Highlights
-
•
The overall mortality rate reported in the studies in Japan (25%) is considerably higher than that reported in a systematic review conducted of similar studies in other countries (3.3%).
-
•
Japan is a low-risk area for amebiasis, and many physicians fail to consider amebiasis in the differential diagnosis of acute appendicitis. In all of the cases, the diagnosis occurred only after surgery.
-
•
It is important to conduct further examinations, including those for amebiasis, when appendectomy does not resolve acute appendicitis.
Keywords: Amebiasis, Acute appendicitis, Metronidazole
Abstract
INTRODUCTION
Outside of these high-risk regions, acute amebic appendicitis is considerably rarer and the mortality rate is much higher than with non-amebic appendicitis.
PRESENTATION OF CASE
A 31-year-old woman presented with fever and right lower abdominal pain with no history of traveling abroad or sexual infection. Computed tomography revealed a dilated appendix and thickened cecal and ascending colon walls. She underwent an appendectomy for appendicitis. Owing to a lack of symptom resolution, we performed a pathologic examination of the appendix again that revealed multiple Entamoeba histolytica trophozoites; the serum amebic antibody was positive. She was treated postoperatively with metronidazole for amebiasis and discharged on postoperative day 12.
DISCUSSION
The mortality rate and frequency of severe postoperative intraabdominal complications were higher in the Japanese literature (1995–2013) (25% and 33%, respectively) than in other developed countries (3.3% and 19.4%, respectively). Japan is a low-risk area for amebiasis; many physicians fail to consider amebiasis in the differential diagnosis of acute abdomen. It is important to conduct further examinations, including those for amebiasis, when appendectomy does not resolve acute appendicitis.
CONCLUSION
We report a case of acute amebic appendicitis in a 31-year-old woman and review the ages at presentation, causative factors, treatments, and outcomes of 11 cases reported in Japan between 1995 and 2013.
1. Introduction
Acute appendicitis, which occurs when the appendix lumen is obstructed,1 is the most common cause of acute abdominal pain and often requires surgical intervention. Appendiceal obstruction can be caused by fecaliths, calculi, lymphoid hyperplasia, infectious processes, or benign or malignant tumors.2
However, appendicitis of amebic origin is considered relatively rare, with reported incidence of 0.5–2.3% in an amebiasis endemic area.3,4 Outside of these high-risk regions, acute amebic appendicitis is considerably rarer and often not at the forefront of the treating physician's mind, which may result in a missed diagnosis or misdiagnosis and unfavorable prognosis for patients.5 Moreover, complicated appendicitis is present in 30.7% cases of amebic appendicitis, and the mortality rate is much higher than with non-amebic appendicitis.5,6 In this paper, we report a case of acute amebic appendicitis in a 31-year-old woman and review the ages at presentation, causative factors, treatments, and outcomes of 11 cases reported in Japan between 1995 and 2013.
2. Case
A 31-year-old woman was admitted to our hospital with acute right lower abdominal pain that had lasted for 2 days prior to admission. Her medical history revealed several bouts of right lower abdominal pain that resolved with conservative treatment. She had no history of traveling abroad or a sexually transmitted infection such as human immunodeficiency virus (HIV) infection, hepatitis B virus (HBV), or syphilis. On admission, her body temperature was 37.5 °C. Abdominal examination revealed diffuse tenderness in the right lower abdomen with positive guarding and rebound tenderness at the McBurney point. Laboratory tests revealed a C-reactive protein (CRP) level of 15.06 mg/dL and white blood cell (WBC) count of 8620 μL−1. Abdominal computed tomography (CT) showed a dilated appendix with maximum diameter of 2 cm and thickened cecal and ascending colon walls (Fig. 1), which was consistent with acute appendicitis. According to the patient's request, she was treated with antibiotics (intravenous cefmetazole) for 2 days without improvement. Therefore, an appendectomy was performed. Her appendix showed acute inflammation, especially from the cecum to the root of the appendix, without necrosis, perforation, or formation of localized abscess. Histopathology revealed phlegmonous appendicitis.
Fig. 1.
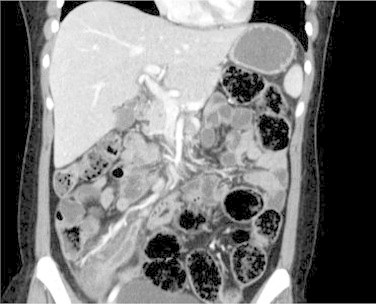
An axial pelvic and abdominal image from a contrast-enhanced computed tomography (CT) scan obtained on admission showing marked thickening of the appendix and the colonic wall, especially prominent in the terminal ileum and ascending colon.
The clinical course after admission is described in Fig. 2. After the appendectomy, her body temperature remained >38 °C, and her CRP and WBC were elevated more than before the operation. Abdominal CT on the third postoperative day showed thickened cecal and ascending colon walls. We considered pseudomembranous enterocolitis and changed the treatment from intravenous cefmetazole to oral vancomycin. However, the test for Clostridium difficile was negative, and her symptoms and laboratory data did not improve. Therefore, we also considered an amebic infection; on the sixth postoperative day, we examined a fecal culture that was immediately maintained at 37 °C, tested for serum amebic antibody, requested the pathologists to reexamine the pathology regarding amebic infection from her appendix, and added oral metronidazole to her treatment. Following the oral metronidazole treatment, her clinical condition significantly improved. The pathologic examination of the appendix with periodic acid–Schiff (PAS) stain revealed multiple trophozoites of Entamoeba histolytica (Fig. 3), and her serum amebic antibody was positive. On the 12th day after the procedure, the patient was discharged home; in addition, 12 days after the oral metronidazole treatment, we treated the cyst form of the parasite with paromomycin. She had no further recurrence for 6 months.
Fig. 2.
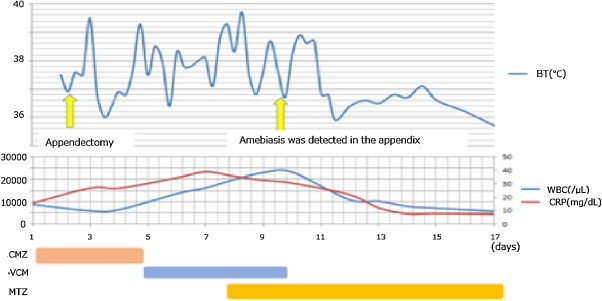
The clinical course after admission in a patient treated for acute appendicitis.
BT, body temperature; CMZ, cefmetazole; VCM, vancomycin; MTZ, metronidazole.
Fig. 3.
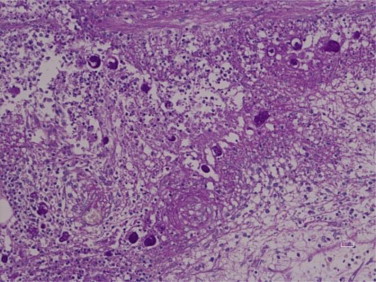
Periodic acid–Schiff stain (400× magnification), showing clusters of trophozoites of Entamoeba histolytica.
3. Discussion
Based on this experience with amebiasis presenting as acute appendicitis that was treated with appendectomy and oral metronidazole, we would like to emphasize 2 points. First, even after the appendectomy, there was still considerable inflammation of the intestinal wall that required metronidazole treatment. Second, amebiasis was not detected with the usual histopathology of the appendix and fecal culture. Histopathological examination using PAS stain and a fecal culture that was immediately maintained at 37 °C was required for diagnosis.7,8
We conducted a search of Japan Center Reviews for similar cases in the past 18 years and reviewed the preoperative clinical features, treatment of choice, and outcomes of the 11 patients in the resulting publications (Table 1).5,9–18 Including the present case, 9 were men (75%), and 3 were women (25%), with an average age of 42.6 years (range, 25–60 years). Almost all (84%) experienced severe pain in the right lower abdominal quadrant, with coexisting bloody diarrhea in 2 of these cases (17%). A history of traveling to a high- or moderate-risk country was cited in 3 cases (25%). The diagnoses of all patients were acute appendicitis, but only one case had a preoperative diagnosis of amebiasis and was treated medically. One of the cases treated with an appendectomy required a total colon resection because of fulminant colitis. After the operation, 8 patients (73%) did not experience symptom improvement. Severe postoperative intraabdominal complications (higher than grade III on the Clavien scale) occurred in 4 cases (37%).
Table 1.
Review of amebiasis cases reported in Japan between 1995 and 2013, including the present case STI, sexually transmitted infection; F, female; M, male; RLA, right lower abdominal pain; HIV, human immunodeficiency virus; HCV, hepatitis C virus; HBV, hepatitis B virus.
| Year | Author | Age | Sex | History of travel | STI | Chief complaint | Diarrhea | Operation | Method of diagnosis | Survival |
|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | Present case | 31 | F | No | No | RLA | No | Appendectomy | Histological pathology | Survived |
| 2012 | Sonoo [9] | 52 | F | No | Not reported | Abdominal pain | No | Ileocecal resection | Morbid anatomy | Deceased |
| 2011 | Kojyou [10] | 53 | M | Yes | HIV, HCV, syphilis | RLA | No | Appendectomy | Morbid anatomy | Deceased |
| 2009 | Hayami [11] | 51 | M | No | No | RLA | No | Right hemicolectomy | Biopsy | Survived |
| 2007 | Isihara [13] | 38 | M | No | HIV | RLA | Yes | Appendectomy | Histological pathology | Survived |
| 2006 | Okumura[12] | 25 | F | Yes | No | Vomiting | No | Appendectomy | Histological pathology | Survived |
| 2005 | Suzuki [14] | 60 | M | No | No | RLA | No | Appendectomy | Morbid anatomy | Deceased |
| 2005 | Miyasaka [15] | 25 | M | Yes | HIV | RLA | No | Appendectomy | Fecal culture | Survived |
| 2004 | Ohe [17] | 33 | M | No | HBV | RLA | No | Appendectomy | Histological pathology | Survived |
| 2002 | Yanagisawa [16] | 51 | M | No | No | RLA | No | Appendectomy | Biopsy | Survived |
| 2000 | Gotohda [5] | 45 | M | No | No | RLA | Yes | Appendectomy | Histological pathology | Survived |
| 1996 | Ou [18] | 48 | M | No | No | Diarrhea | Yes | No | Biopsy | Survived |
This article is published Open Access at sciencedirect.com. It is distributed under the IJSCR Supplemental terms and conditions, which permits unrestricted non commercial use, distribution, and reproduction in any medium, provided the original authors and source are credited.
The overall mortality rate reported in the studies in Japan (25%) (Table 1) is considerably higher than that reported in a systematic review conducted of similar studies in other countries5 (3.3%). The same is true for severe postoperative intraabdominal complications (33 vs. 19.4%).
One potential explanation for these differences is that, compared to the other countries, accurate diagnosis and treatment with oral metronidazole was delayed in Japan, with 9 of the 12 cases requiring further postoperative investigations and treatment. Oral metronidazole is required for amebiasis even after appendectomy. The amebiasis infection is spread through ingestion of the cyst form of the parasite and is generally transmitted via the fecal-oral route, although it can also be transmitted indirectly through contact with dirty hands or dirty objects, in addition to anal-oral contact. Excystation occurs in the small intestine, where motile and potentially invasive trophozoites are formed that typically migrate to the large intestine and aggregate in the intestinal mucin layer to form new cysts.19 Therefore, aggregated trophozoites in the cecum and small intestine after appendectomy are likely and require treatment with antibiotics.
In addition, Japan is a low-risk area for amebiasis, and many physicians fail to consider amebiasis in the differential diagnosis of acute appendicitis.5 Furthermore, trophozoites are difficult to detect in the usual histopathological examination or fecal culture.19 In a retrospective study of amebic appendicitis and previous case reports, all of the patients presented with symptoms that suggested acute appendicitis, but few had symptoms of dysentery. In all of the cases, the diagnosis occurred only after surgery. Moreover, in 3 of the 12 cases, amebiasis was found only in morbid anatomy.
Therefore, when symptoms are not improved after the operation, it is important to investigate other potential causative underlying medical diseases such as amebiasis. When amebiasis is suspected, pathologists and laboratory technicians should be alerted to the possibility of amebiasis and correctly assess the collected samples because histopathological examination with PAS stain and a fecal culture that is maintained at 37 °C is required for definitive diagnosis.
Conflict of interest statement
The authors have no conflict of interest.
Funding
No sources of funding.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Author contribution
Daisuke Ito contributed to data collections and writing. Shojiro Hata, Seiichiro Shimizu, Kaoru Kobayashi, Masanori Teruya, Michio Kaminishi contributed to data collections.
References
- 1.Arnbjörnsson E., Bengmark S. Obstruction of the appendix lumen in relation to pathogenesis of acute appendicitis. Acta Chir Scand. 1983;149:789–791. [PubMed] [Google Scholar]
- 2.Burkitt D.P. The aetiology of appendicitis. Br J Surg. 1971;58:695–699. doi: 10.1002/bjs.1800580916. [DOI] [PubMed] [Google Scholar]
- 3.Nadler S., Cappell M.S., Bhatt B., Matano S., Kure K. Appendiceal infection by Entamoeba histolytica and Strongiloides stercoralis presenting like acute appendicitis. Dig Dis Sci. 1990;35:603–608. doi: 10.1007/BF01540408. [DOI] [PubMed] [Google Scholar]
- 4.Gotohda N., Itano S., Okada Y., Horiki S., Endo A., Terada N. Acute appendicitis caused by amebiasis. J Gastroenterol. 2000;35:861–863. doi: 10.1007/s005350070024. [DOI] [PubMed] [Google Scholar]
- 5.Otan E., Akbulut S., Kayaalp C. Amebic acute appendicitis: systematic review of 174 cases. World J Surg. 2013;37:2061–2073. doi: 10.1007/s00268-013-2079-5. [DOI] [PubMed] [Google Scholar]
- 6.Guzmán-Valdivia G. Acute amebic appendicitis. World J Surg. 2006;30:1038–1042. doi: 10.1007/s00268-005-0104-z. [DOI] [PubMed] [Google Scholar]
- 7.Peison B. Acute localized amebic appendicitis: report of a case. Dis Colon Rectum. 1973;16:532–536. doi: 10.1007/BF02588885. [DOI] [PubMed] [Google Scholar]
- 8.Nadler S., Cappell M.S., Bhatt B., Matano S., Kure K. Appendiceal infection by Entamoeba histolytica and Strongyloides stercoralis presenting like acute appendicitis. Dig Dis Sci. 1990;35:603–608. doi: 10.1007/BF01540408. [DOI] [PubMed] [Google Scholar]
- 9.Tomohiro S., Yukisuke M., Ayuko S., Naoyuki U., Yukio T., Yukiko K. Teishin Igaku. 2012;64:213–221. [Google Scholar]
- 10.Miyako K., Yusuke T., Tasuku M., Atsuo K., Kyoko K., Shinpei M. The case of the AIDS patient whom it occurred from acute appendicitis, and died for a multiple liver abscess by the amoebic dysentery and sepsis. J Jpn Soc Surg Infect. 2011;8:387–391. [Google Scholar]
- 11.Masaru H., Akiho F., Masahiro M., Tsunehito K., Kazuki A., Shingo K. A case of fulminant amebic colitis with colon perforation. J Jpn Surg Assoc. 2009;70:2048–2115. [Google Scholar]
- 12.Okumura K., Lee C.J., Endo Y., Kurioka H., Enoki Y., Hosokawa Y. Amoebic colitis presenting as acute appendicitis. Jpn J Gastroenterol Surg. 2006;39:1547–1552. [Google Scholar]
- 13.Ishihara S., Kitayama J., Nagawa H. Clinical challenges and images in GI: amoebic appendicitis. Gastroenterology. 2007;133(1412):1747. doi: 10.1053/j.gastro.2007.09.053. [DOI] [PubMed] [Google Scholar]
- 14.Yasuhiro S., Yasushi A., Ryoji Y., Akiharu O., Hideki K., Daisaku H. Amebiases: two autopsy cases where diagnosis could not be established during the lifetime of the patients. Jpn J Diagn Pathol. 2005;22:25–28. [Google Scholar]
- 15.Yoshihiro M., Daisuke Y., Masamune N., Yasuto W., Nukashi D. A case of amebic appendicitis. Dig Surg. 2005;28:503–506. [Google Scholar]
- 16.Yanagisawa M., Kaneko M., Aizawa T., Michimata T., Takagi H., Mori M. A case of amebic liver abscess complicated by hemobilia due to rupture of hepatic artery aneurysm. Hepatogastroenterology. 2002;49:375–378. [PubMed] [Google Scholar]
- 17.Ohe T., Yamaguchi T., Kitakado Y. A case of successfully treated amebic colitis with total colon necrosis. J Jpn Surg Assoc. 2004;65:3231–3235. [Google Scholar]
- 18.Kouji O. Amoebic colitis restricted in the cecum and appendix, report of a case. Stomach Intest. 1995;30:1209–1214. [Google Scholar]
- 19.Haque R., Huston C.D., Hughes M., Houpt E., Petri W.A., Jr. Amebiasis. N Engl J Med. 2003;348:1565–1573. doi: 10.1056/NEJMra022710. [DOI] [PubMed] [Google Scholar]


