Abstract
Aim
To carry out a systematic study on the effect of different storage conditions on the number as well as the physical and functional properties of antibacterial extracellular vesicles (EVs) derived from human neutrophilic granulocytes.
Methods
Production of EVs with antibacterial properties was initiated by opsonized Zymosan A particles. The number of released fluorescent EVs was determined by flow cytometry following careful calibration. Physical properties and size of EVs were investigated by flow cytometry, dynamic light scattering and electron microscopy. Functional properties of EVs were tested by bacterial survival assay.
Results
Storage at +20°C or +4°C resulted in a significant decrease of EV number and antibacterial effect after 1 day. Storage at −20°C did not influence the EV number up to 28 days, but induced a shift in EV size and almost complete loss of antibacterial function by 28 days. Storage at −80°C had no significant effect either on EV number or size and allowed partial preservation of the antibacterial function up to 28 days. Snap-freezing did not improve the results, whereas the widely used cryoprotectants induced EV lysis.
Conclusion
Storage significantly alters both the physical and functional properties of EVs even if the number of EVs stays constant. If storage is needed, EVs should be kept at −80°C, preferably not longer than 7 days. For functional tests, freshly prepared EVs are recommended.
Keywords: storage conditions, vesicle function, antibacterial effect, extracellular vesicle, microvesicle
According to current thinking, extracellular vesicles (EVs) are formed by almost every cell type and in most living species (1). EVs represent an important intercellular communication channel that has been neglected until recently. In addition to their role in signal transfer in a broad variety of physiological and pathological processes (2–6), they also provide unique source for diagnostical purposes and offer potential new therapeutic approaches (7–9). Storability of different EVs is a critical point both for research and for medical applications, but only very few relevant data are available (10–12). There is no consensus on optimal storage conditions, such as temperature, time or application of cryoprotectants (13), despite existing recommendations (13–15).
Neutrophilic granulocytes (PMNs) play a critical role in innate immunity. They are able to detect, migrate to, engulf and eliminate various potentially harmful microorganisms. The most important weapons in this process consist of phagocytosis, production of reactive oxygen species (ROS) and release of antibacterial proteins leading eventually to killing and degradation of the foreign particle enclosed in the phagosome. We have described recently that PMNs are able to produce – upon specific stimulation – EVs that impair bacterial growth (16). The antibacterial mechanism of EVs differs from that of PMNs in significant ways: EVs do not phagocytize and do not produce ROS, but form large aggregates with bacteria (17).
This remarkable and quantifiable effect of PMN-derived EVs allowed us to carry out a detailed investigation on the effect of storage conditions not only on physical but also on functional properties of EVs.
Materials and methods
Materials
Saponin was from Merck (Darmstadt, Germany), Zymozan A, albumin, DMSO and glycerol from Sigma (St. Louis, MO, USA), sterile endotoxin-free Hank’s balanced salt solution (HBSS) from Thermo Scientific (Waltham, MA, USA) and Ficoll from Phadia (Uppsala, Sweden). All other reagents were of research grade. HBSS contained 135 mM NaCl, 4 mM KCl, 1 mM MgCl2, 2 mM CaCl2, 10 mM glucose, 1 mM Na2HPO4, 20 mM HEPES and pH=7.3. Green fluorescent protein (GFP)-expressing Staphylococcus aureus was a kind gift from Professor William Nauseef (University of Iowa, IA, USA).
Preparation of EVs from PMNs
Venous blood was drawn from healthy adult volunteers according to procedures approved by the Institutional Review Board of the Semmelweis University. Neutrophils were obtained by dextran sedimentation followed by Ficoll-Paque gradient centrifugation as described previously (18). The preparation contained over 95% PMNs and less than 0.5% eosinophils.
For production of antibacterial EVs, PMNs (typically 4.5×106 cell in 450 µL HBSS) were incubated with opsonized Zymozan A particles (5 mg added in 50 µL HBSS) for 30 minutes at 37°C on a linear shaker (80 rpm/min). After incubation, PMNs were sedimented (500×g, Hermle Z216MK 45° fixed angle rotor, 5 minutes, 4°C), and the supernatant was filtered through a 5 µm pore sterile filter (Sterile Millex Filter Unit, Millipore, Billerica, MA, USA). The filtered fraction was sedimented again (15,700×g, Hermle Z216MK 45° fixed angle rotor, 10 minutes, 4°C). The sediment was suspended in HBSS at the original incubation volume. Albumin concentration was 1 mg/mL (dissolved in HBSS) in the indicated samples.
Opsonization of Zymozan A and S. aureus
Five-milligram Zymozan A or 4.5×108/mL S. aureus was opsonized with 100 µL pooled normal human serum for 30 minutes at 37°C. After opsonization, the particles were centrifuged (8,000×g, Hermle Z216MK 45° fixed angle rotor, 10 minutes, 4°C), and washed in HBSS.
Storage of EVs
EVs induced by opsonized Zymozyan A were prepared and labelled for flow cytometric analysis as described below. Then they were suspended in HBSS and stored at different temperatures (+20°C, +4°C, −20°C, −80°C) for different periods (1 day, 7 days, 28 days). By snap-freezing, liquid nitrogen was used to freeze the samples. Samples were stored in 1.5 mL polypropylene microtubes (Sarstedt, Nümbrecht, Germany). Samples were thawed at room temperature or in 37°C water bath in case of a snap-thawed sample.
EV detection by flow cytometry
EVs were labelled with a monoclonal Ab against the alpha chain of the major PMN integrin (anti-CD11b-RPE, 1 µg/mL, Dako, Glostrup) for 30 minutes at 37°C, and then washed in HBSS.
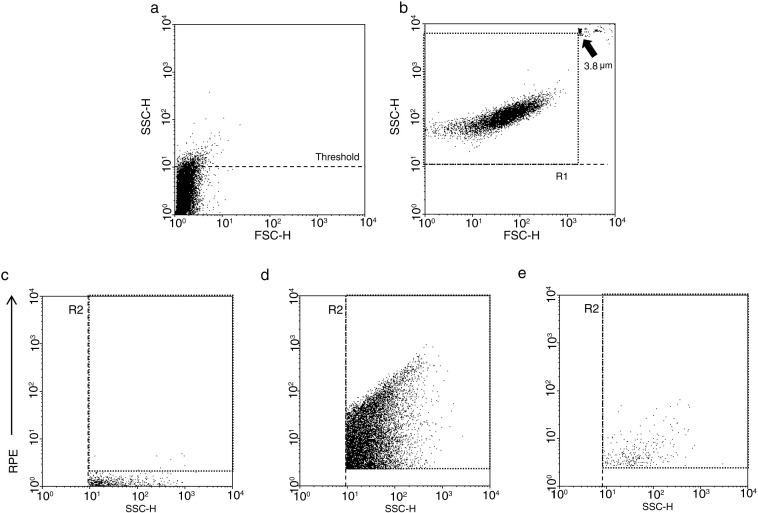
For flow cytometric characterization, a Becton Dickinson FACSCalibur flow cytometer was used. The procedure of measurement is summarized in Fig. 1. Pure HBSS medium was used for setting the threshold to eliminate instrument noise (Fig. 1a). In the next step, fluorescent beads (3.8 µm SPHERO Rainbow Alignment Particles from Spherotech Inc., USA) and green-fluorescent bacteria were detected together (Fig. 1b). The upper size limit of EV detection range was set to exclude the signals from the beads. The refractive index of biological membranes was shown to differ from that of artificial calibration beads (19,20). Therefore, in our studies, GFP-expressing bacteria were used to calibrate both the gain and the flow rate. The diameter of coccus form S. aureus was defined by dynamic light scattering (DLS). It showed a sharp distribution around 800 nm (not shown). The FACScalibure gain settings were chosen to include the entire distribution range of labelled bacteria (Fig. 1b). Although the PMN-derived EVs are mostly below 800 nm (16), we chose a significantly broader size range allowing for potential swelling or fusion of EVs during storage. The smallest fluorescent particles reliably detected by a conventional cytometer could be around 300 nm (20). The fluorescent gate was set above the signal of the control isotype antibody labelled EVs (Fig. 1c). PMN-derived EVs were enumerated and characterized in the fluorescent gate above (Fig. 1d). To confirm the vesicular nature of detected events 1% TritonX-100 detergent was used to solubilize vesicles. Non-solubilized events (around 5%) were subtracted (Fig. 1e).
Fig. 1.
Gating strategy of flow cytometric measurements. In panels a and b, side scatter is presented against forward scatter, whereas in panels c–e, fluorescence is presented against side scatter. Representative dot plots on (a) pure HBSS medium; (b) fluorescent beads (3.8 µm) and GFP-expressing S. aureus (0.8 µm) measured in parallel; (c) isotype antibody labelled fresh EVs; (d) anti-CD11b antibody labelled fresh EVs; and (e) anti-CD11b antibody labelled fresh EVs treated with 1% Triton X-100.
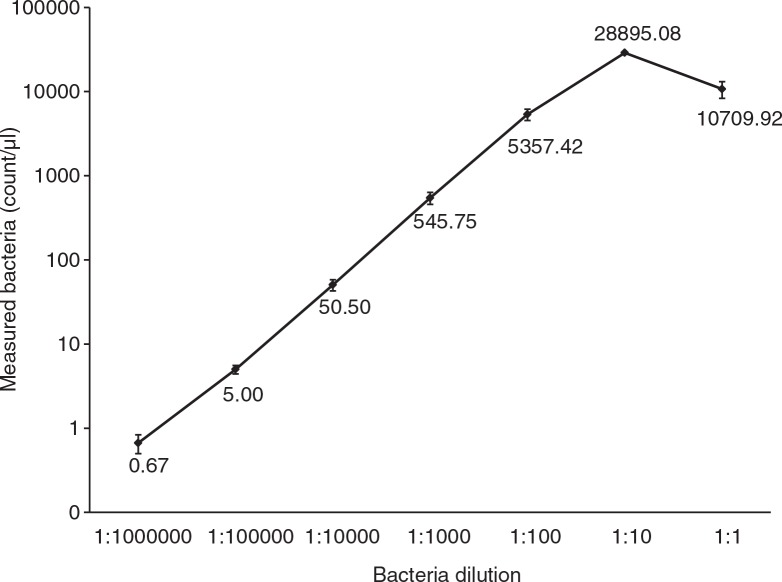
To avoid swarm detection optimal flow rate was defined with a dilution scale of fluorescent bacteria. Undiluted bacteria had an optical density of 1.00 at 600 nm. Serial 10-fold dilution of this initial solution was counted in the flow cytometer. Good correlation was observed between measured events and dilution between 1:1000,000 and 1:100 dilutions (Fig. 2). At the top of the linear phase (dilution 1:100), the flow rate was around 2,000 events/s during the measurements. In later measurements, the flow rate was held below 1,000 events/s.
Fig. 2.
Calibration of the optimal measuring range of the BD FACScalibur flow cytometer. GFP-expressing S. aureus bacteria were used for calibration. The undiluted sample had an optical density of 1.00 at 600 nm. Bars represent SEM; n=3.
Electron microscopy of EV
Pelleted EVs were fixed at room temperature for 60 minutes with 4% paraformaldehyde in phosphate buffered saline. The preparations were postfixed in 1% OsO4 (Taab) for 30 minutes. After rinsing with distilled water, the pellets were dehydrated by ethanol, including block staining with 1% uranyl-acetate in 50% ethanol for 30 minutes, and embedded in Taab 812 (Taab). After overnight polymerization at 60°C and sectioning for electron microscopy, the ultrathin sections were analyzed with a Hitachi 7,100 electron microscope equipped by Veleta, a 2 k×2 k MegaPixel side-mounted TEM CCD camera (Olympus). Contrast and brightness of electron micrographs were edited by Adobe Photoshop CS3 (Adobe Photoshop Incorporation).
Dynamic light scattering
DLS measurements were performed at room temperature, using an ALV goniometer with a MellesGriot diode-pumped solid-state laser (CVI MellesGriot) at 457.5 nm wavelength (type 58 BLD 301). The radius of the particles was calculated using sphere approximation.
Measurement of bacterial survival
EV samples in HBSS were incubated with (2.5×107/mL) opsonized S. aureus for 30 minutes at 37°C. Samples were taken at starting point and 30 minutes later. Samples were lysed in ice-cold HBSS containing 1 mg/mL saponin and frozen at −80°C for 20 minutes, and then thawed to inactivate EVs. Freezing did not impair subsequent growth of S. aureus. Lysed samples were diluted in Lysogeny Broth (LB medium; 10 g tryptone, 5 g yeast extract, 10 g NaCl in 1 L water, pH adjusted to 7.0 with NaOH), then bacteria were grown in a shaking plate reader (Labsystems iEMS Reader MF) at 37°C for 8 hours and the OD was followed continuously at 650 nm, as described earlier (18). Samples were run in 8 parallels.
Statistics
Statistical analysis was performed with STATISTICA 8.0 software with the 1-sample t-test or 2-sample t-test. All p values<0.05 were considered significant.
Results
Three structural (number, size and electron microscopic morphology) and one functional parameter of stored samples were compared to freshly prepared and immediately measured EV samples. As functional test, antibacterial capacity measurement can indicate changes in fine structure of EVs, which are not detectable with physical methods. Three different storage periods were tested. One day and one week storage are relevant for experimental and diagnostic usage of EVs; 1 month period indicates long-term storage for potential therapeutic applications.
Effect of storage on EV number detected by flow cytometry
Activation of PMNs with opsonized Zymozan A induced abundant EV production. By flow cytometry, the immediately measured EV counts were around 3,700 EVs/μL. All the stored parallels were compared to the fresh EV sample. There was a significant time-dependent decrease of vesicle number if samples were held at room temperature or at +4°C (Fig. 3a). Massive vesicle loss was evident by 7 days. In contrast, EV number was slightly elevated after 1 day storage at +4°C. Elevation of EV numbers could be due to swelling of the vesicles. There are vesicles below the flow cytometry detection limit that could be shifted to the detection range upon swelling.
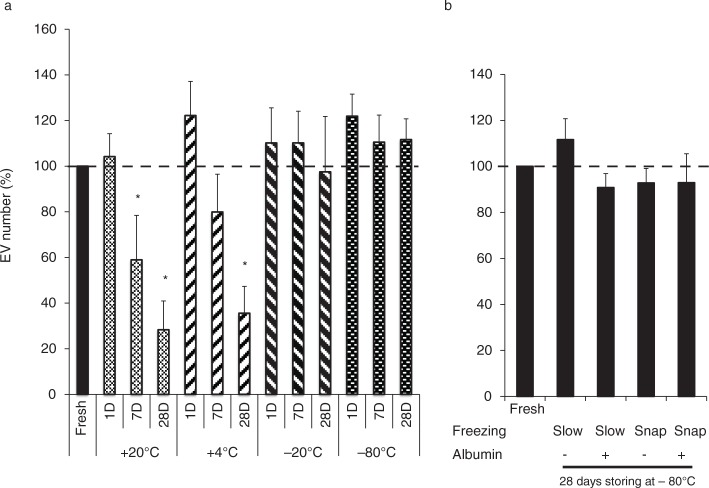
Fig. 3.
Effect of various storage conditions on the EV number. The EV number was measured by flow cytometry. The number of EVs in stored samples was compared to the fresh EV sample. (a) Effect of storage of vesicles at +20°C, +4°C, −20°C or at −80°C (n=8, or 4 in the case of −80°C, +SEM, p<0.05). (b) Effect of rapid freezing in liquid nitrogen and thawing in a 37°C water bath (snap) and presence of albumin (1 mg/mL) during storage. All samples were stored at −80°C for 28 days (n=4, +SEM).
At −20°C and −80°C, the EV number did not show any decrease up to 1 month period (Fig. 3a). Similarly, there was no change in EV number if rapid freezing in liquid nitrogen and thawing in water bath (snap-freezing/thawing) was carried out or albumin was added to preserve the EVs (Fig. 3b). Other cryoprotectants as DMSO (1%) or glycerine (5%) fully or partially lysed the EVs (not shown).
Further structural experiments were carried out only with samples stored at −20°C or −80°C because of the massive loss of vesicle number in other conditions.
Effect of storage on light scattering properties
To analyze possible changes in physical properties of EVs, characterization of the forward (FSC) and side scattering (SSC) properties of stored EV fractions was performed by flow cytometry (Fig. 4a–c).
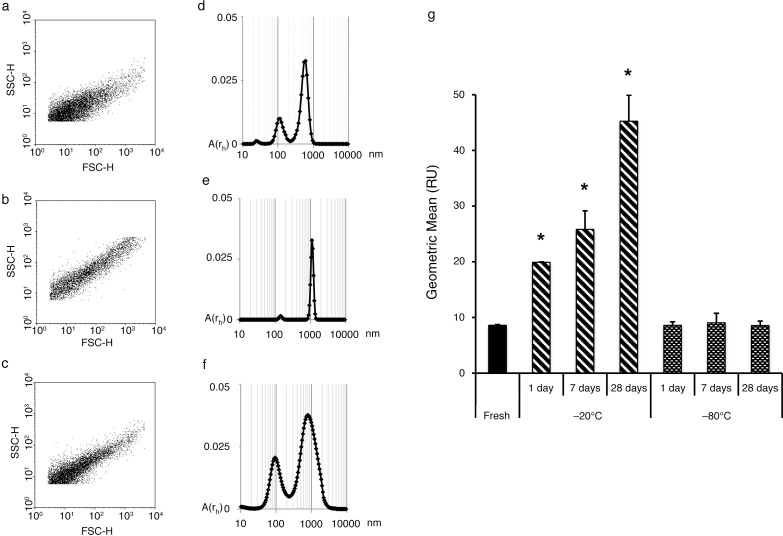
Fig. 4.
Effect of different storage conditions on light scattering of EVs. Representative dot plot shows SSC and FSC characteristics of (a) fresh EVs and (b) EVs stored for 28 days at −20°C or (c) at −80°C. DLS characteristics of (d) fresh EVs and (e) EVs stored for 28 days at −20°C or (f) at −80°C. (g) Geometric mean of cytometer detected SSC distribution of EV fractions (n=4, +SEM, *p<0.05).
Although there was no change in the number of EVs stored at −20°C, reproducible changes were seen both in FSC and SCC characteristics of the EV fraction. Compared to fresh samples (Fig. 4a), in the EV fraction stored at −20°C the events shifted to the right and upward (Fig. 4b) indicating larger events. For quantitative analysis, the geometric mean of the SSC distribution was calculated. In the case of samples stored at −20°C, a significant time-dependent increase was detected (Fig. 4g). No change of the scattering properties was detectable in the EV fraction stored at −80°C (Fig. 4c and g).
DLS is a more precise method to determine the vesicle size distribution; however, it has strong limitations in quantification (21,22). The changes indicated by FSC and SSC were confirmed by DLS. Fresh EV fraction contained 2 vesicle populations: exosome size vesicles between 70 and 200 nm and a microvesicle size population between 300 and 900 nm with a peak around 600 nm (Fig. 4d). In samples stored at −20°C, one major peak was detected around 1,000 nm (Fig. 4e). A tendency of a shift towards larger vesicles was also visible in samples stored at −80°C; however, the changes were moderate (Fig. 4f).
The shift of the EV population towards a larger size may be the result of swelling and it could represent an initial step of vesicle disruption. This swelling is concordant with previous observations at higher temperature storage (at +20°C and +4°C).
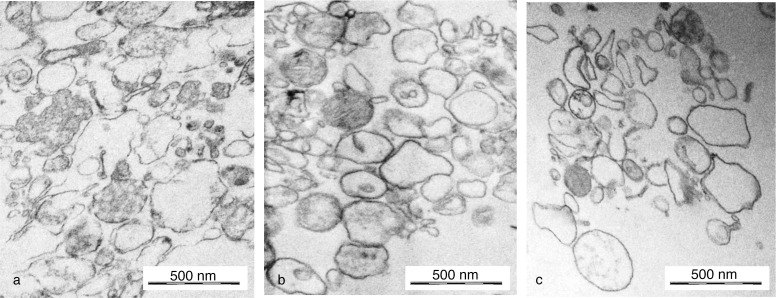
Electron microscopic characterization of stored EVs
The electron micrographs of PMN-derived, activation-induced EVs showed a heterogeneous EV population. There are vesicles in exosome (around 100 nm) and in microvesicles (200–1,000 nm) range. Some vesicles were electron dense and others seemed to be empty. There were some with “vesicles in vesicle” phenomenon. This heterogeneity was also seen in samples stored at −20°C or at −80°C. No typical and dominant changes were observed: the size distribution and the proportion of electron dense to empty vesicles were similar, as well as the occurrence of “vesicles in vesicle” phenomenon. The integrity of the visualized vesicles remained preserved in all samples. No enrichment of any typical shape (rounded, flat or indented vesicles) is visible (Fig. 5).
Fig. 5.
Representative electron microscopic images. (a) Freshly prepared EVs, (b) EVs stored for 28 days at −20°C and (c) EVs stored for 28 days at −80°C. Original magnification is 30,000×. (Black osmium aggregates are artefacts in picture b.)
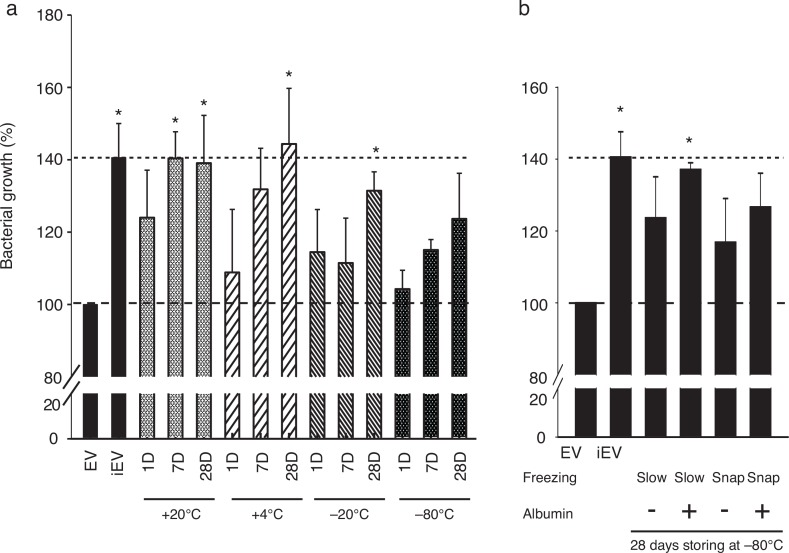
Effect of storage on antibacterial capacity of EVs
Opsonized particle activation-induced, PMN-derived EVs have a dose-dependent antibacterial effect on S. aureus and Escherichia coli as we showed earlier (16). In this study, the S. aureus survival assay was used to test the effect of storage of EVs on their biological function. Fresh EVs interfered with the bacterial growth. In contrast, bacteria could grow up on heat-inactivated EVs. In Fig. 6, all stored samples are compared to the antibacterial capacity of the fresh EVs (which is represented as 100%). All data above 100% represent an impairment of antibacterial capacity.
Fig. 6.
Effect of various storage conditions on antibacterial capacity of the EVs. Bacterial growth after co-incubation of EVs in stored samples was compared to the bacterial growth after co-incubation of the bacteria with fresh EVs. iEV represents the bacterial growth on fully heat denatured EVs as negative control. (a) Effect of storage of vesicles at +20°C, +4°C, −20°C or at −80°C (n=6, or 4 in the case of −80°C for 28 days +SEM, *p<0.05). (b) Effect on antibacterial capacity of rapid freezing and thawing (snap) and presence of albumin during storage. All samples were stored at −80°C for 28 days (n=4, +SEM).
If EVs were stored at +20°C or +4°C, the antibacterial capacity was seriously impaired after 1 day and completely lost in a 1-week period. Significant loss of antibacterial capacity was also seen in samples stored at −20°C for 1 month. In contrast to promising flow cytometric and electron microscopic characteristics, there was a tendency for time-dependent loss of antibacterial effect also in EVs stored at −80°C (Fig. 6a). Snap-freezing and thawing or presence of albumin could not preserve functionality better than slow freezing (Fig. 6b).
Discussion
A systematic study was carried out on different storage conditions for EVs. The remarkable antibacterial effect of PMN-derived EVs allowed us to apply, for the first time also, a quantifiable functional test. For the characterization of the physical properties of stored EVs, we applied flow cytometry after careful calibration. We suggest using fluorescent bacteria to set gain and gate adjustments and flow rate for calibration in the larger size range of EVs.
PMN-derived EVs could not be stored at room temperature or at +4°C for a day without loss of function although the vesicle number did not decrease yet. This observation raises the possibility that in the case of lengthy EV preparation protocols, EVs may already undergo some loss of function. Thus, the time factor should be considered when choosing the protocol and faster preparation techniques such as filtration or size exclusion chromatography (22–24) may be preferable for functional studies.
Storage at −20°C induces structural changes reflected by alteration of light scattering properties, whereas no major change was visible by electron microscopy. The shift observed both by flow cytometry and by DLS may be due to swelling of vesicles. The number of events detected in the preset gate of the flow cytometer did not change, but swelling may cause smaller vesicles to become detectable and larger vesicles to disrupt. Thus, the apparently constant number of vesicles may represent an altered population.
Storage at −80°C for 1 month resulted in no change in scattering properties and only a mild increase in the number and size of vesicles. This condition may thus be suitable for storage of vesicles for diagnostic purposes. However, the antibacterial function of the PMN-derived EVs was not completely preserved. The partial loss of function may be the result of alterations which are not expected to modify the investigated physical properties of vesicles, such as change of receptor density, surface glycosylation or microdomain pattern. Snap-freezing/thawing or presence of albumin during storage did not improve the results. In contrast, some of the well-known cryoprotectants destroyed the vesicular structure.
Taken together, our results highlight the potential changes occurring during storage of EVs and emphasize the need to also consider storage conditions when interpreting and comparing data or standardizing protocols. Fresh preparations can be recommended for functional studies.
Acknowledgements
The authors are indebted to Ms. Regina Tóth-Kun and Edit Fedina for devoted and expert technical help. Experimental work was supported by the Hungarian National Research Fund (OTKA K108382).
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Thery C, Zitvogel L, Amigorena S. Exosomes: composition, biogenesis and function. Nat Rev Immunol. 2002;2:569–79. doi: 10.1038/nri855. [DOI] [PubMed] [Google Scholar]
- 2.Raposo G, Stoorvogel W. Extracellular vesicles: exosomes, microvesicles, and friends. J Cell Biol. 2013;200:373–83. doi: 10.1083/jcb.201211138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choudhuri K, Llodra J, Roth EW, Tsai J, Gordo S, Wucherpfennig KW, et al. Polarized release of T-cell-receptor-enriched microvesicles at the immunological synapse. Nature. 2014;507:118–23. doi: 10.1038/nature12951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robbins PD, Morelli AE. Regulation of immune responses by extracellular vesicles. Nat Rev Immunol. 2014;14:195–208. doi: 10.1038/nri3622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buzas EI, Gyorgy B, Nagy G, Falus A, Gay S. Emerging role of extracellular vesicles in inflammatory diseases. Nat Rev Rheumatol. 2014;10:356–64. doi: 10.1038/nrrheum.2014.19. [DOI] [PubMed] [Google Scholar]
- 6.Loyer X, Vion AC, Tedgui A, Boulanger CM. Microvesicles as cell-cell messengers in cardiovascular diseases. Circ Res. 2014;114:345–53. doi: 10.1161/CIRCRESAHA.113.300858. [DOI] [PubMed] [Google Scholar]
- 7.Properzi F, Logozzi M, Fais S. Exosomes: the future of biomarkers in medicine. Biomarkers Med. 2013;7:769–78. doi: 10.2217/bmm.13.63. [DOI] [PubMed] [Google Scholar]
- 8.El Andaloussi S, Mager I, Breakefield XO, Wood MJ. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat Rev Drug Discov. 2013;12:347–57. doi: 10.1038/nrd3978. [DOI] [PubMed] [Google Scholar]
- 9.Revenfeld AL, Baek R, Nielsen MH, Stensballe A, Varming K, Jorgensen M. Diagnostic and prognostic potential of extracellular vesicles in peripheral blood. Clin Therapeut. 2014;36:830–46. doi: 10.1016/j.clinthera.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 10.Jayachandran M, Miller VM, Heit JA, Owen WG. Methodology for isolation, identification and characterization of microvesicles in peripheral blood. J Immunol Meth. 2012;375:207–14. doi: 10.1016/j.jim.2011.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sokolova V, Ludwig AK, Hornung S, Rotan O, Horn PA, Epple M, et al. Characterisation of exosomes derived from human cells by nanoparticle tracking analysis and scanning electron microscopy. Colloids Surf B Biointerfaces. 2011;87:146–50. doi: 10.1016/j.colsurfb.2011.05.013. [DOI] [PubMed] [Google Scholar]
- 12.Zhou H, Yuen PS, Pisitkun T, Gonzales PA, Yasuda H, Dear JW, et al. Collection, storage, preservation, and normalization of human urinary exosomes for biomarker discovery. Kidney Int. 2006;69:1471–6. doi: 10.1038/sj.ki.5000273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yuana Y, Bertina RM, Osanto S. Pre-analytical and analytical issues in the analysis of blood microparticles. Thromb Haemostasis. 2011;105:396–408. doi: 10.1160/TH10-09-0595. [DOI] [PubMed] [Google Scholar]
- 14.Lacroix R, Judicone C, Mooberry M, Boucekine M, Key NS, Dignat-George F, et al. Standardization of pre-analytical variables in plasma microparticle determination: results of the International Society on Thrombosis and Haemostasis SSC Collaborative workshop. J Thromb Haemost. 2013;11:1190–3. doi: 10.1111/jth.12207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Witwer KW, Buzás EI, Bemis LT, Bora A, Lässer C, Lötvall J, et al. Standardization of sample collection, isolation and analysis methods in extracellular vesicle research. J Extracell Vesicles. 2013;2 doi: 10.3402/jev.v2i0.20360. 20360, doi: http://dx.doi.org/10.3402/jev.v2i0.20360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Timar CI, Lorincz AM, Csepanyi-Komi R, Valyi-Nagy A, Nagy G, Buzas EI, et al. Antibacterial effect of microvesicles released from human neutrophilic granulocytes. Blood. 2013;121:510–8. doi: 10.1182/blood-2012-05-431114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Timar CI, Lorincz AM, Ligeti E. Changing world of neutrophils. Pflugers Archiv: Eur J Physiol. 2013;465:1521–33. doi: 10.1007/s00424-013-1285-1. [DOI] [PubMed] [Google Scholar]
- 18.Rada BK, Geiszt M, Kaldi K, Timar C, Ligeti E. Dual role of phagocytic NADPH oxidase in bacterial killing. Blood. 2004;104:2947–53. doi: 10.1182/blood-2004-03-1005. [DOI] [PubMed] [Google Scholar]
- 19.Chandler WL, Yeung W, Tait JF. A new microparticle size calibration standard for use in measuring smaller microparticles using a new flow cytometer. J Thromb Haemost. 2011;9:1216–24. doi: 10.1111/j.1538-7836.2011.04283.x. [DOI] [PubMed] [Google Scholar]
- 20.van der Pol E, van Gemert MJ, Sturk A, Nieuwland R, van Leeuwen TG. Single vs. swarm detection of microparticles and exosomes by flow cytometry. J Thromb Haemost. 2012;10:919–30. doi: 10.1111/j.1538-7836.2012.04683.x. [DOI] [PubMed] [Google Scholar]
- 21.Filipe V, Hawe A, Jiskoot W. Critical evaluation of Nanoparticle Tracking Analysis (NTA) by NanoSight for the measurement of nanoparticles and protein aggregates. Pharmaceut Res. 2010;27:796–810. doi: 10.1007/s11095-010-0073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Varga Z, Yuana Y, Grootemaat AE, van der Pol E, Gollwitzer C, Krumrey M, et al. Towards traceable size determination of extracellular vesicles. J Extracell Vesicles. 2014;3 doi: 10.3402/jev.v3.23298. 23298, doi: http://dx.doi.org/10.3402/jev.v3.23298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gercel-Taylor C, Atay S, Tullis RH, Kesimer M, Taylor DD. Nanoparticle analysis of circulating cell-derived vesicles in ovarian cancer patients. Anal Biochem. 2012;428:44–53. doi: 10.1016/j.ab.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Taylor DD, Chou IN, Black PH. Isolation of plasma membrane fragments from cultured murine melanoma cells. Biochem Biophys Res Commun. 1983;113:470–6. doi: 10.1016/0006-291x(83)91749-7. [DOI] [PubMed] [Google Scholar]