Abstract
Pacemaker infection with Mycobacterium chelonae has not been reported previously. We report the first case of pacemaker lead endocarditis due to M. chelonae, which was successfully treated with multidrug regimen. M. chelonae is regarded as an environmental bacterium and its pathogenicity has been recognised recently. The present case illustrates its ability as a primary invader should not be underestimated, especially in an immunocompetent patient with indwelling devices. Epidemiology and management of this rare cause of culture-negative endocarditis is discussed.
Background
The present case illustrates that ability of Mycobacterium chelonae as a primary invader should not be underestimated, especially in an immunocompetent patient with indwelling devices. This is the first case of pacemaker lead endocarditis due to M. chelonae, which was successfully treated with a multidrug regimen.
Case presentation
A 63-year-old man had pacemaker implantation for complete heart block in 2001 and later a pulse generator change in 2012. In 2012, due to persisting pacemaker malfunction, the pulse generator had to be changed three times over a period of 1 year at his local hospital. Both infra-clavicular areas were used for the procedures. The patient presented to our institute with recurrent episodes of presyncope. There was no history of fever, rash or other systemic symptoms. ECG showed paced ventricular rhythm at a rate of 60/min, but 24 h Holter monitoring revealed intermittent failure to capture. Blood biochemistry was within normal range except elevated erythrocyte sedimentation rate (45 mm) and C reactive protein (33.3 mg/L). Two-dimensional echocardiography showed large (>10 mm) mobile vegetation on right ventricular (RV) lead, which was confirmed on transoesophageal echocardiogram (figure 1). Repeated blood cultures were negative. The patient underwent sternotomy and explanation of lead and pulse generator under cardiopulmonary bypass. In view of the large vegetation and multiple implantations in the pectoral region, an epigastric single-chamber pacemaker was inserted. Culture of excised RV vegetation isolated M. chelonae. This was also isolated from bone marrow culture. Therefore, a diagnosis of disseminated mycobacterial infection leading to pacemaker lead endocarditis was made and the patient was started on injectable amikacin (15 mg/kg intramuscularly once daily), oral levofloxacin (750 mg twice daily) and clarithromycin (500 mg twice daily).
Figure 1.
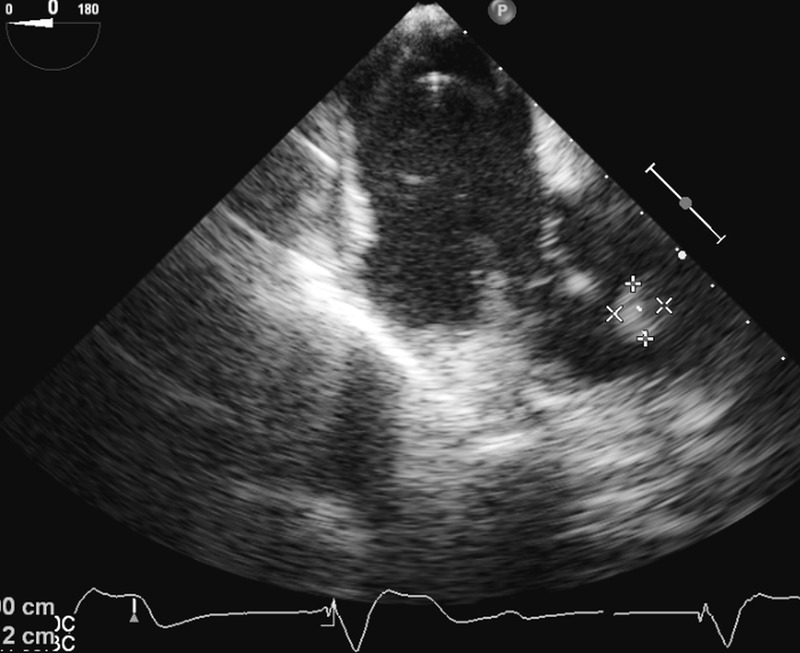
Two-dimensional transoesophageal echocardiography showing 12×14 mm vegetation attached to the right ventricular (RV) lead.
After 1 month, the patient presented with a sternal wound and pacemaker pocket site infection. The pus swab grew M. chelonae. After extensive debridement and 6 weeks of antimycobacterial therapy with temporary pacemaker in situ, a new pacemaker was inserted in the left infra-clavicular fossa. On follow-up, the patient remained asymptomatic and was continued on prolonged antimycobacterial therapy with amikacin, levofloxacin and clarithromycin.
Treatment
The patient was managed with injectable amikacin (15 mg/kg intramuscularly once daily), oral levofloxacin (750 mg twice daily) and clarithromycin (500 mg twice daily).
Outcome and follow-up
On follow-up after 2 months, the patient remained asymptomatic and was continued on prolonged antimycobacterial therapy with amikacin, levofloxacin and clarithromycin.
Discussion
M. chelonae is a rapidly growing mycobacterium (RGM) that is a member of the Runyon group IV.1 Although ubiquitous in nature, it rarely causes infection. It has been found to cause a wide array of infections, from skin and soft tissue infection following puncture wounds to infections of foreign material (porcine and prosthetic cardiac grafts, intravenous and dialysis catheters), especially in immunocompromised hosts.2–4 Our patient was immunocompetent and CD4 counts were in normal range. Pacemaker infection with M. chelonae has not been reported previously. Diagnosis of RGM infections may be difficult; conventional methods may lead to inconclusive identification. Molecular identification methods remain essential for rapid diagnosis and for guiding prompt and adequate antimicrobial therapy. M. chelonae in our patient was isolated from blood and bone marrow culture. M. chelonae grew on Lowenstein-Jensen medium as smooth cream-coloured colonies within 7 days of incubation. They were non-chromogenic, did not reduce nitrate, and did not grow on medium with sodium chloride. However, they produced urease and arylsulfatase. They were further identified by line probe assay using GenoType Mycobacterium CM (Hain Lifescience).5
However, in the light of its ubiquitous distribution, infection with M. chelonae could have occurred at any of the implantation procedures. We hypothesise that our patient carried mycobacterial infection, which seeded onto the device pocket at the time of his pulse generator change, and subsequently remained clinically silent in the vicinity of the device for several months. Owing to the rarity of non-tuberculous mycobacteria-related cardiac device-related infective endocarditis, there are no clear management guidelines as to the duration of therapy. Based on prior reports, a combination therapy of two or three drugs for 6–12 months appears necessary. The choice of antibiotics depends on the results of susceptibility testing. Overall, clarithromycin is the drug most active against M. chelonae. Clarithromycin is significantly superior to erythromycin and azithromycin in vitro with variable susceptibility to aminoglycosides, doxycycline, imipenem and ciprofloxacin. Trimethoprim-sulfamethoxazole and the newer β-lactam antibiotics are ineffective against M. chelonae.6 Removal of the infected pacemaker device is of paramount importance because of the high rate of relapse, despite prolonged antimicrobial therapy.
Learning points.
Although rare, Mycobacterium chelonae as a primary invader should not be underestimated, especially in a patient with indwelling devices.
Prompt diagnosis and treatment can be lifesaving.
Molecular identification methods remain essential for rapid diagnosis and for guiding prompt and adequate antimicrobial therapy.
A prolonged multidrug regimen is key to successful management of M. chelonae-related infections.
Footnotes
Contributors: All authors have contributed to the patient diagnosis, management and follow-up; conception and design, acquisition of data or analysis and interpretation of data; and drafting the article or revising it critically for important intellectual content.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Galil K, Turer R, Glatter K et al. . Disseminated Mycobacterium chelonae infection resulting in endocarditis. Clin Infect Dis 1996;23:1322–3. [DOI] [PubMed] [Google Scholar]
- 2.Altmann G, Horowitz A, Kaplinsky N et al. . Prosthetic valve endocarditis due to Mycobacterium chelonei. J Clin Microbiol 1975;1:531–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma S, Tleyjeh IM, Espinosa RE et al. . Pacemaker Infection due to Mycobacterium fortuitum. Scand J Infect Dis 2005;37:66–7. [PubMed] [Google Scholar]
- 4.Cutay AM, Horowitz HW, Pooley RW et al. . Infection of epicardial pacemaker wires due to Mycobacterium abscessus. Clin Infect Dis 1998;26:520–1. [DOI] [PubMed] [Google Scholar]
- 5.Lee AS, Jelfs P, Sintchenko V et al. . Identification of non-tuberculous mycobacteria: utility of the GenoType Mycobacterium CM/AS assay compared with HPLC and 16S rRNA gene sequencing. J Med Microbiol 2009;58:900–4. [DOI] [PubMed] [Google Scholar]
- 6.Swenson JA, Wallace RJ Jr, Silcox VA et al. . Antimicrobial susceptibility of five subgroups of Mycobacterium fortuitum and Mycobacterium chelonae. Antimicrob Agents Chemother 1985;28:807–11. [DOI] [PMC free article] [PubMed] [Google Scholar]


