Abstract
Background:
The aim of this study was to determine the impact of malocclusions on oral health-related quality of life (OHRQOL) among female adolescents.
Materials and Methods:
This is an observational cross-sectional descriptive study. A total of 129 female students with age ranges between 14 and 17 years old were randomly selected from Mashhad (Iran) high schools and were asked to fill out an OHRQOL questionnaire included in four parts: Oral symptoms, functional limitations, emotional well-being and social well-being. Each participant was clinically examined to assess her malocclusion according to the index of complexity, outcome and need (ICON) and finally the data were entered to SPSS 11.5 and the relation between these two variables was assessed with Pearson correlation test. P < 0.05 was considered as statistically significant.
Results:
There was statistically significant correlation between ICON scores and quality of life (P = 0.0176). Being separately assessed, among four parts of the questionnaire, only emotional well-being was significantly correlated with the ICON score (P < 0.05).
Conclusion:
Malocclusions play a vital role in OHRQOL. However, in female adolescents among four parts of OHRQOL, emotional well-being had significant relationship with malocclusions.
Keywords: Adolescent, index of complexity, malocclusion, oral health-related quality of life, outcome and need
INTRODUCTION
Over the past decade, researchers and clinicians have focused more on the impact of oral health and disease, malocclusion, dental and skeletal appearance and treatment for those conditions on psychological and functional well-being.[1] Oral diseases and abnormalities are highly prevalent and can have not only physical, but also economic, social and psychological consequences.[2]
Since the majority of dental care conditions are not life-threatening, there is a need to evaluate the impact of dental care on quality of life (QOL) with new indices.[3]
QOL has been defined by the World Health Organization as “people's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns,”[4] Or more simply, as “a sense of well-being that stems from satisfaction or dissatisfaction with areas of life that are important to the individual”.[5]
There is little doubt about the integral impact of oral health on general health and whether it contributes to overall health-related quality of life (HRQOL). The oral cavity contributes to HRQOL both biologically and psychologically and when oral health is compromised, it can adversely affect oral health and HRQOL.[6] The more specific concept of oral health-related quality of life (OHRQOL) is the extent to which oral and paraoral conditions affect one's life. This concept has been defined as “a standard of health of the oral and related issues which enables an individual to eat, speak and socialize without active disease, discomfort or embarrassment and which contributes to general well-being.”[7]
There is a growing recognition that oral health researchers and clinicians must expand their focus on more subjective, patient-based outcomes such as QOL. As a result, researchers have increasingly worked on the role of malocclusions on OHRQOL recently, as well as the impact of orthodontic treatment on OHRQOL. Some of these authors have proved a strong relationship between malocclusions or orthodontic treatment need and OHRQOL,[8,9,10,11,12,13,14] whereas others have found no clear and direct relationship.[5,15,16,17,18,19,20]
The difference between conclusions could be due to differences in cultural, economic and social conditions, indices used for malocclusions assessment and different QOL questionnaires.[11]
Today, in order to facilitate proper treatment planning, it is necessary to provide patients with evidence-based information collected through epidemiological studies. Until date, few studies have been carried out in Iran on the relationship between malocclusions and the QOL. Therefore, this study was launched to assess the relationship between untreated malocclusions and the OHRQOL in female adolescent high school students of Mashhad (the second largest city of Iran).
MATERIALS AND METHODS
Following a pilot study on 30 students to determine sample size, 129 subjects (female, 14-17 years of age and willing to participate) were selected for this observational cross-sectional descriptive study.
A two-stage cluster sampling was done to select the participants among female students of Mashhad high schools. In this method, initially, 15 high schools were randomly selected from 7 districts and 7-10 students were picked from each high school using random-numbers table. The ratio of selected girls to the total number of students was equal for all high schools. Therefore, the chance of selecting each student was equal in the cluster.
Exclusion criteria of this study were: Mixed dentition (or impacted tooth), previous orthodontic treatment, craniofacial anomalies such as cleft lip and palate, being under 14 and over 17 years of age, untreated dental caries and poor periodontal health condition to prevent possible confusing interactions of these conditions on the participant's QOL.
The structure and goal of the study were explained to the subjects who had met the entire inclusion criteria. The proposal for this study was approved by the Ethics Committee of Mashhad University of Medical Sciences. Participants consented to participate in the study by signing the consent form.
To assess OHRQOL, a variety of questionnaires are available, e.g., Child Perceptions Questionnaire (CPQ)[21] and oral impact daily performance.[22] In this study, after evaluating different questionnaires, consultation with orthodontists and psychiatrists and considering the culture and age of participants, 43 questions were carefully selected in four sections: Oral symptoms, functional limitations, social well-being and emotional well-being, as in the CPQ of Jokovic et al.[21] The validity of the questionnaire was approved by an orthodontist and a psychiatrist and its reliability was assessed by a pilot study and the alpha Cronbach test (α = 0.85).
The Likert scale[23] was used in the questionnaire; five scores for every question that indicates the incidence of the given item in the past 3 months: 0 as never, 1as once or twice and 2, 3, 4 as sometimes, often and every day, respectively. The sum total of these points for each student yielded the OHRQOL score. The greater total score indicates the lower level of the OHRQOL and the lower total score indicates the greater level of OHRQOL. The students were given 15 min to answer the questions.
Index of complexity, outcome and need (ICON)[24] was used to evaluate the severity of malocclusions in this study. This index included five components. Students’ malocclusions were clinically examined by a single practitioner according to the ICON chart. Five scores were recorded for each student. These scores, multiplied by the specific weighing factor of that component in the five parts of ICON chart, yielded the ICON score. Higher scores indicate more severe malocclusions and lower scores indicate less severe form of malocclusions. For bias prevention, the practitioner who measured ICON of students was not informed about the OHRQOL questionnaire scores. Finally, data entered to SPSS 11.5 (SPSS Inc., Chicago, IL, USA) and the relationship between ICON scores and the OHRQOL questionnaire scores were assessed by Pearson's correlation test and analysis of variance (ANOVA). P < 0.05 was considered as statistically significant.
RESULTS
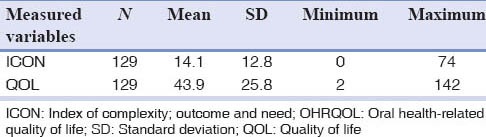
Mean values and standard deviations of ICON and OHRQOL are illustrated in Table 1. After tabulating, data were analyzed by the one-sample Kolmogorov-Smirnov normality test, which showed normal distribution of both ICON and OHRQOL.
Table 1.
Descriptive statistics of malocclusions severity ICON and OHRQOL, among students
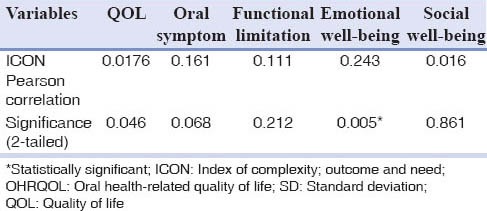
Pearson's correlation test indicated a statistically significant correlation between ICON and OHRQOL (P = 0.008). By assessing all four sections of the questionnaire, among those four sections (oral symptoms, functional limitations, emotional well-being and social well-being), only emotional well-being had a significant relationship with the ICON score (P = 0.005) [Table 2]. On the other hand, the sum of the other three components (except emotional well-being) scores showed a significant relationship with ICON.
Table 2.
Pearson's correlation and 2-tailed significance between ICON and OHRQOL and its components
Moreover, malocclusions were divided into three sets according to the ICON chart:
Acceptable occlusion: ICON <31.
Moderate malocclusions and relative treatment need: 31<ICON< 43.
Definite treatment need: ICON >43.
The mean OHRQOL scores in these three groups are illustrated in Figure 1. Students with severe malocclusions had higher OHRQOL scores, indicating a lower OHRQOL. However, when we compared the OHRQOL scores of these three groups using one-way ANOVA, there was no statistically significant difference between them (P = 0.08).
Figure 1.
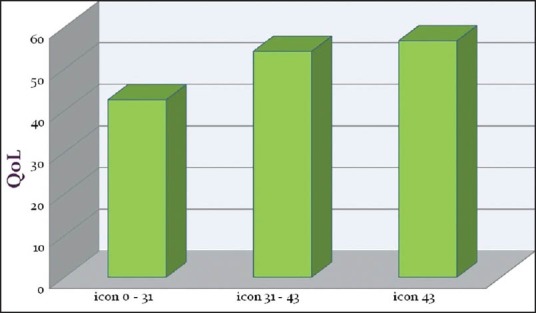
Bar diagram of quality of life levels for three severity grades of malocclusions based on the index of complexity, outcome and need
Total scores of all participants are illustrated in Figure 2, which indicates that generally a higher OHRQOL score was associated with severe malocclusions.
Figure 2.
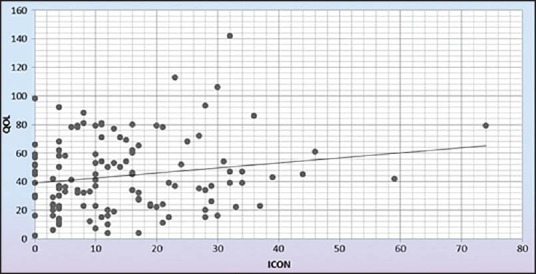
Scatter plots of total oral health-related quality of life versus index of complexity, outcome and need for the 129 students
Students with a high QOL presented all degrees of malocclusions, while those with the most severe malocclusions did not experience the lowest level of QOL, but instead, had a moderate one. Furthermore, students with moderate malocclusions were the ones who experienced the lowest level of QOL.
DISCUSSION
A large number of studies in recent years have emphasized on what was intuitively obvious; severe malocclusion is likely to be a social handicap.
Well-aligned teeth and a pleasing smile have positive impacts on all social levels and ages, whereas irregular or protruded teeth have negative impacts. Pleasing appearance can affect teachers’ expectations and as a result, students’ progress in school. Furthermore, the impact that appearance can have on one person's employability and competition for a mate are not to be neglected.[25]
This study was launched to evaluate the relationship between the severity of malocclusions and OHRQOL in a group of 14-17-year-old female adolescents of Mashhad, Iran, high schools.
In this study, ICON score was used, which emphasizes on the appearance of anterior teeth instead of the whole arch. Besides, this index uses incisor irregularity contact points and tooth displacement instead of crowding, which implies space deficiency and not necessarily the apparent misalignment of teeth. These points make ICON more useful in the objective assessment of dental appearance.
We found that students with more severe malocclusions had a lower level of QOL [Figures 1 and 2]. This significant relationship between malocclusions and OHRQOL had also been found by Heravi et al.,[11] Feu et al.,[8] Hassan and Amin,[9] Zhang et al.[26] and Bernabé et al.,[10] but not by Taylor et al.[5] in Washington adolescents. Besides, Kenealy et al.[20] after a 20-year follow-up study concluded that there was little objective evidence to support the assumption that orthodontic therapies improve long-term psychological health.
There might be reasons for such differences: First and foremost is lack of a single definition for the concept of QOL and a certain index for measurement of malocclusion in different studies. On the other hand, cultures, traditions and social behavior make different perception of beauty in each society. Finally, a high frequency of malocclusions in some races and ethnic groups can make a malocclusion normal for them.
In spite of general relationship between malocclusions and OHRQOL, we concluded that among four parts of the OHRQOL questionnaire (oral symptoms, functional limitations, emotional well-being, social well-being), only emotional well-being has a significant relationship with the ICON score (P = 0.005), while in the study on male adolescents among these four components only oral symptoms had a significant relationship with the ICON score.[11] Since girls may be more self-conscious about their appearance, the results are as expected. A study by Peres et al.[27] also found a significant correlation between malocclusions and appearance satisfaction only in girls.
Students with the most severe malocclusions did not tend to have the lowest life quality score and instead, their scores were in the middle range of QOL [Figure 2], in contrast with what might be expected. An explanation for this finding may be their adaptation to their malocclusions and hence that malocclusion could not affect their QOL. On the other hand, some students with very mild problems in occlusion had a lower level of QOL. This can be a sign of exaggeration of a simple problem in a person's mind and therefore affecting their OHRQOL and if this exaggeration does not get eliminated during orthodontic treatment, it can lead to patients’ dissatisfaction even after treatment.
Zhang et al.[19] in their study have reported similar results based on the fact that those with moderate malocclusion problems are more often despised by others. While people with severe problems usually receive sympathetic responses from others and these social attitudes have significant effects on a patient's perception of the problem.
Macgregor[28] claimed that unpleasant appearance might lead to negative responses from the society, whereas less disagreeable looks receive very different reactions, sometimes negative and sometimes positive. These unexpected reactions from the society would cause more tension. As a result, we should consider the QOL as adaptations of the patient with his living condition rather than his health condition according to a specialist's point of view.
Finally, it must be mentioned that although the results of this study support the idea of a relationship between malocclusions and a decrease in life quality, further research is needed to evaluate every aspect of orthodontic treatments impacts on the QOL.
CONCLUSION
According to this study, malocclusions play an important role in the OHRQOL in female students of Mashhad high schools. In spite of a general relationship between malocclusions and OHRQOL, among four parts of the OHRQOL questionnaire (oral symptoms, functional limitations, emotional well-being and social well-being), only emotional well-being showed significant relationship with ICON score.
Considering how patients adapt differently to their appearance and health problems, the patients with the most severe forms of malocclusion did not experience the lowest level of OHRQOL. Furthermore, those with moderate cases experienced a lower OHRQOL, in contrast to what was expected.
ACKNOWLEDGMENTS
This study was financially supported by the office of Vice Chancellor for Research of Mashhad University of Medical Science. The authors would like to thank this group for their assistance.
Footnotes
Source of Support: The authors would like to thank the Research Chancellor of Mashhad University of Medical Sciences who financially supported this research.
Conflict of Interest: None declared.
REFERENCES
- 1.Kiyak HA. Does orthodontic treatment affect patients’ quality of life? J Dent Educ. 2008;72:886–94. [PubMed] [Google Scholar]
- 2.Azuma S, Kohzuki M, Saeki S, Tajima M, Igarashi K, Sugawara J. Beneficial effects of orthodontic treatment on quality of life in patients with malocclusion. Tohoku J Exp Med. 2008;214:39–50. doi: 10.1620/tjem.214.39. [DOI] [PubMed] [Google Scholar]
- 3.de Oliveira CM, Sheiham A. Orthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescents. J Orthod. 2004;31:20–7. doi: 10.1179/146531204225011364. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Geneva: World Health Organization; 1993. Measuring quality of life: The development of the world health organization quality of life instrument (WHOQOL) [Google Scholar]
- 5.Taylor KR, Kiyak A, Huang GJ, Greenlee GM, Jolley CJ, King GJ. Effects of malocclusion and its treatment on the quality of life of adolescents. Am J Orthod Dentofacial Orthop. 2009;136:382–92. doi: 10.1016/j.ajodo.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham SJ, Hunt NP. Quality of life and its importance in orthodontics. J Orthod. 2001;28:152–8. doi: 10.1093/ortho/28.2.152. [DOI] [PubMed] [Google Scholar]
- 7.London, United Kingdom: HMSO; 1994. Department of Health. An oral health strategy for England. [Google Scholar]
- 8.Feu D, de Oliveira BH, de Oliveira Almeida MA, Kiyak HA, Miguel JA. Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop. 2010;138:152–9. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Hassan AH, Amin Hel-S. Association of orthodontic treatment needs and oral health-related quality of life in young adults. Am J Orthod Dentofacial Orthop. 2010;137:42–7. doi: 10.1016/j.ajodo.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 10.Bernabé E, de Oliveira CM, Sheiham A. Condition-specific sociodental impacts attributed to different anterior occlusal traits in Brazilian adolescents. Eur J Oral Sci. 2007;115:473–8. doi: 10.1111/j.1600-0722.2007.00486.x. [DOI] [PubMed] [Google Scholar]
- 11.Heravi F, Farzanegan F, Tabatabaee M, Sadeghi M. Do malocclusions affect the oral health-related quality of life? Oral Health Prev Dent. 2011;9:229–33. [PubMed] [Google Scholar]
- 12.Foster Page LA, Thomson WM, Jokovic A, Locker D. Validation of the Child Perceptions Questionnaire (CPQ 11-14) J Dent Res. 2005;84:649–52. doi: 10.1177/154405910508400713. [DOI] [PubMed] [Google Scholar]
- 13.Locker D, Jokovic A, Tompson B, Prakash P. Is the Child Perceptions Questionnaire for 11-14 year olds sensitive to clinical and self-perceived variations in orthodontic status? Community Dent Oral Epidemiol. 2007;35:179–85. doi: 10.1111/j.1600-0528.2006.00324.x. [DOI] [PubMed] [Google Scholar]
- 14.Johal A, Cheung MY, Marcene W. The impact of two different malocclusion traits on quality of life. Br Dent J. 2007;202:E2. doi: 10.1038/bdj.2007.33. [DOI] [PubMed] [Google Scholar]
- 15.de Oliveira CM, Sheiham A, Tsakos G, O’Brien KD. Oral health-related quality of life and the IOTN index as predictors of children's perceived needs and acceptance for orthodontic treatment. Br Dent J. 2008;204:1–5. doi: 10.1038/bdj.2008.239. [DOI] [PubMed] [Google Scholar]
- 16.Kok YV, Mageson P, Harradine NW, Sprod AJ. Comparing a quality of life measure and the Aesthetic Component of the Index of Orthodontic Treatment Need (IOTN) in assessing orthodontic treatment need and concern. J Orthod. 2004;31:312–8. doi: 10.1179/146531204225020625. [DOI] [PubMed] [Google Scholar]
- 17.O’Brien K, Kay L, Fox D, Mandall N. Assessing oral health outcomes for orthodontics – Measuring health status and quality of life. Community Dent Health. 1998;15:22–6. [PubMed] [Google Scholar]
- 18.Tsakos G, Gherunpong S, Sheiham A. Can oral health-related quality of life measures substitute for normative needs assessments in 11 to 12-year-old children? J Public Health Dent. 2006;66:263–8. doi: 10.1111/j.1752-7325.2006.tb04079.x. [DOI] [PubMed] [Google Scholar]
- 19.Zhang M, McGrath C, Hägg U. The impact of malocclusion and its treatment on quality of life: A literature review. Int J Paediatr Dent. 2006;16:381–7. doi: 10.1111/j.1365-263X.2006.00768.x. [DOI] [PubMed] [Google Scholar]
- 20.Kenealy PM, Kingdon A, Richmond S, Shaw WC. The Cardiff dental study: A 20-year critical evaluation of the psychological health gain from orthodontic treatment. Br J Health Psychol. 2007;12:17–49. doi: 10.1348/135910706X96896. [DOI] [PubMed] [Google Scholar]
- 21.Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81:459–63. doi: 10.1177/154405910208100705. [DOI] [PubMed] [Google Scholar]
- 22.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 23.Gadbury-Amyot CC, Williams KB, Krust-Bray K, Manne D, Collins P. Validity and reliability of the oral health-related quality of life instrument for dental hygiene. J Dent Hyg. 1999;73:126–34. [PubMed] [Google Scholar]
- 24.Daniels C, Richmond S. The development of the index of complexity, outcome and need (ICON) J Orthod. 2000;27:149–62. doi: 10.1093/ortho/27.2.149. [DOI] [PubMed] [Google Scholar]
- 25.Proffit WR, Fields HW, Sarver DM. ed 4. St Luis: Mosby; c2007. Contemporary orthodontics; p. 16. [Google Scholar]
- 26.Zhang M, McGrath C, Hägg U. Orthodontic treatment need and oral health-related quality among children. Community Dent Health. 2009;26:58–61. [PubMed] [Google Scholar]
- 27.Peres KG, Barros AJ, Anselmi L, Peres MA, Barros FC. Does malocclusion influence the adolescent's satisfaction with appearance? A cross-sectional study nested in a Brazilian birth cohort. Community Dent Oral Epidemiol. 2008;36:137–43. doi: 10.1111/j.1600-0528.2007.00382.x. [DOI] [PubMed] [Google Scholar]
- 28.Macgregor FC. Social and psychological implications of dentofacial disfigurement. Angle Orthod. 1970;40:231–3. doi: 10.1043/0003-3219(1970)040<0231:SAPIOD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]


