Highlights
-
•
Primary malignant hepatic mesothelioma is usually diagnosed postoperatively, as there are no specific radiologic features for this tumor.
-
•
The surgeon should be alert in cases of patients with known history of asbestos exposure.
-
•
Proper surgical treatment may offer prolonged survival to the patient, without adjuvant therapy.
Keywords: Malignant mesothelioma, Intrahepatic, Epithelioid type
Abstract
INTRODUCTION
Primary malignant hepatic mesotheliomas are extremely rare. We report the case of a patient with primary intrahepatic malignant mesothelioma who was treated in our department.
PRESENTATION OF CASE
A 66-year old male patient was admitted to our department for the evaluation of anemia. An abdominal computed tomography scan revealed a large space occupying lesion in the right liver lobe.
DISCUSSION
The tumor was subsequently resected and a diagnosis of primary intrahepatic malignant mesothelioma was made after pathologic examination. The patient did not receive adjuvant therapy and is currently alive and free of disease, 36 months after the resection.
CONCLUSION
To our knowledge this is the eighth adult case of primary intrahepatic malignant mesothelioma reported in the literature. These tumors are rarely diagnosed preoperatively. Absence of previous asbestos exposure does not exclude malignant mesothelioma from the differential diagnosis. Proper surgical treatment may offer prolonged survival to the patient, without adjuvant therapy.
1. Introduction
Mesothelioma is an insidious neoplasm arising from the mesothelial surfaces of the pleural and peritoneal cavities, the tunica vaginalis, or the pericardium. Eighty percent of all cases are pleural in origin. The predominant cause of malignant mesothelioma is inhalational exposure to asbestos. The annual incidence of mesothelioma in the United States is estimated to be approximately 3300 cases per year.1 Primary malignant mesotheliomas arising in the liver are extremely rare. We present the case of a 66-year old male patient with primary intrahepatic malignant mesothelioma who was treated in our department.
2. Presentation of case
A 66-year old male patient was referred to our department in November 2011 with a history of malaise during the previous two months. The patient's medical history was significant only for arterial hypertension, being treated with two antihypertensive drugs. The patient had no history of prior asbestos exposure or chronic liver disease. Previous laboratory examinations had revealed anemia (Hb = 8.5 g/dL, Hct% = 29.3%) and the patient had received oral iron supplementation for two months with no improvement. Colonoscopy and gastroscopy had no significant findings, apart from mild gastritis and hemorrhoids.
Upon presentation, physical examination revealed a palpable mass in the right upper abdomen. There were no signs of jaundice or abdominal tenderness. Significant results of laboratory tests on admission were as follows: hemoglobin = 7.5 g/dL, hematocrit = 23.8%, INR = 1.4, alkaline phosphatase (ALP) = 227 IU/L (normal range 40–150), total proteins = 9.1 g/dL (normal range 6.7–8.8), albumin = 2.3 g/dL (normal range 3.5–5), C-reactive protein = 67 mg/L (normal range <5), carcinoembryonic antigen (CEA) = 1.9 μg/L (normal range <5), a-fetoprotein (AFP) = 2.4 μg/L (normal range <20), Ca19-9 <2 U/mL (normal range <37), Ca125 = 259.7 U/mL (normal range <35), Ca15-3 = 69 U/mL (normal range <30). The rest of the laboratory examinations were within normal range.
The patient underwent computed tomography of the chest and abdomen, which revealed an extensive space occupying lesion in the right liver lobe, measuring 17 cm in diameter. The tumor displayed abnormal enhancement following intravenous administration of contrast material (Figs. 1 and 2). A core needle biopsy which was performed was not helpful as it contained only necrotic material without evidence of malignancy.
Fig. 1.
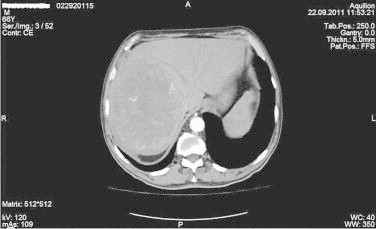
Computed tomography showing an ill defined, intraparenchymal tumor obliterating most of the right lobe of the liver (transverse section).
Fig. 2.
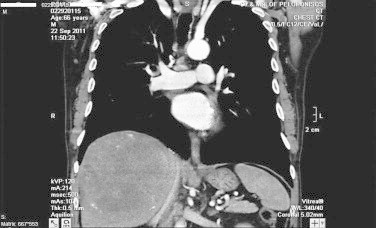
Computed tomography showing an ill defined, intraparenchymal tumor obliterating most of the right lobe of the liver (coronal section).
On November 7, 2011 the patient underwent exploratory laparotomy which revealed a sizable mass in the right liver lobe without evidence of metastatic disease in the abdomen. A typical right hepatectomy was undertaken. In the first postoperative day liver function tests revealed a sudden increase in bilirubin and transaminases levels, which was attributed to hemolysis and transient liver failure. Liver function tests returned progressively to normal and the patient was discharged on the seventh postoperative day.
On gross examination the lobectomy specimen was massively infiltrated by a brown, partly hemorrhagic tumor, with soft consistency, measuring 18 × 15.5 × 8 cm, extending to the capsular surface (Fig. 3). Microscopically, the tumor was composed of tubular or cord like arrangements of epithelioid cells with eosinophilic cytoplasm and atypical nuclei (Fig. 4). Immunohistochemically, tumor cells were positive for EMA, CK-7, CK 5/6, Calretinin (Fig. 5), Pankeratin and Vimentin, but negative for CEA (monoclonal), P-63, CD-10, CK-20, Synaptophysin, Chromogranin, CD-56, TTF-1, HepPar-1, HBsAg, CD-15, CD-30, PLAP and β-HCG. Immunohistological analysis of the proliferation marker Ki-67 showed expression in 15–20% of the tumor cells. These findings were consistent with our diagnosis of primary intrahepatic malignant mesothelioma of the epithelioid type. Resection margins were free of disease.
Fig. 3.
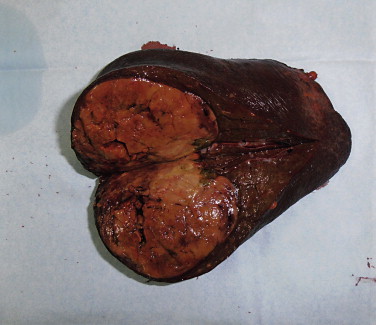
Macroscopic view of the surgical specimen, showing a large intraparenchymal tumor of the right liver lobe.
Fig. 4.
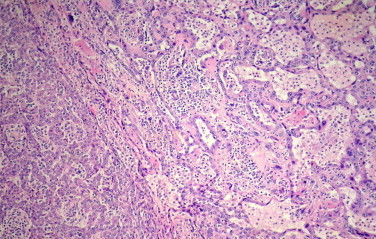
Irregular cystic and tubular spaces lined by a single layer of mesothelial cells or compact pattern of anastomosing cords of neoplastic cells.
Fig. 5.
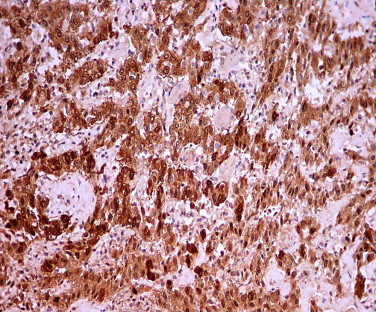
Antibody against calretinin is the most specific and reproducible positive marker of epithelioid mesothelioma. Cells labeled by the antibody display both a cytoplasmic and a nuclear staining pattern.
After oncology consultation, the patient did not receive adjuvant chemotherapy postoperatively. He remains alive and free of disease 36 months after the operation.
3. Discussion
Primary intrahepatic malignant mesotheliomas are extremely rare. To our knowledge this is the eighth adult case of primary intrahepatic malignant mesothelioma reported in the literature.2–8 There have been reports of mesotheliomas originating in the falciform ligament9 or the liver surface,10 which probably represent peritoneal mesotheliomas involving the liver.
Three different characteristic histological patterns can be discriminated based on routine hematoxylin–eosin staining: epithelioid, sarcomatoid and biphasic. Six cases (including ours) out of eight reported in the literature, were of the epithelioid type, while two were of the biphasic type.
In detail, there were four men and three women, aged between 50 and 68 years old. Five patients had no history of asbestos exposure, one patient had occupational exposure to asbestos and pulmonary asbestosis and in another case there was no indication. One patient without asbestos exposure had chronic hepatitis C. Tumor size ranged between 3.2 and 16 cm. All patients except from one had solitary lesions. Seven patients were surgically treated. In one patient hepatic rupture occurred due to rapid tumor growth with consequent clinical deterioration, thus not allowing surgical resection. Another patient developed subsequent lymph node metastases and was treated with repeated lymphadenectomy, resulting in prolonged survival.4,11 No clinical or radiological evidence of recurrent disease has been detected in our patient up to 36 months following resection. Table 1 summarizes the seven cases of primary intrahepatic malignant mesotheliomas reported in the literature.
Table 1.
Primary intrahepatic malignant mesotheliomas reported in the literature.
| Author | Year | Sex | Age (years) | Asbestos exposure | Viral hepatitis | Size (cm) | Type | Treatment | Reported survival (months) |
|---|---|---|---|---|---|---|---|---|---|
| Imura et al.2 | 2002 | Male | 64 | No | HepC | 3.2 | Epithelioid | Surgical | 40 |
| Leonardou et al.3 | 2003 | Female | 54 | Not reported | No | 16 | Epithelioid | Surgical | 2 |
| Gutgemann et al.4 | 2006 | Male | 62 | No | No | 5.8 | Epithelioid | Surgical | 36 |
| Sasaki et al.5 | 2009 | Male | 66 | Yes | No | 4.4 | Biphasic | Surgical | 6 |
| Dong et al.6 | 2013 | Female | 50 | No | No | Not reported | Epithelioid | Surgical | Not reported |
| Kim et al.8 | 2008 | Male | 53 | No | No | 13.0 | Biphasic | Surgical | Not reported |
| Inagaki et al.7 | 2013 | Female | 68 | No | No | 7.0 | Epithelioid | Supportive | Not reported |
4. Conclusion
In conclusion malignant mesothelioma of the liver is rarely diagnosed preoperatively, as there are no specific radiologic features for this tumor. Absence of previous asbestos exposure does not exclude malignant mesothelioma from the differential diagnosis. Proper surgical treatment may offer prolonged survival to the patient, without adjuvant therapy.
Conflict of interest statement
I. Perysinakis, A. Nixon, I. Spyridakis, G. Kakiopoulos, C. Zorzos and I. Margaris have no conflicts of interest or financial ties to disclose.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Study concept: Margaris I; Study design: Perysinakis I, Nixon A; Data collection: Spyridakis I, Kakiopoulos G, Zorzos Ch; Data analysis: Margaris I, Nixon A, Kakiopoulos G; Writing: Perysinakis I, Spyridakis I.
References
- 1.Teta M.J., Mink P.J., Lau E., Sceurman B.K., Foster E.D. US mesothelioma patterns 1973–2002: indicators of change and insights into background rates. Eur J Cancer Prev. 2008;17:525–534. doi: 10.1097/CEJ.0b013e3282f0c0a2. [DOI] [PubMed] [Google Scholar]
- 2.Imura J., Ichikawa K., Takeda J., Iwasaki Y., Tomita S., Kubota K. Localized malignant mesothelioma of the epithelial type occurring as a primary hepatic neoplasm: a case report with review of the literature. APMIS. 2002;110:789–794. doi: 10.1034/j.1600-0463.2002.t01-1-1101102.x. [DOI] [PubMed] [Google Scholar]
- 3.Leonardou P., Semelka R.C., Kanematsu M., Braga L., Woosley J.T. Primary malignant mesothelioma of the liver: MR imaging findings. Magn Reson Imaging. 2003;21:1091–1093. doi: 10.1016/s0730-725x(03)00197-8. [DOI] [PubMed] [Google Scholar]
- 4.Gutgemann I., Standop J., Fischer H.P. Primary intrahepatic malignant mesothelioma of epithelioid type. Virchows Arch. 2006;448:655–658. doi: 10.1007/s00428-006-0175-8. [DOI] [PubMed] [Google Scholar]
- 5.Sasaki M., Araki I., Yasui T., Kinoshita M., Itatsu K., Nojima T. Primary localized malignant biphasic mesothelioma of the liver in a patient with asbestosis. World J Gastroenterol. 2009;15:615–621. doi: 10.3748/wjg.15.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong A., Dong H., Zuo C. Multiple primary hepatic malignant mesotheliomas mimicking cystadenocarcinomas on enhanced CT and FDG PET/CT. Clin Nucl Med. 2014;39:619–622. doi: 10.1097/RLU.0b013e31828da61d. [DOI] [PubMed] [Google Scholar]
- 7.Inagaki N., Kibata K., Tamaki T., Shimizu T., Nomura S. Primary intrahepatic malignant mesothelioma with multiple lymphadenopathies due to non-tuberculous mycobacteria: a case report and review of the literature. Oncol Lett. 2013;6:676–680. doi: 10.3892/ol.2013.1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim D.S., Lee S.G., Jun S.Y., Kim K.W., Ha T.Y., Kim K.K. Primary malignant mesothelioma developed in liver. Hepatogastroenterology. 2008;55:1081–1084. [PubMed] [Google Scholar]
- 9.Marubayashi S., Ohdan H., Asahara T., Ikeda M., Hinoi T., Fukuma K. Malignant mesothelioma originating in the hepatic falciform ligament: report of a case. Surg Today. 1998;28:929–931. doi: 10.1007/s005950050254. [DOI] [PubMed] [Google Scholar]
- 10.Rout P., Rameshkumar K., Srikrishna N.V. Hepatic mesothelioma. Indian J Gastroenterol. 1999;18:176–177. [PubMed] [Google Scholar]
- 11.Buchholz B.M., Gutgemann I., Fischer H.P., Gorschluter M., Turler A., Kalff J.C. Lymph node dissection in primary intrahepatic malignant mesothelioma: case report and implications for diagnosis and therapy. Langenbecks Arch Surg. 2009;394:1123–1130. doi: 10.1007/s00423-009-0476-x. [DOI] [PubMed] [Google Scholar]


