Highlights
-
•
Morgagni hernia is a rare diaphragmatic hernia and standard therapy has not been established.
-
•
The laparoscopic repair of a rare diaphragmatic Morgagni hernia in an elder patient using the reduced port approach is described.
-
•
This reduced port approach is a good indication for this type of hernia because of less invasive ness, cosmetics and safety.
Keywords: Morgagni hernia, Reduced port surgery, Laparoscopic surgery
Abstract
INTRODUCTION
The laparoscopic repair of a rare diaphragmatic Morgagni hernia using the reduced port approach is described.
PRESENTATION OF CASE
An 85-year-old female presented with a 2 days history of upper abdominal discomfort and loss of appetite. We diagnosed her condition as a Morgagni hernia by morphological studies and performed laparoscopic mesh placement with a multi-channel port and 12-mm port. This elderly patient had a rapid postoperative recovery. A 2-year follow-up CT showed no recurrence of the hernia.
DISCUSSION
Recent trends in laparoscopic procedures have been toward minimizing the number of incisions to reduce invasiveness. This case indicated that the reduced port approach can be considered a suitable and safe procedure for treatment of Morgagni hernia.
CONCLUSION
The reduced port approach is a good indication for Morgagni hernia.
1. Introduction
Morgagni hernia is a congenital herniation of abdominal viscera into the thoracic cavity through a retrosternal diaphragmatic defect.1,2 It could be an incidental diagnosis in adulthood or could present with obstructive symptoms from the herniated viscera.3 Symptomatic Morgagni hernia sometimes requires surgical treatment because of the risk of incarceration.4 Surgical treatment consists of direct closure or mesh placement for the diaphragmatic defect, or suturing by transabdominal or transthoracic access.5–7 We report a patient with Morgagni hernia who underwent a laparoscopic mesh placement with reduced port surgery (RPS).
2. Presentation of case
An 85-year-old female presented in ER with a 2-day history of upper abdominal discomfort and loss of appetite. She had never experienced the same symptoms previously, and she denied any history of abdominal trauma. She had a history of hypertension and was taking medicines for that condition. Physical examination revealed no palpable mass in the upper abdomen, and local tenderness on upper abdomen was shown without any peritoneal inflammatory signs.
Serum blood test showed a hyperlipidemia and mild elevation of urea nitrogen (total cholesterol, 250 mg/dl; urea nitrogen, 22.5 mg/dl). The white blood cell count and C-reactive protein level were not elevated. A CT scan showed a huge diaphragmatic anterior hernia with a segment of transverse colon and fat tissue migration (Fig. 1). The diagnosis of Morgagni hernia was made and the patient was considered for repair of the diaphragmatic defect by the laparoscopic approach.
Fig. 1.
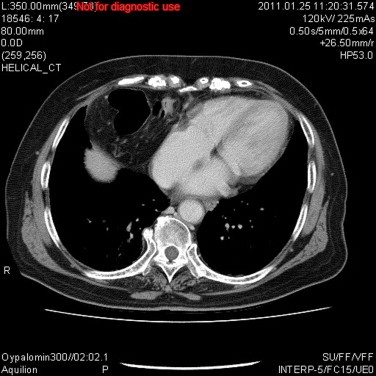
A CT scan showed a huge diaphragmatic anterior hernia with partial transverse colon and fat tissues migration.
Under general anesthesia in the lithotomy position, the SILS port (Covidien, Tokyo, Japan) was inserted into a 2.5-cm umbilical incision vertically. After inspection of the visceral space, a second port, 12 mm in size, was inserted into the left lower abdomen. The herniated bowel and fat tissues were gently pulled down with grasping forceps and placed entirely into the abdominal cavity (Fig. 2). The defect was ovoid and approximately 5 cm in size, and difficult to close by the suturing technique; therefore we performed mesh placement with Gore-Tex Dual Mesh (Gore Inc., Tokyo, Japan) after partial resection of the hernia sac (Fig. 3). Operation time and operative blood loss were 157 min and 5 ml, respectively.
Fig. 2.
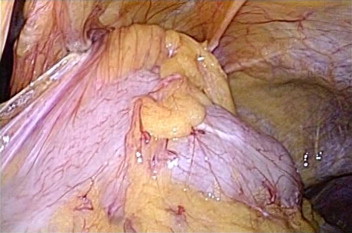
Intra-operative findings in this case. Partial segment of transverse colon with fat tissues is inserted into the hernia cavity.
Fig. 3.
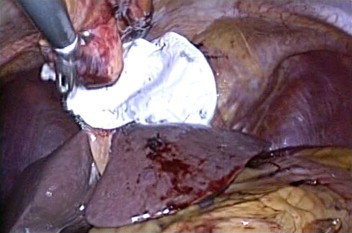
Intra-operative-findings of mesh placement. Non-absorbable mesh covers the hernia cavity.
The patient started to eat a soft meal on day 1 after surgery and was discharged from our hospital on day 8 after surgery without any symptoms. After 6-month, 12-month, and 24-month follow-ups, the patient had no sign of recurrence of the Morgagni hernia (Figs. 4 and 5).
Fig. 4.

Surgical wound after surgery at clinic.
Fig. 5.
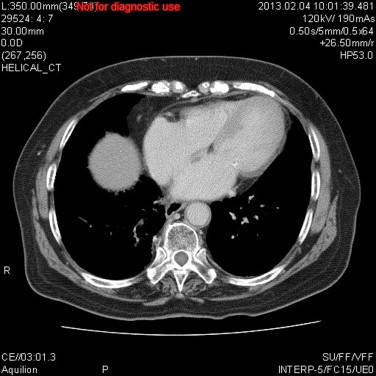
The CT scan demonstrates no recurrence of Morgagni hernia two years after surgery.
3. Discussion
Giovanni-Battista Morgagni first described this type of hernia in 1769.8 At present, Morgagni hernia is rare and account for only 1–5% of all congenial diaphragmatic hernias.9,10 It could be an incidental diagnosis in adulthood or could present with obstructive symptoms of the herniated viscera.11 Surgical treatment is required to relive current symptoms or to prevent possible future complications such as strangulation ileus or incarceration.10 Originally, direct closure of the hernia site or mesh placement was used as the surgical options by laparotomy or thoracotomy. Recently, the laparoscopic procedure has become available to treat this type of hernia and has bought a number of advantages such as reduced pain, shorter recovery time, and cosmetic benefits.5,6 In addition, recent trends in laparoscopic procedures have been toward minimizing the number of incisions to achieve less invasiveness. Examples of such approaches are single incision laparoscopic surgery (SILS) and reduced port surgery (RPS).12 Only one report previously described Morgagni hernia repair using single port access and closing the hernia site by non-absorbable suturing into extra-abdominal region.13 This report was very successful, however postoperative pain might be occurred because of suturing tension by lifting the interrupted sutures to close the hernia site. Some technical problems associated with SILS have been reported: restriction of the working field and interference of surgical instrument. The SILS technique does not rely on triangulation, which is one of the core principles of conventional laparoscopic surgery, allowing adequate operative exposure while maintaining an ergonomic position for the surgeon and assistant. Consequently, the inherent technical challenge that arises from the SILS technique is that of a compromised view and locomotive field. Therefore unfavorite outcomes such as longer operative time and possibly higher complication rate have been reported in early period of SILS operation.14 A small additional port or a reduced number of ports as with RPS are modifications that may overcome these problems. In combination with the SILS port and the additional port enable the performance of dual-port surgery, even for complex operation such as laparoscopic gastrectomy.15
We performed Morgagni hernia repair by mesh placement onto surrounding fascia using RPS. This type of repair is technically easy and should have a high probability of success because of the “tension free” condition. Also, less postoperative pain is also expected, compared to the external knot tying technique. Thoracoscopic approach is also other option for this type of hernia as a less invasive treatment, although the benefits over conventional laparoscopic approach have not been cleared.5 This may depend on surgeon's or institution's experiences.
Although the benefits of SILS or RPS over conventional laparoscopic surgery have not been established, either SILS or RPS could be the first choice for symptomatic Morgagni hernia repair because of the acceptable operation time, blood loss, and clinical outcome. Basically, cosmetic benefits and less operative pain are also expected as advantages of SILS or RPS originating from fewer incisions. In addition, tissue trauma and port-related complications such as organ damage, adhesions, bleeding, wound infections and hernias could be decreased. For the future direction, additional experience and continued investigations are warranted.
4. Conclusion
We reported a Morgagni hernia treated by RPS. This approach is safe and can be the good indication for this kind of hernia.
Conflict of interest
None.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Author contributions
Dr. Hiroyuki Kashiwagi is the corresponding author, and other doctors, Dr. Kenta Kumagai, Mutsumi Nozue and Yasushi Terada have cooperated in manuscript.
References
- 1.Das P.B., Neelaksh, Garg P.K., Oswall S.K., Dogra V.K. Morgagni hernia: an interesting congenital defect of the diaphragm. Indian J Chest Dis Allied Sci. 1978;20:204–207. [PubMed] [Google Scholar]
- 2.Sinclair L., Klein B.L. Congenital diaphragmatic hernia – Morgagni type. J Emerg Med. 1993;11:163–165. doi: 10.1016/0736-4679(93)90513-7. [DOI] [PubMed] [Google Scholar]
- 3.Wolloch Y., Grunebaum M., Glanz I., Dintsman M. Symptomatic retrosternal (Morgagni) hernia. Am J Surg. 1974;127:601–605. doi: 10.1016/0002-9610(74)90327-4. [DOI] [PubMed] [Google Scholar]
- 4.Kurkcuoglu I.C., Eroglu A., Karaoglanoglu N., Polat P., Balik A.A., Teknbas C. Diagnosis and surgical treatment of Morgagni hernia: report of three cases. Surg Today. 2003;33:525–528. doi: 10.1007/s10595-002-2522-z. [DOI] [PubMed] [Google Scholar]
- 5.Aydin Y., Altuntas B., Ulas A.B., Dahai C., Eroglu A. Morgagni hernia: transabdominal or transthoracic approach? Acta Chir Belg. 2014;114:131–135. [PubMed] [Google Scholar]
- 6.Godazandeh G., Mortazian M. Laparoscopic repair of Morgagni hernia using polyvinylidene fluoride (PVDF) mesh. Middle East J Dig Dis. 2012;4:232–235. [PMC free article] [PubMed] [Google Scholar]
- 7.Palanivelu C., Rangarajan M., Rajapandian S., Amar V., Parthasarathi R. Laparoscopic repair of adult diaphragmatic hernias and eventration with primary sutured closure and prosthetic reinforcement: a retrospective study. Surg Endosc. 2009;23:978–985. doi: 10.1007/s00464-008-0294-1. [DOI] [PubMed] [Google Scholar]
- 8.Komatsu T., Takahashi Y. Is this a mediastinal tumor? A case of Morgagni hernia complicated with intestinal incarceration mistaken for the mediastinal lipoma previously. Int J Surg Case Rep. 2013;4:302–304. doi: 10.1016/j.ijscr.2012.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aghajanzadeh M., Khadem S., Khajeh J.S., Gorabi H.E., Ebrahimi H., Maafi A.A. Clinical presentation and operative repair of Morgagni hernia. Interact Cardiovasc Thorac Surg. 2012;15:608–611. doi: 10.1093/icvts/ivs203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kesieme E.B., Kesieme C.N. Congenital diaphragmatic hernia: review of current concept in surgical management. ISRN Surg. 2011;2011:974041. doi: 10.5402/2011/974041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pousios D., Panagiotopoulos N., Piyis A., Gourgiotis S. Transthoracic repair of asymptomatic Morgagni hernia in an adult. Indian J Surg. 2012;74:431–433. doi: 10.1007/s12262-011-0304-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kashiwagi H., Kumagai K., Nozue M. Single incision laparoscopic surgery for a life-threatening, cyst of liver. Tokai J Exp Clin Med. 2011;36:13–16. [PubMed] [Google Scholar]
- 13.van Niekerk M.L. Laparoscopic Morgagni hernia repair using single-site umbilical and full-thickness abdominal wall repair: technical report of two cases. Afr J Paediatr Surg. 2013;10:55–57. doi: 10.4103/0189-6725.109401. [DOI] [PubMed] [Google Scholar]
- 14.Greaves N., Nicholson J. Single incision laparoscopic surgery in general surgery: a review. Ann R Coll Surg Engl. 2011;93:437–440. doi: 10.1308/003588411X590358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kashiwagi H., Kumagai K., Monma E., Nozue M. Dual-port distal gastrectomy for the early gastric cancer. Surg Endosc. 2014 doi: 10.1007/s00464-014-3827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


