Abstract
INTRODUCTION
Colon cancer in pregnant women is rare and tends to produce unspecific symptoms until advanced stage. Therefore common manifestations during pregnancy must be properly evaluated to avoid delayed diagnosis.
PRESENTATION OF CASE
A 31-year-old pregnant woman presented with nausea, vomiting and obstipation. An obtained magnetic resonance imaging (MRI) showed distended colon and the consecutive colonoscopy with biopsies confirmed the diagnosis of stenosing carcinoma of the descending colon. Left sided hemicolectomy was performed 10 days after initial presentation. Tumor histology confirmed the diagnosis of adenocarcinoma of the descendo-sigmoidal junction. Adjuvant chemotherapy with 5-fluorouracil was started in the 29th gestational week. The patient had an uneventful delivery of a healthy baby in her 39th gestational week.
DISCUSSION
Colorectal carcinoma during pregnancy is a rare event and its diagnosis is often delayed because symptoms are unspecific until the disease is advanced. Although constipation in pregnancy is a common symptom differential diagnosis of a mechanical stenosis should always be contemplated, especially when conservative treatment of constipation fails. MRI is the imaging tool of choice as abdominal computed tomography (CT) is contraindicated in pregnancy. Endoscopic confirmation should be obtained to gain pathological diagnosis of colorectal carcinoma. Surgery is the gold standard of treatment. In relation to the stage of the disease chemotherapy is of great importance.
CONCLUSION
Obstructing colorectal cancer can be a rare reason for the common problem of constipation in pregnancy. Beside clinical examination, MRI scan and colonoscopy will reveal the tumor in most cases and should be followed by surgical treatment and chemotherapy according to the stage of disease.
Keywords: Colon cancer, Pregnancy, Obstipation
1. Introduction
Colon cancer is the third most common cause of mortality from cancer in women.1 Colon cancer, however, is generally a disease of the elderly and occurs only rarely during pregnancy. The reported incidence in pregnant women is 0.002%.2 Its symptoms typically include nausea, vomiting, abdominal pain, and altered bowel movements, which commonly overlap with symptoms of normal pregnancy. Therefore, physicians and patients usually attribute them to the general manifestations of pregnancy without further workup or delay diagnostic tests because of potential fetal risks. A missed diagnosis of colorectal cancer is accordingly associated with development of advanced disease and poorer prognosis.3 Although the evaluation of colon cancer in the general population includes abdominal computed tomography (CT) to detect pericolonic extension and intraperitoneal metastases, CT is contraindicated during pregnancy, particularly the first trimester, because of radiation teratogenicity4 and colonoscopy is not yet an established procedure because of concerns about fetal risk.5 Treatment of colon cancer during pregnancy is also different from therapy for colon cancer in normal population. For example, adjuvant chemotherapy or adjuvant radiotherapy is beneficial to the mother but may be harmful to the fetus.
In this paper, we report the case of a pregnant woman that was diagnosed with adenocarcinoma of the descending colon at her 22nd gestational week.
2. Presentation of case
A 31-year-old gravida III para I patient presented at the emergency department in her 22nd gestational week with crampy left sided flank pain, which were first attributed to possible kidney stones. After outpatient treatment with acetaminophen and NSAIDs she was readmitted 2 days later with nausea, vomiting and obstipation. Physical examination revealed a gravid abdomen with left sided abdominal pain on palpation and normal bowel sounds, meeting the criteria of constipation, which is known to be common in pregnant women. Despite receiving conservative treatment for her constipation, her symptoms became worse. After 3 days of ineffective treatment of her obstipation a magnetic resonance imaging (MRI) scan of her abdomen was obtained. The scan showed distended small and large bowel with a sudden change of diameter between the distended descending colon and the collapsed sigmoid colon and rectum (Fig. 1). A subsequent colonoscopy revealed a stenosing carcinoma of the descending colon, which was confirmed by endoscopic biopsies. All laboratory values including carcinoembryonic antigen (CEA) level were within normal range.
Fig. 1.
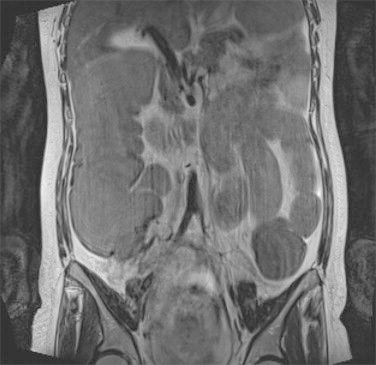
MRI of the abdomen showing distended small and large bowel.
After consultation with the obstetricians an open left sided hemicolectomy with end-to-side hand-sewn transversosigmoidostomy was performed 10 days after initial presentation. Intraoperatively dilated small and large bowel with a palpable tumor mass at the descendo-sigmoidal junction could be identified (Fig. 2). Directly behind the tumor mass the colon presented totally collapsed. Further abdominal exploration did not reveal any metastatic lesions. Tumor histology confirmed the diagnosis of adenocarcinoma of the descendo-sigmoidal junction with a diameter of 50 mm. Final pathological staging provided a pT3 pN2a Mx G2 V1 L1 Pn1 stage.
Fig. 2.
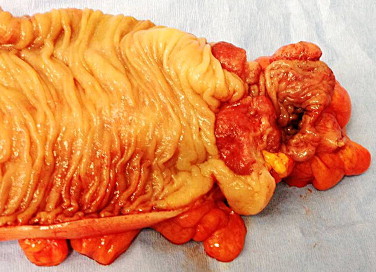
Resected colon with stenosing cancer.
The postoperative course was complicated. The patient developed an anastomotic insufficiency 4 days after hemicolectomy with acute peritonitis. Within the same day a re-laparotomy was carried out. Intraoperatively the anastomosis was found dehiscent involving half of the suture with consecutive fecal peritonitis. Unusually the sigmoid colon distal to the anastomosis was dilated due to entrapment of the distal sigmoid colon between the uterus and the pelvis. A Hartmann procedure was carried out, without intraoperative complications. Five days after Hartmann's procedure the patient was diagnosed with dehiscence of the abdominal wall, necessitating a third operation. The abdomen was reclosed and a VAC dressing was applied. Finally, the patient was discharged from the hospital 41 days after initial presentation. After discussion at the tumor board conference chemotherapy with 5-fluorouracil was started in the 29th gestational week. Despite the eventful and complicated postoperative course the obstetric surveillance of the baby did not show any abnormalities during in-patient treatment. The patient had an uneventful delivery of a healthy baby in her 39th gestational week.
3. Discussion
Colorectal carcinoma during pregnancy remains an interdisciplinary diagnostic and therapeutic challenge. It is a rare event6 and its symptoms (e.g. constipation, change in bowel habits, nausea and vomiting), which can occur due to physiological changes during pregnancy, can create difficulties to establish the diagnosis.7–10 However, there is a few epidemiological data for this rare condition. A study by the American Society of Colon and Rectal Surgeons investigating 41 cases revealed a mean age of 31 years11 when diagnosis was obtained. Majority of tumors were localized in the rectum (63%) and the sigmoid colon (20%), and Dukes stage at presentation was B or higher in all patients.11
Diagnosis of colorectal cancer during pregnancy is often delayed because symptoms are unspecific until the disease is advanced. In one reported case diagnosis was occasionally made during delivery by cesarean section.14 Although constipation in pregnancy is a common symptom differential diagnosis of a mechanical stenosis should always be contemplated, especially when conservative treatment of constipation fails. The mainstay of diagnostic evaluation in pregnant patients with colorectal cancer includes abdominal imaging and endoscopy. CEA can be used as a prognostic factor since elevated values prior to surgery are related to a higher rate of recurrence and disseminated disease.12 Magnetic resonance imaging (MRI) is the imaging tool of choice as abdominal computed tomography (CT) is contraindicated in pregnancy.4 Despite of relative contraindications in pregnant women, endoscopic confirmation should be obtained to gain pathological diagnosis of colorectal carcinoma.5
Surgery is the gold standard of treatment for colon cancer in pregnancy based on maternal cancer prognosis, gestational age and intraoperative findings. The tumor resection should not be delayed owing to significant tumor progression and worsening of the prognosis. In relation to the stage of the disease chemotherapy is of great importance. 5-FU has been shown to increase survival in colorectal cancer13 and to be safe in pregnant women.
4. Conclusion
In summary, obstructing colorectal cancer can be a rare reason for the common problem of constipation in pregnancy. If adequate treatment of constipation fails, further diagnostics is essential. Clinical examination, MRI scan and colonoscopy will reveal the tumor in most cases and should be followed by surgical treatment and chemotherapy according to the stage of disease. Early involvement of obstetric specialists is mandatory.
Conflict of interest
The authors declare that there is no conflict of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contributions
Marko Kraljevic carried out the writing of the manuscript. Henry Hoffmann supported Marko Kraljevic during the writing process and designed the final artwork. Alexandra Knipprath was the treating gynaecologist. Urs von Holzen was the treating surgeon and participated in design and coordination and helped to draft the manuscript.
Key learning points.
-
•
Colorectal carcinoma is a rare but fatal event during pregnancy.
-
•
Presentation can coincide with the signs and symptoms of pregnancy.
-
•
Diagnoses are often delayed.
-
•
Treatment is not different from those in the general population.
-
•
Special care regarding fetal safety should be considered.
References
- 1.Siegel R., Naishadham D., Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Girard R.M. Carcinoma of the colon associated with pregnancy: report of a case. Dis Colon Rectum. 1981;24(6):473–475. doi: 10.1007/BF02626787. [DOI] [PubMed] [Google Scholar]
- 3.Nesbitt J.C., Moise K.J., Sawyers J.L. Colorectal carcinoma in pregnancy. Arch Surg. 1985:636–640. doi: 10.1001/archsurg.1985.01390290110020. [DOI] [PubMed] [Google Scholar]
- 4.Brent R.L. The effects of embryonic and fetal exposure to X-ray, microwaves, and ultrasound. Clin Perinatol. 1986;13:615–648. [PubMed] [Google Scholar]
- 5.Cappell M.S. Gastrointestinal endoscopy in high-risk patients. Dig Dis. 1996;14:228–244. doi: 10.1159/000171555. [DOI] [PubMed] [Google Scholar]
- 6.Vitoratos N., Salamalekis E., Makrakis E., Creatsas G. Sigmoid colon cancer during pregnancy. Eur J Obstet Gynecol Reprod Biol. 2002;104:70–72. doi: 10.1016/s0301-2115(02)00052-0. [DOI] [PubMed] [Google Scholar]
- 7.Minter A., Malik R., Ledbetter L., Winokur T.S., Hawn M.T., Saif M.W. Colon cancer in pregnancy. Cancer Control. 2005;12(July(3)):196–202. doi: 10.1177/107327480501200310. [DOI] [PubMed] [Google Scholar]
- 8.Khodaverdi S., Valeshabad A.K., Khodaverdi M. A case of colorectal cancer during pregnancy: a brief review of the literature. Case Rep Obstet Gynecol. 2013;2013 doi: 10.1155/2013/626393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mechery J., Ikhena S.E., Hospital R.B., Hospital P. Cancer of the descending colon during pregnancy. J Obstet Gynaecol. 2002:311–312. doi: 10.1080/01443610701241159. [DOI] [PubMed] [Google Scholar]
- 10.Chan Y.M., Ngai S.W., Lao T.T. Colon cancer in pregnancy: a case report. J Reprod Med Obstet Gynecol. 1999;44:733–736. [PubMed] [Google Scholar]
- 11.Bernstein M., Madoff R., Cashaj P. Colon and rectal cancer in pregnancy. Dis Colon Rectum. 1993;36(2):172–178. doi: 10.1007/BF02051174. [DOI] [PubMed] [Google Scholar]
- 12.Fletcher R.H. Carcinoembryonic antigen. Ann Intern Med. 1986;104:66–73. doi: 10.7326/0003-4819-104-1-66. [DOI] [PubMed] [Google Scholar]
- 13.Grage T.B., Moss S.E. Adjuvant chemotherapy in cancer of the colon and rectum: demonstration of effectiveness of prolonged 5-FU chemotherapy in a prospectively controlled, randomized trial. Surg Clin North Am. 1981:1321–1329. doi: 10.1016/s0039-6109(16)42587-9. [DOI] [PubMed] [Google Scholar]
- 14.Colecchia G., Nardi M.G., Chir Colorectal cancer in pregnancy. A case report. 1999;20(4):159–161. [PubMed] [Google Scholar]


