S.D.M. Medical College, Dharwad, Karnataka using the Dell Inspiron 1525 series laptop, i ball i-630MV Multimedia Headphone with Mic i-630 MV and the Software PRAAT version 5.0.47 developed by Paul Boersma and David Weenink, Phonetic Sciences, Faculty of Humanities, University of Amsterdam, Amsterdam, Netherlands and obtained from www.praat.org. The microphone was placed about 1 cm anterior to the mentolabial fold below the breath stream. The patients were not allowed to use relief wax during the recording sessions. Three recordings of each patient were made at all the four recording sessions (T1, T2, T3, and T4) in the following sequence:
Each patient was asked to record a short introduction of him/her that comprised of name, age, educational qualification and corresponding address.
The list of 58 words from the Test of articulation in Kannada used in S.D.M. Medical College and Hospital, Dharwad, Karnataka was used as speech stimulus. The words were presented to each patient in a different order at each recording session to prevent them from memorizing the words.
Four words containing/s/sound (“shartu”, “brush”, “surya” and “bassu”) were selected from the list of 58 words from the Test of Articulation in Kannada and the subjects were asked to read those words which were then recorded at the four recording sessions.
Objective analysis of articulation using PRAAT
The Four words “surya”, “brush”, “surya” and “bassu” were selected from the list of 58 words from the Test of Articulation in Kannada. Acoustic analysis of the/s/sound in the initial position of the word “surya” (W1) and the middle position in the word “bassu” (W2) was performed by digital spectrographs. The assessment of/s/in the terminal position was not done since no Kannada word ends with this fricative. The/s/sound was selected since it is considered well suited for evaluating speech performance, and because this fricative is considered especially sensitive to morphological changes in the maxillary incisors and is common in most languages throughout the world.
The patients in both groups-LI (lingual) and LA (labial) read the standardized text aloud at T1, T2, T3 and T4. The Recorded speech samples were saved and assessed using PRAAT 5.0.47. Spectrography[8] is a technique widely used in phonetic research to prepare spectrogram or voice print. Sound intensity is measured on a spectrogram by darkness of shading. Wide-band spectrography was used to analyze the upper boundary frequency of the fricative/s/. This parameter is defined as the maximum frequency of the band width of the fricative sound, represented in the wide-band spectrogram as the range of maximum greyness. The/s/sound was selected for spectrographic analysis since this fricative is considered especially sensitive to morphological changes in the maxillary incisors and is common in most languages throughout the world.[1,9,10,11]
Semi objective auditive analysis of the articulation by four Speech Language Pathologists and Audiologists
Four clinical judges, two males and two females, trained in speech pathology listened independently to the recording of 58 words. The recordings were played in a random manner, thereby preventing the identification of patient or treatment period of which the recording was being presented. Each test syllable was judged for addition, omission, substitution and distortion on a five-point scale ranging from non-pathologic to highly pathologic speech performance. A mean of the score of each patient at a given time was used for statistical analysis. The scale used had the following classification grades:[4]
Grade 1-Non-pathological speech performance.
Grade 2-Slightly pathological speech performance.
Grade 3-Moderately pathological speech performance.
Grade 4-Pathological speech performance.
Grade 5-Highly pathological speech performance.
Subjective evaluation of speech by four laypersons
The subjective evaluation of speech was performed by four blinded individuals who were randomly selected from the first B.D.S. students of S.D.M. College of Dental Sciences, Dharwad, Karnataka. These individuals did not have any training in speech and hearing pathology. They were independently asked to rate the speech performance using the aforementioned scale. A speech stimulus was said to be pathological if it was perceived as less clear. The recordings made at T1, T2, T3 and T4 of both the LI and LA groups were played in a random manner to the evaluators.
The statistical analysis was performed using SPSS 17.0 for Windows (SPSS, Chicago, IL, USA). A mean score for each time was calculated for both groups and used for statistical analysis. The Kendall coefficient of concordance W was used to measure the level of agreement between the 4 blinded evaluators. A high degree of agreement was found between them for both semi-objective and subjective method. The Mann-Whitney U-test for independent samples was used to assess the significance difference between the labial and lingual appliances at T1, T2, T3 and T4. A speech alteration with P < 0.05 was considered to be significant.
RESULTS
For ease of presentation and convenience of comparison the results have been tabulated and presented as:
Objective analysis of articulation using PRAAT
Semi objective auditive analysis of the articulation by four speech language pathologists and audiologists.
Data of only those groups of consonants are put forth for publication in this paper where a significance difference between the two groups studied was noted.
Subjective evaluation of speech by four laypersons.
DISCUSSION
The discussion of this study has been done under.
Overview of phonetic terminologies.
Critical appraisal of the previous studies.
Interpretation of the results and comparison with the previous studies.
Limitations of the study.
Clinical recommendations.
Overview of phonetic terminologies
Sound can be considered as a series of vibrations of the air of such frequency, or pitch that is audible to the normal human ear. Speech is the vocalized form of human communication. It is based upon the syntactic combination of lexical and names that are drawn from very large (usually >10,000 different words) vocabularies.[12] Before proceeding into the discussion further, a traditional distinction between two major classes of sounds, that is, vowels and consonants would be described. A vowel is a sound that is produced with vocal cord vibration. The word consonant suggests – again, on a strictly etymological basis – that the respective sound does not have an articulatory autonomy, or to put it differently, has to be pronounced in association with other sounds. The laryngeal sounds get amplified by the oral cavity which functions as a resonator in case of vowels, while in case of consonants, it reduces the resonance of the laryngeal sounds, a noise-like effect being produced by the intercession of oral articulators. it is postulated that the main distinction between vowels and consonants is that, while we utter a vowel, the outgoing airstream does not meet any major obstacle or constriction in its way from the lungs out of the mouth and the articulation of the sound allows spontaneous voicing, whereas the articulation of a consonant always involves some kind of blocking of the airstream. Traditionally, the three basic criteria that have been used in the articulatory description of a consonant are vocal cord vibration (voicing), the place of articulation and the manner of articulation.
The manner in which this obstruction is achieved while producing consonants can be of different kinds. Plosives are the sounds produced with a complete closure of the vocal tract followed by a sudden release of the air. Fricatives are the sounds produced by an incomplete closure of the vocal tract. As the narrowing of the tract is incomplete and a passage is left for the air to go out, the pressure building up in the case of plosives is absent. The sound is uttered not with a sudden burst, but continuously. Since, their articulation is accompanied by friction between the airstream and the speech organs they are therefore called as fricatives. A major distinction between the fricatives and the stops is that the fricatives are continuous, non-abrupt sounds, so their articulation can be, at least theoretically, continued indefinitely. Affricates are the next major group of consonants that can be identified on the basis of the manner of articulation. Affricates combine the features of the two previous classes of sounds, since their articulation starts like that of a plosive, by a complete blockage of the airstream, but continues like that of a fricative, as the next stage does not involve an abrupt release of the air, but a gradual one. Labial sounds are the sounds produced with the participation of the lips as active articulators. Bilabial sounds are the sounds produced by the use of both the lips as active articulators.[13] Labio-dental sounds are articulated with the help of both the lips (the lower one, more precisely) and the (upper) teeth. The interdental sounds are the sounds where the teeth participate as passive articulators. They can more precisely be called as apico-interdental sounds. Alveolar sounds are produced in the region immediately behind the teeth by placing the tip of the tongue against the alveolar ridge. If the active member (the apex of the tongue) is also specified, we can call them apico-alveolar. Palatal sounds are produced when the tongue approximates the hard palate. Velar sounds are those which are produced with the body of the dorsum of tongue contacting against the region of the soft palate or velum. Glottal sounds are the sounds produced in the region of the glottis. Blends are the words that combine two (rarely three or more) words into one, deleting materials from one or more of the source words.[14]
Critical appraisal of the previous studies
Lingual orthodontic patients are usually informed that there may be some tongue discomfort and speech difficulty associated with the insertion of the appliance. However, the intensity and duration of the problems are not yet entirely clear and orthodontists are still dubious of the patient's ability to adapt to the lingual brackets.[15]
Various studies have reported restrictions in oral comfort,[10,11,15,16,17] mastication[10,11,16,17,18] speech,[10,11,16,17,19] and oral hygiene[9,10,16] with lingual orthodontic treatment. These studies, however, display certain drawbacks. Figurative results were absent,[16] they were case reports[9] or the design was retrospective,[10,11,18,19] which may have caused the primary negative experiences on the part of patients to have lost its significance in retrospect.[20]
Fujita[16] assessed 20 patients, who had been under treatment for 3 months or more with labial or lingual treatment, for their difficulties experienced during the treatment using a questionnaire survey. Most of the patients in both the group agreed that they did not have any speech difficulty after 3 months. However, unlike the labial patients, the lingual patients did report pronunciation difficulty. Again, this study did not quantify subjective or objective difficulties in speech and no statistical tests were used to compare the two groups. Besides, the negative effect on perception would have reduced when evaluated in retrospect.
Mariotti[21] did an extensive comparison between eight labial patients and 13 lingual patients using semi-objective assessment by three speech pathologists. Although the labial appliances did not cause any speech change, the lingual appliances caused a statistically significant speech deterioration that was limited to a period of less than 1 month for/s/, /sh/, /t/, /d/, /th/ sounds. Besides, the lingual patients, with both the arches bonded at the same appointment, had greater difficulty in adapting. This study, though extensive, did not use any objective assessment method.
Sinclair et al.[10] used objective spectrography, semi objective assessment by the speech pathologist and a subjective assessment by questionnaire survey to assess patients’ response to lingual appliance. This study reported that all patients had speech difficulty which was statistically significant immediately after bonding and after 48 h. The difficulty in most of these patients subsided by the end of 1st week. This study, however, did not use labial group for comparison. Besides, in the self-administered questionnaire, the possibility of patient to miss-rate their speech performance, depending upon their anxiety status at the time of examination, could not be ruled out.
Interpretation of results and comparison with previous studies
Objective evaluation of articulation
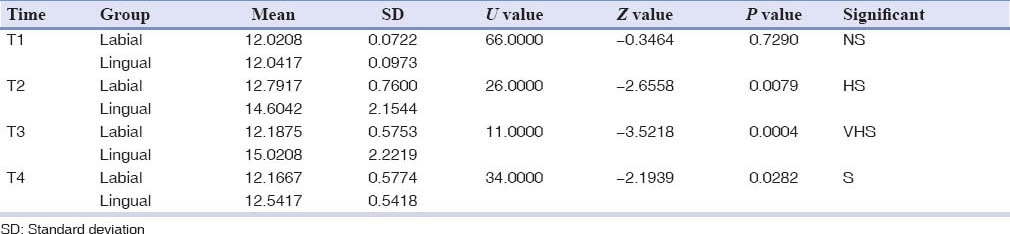
/s/sound in the initial position got equally affected in both the groups at all the time interval evaluated and no statistically significant difference was observed between the two groups at any of the time interval evaluated (P > 0.05) [Table 1].
Table 1.
Spectrographic assessment of the “s” sound in the initial position of “surya”
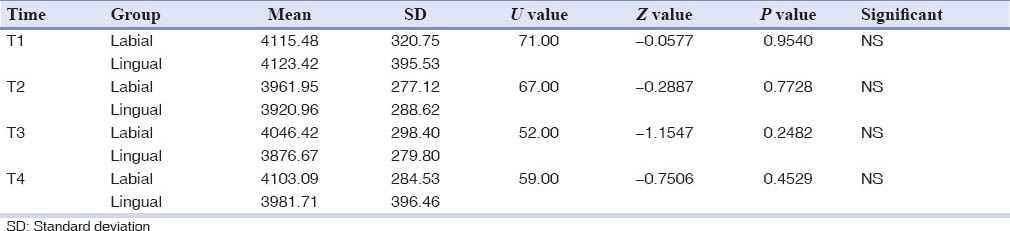
However,/s/sound in the middle position was affected to a significantly greater level in lingual group at T3 (P < 0.001) and T4 (P < 0.01) [Table 2].
Table 2.
Spectrographic assessment of the “s” sound in the middle position of “bassu”
Our findings were in accordance with the findings of Hohoff et al.,[1] Sinclair et al.[10] and Erb[19] and Seifert et al.[22] but in disagreement with the findings of Mariotti.[21]
Impaired/s/sound production extending from a period 1-3 weeks have also been reported in lingual patients by Hohoff et al.[1] and Sinclair et al.[10] This wide time interval for the speech to return to pre-treatment level may be attributed to the linguistic differences existing between the different languages of the world.[15] No studies were found assessing the effect of labial appliance on speech using spectrography. The speech in the labial group was shown to be immediately affected with the appliance placement unlike the findings of Mariotti,[21] who showed that labial appliance do not have any effect on the speech production. This difference in findings can be attributed to the presence of transpalatal arch[15] causing highly significant drop in frequency of the sound produced, which however, returned to the pre-treatment level in 1 week. This was in accordance with the findings of Erb[19] and Seifert et al.,[22] who reported that removable orthodontic appliances have a negative effect on speech production at least for a short duration of time which amounted for 2 weeks in their study.
Since both groups caused an equal impairment in sound production immediately after the initiation of treatment (shown by the absence of statistical difference between the two groups immediately after bonding, i.e., at T2), a similar modus operandi might be the pathomechanic functioning as proposed by Sinclair et al.[10] being, breaking of the consonant air flow (frication) as the tongue encountered the unfamiliar appliance leading to lowering of the noise frequency band that contained most of the consonant energy and thus producing a sound with lowered resistance and reduced overall intensity of consonants. Both groups show a greater drop in mean frequency of/s/sound in the middle position of the word (In “bassu”) than the initial position (In “surya”) which may be due to the greater pressure which the tongue has to exert against the articulatory apparatus during the production of/s/when it comes in the middle of a word. This was analogous to the findings of Sinclair et al.,[10] who compared the initial and final consonants and reported that the final consonants were more affected than the initial by lingual brackets.
Semi-objective auditive analysis of the articulation
The semi-objective analyses of articulation involved the assessment of various vowels, consonants and blends from Kannada articulation test using the Likert Scale, wherein an increasing score was suggestive of increasing articulatory errors.
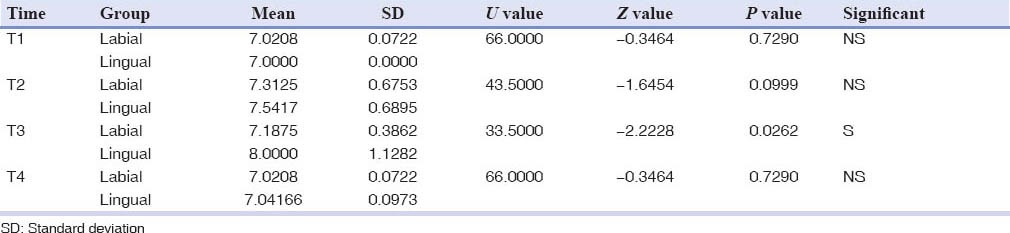
Vowels
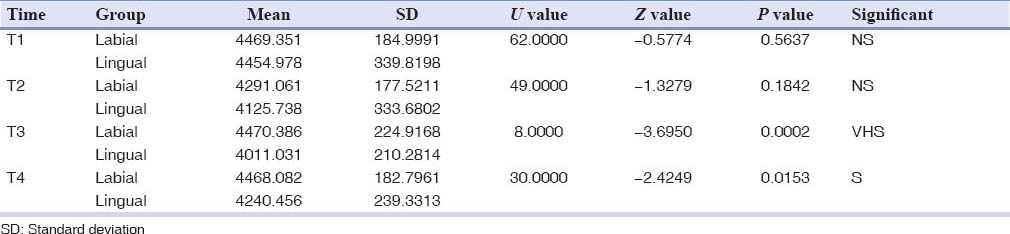
A significant difference between the two groups existed only at T3 (P < 0.01), with the lingual group showing poorer speech performance than the labial [Table 3].
Table 3.
Speech pathologist's assessment of vowels
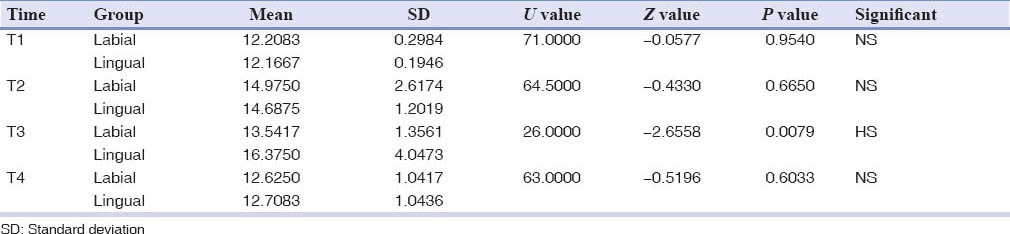
Vowel formation had only been assessed only by Fujita[9] and our findings differed from his.
Vowels are sounds produced with laryngeal vibrations and a relatively open vocal tract that is shaped to produce a particular pattern of resonance.[23] As one goes from the position necessary for making the high vowels to that for low vowels, the front of the tongue is gradually lowered and moves posteriorly. Since the frequency of the vowels is directly proportional to the length of the vocal tract, a posterior and inferior movement of the tongue, to reduce the length of the vocal tract, tends to lower the frequency of the vowel sound.[24] The most significantly affected vowels were/ii/,/i/,/u/,/a/,/uu/and/aa/in the labial group and/ii/,/i/,/a/and/o/in the lingual group. Technically speaking, vowel formation does not take place in the articulation zone in which the lingual brackets are applied; hence, they should not get affected with the placement of lingual brackets.[6,9,20] Contrary to this corollary, in our study vowel production was also found to be affected in the lingual group. This observation can probably be attributed to the place of tongue contact during their production and the effect of co-articulation. The tongue contacts the palate in its antero-superior part during the production of/i/and/e/where it came under the influence of the lingual brackets. Tongue contact in the production of/u/is located in the postero-superior part of the palate which is being influenced by the trans-palatal arch in the labial group, thus shifting inferiorily to lower the tongue volume and causing a change in its enunciation.
“Co-articulation” is the phenomenon in speech in which the attributes of successive speech unit overlap in articulatory or acoustic patterns. Hence, one feature of speech unit may be anticipated in the production of earlier unit in the string (anticipatory or forward coarticulation) or retained during production of a unit that comes later (retentive or backward coarticulation). In our case, this effect of coarticulation comes into picture where the succeeding (as/l/in Illi) or preceding (as/l/in Eli) consonant sound affects and brings about the change in the associated accompanying vowel sound./l/is an alveolar consonant[24] and the tongue tip moves anteriority towards the alveolar ridge in anticipation of its production, where it contacts the lingual brackets leading to its impaired production which is reflected as distorted production of the entire syllable. The vowel sound production in our study was below the pre-treatment level even after 1 month in both the groups unlike in Fujita's study,[9] wherein he stated that the pronunciation of /i/, /u/ and /e/ was affected on the first 4 days of lingual bracket placement and returned to pre-treatment level as early as the 6th day. No study was available to make such a comparison in the labial group. This variability in timing for the speech to return to normal could be due to pronunciation differences in different languages evaluated.[15]
Consonants
Kent and Read[25] classification based on the place of articulation of consonants was deemed most appropriate and used in this study. The consonants were grouped as glottal, velar, palatal and alveolar, inter dental, labio dental and bilabial.
An inter group comparison between the labial and the lingual group for glottal, velar, interdental, labiodental, bilabial did not show any significant difference between the two groups at any of the time intervals evaluated.
A highly significant difference (P < 0.01) between the two groups was present at T3 and T4 for the palatal consonants, with the lingual group being worst of the two [Table 4].
Table 4.
Speech pathologist's assessment of the palatal consonants
The most affected palatal consonants in the labial group were/sh/,/ch/and/ja/and in the lingual group were/sh/,/r/,/ch/and/ja/.
The alveolar consonants also showed a significant difference between the labial and the lingual group at T2 (P < 0.01), T3 (P < 0.001) and T4 (P < 0.05) [Table 5]. The most significantly affected sounds in the labial group were/s/and/l/, while those in the lingual group were/s/,/l/,/t/and/d/. As against the palatal sounds the significant difference observed in the alveolar consonants as early as T2 can be reasoned by the fact that the effect of lingual appliance is more pronounced in the region of anterior alveolus where the arch constricts than in the posterior alveolus and the palatal area which form the site of production of the palatal consonants.
Table 5.
Speech pathologist's assessment of the alveolar consonants
Although the orthodontic treatment does not affect the place of articulation of the velar sounds, the effect on it might be attributed to the initial difficulty caused to patients by both the labial and lingual appliances. This hypothesis might further be supported by the fact that both groups are equally affected. After an initial adaptive phase, which lasted for a week, the velar sounds return to normal.
Since the orthodontic treatment does not have any influence on the zones of articulation of glottal sounds no changes were seen in them.
The interdental sounds did not show a statistically significant difference in the increase in misarticulation between the groups. However, the numbers of misarticulations produced were more in the lingual group than the labial.
The bilabial and the labiodental sounds also showed an increase in misarticulation limited mainly to the labial grop and were not statistically significant. These minimal misarticulations can be attributed to the altered touch perception of the lips when they come in contact with the labial brackets.
No studies are available to the knowledge of the authors which have done a detailed analysis of various consonant subgroups individually.
The fricatives in general and the palatal and alveolar sounds in particular, were seen to be most affected by both the lingual and the labial appliances. This alteration in the sound production can be accounted-for by their place of production. The palatal fricatives are produced by the dorsum of tongue contacting the palate and the alveolar fricatives are produced by the tip of tongue contacting the alveolus. The articulatory errors produced in both these consonant were comparable between the labial and the lingual groups at T2 (immediately after bonding). Whereas the labial group showed a rapid improvement returning to nearly pre-treatment levels in a week's time, the lingual group continued to deteriorate until T3 (1 week after bonding) and improved thereafter. However, the scores in the lingual group were still significantly below the pre-treatment level, even after 1 month, for both of these consonants.
The aforementioned findings apparently suggest that the labial appliances cause comparable speech changes as the lingual appliances. However, this may be a delusive assumption and challenged by the finding that the bilabial and the labio dental sounds are not getting significantly affected in the labial group. Since the place of articulation of these sounds involves a direct interaction between the labial brackets and the articulate (lips and teeth), they should get significantly affected, had the labial appliance been a hindrance to the articulatory apparatus. Based on this illation, it can be inferred that the labial brackets per se do not bring about significant articulatory changes and the changes observed in the labial group could be attributed to transpalatal arch used in our study.
This reasoning is supported by the findings of Caniklioglu and Oztürk et al.[15] who stated that the speech difficulty encountered in the labial group could be attributed to TPA and Nance appliance used in combination with labial orthodontic appliance. Mariotti[21] also stated that the labial appliances do not cause any speech changes. There was no mention of any anchorage reinforcer being used in her study either. Erb,[19] Stratton and Burkland[26] and Haydar et al.[27] have also stated in prosthetic literature that the removable prosthodontic or orthodontic appliances cause an initial phase of speech difficulty when they encroach upon the tongue space.
Blends
An inter group comparison between the labial and the lingual groups showed a significant difference between the two groups to be present only at T3 (P < 0.05), with the lingual group exhibiting poorer articulation of the two [Table 6].
Table 6.
Speech pathologist's assessment of the blends
Blends were not evaluated previously by any of the studies.
Blends are compound sounds where two or three consonants are blended together and each consonant sound may be heard in the blend. The changes observed in blends may possibly be due to the effect of co-articulation.
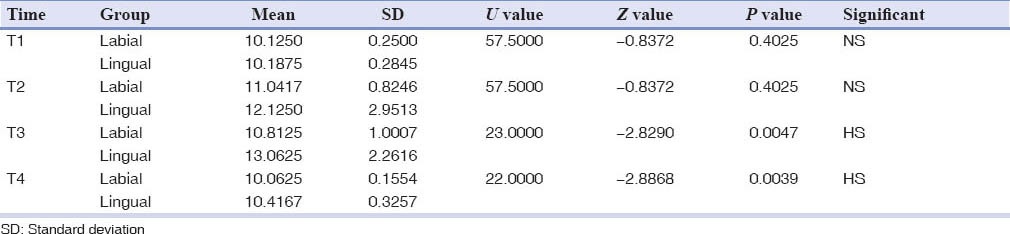
Subjective evaluation of speech
Likert scale was used for the speech assessment by four laypersons, wherein an increasing score suggested deterioration of the speech performance. An inter group comparison made between the labial and lingual group showed a significant difference between the two groups at T3 (P < 0.01) and T4 (P < 0.05) [Table 7].
Table 7.
Speech assessment by the layperson
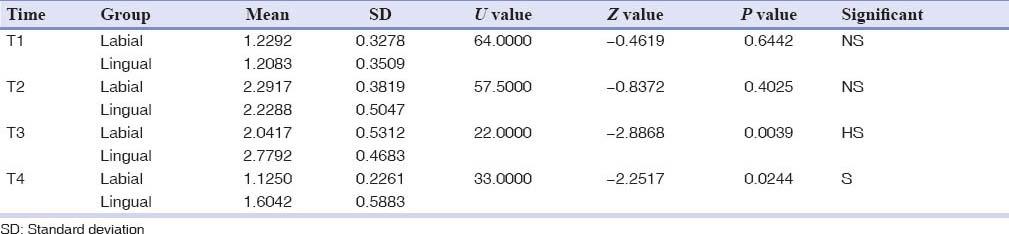
The subjectively perceived disturbances in the sound formation, caused by lingual brackets, which were recorded in our study, have been reported in the previous studies, with varying information on the duration of the disturbances and the number of patients affected,[4,10,15,16] which might be due to variations in the study design (prospective vs. retrospective) and the multifactorial etiology of speech disturbance. The information imparted by these studies using a self-administered questionnaire should be interpreted with caution since the patients tend to be pre-occupied with their speech and may overrate their level of speech discomfort.[1]
Fujita[16] reported the most popular answer from a questionnaire administered to his patients undergoing labial and lingual orthodontics, where all patients undergoing labial orthodontics agreed that their speech returned to normal within a week's time and those in the lingual group reported that they did not experience any speech difficulty after a month. Hohoff et al.[1] used patients’ close contacts (friends and family) for a questionnaire based evaluation showed that the patients’ close contacts found the worst speech performance 24 h after bonding and the speech improved over duration of 3 months. However, this study had a serious drawback of evaluating the speech after 3 months and the change in speech between the 24 h and 3 month period was not done. Besides, close contacts were used for the study and it is likely that prolonged stay with the patient may nullify or mask the speech changes which can easily be perceived by a stranger or a person who does not meets the patient so often.
It is also conceivable that the difference in bracket positioning techniques could play a role in the level of speech discomfort experienced. With BEST positioning technique, the space for the tongue is restricted more than TOP system, hence, the former causes more alteration in the patients’ speech.[1,6,28] However, no such comparison could be made in our study as a single bracket positioning method using TAD-BPD machine was used and no studies using and comparing this machine with others were found in the literature search.
Strength of this study
By combining an objective, semiobjective and a subjective method, an effort was made to minimize bias due to patient or investigator related misinterpretation. A high degree of inter-assessor agreement was present among the evaluation done by speech pathologist and the layperson in their respective groups as assessed by Kendall coefficient of concordance W.
The objective methodology used, i.e., method I (spectrography) is a sophisticated technique to evaluate the speech performance and verifies that the speech changes reported by method II (speech pathologist assessment) and method III (lay person assessment) do actually exist and are not based solely on the subjective perceptions.
This is the first study to assess sound (spectrography), articulation (speech pathologists) and speech (lay person) changes between the labial and lingual group.
This study is the first study in orthodontic literature that evaluates and compares all groups of speech sounds namely, vowels, consonants and blends between any appliance system in-toto.
Limitations of this study
A convenience sampling method was used to recruit the samples.
Sample size was restricted to 12 per group. Since the lingual technique was relatively new at the centre of study, the lack of sufficient expertise, the high cost involved in the treatment and the strictness of inclusion criteria especially the clearance from speech language and hearing pathologist was a major limitation for inclusion of subjects in this study and thus the use of convenience and judgement sampling method.
Sexual dimorphism and the effect of age on phonetic pattern were not assessed on the ground that such variation have been reported to be absent by a previous study besides the limitation of sample size due to aforementioned reason. Moreover, its absence cannot be objectively proven unless assessed keeping in light the fact that male and female vary in their level of tolerance and acceptability of pain.
Prospective phase of study lasted only for 1 month in this study due to technical limitations. A protracted and regular period of observation till the treatment ends may actually give an insight into the pattern of speech change due to lingual therapy and is acknowledged as a major limitation of this study.
This study was mainly designed to objectively quantify the perception of “others” to the speech of patients wearing lingual appliance than “self” perception by the patient so the patients or their close contacts were eliminated from making any assessments. However the patient's feedback and perception of speech by close contacts may be very important especially during the initial adaptive phase of therapy to console the patient that their speech may not be sounding as erroneous as they perceive.
This study involved the use of transpalatal arch in the labial group to reinforce anchorage. The use of transpalatal arch could have a major effect on the speech of the patient in the labial group. The labial group may have not shown the same changes had this been eliminated. This limitation is also acknowledged in light of the fact that prosthetic and removable orthodontic appliances which encroach upon the palatal space do bring a temporary speech alteration.
Speech changes observed in this study were explained mainly on the basis of alteration in the place of articulation. However, the multifactorial etiology of these changes observed (as motivation for treatment, psychology of patient, tongue soreness, type of malocclusion etc.,) cannot be ruled out and may have acted as confounding variables in our study. Some of these viz. tongue soreness, pain tolerance and motivational levels could be a major determining factor producing speech alterations, which were not assessed in this study.
The stereognostic and psychological status of the evaluators that could have affected their ratings was not assessed in this study.
The correlation between the results of studies done in the European and Indian languages may not be absolutely appropriate since every language has its own phonetic pattern, for example, there is more stress on dentoalveolar apparatus when speaking Arabic than English. Besides, different dialectic variations also exist. However, the results obtained here could act as a guideline for researchers in different languages. The only other way to eliminate this limitation is to formulate test material with common words/text in different languages and use it for assessment in their respective native speakers. However, the individual speech sounds will have the same pattern and place of production in different languages of the world, for example,/s/produced in Kannada, English or French would always involve the pressing of tongue against the palatal surface of maxillary incisors hence would show the same result done in any language, hence its universal applicability.
The objective assessment was limited only to/s/sound and may be present in other sounds as well which may be present in other sounds as well.
Owing to the unavailability of articulate sound classification in Kannada, the classification for English sounds was used.
Clinical recommendations
The clinical recommendations which can be given based on this study are summarized as under:
Patients must understand before treatment that there will be some inconvenience and discomfort with the lingual appliance. However, too much pretreatment emphasis on potential problems can become a self-fulfilling prophecy.
The orthodontist should closely evaluate the patient's speech immediately after bonding because patients with severe speech distortions, at this point, often take the longest to adapt.
Considerable counselling may be required during the first few days of treatment, when the discomfort due to the lingual appliance peaks up. Patients should be forewarned about the initial difficulty of making telephone calls and giving verbal presentations.
Patients should be advised to be forgiving of their own speech problems at the beginning of the treatment. They should speak more slowly and accept that some sounds such as/s/,/l/and/z/will be hard to communicate clearly for a few days.
One should avoid the use of auxiliaries such as transpalatal arch and Nance appliances along with lingual brackets as far as possible. Mini screws and implants should be considered more often to reinforce anchorage when using this technique.
CONCLUSION
The null hypothesis that there is no difference between the speech changes produced by the labial and lingual appliance was thus refuted by this study.
Both the lingual and the labial appliance systems showed a comparable speech difficulty immediately after bonding. While the speech difficulty lasted for approximately a week in the labial group, the lingual group continued to experience discomfort even after a month. The difficulty encountered in the labial group was mainly due to the use of TPA and may not exist if treatment in the said group is done eliminating this, and restoring other means to reinforcer anchorage.
Our results suggest a need of detailed briefing on the possible extent and duration of changes in the articulation resulting from the placement of lingual brackets, especially for patients who are in a “speech-intensive” profession as front desk officers and public speakers.
Such detailed briefing will protect both orthodontists and patients opting for lingual treatment from misconceptions and disappointments about articulation problems and might enhance the patient's and orthodontist's satisfaction with the lingual technique.
It is necessary that the orthodontist's staffs empathize with the patient during the initial phase of adaptation.
Lingual appliances do cause more speech changes than the labial appliance and the patient must be well informed for this. A detailed briefing may minimize early disappointment. Finally, the bottom line is a truthful clinician and a well-informed patient makes the best combination for the success of treatment.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Hohoff A, Seifert E, Fillion D, Stamm T, Heinecke A, Ehmer U. Speech performance in lingual orthodontic patients measured by sonagraphy and auditive analysis. Am J Orthod Dentofacial Orthop. 2003;123:146–52. doi: 10.1067/mod.2003.12. [DOI] [PubMed] [Google Scholar]
- 2.Seifert E, Runte C, Lamprecht-Dinnesen A. Dentistry and speech production. Correlations between the morphology of the articulation zone and acoustics exemplified in/s/articulation. J Orofac Orthop. 1997;58:224–31. doi: 10.1007/BF02679963. [DOI] [PubMed] [Google Scholar]
- 3.Hohoff A, Stamm T, Goder G, Sauerland C, Ehmer U, Seifert E. Comparison of 3 bonded lingual appliances by auditive analysis and subjective assessment. Am J Orthod Dentofacial Orthop. 2003;124:737–45. doi: 10.1016/j.ajodo.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Wiechmann D, Gerss J, Stamm T, Hohoff A. Prediction of oral discomfort and dysfunction in lingual orthodontics: A preliminary report. Am J Orthod Dentofacial Orthop. 2008;133:359–64. doi: 10.1016/j.ajodo.2006.03.045. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs R, Bou Serhal C, van Steenberghe D. Oral stereognosis: A review of the literature. Clin Oral Investig. 1998;2:3–10. doi: 10.1007/s007840050035. [DOI] [PubMed] [Google Scholar]
- 6.Hohoff A, Stamm T, Ehmer U. Comparison of the effect on oral discomfort of two positioning techniques with lingual brackets. Angle Orthod. 2004;74:226–33. doi: 10.1043/0003-3219(2004)074<0226:COTEOO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Gange P. Bonding in today's orthodontic practice. J Clin Orthod. 2006;40:361–7. 357. [PubMed] [Google Scholar]
- 8.Koenig W, Dunn HD, Lacy LY. The sound spectrograph. J Acoust Soc Am. 1946;17:19–49. [Google Scholar]
- 9.Fujita K. New orthodontic treatment with lingual bracket mushroom arch wire appliance. Am J Orthod. 1979;76:657–75. doi: 10.1016/0002-9416(79)90211-2. [DOI] [PubMed] [Google Scholar]
- 10.Sinclair PM, Cannito MF, Goates LJ, Solomos LF, Alexander CM. Patient responses to lingual appliances. J Clin Orthod. 1986;20:396–404. [PubMed] [Google Scholar]
- 11.Fillion D. Improving patient comfort with lingual brackets. J Clin Orthod. 1997;31:689–94. [PubMed] [Google Scholar]
- 12.Speech. 2010. [Last updated on 2010 Oct 20; Last cited on 2010 Oct 20]. Available from: http://www.en.wikipedia.org/wiki/Speech .
- 13.Dan M. English Phonetics and Phonological Theory-20th Century Approaches. Bucureşti: [monograph online] Universitatea din Bucureşti. 2003. [Last cited on 2010 Nov 20]. Available from: http://www.ebooks.unibuc.ro/filologie/mateescu/cuprins.htm .
- 14.Speech. 1995. [Last updated on 1995; Last cited on 2010 Oct 20]. Available from: http://www.uv.es/EBRIT/macro/macro_5005_97_1.html .
- 15.Caniklioglu C, Oztürk Y. Patient discomfort: A comparison between lingual and labial fixed appliances. Angle Orthod. 2005;75:86–91. doi: 10.1043/0003-3219(2005)075<0086:PDACBL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Fujita K. Multilingual-bracket and mushroom arch wire technique. A clinical report. Am J Orthod. 1982;82:120–40. doi: 10.1016/0002-9416(82)90491-2. [DOI] [PubMed] [Google Scholar]
- 17.Miyawaki S, Yasuhara M, Koh Y. Discomfort caused by bonded lingual orthodontic appliances in adult patients as examined by retrospective questionnaire. Am J Orthod Dentofacial Orthop. 1999;115:83–8. doi: 10.1016/s0889-5406(99)70320-3. [DOI] [PubMed] [Google Scholar]
- 18.Fritz U, Diedrich P, Wiechmann D. Lingual technique – Patients’ characteristics, motivation and acceptance. Interpretation of a retrospective survey. J Orofac Orthop. 2002;63:227–33. doi: 10.1007/s00056-002-0124-3. [DOI] [PubMed] [Google Scholar]
- 19.Erb DP. Speech effects of the maxillary retainer. Angle Orthod. 1967;37:298–303. doi: 10.1043/0003-3219(1967)037<0298:SEOTMR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Hohoff A, Fillion D, Stamm T, Goder G, Sauerland C, Ehmer U. Oral comfort, function and hygiene in patients with lingual brackets. A prospective longitudinal study. J Orofac Orthop. 2003;64:359–71. doi: 10.1007/s00056-003-0307-6. [DOI] [PubMed] [Google Scholar]
- 21.Mariotti J. The speech effect of the lingual appliance. Am J Orthod. 1985;88:525–6. [Google Scholar]
- 22.Seifert E, Runte C, Riebandt M, Lamprecht-Dinnesen A, Bollmann F. Can dental prostheses influence vocal parameters? J Prosthet Dent. 1999;81:579–85. doi: 10.1016/s0022-3913(99)70213-1. [DOI] [PubMed] [Google Scholar]
- 23.Hamlet SL, Geoffrey VC, Bartlett DM. Effect of a dental prosthesis on speaker-specific characteristics of voice. J Speech Hear Res. 1976;19:639–50. doi: 10.1044/jshr.1904.639. [DOI] [PubMed] [Google Scholar]
- 24.Kent RD. Normal aspect of articulation. In: Bernthal JE, Bankson NW, editors. Articulation and Phonological Disorders. 3rd ed. Boston: Allyn and Bacon; 1993. [Google Scholar]
- 25.Kent RD, Read C. 2nd ed. San Diego: Singular Publishing Group; 1992. Acoustic Analysis of Speech. [Google Scholar]
- 26.Stratton CS, Burkland GA. The effect of maxillary retainers on the clarity of speech. J Clin Orthod. 1993;27:338–40. [PubMed] [Google Scholar]
- 27.Haydar B, Karabulut G, Ozkan S, Aksoy AU, Ciğer S. Effects of retainers on the articulation of speech. Am J Orthod Dentofacial Orthop. 1996;110:535–40. doi: 10.1016/s0889-5406(96)70062-8. [DOI] [PubMed] [Google Scholar]
- 28.Wiechmann D. Lingual orthodontics (part 1): Laboratory procedure. J Orofac Orthop. 1999;60:371–9. doi: 10.1007/BF01301249. [DOI] [PubMed] [Google Scholar]


