Abstract
Being in a happy marriage is related to better psychological and physical health. This paper describes current approaches to conceptualizing and measuring marital quality and physical health, and results from a recent meta-analysis examining associations between marital quality and physical health outcomes. To illustrate the practical significance of these findings, this paper also illustrates how the magnitude of the marital quality – physical health association is similar in size to associations between health behaviors (diet, physical activity) and health outcomes, and briefly reviews the state of the science regarding plausible biobehavioral pathways that explain how marital functioning influences health. After describing the current state of research on factors that might modify the association between marital quality and health, particularly individual differences and gender, the paper concludes with implications of the past 50 years of research on marital quality and health for marriage in the 21st century.
Keywords: Marriage, health, marital quality, gender, close relationships
Marriage often involves a public commitment to stay together through “sickness and health,” and marriage itself may influence sickness and physical health as well. Being married is associated with better physical health compared to not being married. However, the effect is likely due to several factors (Liu & Umberson, 2008), including selection (healthier people may be more likely to get and stay married), shared resources (joint economic, psychosocial, and societal benefits), and the negative effects of marital disruptions (divorce, widowhood).
The degree of happiness with the marriage, or marital quality, is also related to physical health (Kiecolt-Glaser & Newton, 2001). In this article, I review the results from a recent meta-analysis of marital quality and physical health research (Robles, Slatcher, Trombello, & McGinn, 2014). Meta-analysis involves statistically aggregating results across studies to determine the magnitude of association (the effect size) between marital quality and health outcomes. I then describe plausible explanations for why marital quality might be related to physical health, whether such associations might differ for different people, and implications for marriage and health in the 21st century.
WHAT IS MARITAL QUALITY AND HOW IS IT RELATED TO HEALTH?
Researchers define marital quality as a subjective, global evaluation of the relationship and behaviors in the relationship (Fincham & Bradbury, 1987), and can be measured in a variety of ways. Common measures involve self-reported attitudes towards one’s partner and marriage, ratings of the frequency or acceptability of partners’ behaviors, or both. Researchers can also videorecord couples while they discuss problems or other issues in their relationship, and then code the recordings for behaviors indicating high (supportive behaviors) or low marital quality (hostile or withdrawing behaviors).
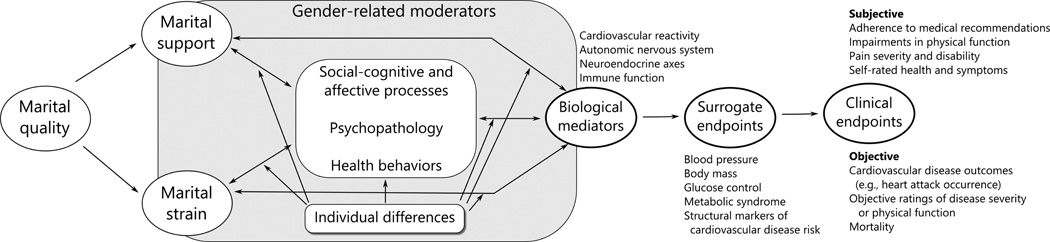
Likewise, physical health can be measured many ways, including physician ratings of a patient’s functioning, participant self-reports of how healthy they feel, or objective biological markers like blood pressure or cholesterol levels. The increased use of biological markers in psychological research makes developing a clear definition of what is (and is not) a physical health outcome critical. Fortunately, the National Institutes of Health provided useful definitions (Biomarker Definitions Working Group, 2001), which were used in the meta-analysis to categorize health outcomes into three categories: 1) Objective, and 2) Subjective clinical endpoints, where “clinical endpoints” refer to how a patient feels, functions, or survives; and 3) Surrogate endpoints, which are biological markers that can substitute for clinical endpoints based on empirical research. Examples of the latter include blood pressure and coronary artery calcification (for more examples see Table 1 in Robles et al., 2014). The theoretical framework guiding the meta-analysis shown in Figure 1 (derived from Burman & Margolin, 1992; Kiecolt-Glaser & Newton, 2001; Robles et al., 2014; Slatcher, 2010), includes examples of each type of health outcome.
Figure 1.
Conceptual framework depicting mechanisms that explain how marital quality may influence health, modifying factors such as individual differences and gender differences, and examples of surrogate and clinical endpoints.
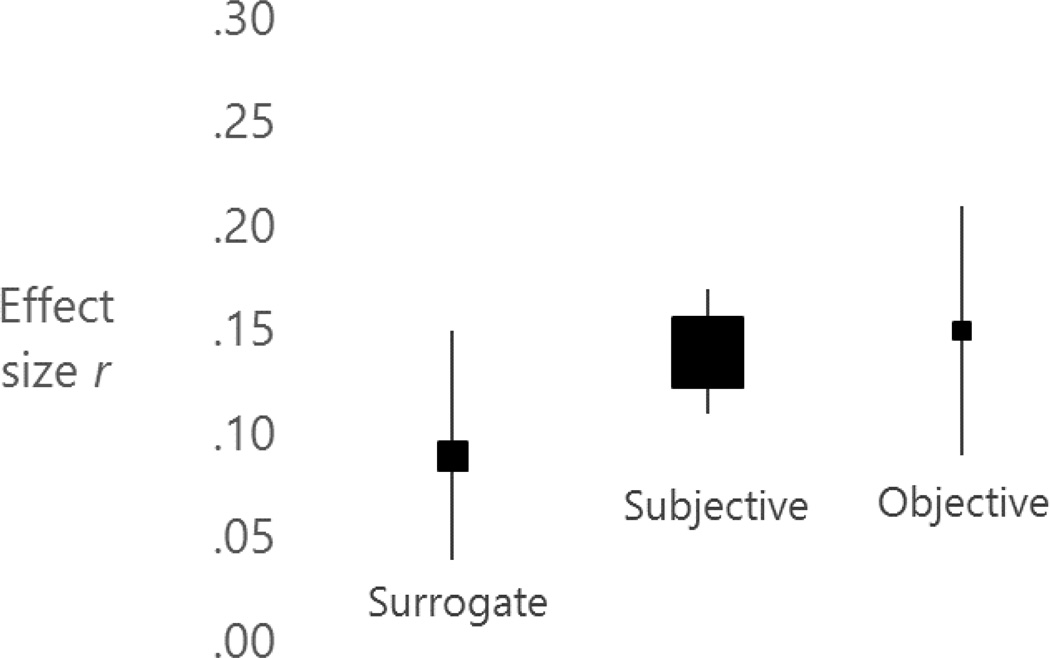
Across all health outcome categories, the meta-analysis showed small but consistent associations between greater marital quality and better health (Figure 2). Of course, health problems may put strain on the marriage, and reduce marital quality. However, in longitudinal studies, marital quality generally predicts poorer health, rather than the reverse. Unfortunately, most studies measured marital quality with measures that could not distinguish whether effects were due to high marital strain, low marital support, or both. Assessing both positive and negative aspects of marital functioning and relating both to health outcomes is a key direction for future work.
Figure 2.
Summary of effect sizes in the Robles et al. (2014) meta-analysis. Effect sizes are depicted as the correlation coefficient r, which ranges from −1.00 to +1.00. Positive values indicate that greater marital quality is related to better physical health. The size of the squares is proportional to the number of studies in each category. The height of the vertical bars indicates the 95% confidence interval around the effect size, which is the range of average effect sizes one would expect in 95 out of 100 future meta-analyses.
Across the studies, the strongest associations were for clinical endpoints, but overall the magnitude of associations would be considered “small” based on most statistical conventions. The small effects raise the question of whether the observed effect sizes have any practical significance for public health. One way to address practical significance is comparing the magnitude of effect sizes to other factors that influence physical health, notably behaviors like diet and physical activity. Thus, we compared effect sizes for links between marital quality and health to effect sizes for links between health behaviors and health outcomes, as daily activities like diet and physical activity are considered important targets for health promotion. Based on other meta-analytic findings, associations between diet, exercise, or sedentary activity and clinical endpoints were also small in magnitude (for specific details, see Robles et al., 2014). However, most experts would agree that changing health behaviors, despite their “small” effects, is important for improving public health.
Another way to address practical significance is considering whether plausible mechanisms explain the association between marital quality and health. Because physical health is the ultimate outcome, such mechanisms should be biologically plausible. In addition, much like health-related behaviors like physical (in)activity, candidate mechanisms should exert their effects on a daily basis. Fortunately, married partners have frequent contact with one another and likely think about each other on a daily basis. In the next section, I briefly review the viable psychosocial pathways that may explain how marital quality influences health.
PSYCHOSOCIAL AND BIOLOGICAL MECHANISMS
The center portion of Figure 1 describes candidate psychosocial mechanisms. Each mechanism likely exerts effects on a daily basis, and can influence biological mediators that can impact health. The evidence linking candidate psychosocial mechanisms to biological mediators is stronger for some mechanisms than others, notably psychopathology and health behaviors (see Robles et al., 2014 for an in-depth review).
Social-cognitive processes refer to how people think about their partner, such as how people explain their spouse’s behavior (Bradbury & Fincham, 1990). Emotional processes refer to how couples regulate each other’s emotional experience and expression. The presence and support provided by one’s spouse is an important resource for reducing negative emotions like anxiety or sadness (Beckes & Coan, 2011), which can further influence biological mechanisms. For example, disclosing thoughts and feelings to one’s spouse may have benefits for sleep, including reducing the time it takes to fall asleep, and increasing the amount of time asleep relative to time in bed (Kane, Slatcher, Reynolds, Repetti, & Robles, in press). Likewise, marital strain can also lead to persistent negative thoughts about one’s partner and difficulties regulating negative emotional experience and expression (Snyder, Simpson, & Hughes, 2006).
The negative effects of marital strain on regulating negative emotions may explain why poor marital quality increases risk for mood and anxiety disorders, and exacerbates and perpetuates substance use disorders (Whisman & Baucom, 2012). Accordingly, psychopathology, particularly depression, may explain the association between marital quality and health. In our meta-analysis, among studies that examined depression and marital quality as predictors, depression and marital quality were typically independent predictors of health, and marital quality often emerged with larger effect sizes than depression.
The associations between marital quality and substance use further suggests a mechanistic role for health behaviors. Relationship strain may increase health-compromising behaviors (substance use, unhealthy eating) as a coping strategy (Whisman, Uebelacker, & Bruce, 2006). More generally, couples tend to become more similar to each other in health behaviors like physical activity and diet over time (Homish & Leonard, 2008). Spouses also influence each others’ health behaviors, such as modeling healthy eating or pestering a spouse to eat healthier (Lewis & Butterfield, 2007). Support may increase personal resources, like self-efficacy, to aid efforts to change behavior (DiMatteo, 2004). Finally, marital quality may be particularly important for health behaviors that often co-occur between spouses, such as eating and sleep (Troxel, Robles, Hall, & Buysse, 2007).
The biological mediators in Figure 1 include the cardiovascular, endocrine, and immune systems (Kiecolt-Glaser & Newton, 2001). The typical approach to studying biological mediators in marriage research involves bringing couples into the laboratory, and asking them to discuss problems in their relationship for 10 – 30 minutes while obtaining physiological measures (e.g., heart rate, blood pressure, blood or saliva samples). Our meta-analysis showed clear evidence that greater marital quality is related to smaller increases in heart rate and blood pressure (smaller cardiovascular reactivity) during problem discussions. These findings are notable because greater cardiovascular reactivity during laboratory stressors (like playing a video game or performing mental arithmetic) predicts faster progression of atherosclerosis (Chida & Steptoe, 2010), the underlying biological process involved in heart disease. While similar links from marital quality to cardiovascular reactivity to atherosclerosis progression have not been made, clear associations exist between marital functioning and cardiovascular reactivity, and marital functioning and cardiovascular disease outcomes.
In summary, compelling data suggests that marital quality is associated with the mechanisms described in this section. However, the studies needed to establish these mechanisms as causal explanations or risk factors for poor health must: 1) explicitly test whether marital quality predicts changes in the explanatory mechanisms described above, and 2) test the degree to which changes in those mechanisms explain later health outcomes. Despite 50 years of research, no study to date has met those stringent criteria.
FOR WHOM IS MARITAL QUALITY PARTICULARLY IMPORTANT FOR HEALTH?
Figure 1 implies that two factors that could make the association between marital quality and health stronger for some and weaker for others: personality and gender (Figure 1). Research on the role of personality, marriage, and health has primarily focused on hostility and neuroticism (Smith, Baron, & Grove, 2013). Beyond modifying the association between marital quality and health, personality may directly impact psychological and behavioral processes, or modify the association between such processes and biological processes. For example, greater trait hostility is associated with greater relationship conflict and less supportive interpersonal relationships, greater physiological responses to interpersonal stressors, health-compromising behaviors like smoking, and depressive symptoms in married couples.
Unfortunately, no studies have directly tested whether personality characteristics modify associations between marital quality and health outcomes. Importantly, as noted by others (illustrated here with a hypothetical married couple named Don and Megan), Megan’s personality is Don’s social context (Smith et al., 2013). Thus, there may be important associations between Megan’s personality and Don’s health, or between Megan’s report of Don’s personality and Don’s health. An example of the latter is a study where spouse-reported ratings of the participant’s personality, particularly high negative affectivity, high dominance, and low affiliation, were related to greater participant’s coronary artery calcification (Smith et al., 2008).
There has been considerable interest in whether associations among marital quality, physiological mechanisms, and health differ between men and women (Kiecolt-Glaser & Newton, 2001; Wanic & Kulik, 2011). The meta-analysis found some, but not overwhelming evidence for gender differences in the link between marital quality and health, and gender differences that emerged were small in magnitude. Thus, extremely large sample sizes (> 1,500 people of each gender), rare in the vast majority of the existing research, are necessary to have enough statistical power to detect gender differences if they exist.
The small gender differences and the enormous sample sizes required to detect such differences suggest a need for focusing on gender-related factors, including the ways people think about relationships relative to themselves and/or focus on others to the potential exclusion of the self, and people’s roles in domestic labor and childcare (Kiecolt-Glaser & Newton, 2001). Incorporating gender-related and theory-based concepts that exist along a continuum more accurately reflects the state of gender relations in modern marriage, and has a side benefit of increasing statistical power. Moreover, same-sex marriage provides an unprecedented opportunity to examine the role of gender-related factors like domestic labor participation without confounds due to gender or biological sex.
Overall, “for whom is marital quality especially beneficial or detrimental?” is an incredibly understudied question. Factors including age, cohort, and well-established predictors of divorce and declines in marital satisfaction such as low socioeconomic status need significant attention in future research on marital functioning and health. Such work would strengthen our understanding of who is at risk for poor health, and identify targets for prevention and intervention efforts.
MARRIAGE AND HEALTH IN THE 21ST CENTURY
The past half-century of research suggests a small, but practically significant association between marital quality and health, which may be explained by a number of plausible psychosocial and biological mechanisms. Considerably less is known about “for whom” the association between marital quality and health is stronger or weaker. I conclude by describing the implications of this work for marriage in the 21st century, which is a product of major demographic and cultural changes, including declining marriage rates, and increasing cohabitation, same-sex marriage, and age of first marriage (Cherlin, 2010). Culturally, the meaning of marriage changed from a formal institution promoting family and economic stability, to a means of obtaining love and companionship, and more recently (late 20th century) into a means of pursuing personal choices and self-fulfillment (Cherlin, 2004).
Noting the demographic and cultural changes, scholars recently noted that modern marriages suffer from “suffocation” (Finkel, Hui, Carswell, & Larson, 2014). Compared to previous history, marriage is being “asked” to fulfill higher-order needs like happiness and personal fulfillment, while modern economic and social challenges make it difficult for couples to invest time and energy in the marriage to fulfill such needs (Finkel et al., 2014). Such challenges include income inequality, economic incentives that favor work over family time, and increased social isolation. Interestingly, those same challenges, combined with others (availability of unhealthy food, and factors that disrupt sleep and limit social activity) are obstacles to maintaining good physical health. To “oxygenate” marriage and thus increase marital quality, Finkel and colleagues suggest that couples make better use of or increase the amount of time and energy invested in marriage. Alternatively, couples might consider revising expectations about marriage; rather than expecting one’s marriage to be the critical source of personal fulfillment, looking to others in one’s social network to fulfill emotional needs may be more optimal (Finkel et al., 2014).
The research reviewed in this paper suggests that any efforts to increase marital quality may have the additional benefit of promoting health. However, strong empirical evidence demonstrating a clear causal role of marital quality for health will be needed to support this assertion. Thus, marital prevention and intervention research should consider measuring physical health outcomes in addition to mental health and marital outcomes. Indeed, couple-focused interventions in chronic illness show considerable promise (Martire, Schulz, Helgeson, Small, & Saghafi, 2010). At the same time, basic research on how and for whom marital quality impacts health is also needed to identify candidate treatment targets and mechanisms of change, and groups of people and patients who might benefit most from marital interventions.
ACKNOWLEDGEMENTS
Preparation of this manuscript was supported by William T. Grant Foundation Research Grant 9333 and National Institutes of Health Grants R21AG032494. I would like to thank the coauthors of the meta-analysis, Richard Slatcher, Joseph Trombello, and Meghan McGinn for their considerable efforts in analyzing articles, interpreting effect sizes, and writing the meta-analysis.
Footnotes
RECOMMENDED READINGS
- A compelling model that integrates research on the history and sociology of American marriage with psychological perspectives on needs and motivation, arguing that contemporary marriage often demands more than can be fulfilled given available time and energy.
- A seminal review of research on marital quality and physiological mechanisms, with a thorough discussion of gender-related factors that may explain gender differences in physiological responses to marital conflict.
- A quantitative review of 50 years of research on marriage and health outcomes, that contains significantly more detail about mechanisms, moderators, and future directions than the current paper.
- A review of research on marital functioning and physiological mechanisms, including the cardiovascular, endocrine, and immune systems.
- A recent review of research on personality and cardiovascular disease, with a focus on how interpersonal perspectives contribute to understanding how personality and emotional processes contribute to risk for cardiovascular disease in the context of marriage.
REFERENCES
- Beckes L, Coan JA. Social baseline theory: The role of proximity in emotion and economy of action. Social and Personality Psychology Compass. 2011;5:976–988. [Google Scholar]
- Biomarker Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clinical Pharmacology and Therapeutics. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- Bradbury TN, Fincham FD. Attributions in marriage: Review and critique. Psychological Bulletin. 1990;107:3–33. doi: 10.1037/0033-2909.107.1.3. [DOI] [PubMed] [Google Scholar]
- Burman B, Margolin G. Analysis of the association between marital relationships and health problems: An interactional perspective. Psychological Bulletin. 1992;112(1):39–63. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Cherlin AJ. The deinstitutionalization of American marriage. Journal of Marriage and Family. 2004;66:848–861. [Google Scholar]
- Cherlin AJ. Demographic trends in the United States: A review of research in the 2000s. Journal of Marriage and Family. 2010;72:403–419. doi: 10.1111/j.1741-3737.2010.00710.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension. 2010;55:1026–1032. doi: 10.1161/HYPERTENSIONAHA.109.146621. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Fincham FD, Bradbury TN. The assessment of marital quality: A reevaluation. Journal of Marriage and Family. 1987;49:797–809. [Google Scholar]
- Finkel EJ, Hui CM, Carswell KL, Larson GM. The suffocation of marriage: Climbing Mount Maslow without enough oxygen. Psychological Inquiry. 2014;25:1–41. [Google Scholar]
- Homish GG, Leonard KE. Spousal influence on general health behaviors in a community sample. American Journal of Health Behavior. 2008;32:754–763. doi: 10.5555/ajhb.2008.32.6.754. [DOI] [PubMed] [Google Scholar]
- Kane HS, Slatcher RB, Reynolds BR, Repetti RL, Robles TF. Daily self-disclosure and sleep in couples. Health Psychology. doi: 10.1037/hea0000077. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton T. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Butterfield RM. Social control in marital relationships: Effect of one’s partner on health behaviors. Journal of Applied Social Psychology. 2007;37:298–319. [Google Scholar]
- Liu H, Umberson DJ. The times they are a changin': Marital status and health differentials from 1972 to 2003. Journal of Health and Social Behavior. 2008;49(3):239–253. doi: 10.1177/002214650804900301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Annals of Behavioral Medicine. 2010;40(3):325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proulx CM, Helms HM, Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family. 2007;69(3):576–593. [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: A meta-analytic review. Psychological Bulletin. 2014;140:140–187. doi: 10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slatcher RB. Marital functioning and physical health: Implications for social and personality psychology. Social and Personality Psychology Compass. 2010;4:455–469. [Google Scholar]
- Smith TW, Baron CE, Grove JL. Personality, emotional adjustment, and cardiovascular risk: Marriage as a mechanism. Journal of Personality. 2013 doi: 10.1111/jopy.12074. [DOI] [PubMed] [Google Scholar]
- Smith TW, Uchino BN, Berg, Cynthia A, Florsheim P, Pearce G, Hawkins M, Yoon H. Associations of self-reports versus spouse ratings of negative affectivity, dominance, and affiliation with coronary artery disease: Where should we look and who should we ask when studying personality and health? Health Psychology. 2008;27(6):676–684. doi: 10.1037/0278-6133.27.6.676. [DOI] [PubMed] [Google Scholar]
- Snyder DK, Simpson JA, Hughes JN, editors. Emotion regulation in couples and families: Pathways to dysfunction and health. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews. 2007;11:389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wanic R, Kulik J. Toward an understanding of gender differences in the impact of marital conflict on health. Sex Roles. 2011;65(5–6):297–312. [Google Scholar]
- Whisman MA, Baucom DH. Intimate relationships and psychopathology. Clinical Child and Family Psychology Review. 2012;15:4–13. doi: 10.1007/s10567-011-0107-2. [DOI] [PubMed] [Google Scholar]
- Whisman MA, Uebelacker LA, Bruce ML. Longitudinal association between marital dissatisfaction and alcohol use disorders in a community sample. Journal of Family Psychology. 2006;20:164–167. doi: 10.1037/0893-3200.20.1.164. [DOI] [PubMed] [Google Scholar]