Abstract
INTRODUCTION
Elastofibroma dorsi(EFD) is slow-growing, benign, soft tissue tumor of unclear pathogenesis, typically located at the subscapular region of elderly people. It may be unilateral or bilateral. As it exhibits benign behavior, it should be surgically removed only in symptomatic patients. Magnetic resonance imaging (MRI) is a useful tool for assessment of EFD and can potentially help avoid the need for unnecessary biopsy and surgery.
PRESENTATION OF CASE
A 62-year-old woman presented with 2 years complaint of back pain, particularly aggravated with shoulder movements and swelling with bilateral elastofibroma dorsi. Both masses were totally excised with bilateral posterolateral subscapular incision. Symptoms were completely controlled and significant discomfort from the surgical procedure was completely resolved with in a few weeks interval from the operation.
DISCUSSION
The pathogenesis of the EFD still remains unclear. Elastofibroma dorsi has an unspecific clinical presentation and can be confused with other tumors of the periscapular region Imaging studies are useful for diagnosis.
CONCLUSION
Elastofibroma dorsi is benign soft tissue tumor mostly observed in the subscapular regions of elderly female patients. The surgery is indicated in symptomatic cases and must be confined to simple excision of the lesion.
Keywords: Elastofibroma dorsi, Magnetic resonance imaging, Surgery
1. Introduction
Elastofibroma dorsi (EFD) is a slow growing, noncapsulated, benign, solid, and soft tissue tumor with no well-defined boundaries, which is often observed in the subscapular region on the thorax wall.1 Jarvi and Saxen first described the condition in 1961.2 Although its etiology is still under debate, it is considered that its development may be influenced by continued mechanical friction between the lower part of the scapula and the ribs and even by a certain genetic component.3
An EFD prevalence rises to 24% and is often observed among women in the fourth to sixth decades.3,4 Although the EFD is usually unilateral, it is bilateral in 30% of the cases.4 It usually manifests as a palpable lump with pain on mobilization of the shoulder. Ultrasound, magnetic resonance imaging (MRI), and computed tomography (CT) are useful for diagnosis,5,6 and the common recommended treatment method for EFD is total surgical excision. The differential diagnosis includes other benign tumors and neoplasias.7
2. Case presentation
A 62-year-old woman presented with 2 years complaint of back pain, particularly aggravated with shoulder movements and swelling under the left scapula. Her laboratory tests were within normal limits and no significant medical history. Her physical examination revealed a palpable mass in the right infrascapular region of approximately 7 cm × 5 cm in the neutral position. The detection of a second mass in the right subscapular region was made by thoracic CT, and the arm was re-examined in hyperabduction. The second mass was approximately 5 cm × 5 cm and was detected on the right. Her thoracic MRI examination revealed noncapsulated and ovoid masses of 7 cm × 5 cm × 4 cm on the left and 5 cm × 5 cm × 4 cm on the right side in the subscapular region between the rhomboid and latissimus dorsi muscle groups, which were isointense with the surrounding muscle tissues and contained linear hyperintense areas in its internal structure (Fıg. 1). Under general anesthesia, both masses were totally excised with bilateral posterolateral subscapular incision with the patient lying in the prone position and with slightly abducted arm (Fıg. 2). The masses were macroscopically noncapsulated, irregular and rubberlike (Fig. 3). Symptoms were completely controlled and significant discomfort from the surgical procedure was completely resolved with in a few weeks interval from the operation. During the 6-month postoperative follow-up, no complications, no local recurrence, and no restrained shoulder movements were identified. The histopathologic examination was reported as elastofibroma.
Fig. 1.
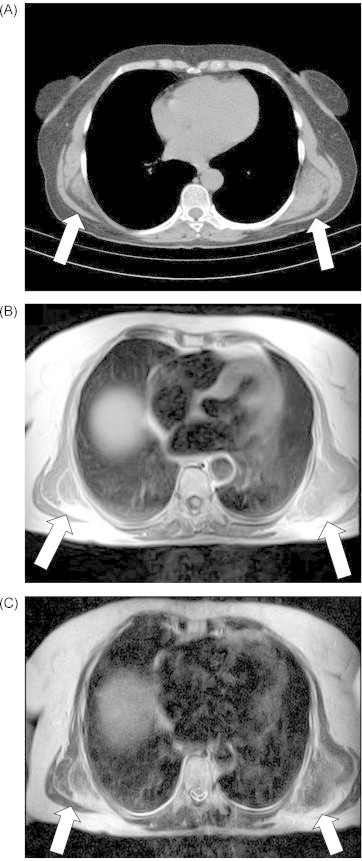
(A) Computed tomography scan shows elastofibroma typical placement of bilateral periscapuler region. Axial T1-weighted MR images: (B) axial T-2 weighted MR images. (C) Magnetic resonance scan of both mass with striated appearance and multiple linear septae of alternating high and low signal intensity due to the interlacing of linear streaks of fat.
Fig. 2.

The typical location for bilateral elastofibroma dorsi in prone position and with slightly abducted arm.
Fig. 3.

Macroscopic appearance of surgical specimen.
3. Discussion
Elastofibroma dorsi is a relatively uncommon benign lesion of the connective tissue of the chest wall, first described in 1961.1,2 Although originally considered a very rare occurrence, recent autopsy studies reported an incidence of 13 to 17% and, in subjects over 60 years of age up to 24%.3,4
The pathogenesis of the EFD still remains unclear. It has been suggested that repetitive microtrauma by friction between the lower part of the scapula and the thoracic wall may cause the reactive hyperproliferation of fibroblastic tissue.1–3 Although this view has been supported by the higher EFD prevalence particularly among individuals who work at hard manual labor, the EFD may also be observed in those who have never worked in hard manual labor jobs and in different locations. Detection of new cases in different regions has led to hypotheses, such as reactive fibromatosis, degeneration due to vascular deficiency, elastotic degeneration, genetic disposition, hereditary enzymatic defect, or systematic involvement.8–10 Perhaps, multiple factors might account for the etiopathogenesis. Karakurt et al.11 reported 16 case with EFD. In this study 6 patients were manual laborers. A new EFD on the contralateral side developed in 2 of these patients at the follow-up. Our patient had no findings that suggested a genetic disposition or enzyme defect, and no history of working with muscle force.
Although usually unilateral, the EFD is bilateral in 10% of the cases and is mostly common located at the inferior pole of the scapula deep to the serratus anterior and latissimus dorsi muscles,12 but in very rare occasion s (<1% of patients), EFD can also be found in other sites. Elastofibroma dorsi is most frequently seen in older women, with a reported female:male ratio of 5/1 and a mean age at diagnosis of 65–70 years.13 Our case was a 62-year-old female with bilateral EFD.
Pain is the most common clinical complaint; however, shoulder pain can be in almost all patients. Additionally EFD has an unspecific clinical presentation and can be confused with other tumors of the periscapular region.14 A good physical examination can detect the mass under the scapula, with 50% of cases being asymptomatic or having mild complaints. There may be limitations in the motions of the upper extremities. Elastofibroma dorsi do not adhere to the skin and can easily be palpated on the thoracic wall. The scapula may sometimes mask the lesion. When both arms of the patient are strongly pulled forward and the body is bent forward at an angle of 10°–15°, the lesion becomes more evident.
Imaging studies are useful for diagnosis. An ultrasound shows in the echogenic fibroblastic background a mass that contains a lipid tissue in the form of scattered linear and curvilinear hypoechoic lines, and a multilayered appearance is characteristic of the EFD.15
However it is not always typically heterogeneous soft tissue mass form and may not be able to make the distinction with the masses which contains lipoma, fibroma, hemangioma, as well as other soft tissue sarcomas, and metastases. The CT scan reveals a heterogeneous soft tissue mass with muscular density, which contains low-density linear areas depending on the lipid tissue.15 It is hard to discriminate it from the surrounding muscles. Computed tomography scan diagnostic in cases where a typical placement of bilateral periscapuler region. However, the sensitivity of MRI is higher than unilateral lesions. The MRI, with its multiplanar capabilities and high contrast resolution, is a useful tool to characterize EFD location, size, composition, and structural relation with adjacent tissues and may help prevent an unnecessary biopsy.16 Magnetic resonance imaging demonstrating two masses that appeared hypo-/hyper-intense structures in T1 and T2 weighted images. On images acquired after contrast injection, both masses displayed enhancement, which was more evident on the left.
Excision of asymptomatic EFD lesions is not necessary because malignant transformation has never been described.17 Magnetic resonance imaging and CT is a useful for diagnosis of EFD and can potentially help avoid the need for unnecessary biopsy and surgery. Surgical excision is indicated in symptomatic patients. Unnecessary large and radical resections should be avoided in such patients as marginal resections would be enough.18
Radiotherapy may be an option particularly in unresectable cases due to their localizations.17,18 Postoperative wound drainage and a compression garment are recommended, as well as shoulder immobilization for 1 week to reduce post operative seroma.17,18
Nagamine et al.19 reported 1 case with recurrence in their 170-patient series. Briccoli et al.20 reported 1 patient with ED who had a second lesion on the other side 2 years after surgical resection. Tamimi Mariño et al.16 reported 10% recurrence rate after a mean post-surgical period of 47 months. Karakurt et al.11 observed no recurrences in their 16 patient series. In our patient, we totally excised the masses by bilateral subscapular incision. Having completed her 6-month follow-up, our patient has exhibited no physical and radiologic findings in favor of recurrence.
4. Conclusion
Elastofibroma dorsi is benign soft tissue tumor mostly observed in the subscapular regions of elderly female patients, the EFD should be considered in patients with chronic back pain. Magnetic resonance imaging has a high sensitivity in the diagnosis of EFD and could avoid the need for biopsy. The surgery is indicated in symptomatic cases and must be confined to simple excision of the lesion.
Conflict of interest
All the authors have no conflict of interest.
Funding
All the authors state that they have no sources of funding for research.
Ethical approval
None.
Author contributions
Inanc Samil Sarici was involved in writing and operation. Elif Basbay was involved in writing. Mehdi Mustu was involved operation. Burak Eskut and Ferhat Kala were involved in data collection. Orhan Agcaoglu, Murat Akici and Enver Ozkurt were involved in study design.
References
- 1.Fibla J., Molins L., Marco V., Pérez J., Vidal G. Bilateral elastofibroma dorsi. Joint Bone Spine. 2007;74:194–196. doi: 10.1016/j.jbspin.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 2.Jarvi O.H., Saxen A.E. Elastofibroma dorsi. Acta Pathol Microbiol Scand. 1961;144(Suppl. 52):83–84. [PubMed] [Google Scholar]
- 3.Parratt M.T., Donaldson J.R., Flanagan A.M., Saifuddin A., Pollock R.C., Skinner J.A. Elastofibroma dorsi: management, outcome and review of the literature. J Bone Joint Surg Br. 2010;92(2):262–266. doi: 10.1302/0301-620X.92B2.22927. [DOI] [PubMed] [Google Scholar]
- 4.Kourda J., Ayadi-Kaddour A., Merai S., Hantous S., Miled K.B., Mezni F.E. Bilateral elastofibroma dorsi. A case report and review of the literature. Orthop Traumatol Surg Res. 2009;95:383–387. doi: 10.1016/j.otsr.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Dinauer P.A., Brixey C.J., Moncur J.T., Fanburg-Smith J.C., Mur-phey M.D. Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults. Radiographics. 2007;27:173–187. doi: 10.1148/rg.271065065. [DOI] [PubMed] [Google Scholar]
- 6.Faccioli N., Foti G., Comai A., Cugini C., Guarise A., Mucelli R.P. MR imaging findings of elastofibroma dorsi in correla-tion with pathological features: our experience. Radiol Med. 2009;114:1283–1291. doi: 10.1007/s11547-009-0442-2. [DOI] [PubMed] [Google Scholar]
- 7.Hayes A.J., Alexander N., Clark M.A., Thomas J.M. Elastofibroma: a rare soft tissue tumour with a pathognomonic anatomical location and clinical symptom. Eur J Surg Oncol. 2004;30:450–453. doi: 10.1016/j.ejso.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Muramatsu K., Ihara K., Hashimoto T., Seto S., Taguchi T. Elastofibroma dorsi: diagnosis and treatment. J Shoulder Elbow Surg. 2007;16:591–595. doi: 10.1016/j.jse.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 9.Daigeler A., Vogt P.M., Bush K., Pennekamp W., Weyhe D., Lehnhardt M. Elastofibroma dorsi-differential diagnosis in chest wall tumors. World J Surg Oncol. 2007;5:1–15. doi: 10.1186/1477-7819-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mlika M., Abdeljalil N.B., Boudaya S., Ayadi-Kaddour A., Kilani T., Mezni F. About a challenging tumour, elastofibroma dorsi: an eight-case study. Pathologica. 2013;3:104–106. [PubMed] [Google Scholar]
- 11.Karakurt O., Kaplan T., Gunal N., Gulbahar G., Kocer B., Han S. Elastofibroma dorsi management and outcomes: review of 16 cases. Interact Cardiovasc Thorac Surg. 2014;2:197–201. doi: 10.1093/icvts/ivt442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.BenHassouna J., Hamdi N., BenBachouche W., Bouzid T., Dhiab T., Rahal K. Elastofibroma dorsi. Orthop Traumatol. 2010;96(6):717–720. doi: 10.1016/j.otsr.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 13.Koksel O., Apaydin F.D., Ayan E., Demir M., Ozdulger A. Elastofibroma dorsi: review of eight cases. Surg Today. 2010;40(5):423–427. doi: 10.1007/s00595-008-4071-5. [DOI] [PubMed] [Google Scholar]
- 14.Abat F., Álvarez C., Trullols L., Peiró A., Bagué S., Gracia I. Elastofibroma dorsi: a 7-year follow-up of 37 cases and a review of the literature. Rev Esp Cir Ortop Traumatol. 2012;56(4):295–299. doi: 10.1016/j.recot.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Battaglia M., Vanel D., Pollastri P., Balladelli A., Alberghini M., Staals E.L. Imaging patterns in elastofibroma dorsi. Eur J Radiol. 2009;72:16–21. doi: 10.1016/j.ejrad.2009.05.024. [DOI] [PubMed] [Google Scholar]
- 16.Tamimi Mariño I., Sesma Solis P., Pérez Lara A., Martinez Malo J., Vazquez M.L., Tamimi F. Sensitivity and positive predictive value of magnetic resonance imaging in the diagnosis of elastofibroma dorsi: review of fourteen cases. J Shoulder Elbow Surg. 2013;22:57–63. doi: 10.1016/j.jse.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Lococo F., Cesario A., Mattei F., Petrone G., Vita L.M., Petracca-Ciavarella L. Elasto fibroma dorsi: clinicopathological. Analysis of 71 cases. Thorac Cardiovasc Surg. 2013;61:215–222. doi: 10.1055/s-0032-1328932. [DOI] [PubMed] [Google Scholar]
- 18.Coskun A., Yildirim M. Bilateral elastofibroma dorsi. Ann Thorac Surg. 2011;92:2242–2244. doi: 10.1016/j.athoracsur.2011.05.112. [DOI] [PubMed] [Google Scholar]
- 19.Nagamine N., Nohora Y., Ito E. Elastofibroma in Okinawa. A clinicopathologic study of 170 cases. Cancer. 1982;50:1794–1805. doi: 10.1002/1097-0142(19821101)50:9<1794::aid-cncr2820500925>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 20.Briccoli A., Casadai R., Di Renzo M., Favale L., Bacchini P., Bertoni F. Elastofibroma dorsi. Surg Today. 2000;30:147–152. doi: 10.1007/PL00010063. [DOI] [PubMed] [Google Scholar]


