Abstract
INTRODUCTION
Intestinal metastasis from gastric cancer is rare, although the most common cause of secondary neoplastic infiltration of the colon is gastric cancer. However, little data is available on recurrence or death in patients with gastric cancer surviving >5 years post-gastrectomy. Here we report two cases of lower intestinal metastasis from gastric cancer >5 years after primary resection and discuss with reference to the literature.
PRESENTATION OF CASE
Case 1: A 61-year-old man with a history of total gastrectomy for gastric cancer 9 years earlier was referred to our hospital with constipation and abdominal distention. We diagnosed primary colon cancer and subsequently performed extended left hemicolectomy. Histological examination revealed poorly differentiated adenocarcinoma resembling the gastric tumor he had 9 years earlier. The patient refused postoperative adjuvant chemotherapy and remained alive with cancerous peritonitis and skin metastases as of 17 months later. Case 2: A 46-year-old woman with a history of total gastrectomy for gastric cancer 9 years earlier presented with constipation. She also had a history of Krukenberg tumor 3 years earlier. We diagnosed metastatic rectal cancer and subsequently performed low anterior resection and hysterectomy. Pathological examination revealed poorly differentiated tubular adenocarcinoma, resembling the gastric tumor. The patient remained alive without recurrence as of 17 months later.
DISCUSSION
We found 19 reported cases of patients with resection of colon metastases from gastric cancer. Median disease-free interval was 74 months.
CONCLUSION
Resection of late-onset colorectal recurrence from gastric cancer appears worthwhile for selected patients.
Keywords: Gastric cancer, Colonic metastasis, Late onset, Surgical resection
1. Introduction
Intestinal metastasis from gastric cancer is rare, although the most common cause of secondary neoplastic infiltration of the colon is gastric cancer.1 To the best of our knowledge, only two reports in the English literature have described lower intestinal metastasis from gastric cancer occurring >5 years after primary surgery.2,3 The characteristics of this situation thus appeared largely unknown. However, we then identified over 30 reported cases in the Japanese literature with or without English abstracts available.4
From January 1999 to July 2012, we performed 1020 gastric cancer surgeries and encountered 3 cases with late-onset lower intestinal recurrence of gastric cancer occurring 9–11 years after primary resection at Obihiro Kosei General Hospital in Japan. We recently reported one of these cases of colon metastasis from gastric cancer, which occurred 11 years after primary surgery.5 Here we report the other 2 cases of late-onset colon metastasis from gastric cancer.
2. Case reports
2.1. Case 1
A 61-year-old man was referred to our hospital with constipation, abdominal distention, and lower abdominal pain. At 52 years old, he had undergone radical total gastrectomy and distal pancreatectomy with regional lymph node dissection. Histological examination revealed poorly differentiated adenocarcinoma involving signet-ring cell carcinoma, categorized as T3N0M0 according to the American Joint Committee on Cancer classification 7th. Surgical margins for the resected primary tumor were free of tumor cells. The patient had received regular follow-up on an outpatient basis for 5 years before being referred to our hospital.
Abdominal computed tomography (CT) showed target-like thickening of the descending colon and moderate accumulation of ascites. Radiographic contrast-enhanced enema and colonoscopy revealed induration and stenosis of the descending colon. The diagnosis was primary cancer of the descending colon.
A small, hard mass was palpated during laparotomy in the middle of the transverse colon, and thus left hemicolectomy and transverse colectomy with mesenteric lymph node dissection were performed. Postoperative course was uneventful. Histological examination of the colon tumor revealed poorly differentiated adenocarcinoma (Fig. 1), showing similar pathological findings to the gastric tumor 9 years earlier. Immunohistochemical staining showed positive results for cytokeratin 7, and negative results for cytokeratin 20 and caudal-type homeobox 2. These findings supported the suggestion that this tumor represented colon metastasis from the previous gastric cancer. The surgical margin on the anal side was positive on pathological examination, with cancer cells spread widely from the submucosal to the muscular layer in all surgical specimens (Fig. 2). Many lymph node metastases were identified in resected specimens. The patient refused chemotherapy after surgery, and remained alive with cancerous peritonitis and skin metastasis as of 17 months later.
Fig. 1.
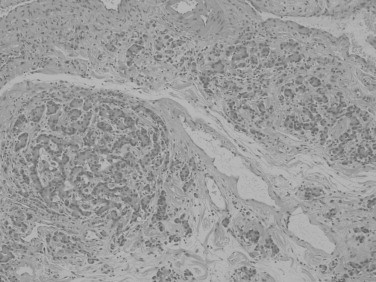
Pathological findings of the resected ascending to transverse colon. Histological examination of the colon tumor reveals tubular adenocarcinoma with signet-ring cell carcinoma.
Fig. 2.
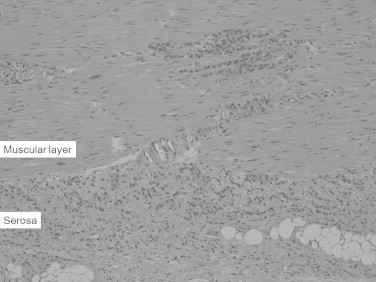
Histological examination of the anal-side margin, showing tumor cells have spread widely into the submucosal and muscular layers. Similar histological findings were also found in almost all of the resected specimen.
2.2. Case 2
A 46-year-old woman presented with constipation, abdominal distention, and lower abdominal pain. At 37 years old, she had undergone radical total gastrectomy and distal pancreatectomy with regional lymph node dissection for poorly differentiated adenocarcinoma identified as T3N2M0 signet-ring cell carcinoma according to the AJCC 7th. The surgical margins of the primary tumor were free of tumor cells. The patient then underwent adjuvant chemotherapy and received regular follow-up on an outpatient basis for 5 years. At 43 years old, 6 years after primary resection, she was diagnosed with an ovarian tumor and underwent ovariectomy. The pathological diagnosis was Krukenberg tumor (metastatic moderately and poorly differentiated adenocarcinoma).
We performed magnetic resonance imaging (MRI) and abdominal CT, both of which showed rectal tumor invading the uterus. Radiographic contrast-enhanced enema and colonoscopy revealed induration and stenosis of the rectum. Metastatic gastric cancer of the rectum was diagnosed after histological examination revealed moderately to poorly differentiated adenocarcinoma resembling the gastric cancer that had occurred 9 years earlier. Low anterior resection and hysterectomy were performed with mesenteric lymph node dissection. The postoperative course was uneventful. Pathological examination revealed that tubular adenocarcinoma with moderately and poorly differentiated components, similar to the pathological findings of the previous gastric tumor, had invaded both the rectum and uterus (Figs. 3 and 4). Two metastases were present in the resected mesenteric lymph nodes. The patient subsequently underwent chemotherapy for 1 year, and remained alive without recurrence as of 24 months later.
Fig. 3.
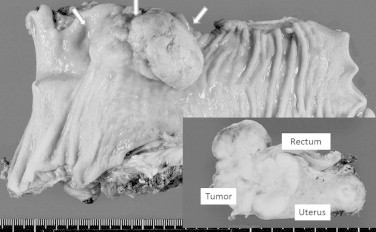
Pathological findings of the resected specimen show the tumor has invaded both the rectum and uterus.
Fig. 4.
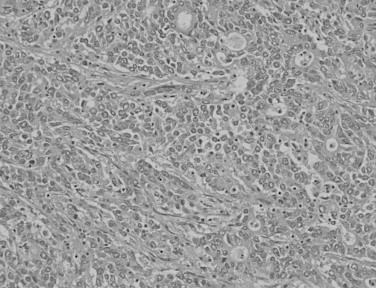
Histological examination of the colon tumor reveals tubular adenocarcinoma with moderately and poorly differentiated adenocarcinoma has invaded the rectum and uterus.
3. Discussion
Recent reports from Japan and Korea have shown a late recurrence rate of about 6% among patients with advanced gastric cancer who survived >5 years post-gastrectomy.6 Intestinal metastasis from gastric cancer itself is rare, although the most common cause of secondary neoplastic infiltration of the colon is gastric cancer. We reviewed reported cases of metastatic colon cancer from gastric cancer in the literature, including those with only the abstract in English (Table 1).
Table 1.
Literature reports of late onset colorectal recurrence of gastric cancer >5 years after primary resection.
| Year | Author | Age | Gender | Recurrent lesion | LNM | Primary tumor | DFI (month) | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1988 | Okabe8 | 49 | F | C, A | Unknown | Por | 60 | Unknown |
| 1988 | Ohta7 | 57 | M | C | Yes | Por | 68 | 42M died |
| Ohta | 51 | F | A, T, D, S | Yes | Por | 69 | 22M died | |
| Ohta | 44 | F | R | Yes | Por | 106 | 27M dieda | |
| 1991 | Yamada9 | 61 | M | T | Unknown | Por | 64 | 3M alive |
| 1994 | Ogiwara3 | 53 | F | D | Yes | Por | 660 | Unknown |
| 2001 | Man-i12 | 58 | M | T, D, S, R | Yes | Sig | 84 | 10M alive |
| 2001 | Kim11 | 75 | M | T | Unknown | Well | 77 | 26M alive |
| Kim | 70 | M | C | Unknown | Well | 68 | 44M alive | |
| 2001 | Hase10 | 44 | F | T | Unknown | Por, Sig | 68 | Unknown |
| 2006 | Hiraki13 | 68 | F | A | Yes | Por, Sig | 60 | 7M alive |
| 2008 | Shiokawa4 | 69 | F | T | Yes | Por | 156 | 4M alive |
| 2009 | Takahashi14 | 76 | M | R | Unknown | Por | 66 | 6M alive |
| 2010 | Iwakawa15 | 75 | F | R | Yes | Por | 83 | 25M died |
| Iwakawa | 76 | F | R | Yes | Por | 82 | 22M died | |
| 2011 | Arai17 | 62 | M | A, D, R | Unknown | Por, Mode | 180 | Unknowna |
| 2011 | Murakami16 | 60 | M | D | Unknown | Mode, Por | 72 | 2M alive |
| 2012 | Watanabe2 | 58 | M | T | Unknown | Por, Sig | 77 | 27M died |
| 2013 | Yamamura4 | 79 | M | T | Yes | Por, Sig | 132 | 19M died |
| – | Our Case 1 | 61 | M | T, D, S | Yes | Por, Mode | 110 | 17M alive |
| – | Our Case 2 | 46 | F | R | Yes | Por | 106 | 24M alive |
LNM: lymph node metastasis; DFI: disease free interval; Gender (M/F: male/female); C: cecum; A: ascending colon; T: transverse colon; D: descending colon; S: sigmoid colon; R: rectum; Por: poorly differentiated adenocarcinoma; Sig: signet ring cell adenocarcinoma; Mode: moderately differentiated adenocarcinoma; Well: well-differentiated adenocarcinoma; M: month.
This patient was not resected; the only treatment was chemotherapy.
We performed a search of the literature using both PubMed and “Ichyu-shi”, a Japanese literature search engine. Since 1980s, we found 21 cases of colonic metastases occurring at least 5 years after primary resection, once cases from gastric cancer the Japanese literature with English abstracts were included.2,4,7–17
Nineteen of the 21 cases had undergone various resections, and the median disease-free interval was 74 months. The most frequent site of metastasis was the transverse colon. The majority of metastatic cases originated from poorly differentiated carcinoma. Eleven cases showed regional lymph node metastasis. Median survival from surgery for metastatic lesions was 26 months, and 2 cases survived >3 years.
The transverse colon was the most frequent site of gastric cancer metastasis to the colon. A previous report showed a similar frequency.18 Transverse colon metastasis represents an example of direct invasion or extension. Several authors have suggested that a common pathway of tumor spread to the gastrointestinal tract is via mesenteric reflections.19 In our report, Case 1 was caused by direct invasion through the mesentery and intraluminal dissemination, whereas Case 2 would have involved intraperitoneal seeding, because the patient had a history of a Krukenberg tumor originating from gastric cancer. However, she showed no other signs of intraperitoneal seeding at other sites.
Several reports have suggested that surgery for selected patients with recurrent gastric tumors is worthwhile, due to the potential survival benefit from surgical intervention. Unfortunately, one of our patients (Case 1) had systematic metastasis, but the other case (Case 2) showed relatively long survival.
Our data (review of literature) showed a median survival time of 26 months after surgery for metastatic gastric cancer to the colon. Nunobe et al. reported outcomes of surgery with curative intent for 36 selected patients with locoregional recurrence.20 Their data showed that median survival after surgery was about 23 months, and 7 of the 36 patients (19.4%) with recurrent gastric cancer achieved long-term survival >3 years after surgery.
Considering these reported data, resection of late-onset colorectal recurrence appears worthwhile for selected patients because of potential gains in long-term survival. When resection is to be performed, careful consideration of the surgical margins is needed due to the likelihood of lymph node metastases and the intramuscular spread of tumor cells.
Consent
Written informed consent was obtained from both patients for publication of this case series and accompanying images. Copies of the written consent are available for review by the Editor-in-Chief of this journal on request.
Conflict of interest
None of the authors have any conflicts of interest to declare for this case report.
Funding
There is no source of funding for our research.
Ethical approval
We confirmed that our study was approved by Ethics Committee of Obihiro Kosei General Hospital.
Author contributions
Takehiro Noji contributes to the design of the manuscript, performed these operations, and wrote all part of the manuscript. Koichi Ohono contributes to performing these operations, and to the design of this manuscript.
Yoshiyuki Yamamura, Jun Muto, Aki Kuroda, Junkichi Koinuma, Tatsuya Yoshioka1, Katsuhiko Murakawa, Setsuyuki Otake, and Satoshi Hirano participated in co-ordination and helped to draft the manuscript. All authors read and approved the final manuscript.
References
- 1.Jang H.J., Lim H.K., Kim H.S., Cho E.Y., Lee S.J., Kim K.A. Intestinal metastases from gastric adenocarcinoma: helical CT findings. J Comput Assist Tomogr. 2001;25(1):61–67. doi: 10.1097/00004728-200101000-00011. [Epub 2001/02/15] [DOI] [PubMed] [Google Scholar]
- 2.Watanabe M., Suzuki H., Maejima K., Komine O., Mizutani S., Yoshino M. Surgical resection of late solitary locoregional gastric cancer recurrence in stomach bed. Med Sci Monit: Int Med J Exp Clin Res. 2012;18(7):CS53–CS56. doi: 10.12659/MSM.883196. [Epub 2012/06/29] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogiwara H., Konno H., Kitayama Y., Kino I., Baba S. Metastases from gastric adenocarcinoma presenting as multiple colonic polyps: report of a case. Surg Today. 1994;24(5):473–475. doi: 10.1007/BF01427044. [Epub 1994/01/01] [DOI] [PubMed] [Google Scholar]
- 4.Shiokawa H., Funahashi K., Koike J., Saito N., Kurihara A., Kaneko T. Metachronous colonic metastasis from gastric adenocarcinoma presenting 13 years after gastrectomy: a case report and review of the literature. Jpn J Gastroenterol Surg. 2008;41(11):1927–1934. [Google Scholar]
- 5.Yamamura Y., Kuroda A., Koinuma J., Murakawa K., Ohtake S., Ono K. A case of resection of metastatic colon cancer 11 years after surgery for gastric cancer. J Jpn Coll Surg. 2013;38(4):875–879. [Google Scholar]
- 6.Shiraishi N., Inomata M., Osawa N., Yasuda K., Adachi Y., Kitano S. Early and late recurrence after gastrectomy for gastric carcinoma. Univariate and multivariate analyses. Cancer. 2000;89(2):255–261. doi: 10.1002/1097-0142(20000715)89:2<255::aid-cncr8>3.0.co;2-n. [Epub 2000/08/05] [DOI] [PubMed] [Google Scholar]
- 7.Ohta H., Kaoru A., Seki M., Takagi K., Nishi M., Maruyama M. Clinicopathological study on metastatic colo-rectal cancer. I to Cho (Stomach Intest) 1988;23(6):633–643. [Google Scholar]
- 8.Okabe S., Kaneko Y., Takemura K., Goseki N., Endo M., Kamiyama R. Secondary linitis plastica type carcinoma of the ileocecal region metastatic from the advanced gastric carcinoma, report of a case. I to Cho (Stomach Intest) 1988;23(6):663–670. [Google Scholar]
- 9.Yamada S., Shimizu T., Miyata Y. Clinicopathological study on colorectal metastasis of gastric carcinoma. Endosc For Dig Dis. 1991;7(2):157–162. [Google Scholar]
- 10.Hase T., Kazui K., Wakisaka Y., Ikuta K., Ikeda Y., Takehara M. Two case of colorectal intramural metastasis from gastric cancer. J Jpn Surg Assoc. 2001;62(10):2403–2407. [Google Scholar]
- 11.Kim S., Tamura S., Matsuyama J., Kishi K., Miyauchi K., Seki Y. Two cases survived for long term after resection of colon metastasis of gastric cancer. Jpn J Gastroenterol Surg. 2001;34(9):1410–1414. [Google Scholar]
- 12.Man-i M., Tsujinaka T., Nishisho I., Mishima H., Yoshikawa N. A case of metastatic diffuse infiltrative carcinoma of the colon and rectum from gastric cancer 7 years after curative resection. Nippon Daicho Komonbyo Gakkai Zasshi. 2001;54(5):335–341. [Google Scholar]
- 13.Hiraki M., Mori M., Iyama A., Yonemitsu N. A case of metastatic carcinoma of the colon from gastric cancer 5 years after cutative resection. J Jpn Surg Assoc. 2006;67(9):2132–2135. [Google Scholar]
- 14.Takahashi M., Kurosawa H., Masui H., Fukushima T., Mogaki M., Nagahori K. A case of diffuse invasive metastatic carcinoma of the rectum occured 5.5 years after resection for gastric cancer. J Jpn Surg Assoc. 2009;70(12):3616–3622. [Google Scholar]
- 15.Iwakawa K., Inoue H., Kiyochi H., Kajiwara S., Nishie M., Hamano R. Surgically treated cases of metastatic colorectal cancer after curative resection for gastric cancer: a clinicopathological study. Nippon Daicho Komonbyo Gakkai Zasshi. 2010;63(4):191–196. [Google Scholar]
- 16.Murakami H. Two cases of metastatic colorectal cancer. Nippon Daicho Komonbyo Gakkai Zasshi. 2011;64(8):492–499. [Google Scholar]
- 17.Arai T., Kakuta Y., Kinouchi Y., Kimura T., Negoro K., Aihara H. Increased expression of NKX2.3 mRNA transcribed from the risk haplotype for ulcerative colitis in the involved colonic mucosa. Hum Immunol. 2011;72(7):587–591. doi: 10.1016/j.humimm.2011.03.023. [Epub 2011/04/26] [DOI] [PubMed] [Google Scholar]
- 18.McQueeney A.J., Olson R.W., Medwid A. Primary scirrhous carcinoma of colon. Roentgenologic diagnosis. Am J Roentgenol Radium Ther Nucl Med. 1967;101(2):306–310. doi: 10.2214/ajr.101.2.306. [Epub 1967/10/01] [DOI] [PubMed] [Google Scholar]
- 19.Feczko P.J., Collins D.D., Mezwa D.G. Metastatic disease involving the gastrointestinal tract. Radiol Clin N Am. 1993;31(6):1359–1373. [Epub 1993/11/01] [PubMed] [Google Scholar]
- 20.Nunobe S., Hiki N., Ohyama S., Aikou S., Sano T., Yamaguchi T. Outcome of surgical treatment for patients with locoregional recurrence of gastric cancer. Dtsch Ges ChirLangenbeck's Arch Surg. 2011;396(2):161–166. doi: 10.1007/s00423-010-0730-2. [Epub 2010/12/15] [DOI] [PubMed] [Google Scholar]


