Abstract
Recent studies have indicated that bipolar disorder is more common than previously believed. The socioeconomic and personal burdens of this illness are significant, and the lifetime risk of suicide attempts by patients with bipolar II disorder is high. It is not uncommon for patients with bipolar disorder, especially those presenting with depression, to be seen first in a primary care setting; therefore, primary care physicians need to be ready to diagnose and manage patients with these mental illnesses. The diagnosis of bipolar disorder or bipolar spectrum disorder is easily missed, or these illnesses may be misdiagnosed. A systematic and detailed initial history from the patient and a reliable family member is essential to making the correct diagnosis. The Mood Disorder Questionnaire, a validated screening instrument for bipolar disorder, may help primary care physicians make an appropriate diagnosis. Long-term management of patients with bipolar disorder should involve close liaison with a psychiatrist.
PRIMARY CARE AND BIPOLAR DISORDER
While bipolar disorder is a complex psychiatric illness and is often more appropriately treated by a psychiatrist, it is not uncommon for patients with mental illness to be seen in a primary care setting, presenting either with problems related to the mental illness or with concerns totally unrelated to the psychiatric disorder. Either way, the primary care physician may be required to diagnose and manage patients with mental illnesses. A 1997 study1 indicated that over 19.8% of patients who had scheduled primary care appointments fulfilled DSM-IV criteria for a psychiatric disorder; 8% of patients had any affective disorder, and approximately 1% had recognized bipolar disorder. It has also been demonstrated that about 50% of anxiety and depressive disorders are treated in a general medical setting.2
Recent evidence points to the fact that diagnoses of bipolar disorder, especially in patients with bipolar II disorder (who present more frequently with depressive episodes) or bipolar spectrum disorder, are frequently missed, both in psychiatric3,4 and primary care settings.5 The risk associated with missed diagnosis and misdiagnosis in these patients is great, and such patients, especially those presenting with depression, are frequently first seen and even treated in the primary care arena. It is, therefore, the responsibility of the primary care physician to recognize that bipolar disorder is more common than previously believed, that the burden associated with this disorder is significant, and that there is a need for improved diagnosis and recognition.
PREVALENCE OF BIPOLAR DISORDER
Historically, epidemiologic studies have indicated that prevalence rates for bipolar disorder are fairly low, with rates in the range of 1% to 2%.6,7 More recent evidence has pointed to a much higher prevalence of bipolar disorder than was previously believed, with leaders in the field of bipolar disorder suggesting prevalence rates approximating 5% to 7%.8–10 This higher prevalence estimation is probably due to a combination of increased recognition of the illness and acceptance of a broader definition of bipolar disorder, on the basis of 2 major advances over the last few years. A DSM-IV diagnosis of bipolar II disorder requires the presence of 1 episode of depression and 1 episode of hypomania. For a diagnosis of hypomania to be made, DSM-IV-TR (text revision)11 now requires a duration of 4 days for hypomanic symptoms. Experts argue that episodes of shorter duration should be recognized in the criteria in order to prevent clinicians from ignoring shorter hypomanic episodes and thus misdiagnosing patients as having major depressive disorder.10,11 The second advance has been the recognition of a “softer” spectrum of bipolar disorders,8,12,13 or bipolar spectrum disorder. The concept of this disorder is evolving but is currently viewed as a longitudinal diagnosis consisting of mood swings that may include mania, hypomania, mixed states (which meet criteria for both a manic and a depressive episode), hyper-thymic temperament (which describes a group of people who show cheerfulness and exuberance, meddlesomeness, lack of inhibitions, overconfidence, grandiosity, and high energy levels, in the absence of a formal thought disorder), major depressive disorder, and mixed depressive states (depression with 1 or 2 manic features).14
Recent epidemiologic data have confirmed suspicions among bipolar experts that bipolar disorder occurs more commonly than previously believed. The Mood Disorder Questionnaire (MDQ),15 a validated screening instrument for bipolar disorders, was sent to a sample of approximately 130,000 people selected as representative of the U.S. adult population on the basis of demographic variables.16 Prevalence of bipolar I and II disorders in the general U.S. population was 3.4%; the rate rose to 3.7% when adjusted for the nonresponse bias.16 In addition, a recent secondary analysis of the U.S. National Epidemiologic Catchment Area (ECA) database17 that reclassified respondents on the basis of the presence of at least 2 episodes of subthreshold symptoms of hypomania or mania of 1-week duration (features of bipolar spectrum disorder) found the prevalence rate for bipolar disorder to be 6.4%. Prevalence of subthreshold symptoms was 5.1%. The subthreshold group did not differ demographically from those with threshold manic or hypomanic symptoms. Compared with subjects from the no-mental-disorder comparison group, the subthreshold group had a 4 times higher suicide attempt rate, with a lifetime prevalence of 8%, significantly higher utilization of health care services, and a greater need for public assistance.
These findings would suggest that such patients should be treated if they are identified in the community setting; however, guidelines for diagnosis may need to be revisited before this becomes common practice. In this re-analysis of ECA data,17 patients who had symptoms in the manic spectrum were more likely to be younger and have greater marital disruption than were patients in the other groups. The authors argue that although subjects with bipolar spectrum disorder do not fulfill existing criteria for a bipolar disorder diagnosis, they do fulfill criteria for “caseness” on the basis of their functional impairment. At present, no data exist that indicate whether and how many patients with such subthreshold symptoms progress to a diagnosis of bipolar I or II disorder.
BIPOLAR BURDEN
The socioeconomic and individual/family burdens related to bipolar disorder are significant. Studies to date have focused predominantly on bipolar disorder, rather than bipolar spectrum disorders, so it is conceivable that the true impact of the full spectrum of bipolar disorders remains unrecognized. In addition, there is no way of determining consequences related to unrecognized cases of bipolar disorder.
Socioeconomic Burden
The economic burden of bipolar disorder in the United States is substantial. Lifetime cost of bipolar disorder calculated in 1991 and 1998 was $45 billion18 and $24 billion,19 respectively; costs in the latter study were lower because indirect costs were not addressed. The 1998 study indicated that average direct medical care costs per patient ranged from $11,720 for patients with a single manic episode to $624,785 for patients with nonresponsive or chronic episodes.19 Indirect costs in the 1991 study amounted to $38 billion and included lost productivity of wage earners, homemakers, and caregivers; institutionalization; and loss due to suicide.18
Personal Burden
The World Health Organization listed bipolar disorder as sixth on a list of 10 disorders that caused disability-adjusted life-years (DALYs) for males and females in developed countries.20 DALYs are a measure of the burden of disease and reflect the total amount of healthy life lost from premature mortality or from disability.
Findings from 3 epidemiologic surveys have indicated that bipolar disorder is associated with substantial and long-lasting functional consequences.21–23 Results from all 3 surveys have been remarkably similar. The most recent was a survey conducted among 600 bipolar support group participants of the National Depressive and Manic Depressive Association (DMDA).21 Despite high levels of education (90% of respondents had attended some college), 57% were unemployed and greater than 50% reported household incomes of less than $15,000 per year. Sixty-five percent of respondents reported difficulty maintaining long-term intimate relationships; 34% were separated or divorced. The report21 compared findings with an earlier, similar survey24 and determined that very little had changed over the 8 years that had elapsed between surveys. Another recent survey25 that evaluated the impact of bipolar disorder involved a sample of 3059 subjects taken from the larger sample of subjects in the Hirschfield et al. study.16 Respondents who screened positive on the MDQ for bipolar disorder reported significantly higher levels of impairment in terms of work/school, social/leisure life, and family life on the Sheehan Disability Scale and the Social Adjustment Scale (p < .0001 for both scales). Significantly more (p < .0001) MDQ-positive respondents than MDQ-negative respondents reported being fired or laid off (54% vs. 29%) or being jailed, arrested, or convicted of a crime aside from drunk driving (26% vs. 5%).25
Suicide
A review of 15 studies determined that 25% to 50% of people with bipolar disorder attempt suicide at least once; completed suicide was more common among women.26 Although bipolar II disorder has traditionally been viewed as resulting in less functional impairment than bipolar I disorder, the lifetime risk of suicide attempts was highest in patients with bipolar II disorder, lower in patients with bipolar I disorder, and lowest in patients with major depressive disorder in another review.27 Bipolar II patients were also overrepresented among suicide completers.
Another survey of 258 patients admitted from 1996 to 1999 to the Stanley Foundation Bipolar Network—an international, multisite network investigating the characteristics and course of bipolar disorder—found that 28.3% of their bipolar I cohort and 25.5% of their bipolar II cohort had a history of 1 or more suicide attempts.28
Although these data are contradictory, the Stanley Foundation survey demonstrated that patients with bipolar II disorder had a risk of suicide almost equal to their bipolar I counterparts, suggesting again that the longer-term risks associated with bipolar II disorder should not be underappreciated and that risk is high in both groups. Most suicides appear to occur in the depressed phase of the illness29,30 and also commonly in association with comorbid substance abuse.31,32
SUBSTANCE ABUSE
The ECA study6 reported that comorbid substance abuse occurred more frequently with bipolar disorder than with any other Axis I psychiatric disorder. Individuals with bipolar disorder abused or were dependent on drugs in 56% of cases and abused alcohol in 44% of cases. Post et al.28 more recently conducted a survey indicating that 41.8% of individuals with bipolar I disorder and 25.5% of individuals with bipolar II disorder abused drugs or alcohol.
Bipolar disorder with comorbid substance abuse is associated with higher rates of refractoriness to lithium treatment33,34 and higher risks of not only suicide attempts but also completed suicides.31
LONGER-TERM CONSEQUENCES OF BIPOLAR DISORDER
The Stanley Foundation Bipolar Network found that, in spite of treatment with a range of both novel and routinely used agents, two thirds of their group had clinically substantial depressive or manic symptoms over a year of follow-up.28 Sixty-three percent of patients experienced 4 or more episodes per year; 31% had more than 8 episodes per year. Of the 33% of patients who were relatively well for most of the year, only 11% were virtually illness free.
Studies have indicated that most patients with bipolar disorder continue to show functional impairment, even patients who achieve euthymia.35–38 Tohen et al.35 assessed 219 patients hospitalized for an initial manic episode for functional recovery at regular intervals. Patients were assessed for syndromal recovery (i.e., no longer meeting DSM-IV criteria for mania) versus functional recovery (i.e., return to baseline vocational and residential status). At 6 months, 84% of patients achieved syndromal recovery, but only 30% achieved functional recovery. At 24 months, 98% of patients attained syndromal recovery, but only 38% attained functional recovery. Overall, only 37% of those patients showing syndromal recovery at 24 months achieved functional recovery. MacQueen et al.,36 in an aggregate review of studies examining psychosocial outcome in bipolar disorder, found that 30% to 60% of individuals with bipolar disorder failed to regain full functioning occupationally and socially. There is also some evidence that patients with bipolar II disorder, compared with bipolar I disorder patients, experienced more illness disability in terms of health, recreation, finances, and sub-syndromal depression.39
MISSED DIAGNOSIS AND MISDIAGNOSIS
There is convincing evidence that bipolar disorder is frequently either completely overlooked or misdiagnosed as major depressive disorder. The DMDA survey conducted in 200021 indicated that 69% of respondents with bipolar disorder were misdiagnosed. Those who were misdiagnosed received a mean of 3.5 alternative diagnoses and saw a mean of 4 physicians before they received an accurate diagnosis. Most respondents who reported being misdiagnosed believed that the greatest barrier to appropriate diagnosis was lack of understanding about bipolar disorder among health care professionals consulted. The most common incorrect diagnosis received was that of major depressive disorder (60% of cases); other diagnoses included anxiety disorder (26%), schizophrenia (18%), and borderline or antisocial personality disorder (17%). Forty-eight percent of respondents reported a lapse of several months to 5 years between seeking the first treatment and receiving an appropriate diagnosis; more than a third of patients reported a lapse of 10 years or more. The extensive gap between treatment-seeking and appropriate diagnosis represents no significant change from the findings in the 1994 survey,24 indicating that there has been little improvement in bipolar disorder recognition and diagnosis over the last decade. The 130,000-person population survey16 indicated that of those patients who screened positive for bipolar disorder, only 20% had received a diagnosis from a physician; 31% said that they were diagnosed with major depressive disorder, and almost 50% said that they had been diagnosed with neither depression nor bipolar disorder.
Bipolar patients frequently present initially with depressive episodes.40 As many as 35% to 60% of patients experience a major depressive episode before experiencing a manic episode.3 In addition, patients tend to underreport their experience of hypomanic episodes,14,41 hence the tendency for misdiagnosis as depression. Ghaemi et al.3,4 determined in 2 separate studies that approximately 40% of those initially diagnosed with major depressive disorder were converted to a diagnosis of bipolar disorder; patients were misdiagnosed even after having experienced an episode of mania or hypomania.
CONSEQUENCES OF MISDIAGNOSIS
In most cases, antidepressants have been associated with risk for adverse outcomes in patients with bipolar disorder; a misdiagnosis of depression and treatment with antidepressants place approximately 30% to 40% of bipolar patients at risk for induction of manic episodes.42–44 Patients with bipolar disorder who take antidepressants also have been thought to have an increased risk of promotion of rapid cycling,4,42,45 which is defined in DSM-IV as at least 4 episodes of affective illness in 1 year, with individual episodes demarcated by 2 months of full or partial remission or a switch to the opposite pole, and which is associated with greater treatment resistance and poorer outcomes. A recent study, however, did not implicate tricyclic antidepressants or, by inference, selective serotonin reup-take inhibitors in the promotion of affective instability.46 This naturalistic study followed 89 patients for 1 or more years, and resolution of rapid cycling was not associated with a reduction in tricyclic antidepressant use. More research is required in this area to clarify relative risks and benefits of antidepressant use. Current guidelines recommend prescribing antidepressants together with a mood stabilizer in patients with bipolar disorder.47 Misdiagnosis and inappropriate treatment of patients with bipolar disorder also delay management with mood stabilizers41 and may increase the risk of lithium resistance, which occurs as more episodes are experienced.48 There is also some evidence that appropriate treatment of bipolar disorders can reduce suicide risk49 and that earlier recognition and treatment of bipolar disorders in children and adolescents reduce subsequent risk of substance abuse.50
IMPROVING DIAGNOSTIC ACCURACY
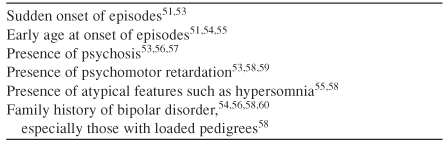
It is only through increased awareness of bipolar disorder that clinicians will begin to consider the diagnosis of bipolar disorder. The key to diagnosis lies in taking a systematic and detailed initial history from the patient,51 which may be particularly difficult given the time constraints of a busy office environment.52 Because patients frequently present with depressive episodes and may not report hypomanic episodes, the clinician should ask specifically about previous and existing symptoms of mania and hypomania, especially the occurrence of hypomania after depressive episodes.41 Patient information alone is of limited value, and taking collateral histories from close family or friends can aid substantially in making the diagnosis.41 In addition, there are a number of presenting features that differentiate bipolar disorder from major depressive disorder, and these features should be specifically addressed during the assessment (Table 1). Presence of these distinguishing features may not aid in discriminating between bipolar I and bipolar II disorder but will raise suspicion of the possibility of a bipolar diagnosis and the need for referral to a psychiatrist for appropriate assessment. Unfortunately, to date little work has been done to aid with diagnosis of bipolar spectrum disorders, and more research is needed in this area.
Table 1.
Features That Distinguish Bipolar Disorder From Unipolar Depression
The MDQ,15 a patient-rated screening tool much like the Beck Depression Inventory,61 may also help to facilitate an appropriate diagnosis of bipolar disorder. The MDQ is not designed to aid in making the distinction among bipolar I, II, or spectrum disorders but merely to raise the possibility of a bipolar diagnosis. A screening score of 7 out of 13 or more items answered affirmatively on the MDQ yields good sensitivity (0.73) and better specificity (0.90).15 Patients with scores above 7 should be thoroughly questioned regarding bipolar features and referred in cases where doubt exists.
MANAGING BIPOLAR DISORDER
Pharmacotherapeutic management of bipolar disorder is extremely complex, fraught with frequent nonresponse and resistance to treatment and side effects. Management requires trial-and-error use of medications, treatment of any comorbidities, polypharmacy, and regular blood level and organ system function monitoring. In addition, non-pharmacologic therapies such as cognitive-behavioral therapy,62,63 psychoeducation,64,65 and family therapy65,66 may be helpful in these patients. For these reasons, bipolar disorder is best managed in a psychiatric setting, and referral of patients with bipolar disorder, as well as those suspected of having bipolar disorder, is the best course of action. Obviously, patients who present an acute risk for suicide should be acutely referred and managed, and the presence of factors that represent increased risk for impulsivity and suicide, such as comorbid alcohol and substance abuse, should also precipitate an acute referral.
Primary care physicians are often the first contacts for both the patient and the family and may be called upon to provide support to family members. An excellent resource for family and patient support and education is the Depression and Bipolar Support Alliance (formerly the DMDA). The organization's Web site (http://www.dbsalliance.org) can be used to locate support groups near the patient's home.
In addition, longer-term care of the patient with bipolar disorder may fall within the remit of the primary care physician, as patients present with complaints both related and unrelated to their mental illness. A strong relationship of consultation-liaison between the primary care physician and the psychiatrist is recommended. Medical comorbidities are common, and conditions such as migraine15,67,68 or obesity and its associated consequences,69,70 such as type II diabetes,71,72 may be frequently seen. Office visits should include assessment for emergence of these comorbidities, as well as the numerous side effects that can be encountered with the use of commonly used mood stabilizers, such as hypothyroidism73 and more rarely renal failure73 associated with lithium use and polycystic ovary syndrome74 associated with valproate use in epileptic women.
Psychiatric comorbidities are also common in these patients, and office visits should include a brief screening history for emergence of evidence of disorders such as obsessive-compulsive disorder,75 anxiety disorders, post-traumatic stress disorder, social phobia,7 panic disorder,76 and personality disorders.77 As abuse of alcohol and other substances is so common in bipolar populations,75,78 the primary care physician should always remain vigilant for these comorbidities in patients with bipolar disorder. Assessment of suicide risk, which is highly prevalent in both bipolar I and II populations, should be evaluated at each office visit.
Stable patients with bipolar disorder taking lithium or valproate may require regular serum level and renal, hepatic, hematologic, and thyroid function monitoring. The American Psychiatric Association's revised guidelines for management of bipolar disorder47 recommend checking renal and thyroid function every 6 months in stable patients taking lithium and conducting tests of hematologic and hepatic function every 6 months in patients taking valproate. Therapeutic levels of lithium range from 0.5 to 1.2 mEq/L, and those of valproate range between 50 and 125 g/mL.47 Lithium levels should be monitored every 2 months,79 and valproate levels, every 3 months in stable patients.
As for any other medical condition, caution should always be taken in considering drug-drug interactions and synergistic, or additive, negative effects of drugs in patients with bipolar disorder.
Other management considerations for patients with bipolar disorder are beyond the scope of this article; however, for more information, the reader is referred to Glick et al.80
FUTURE DIRECTIONS
There is evidence that prevalence rates for bipolar disorder are much higher than previously reported and that bipolar disorder is commonly seen in the primary care setting. The socioeconomic, personal, and family burdens associated with bipolar disorder are substantial, but it is not clear from existing research whether the true impact of bipolar disorder is understood, given that it is so frequently unrecognized. Patients with bipolar spectrum and bipolar II disorders often present with depressive episodes that facilitate misdiagnosis of major depressive disorder and treatment with antidepressants, possibly worsening outcomes for these patients. While it is likely that patients with bipolar disorder are best managed in a psychiatry environment, it is frequently the responsibility of the primary care physician to identify the possibility of a diagnosis of bipolar disorder. Therefore, there is a need for the primary care clinician to be aware of the possible indicators of bipolar disorder in these patients and to make the appropriate management decisions, among them referral. The MDQ may be a useful screening tool to help in this endeavor. As long-term management of bipolar disorder is complex, a strong consultation-liaison relationship between the primary care physician and the psychiatrist is recommended.
Drug name: lithium (Eskalith, Lithobid, and others).
Footnotes
Supported by an unrestricted educational grant from GlaxoSmithKline.
Dr. Glick has been a consultant for, received grant/research support and honoraria from, and served on the speakers or advisory boards of Pfizer, Eli Lilly, Bristol-Myers, Janssen, and AstraZeneca.
REFERENCES
- Olfson M, Fireman B, and Weissman MM. et al. Mental disorders and disability among patients in a primary care group practice. Am J Psychiatry. 1997 154:1734–1740. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, and Rae DS. et al. The de facto US mental and addictive disorders service system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993 50:85–94. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Sachs GS, and Chiou AM. et al. Is bipolar disorder still underdiagnosed? are antidepressants overutilized? J Affect Disord. 1999 52:135–144. [DOI] [PubMed] [Google Scholar]
- Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study [CME] J Clin Psychiatry. 2000;61:804–808. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- Manning JS, Haykal RF, and Connor PD. et al. On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally. Compr Psychiatry. 1997 38:102–108. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, and Rae DS. et al. Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990 264:2511–2518. [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, and Zhao S. et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994 51:8–19. [DOI] [PubMed] [Google Scholar]
- Akiskal HS. The prevalent clinical spectrum of bipolar disorders: beyond DSM-IV. J Clin Psychopharmacol. 1996;16(2 suppl 1):4S–14S. doi: 10.1097/00004714-199604001-00002. [DOI] [PubMed] [Google Scholar]
- Akiskal HS, Bourgeois ML, and Angst J. et al. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J Affect Disord. 2000 59suppl 1. S5–S30. [DOI] [PubMed] [Google Scholar]
- Angst J. The emerging epidemiology of hypomania and bipolar II disorder. J Affect Disord. 1998;50:143–151. doi: 10.1016/s0165-0327(98)00142-6. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders-Text Revision, Fourth Edition. Washington, DC: American Psychiatric Association. 2000 [Google Scholar]
- Dunner DL, Gershon ES, Goodwin FK. Heritable factors in the severity of affective illness. Sci Pro Amer Psychiatric Assn. 1970;123:187–188. [PubMed] [Google Scholar]
- Klerman GL. The spectrum of mania. Compr Psychiatry. 1981;22:11–20. doi: 10.1016/0010-440x(81)90049-3. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM. Bipolar spectrum disorder: improving its recognition and diagnosis. J Clin Psychiatry. 2001 62suppl 14. 5–9. [PubMed] [Google Scholar]
- Hirschfeld RM, Williams JB, and Spitzer RL. et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000 157:1873–1875. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Calabrese JR, and Weissman MM. et al. Screening for bipolar disorder in the community. J Clin Psychiatry. 2003 64:53–59. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS. The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. J Affect Disord. 2003;73:123–131. doi: 10.1016/s0165-0327(02)00332-4. [DOI] [PubMed] [Google Scholar]
- Wyatt RJ, Henter I. An economic evaluation of manic-depressive illness: 1991. Soc Psychiatry Psychiatr Epidemiol. 1995;30:213–219. doi: 10.1007/BF00789056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begley CE, Annegers JF, and Swann AC. et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics. 2001 19:483–495. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64:161–174. [PubMed] [Google Scholar]
- Suppes T, Leverich GS, and Keck PE. et al. The Stanley Foundation Bipolar Treatment Outcome Network, 2: demographics and illness characteristics of the first 261 patients. J Affect Disord. 2001 67:45–59. [DOI] [PubMed] [Google Scholar]
- Kupfer DJ, Frank E, and Grochocinski VJ. et al. Demographic and clinical characteristics of individuals in a bipolar disorder case registry [CME]. J Clin Psychiatry. 2002 63:120–125. [DOI] [PubMed] [Google Scholar]
- Lish JD, Dime-Meenan S, and Whybrow PC. et al. The National Depressive and Manic-Depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994 31:281–294. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Hirschfeld RM, and Reed M. et al. Impact of bipolar disorder on a US community sample. J Clin Psychiatry. 2003 64:425–432. [DOI] [PubMed] [Google Scholar]
- Tondo L, Baldessarini RJ, Hennen J. Lithium and suicide risk in bipolar disorder. Prim Psychiatry. 1999;6:51–56. [Google Scholar]
- Rihmer Z, Pestality P. Bipolar II disorder and suicidal behavior. Psychiatr Clin North Am. 1999;22:667–673. doi: 10.1016/s0193-953x(05)70101-5. [DOI] [PubMed] [Google Scholar]
- Post RM, Denicoff KD, and Leverich GS. et al. Morbidity in 258 bipolar outpatients followed for 1 year with daily prospective ratings on the NIMH life chart method [CME]. J Clin Psychiatry. 2003 64:680–690. [DOI] [PubMed] [Google Scholar]
- Sachs GS, Yan LJ, and Swann AC. et al. Integration of suicide prevention into outpatient management of bipolar disorder. J Clin Psychiatry. 2001 62suppl 25. 3–11. [PubMed] [Google Scholar]
- Oquendo MA, Waternaux C, and Brodsky B. et al. Suicidal behavior in bipolar mood disorder: clinical characteristics of attempters and nonattempters. J Affect Disord. 2000 59:107–117. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Singer TM, and Garno JL. Suicidality and substance abuse in affective disorders. J Clin Psychiatry. 2001 62suppl 25. 35–43. [PubMed] [Google Scholar]
- Leverich GS, Altshuler LL, and Frye MA. et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network [CME]. J Clin Psychiatry. 2003 64:506–515. [DOI] [PubMed] [Google Scholar]
- Frye MA, Altshuler LL. Selection of initial treatment for bipolar disorder, manic phase. Mod Probl Pharmacopsychiatry. 1997;25:88–113. doi: 10.1159/000061663. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Garno JL, and Leon AC. et al. A history of substance abuse complicates remission from acute mania in bipolar disorder. J Clin Psychiatry. 1999 60:733–740. [DOI] [PubMed] [Google Scholar]
- Tohen M, Hennen J, and Zarate CM Jr. et al. Two-year syndromal and functional recovery in 219 cases of first-episode major affective disorder with psychotic features. Am J Psychiatry. 2000 157:220–228. [DOI] [PubMed] [Google Scholar]
- MacQueen GM, Young LT, and Robb JC. et al. Effect of number of episodes on wellbeing and functioning of patients with bipolar disorder. Acta Psychiatr Scand. 2000 101:374–381. [DOI] [PubMed] [Google Scholar]
- Cooke RG, Robb JC, and Young LT. et al. Well-being and functioning in patients with bipolar disorder assessed using the MOS 20-Item short form (SF-20). J Affect Disord. 1996 39:93–97. [DOI] [PubMed] [Google Scholar]
- Gitlin MJ, Swendsen J, and Heller TL. et al. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995 152:1635–1640. [DOI] [PubMed] [Google Scholar]
- Robb JC, Cooke RG, and Devins GM. et al. Quality of life and lifestyle disruption in euthymic bipolar disorder. J Psychiatr Res. 1997 31:509–517. [DOI] [PubMed] [Google Scholar]
- Perugi G, Micheli C, and Akiskal HS. et al. Polarity of the first episode, clinical characteristics, and course of manic depressive illness: a systematic retrospective investigation of 320 bipolar I patients. Compr Psychiatry. 2000 41:13–18. [DOI] [PubMed] [Google Scholar]
- Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52:51–55. doi: 10.1176/appi.ps.52.1.51. [DOI] [PubMed] [Google Scholar]
- Altshuler LL, Post RM, and Leverich GS. et al. Antidepressant-induced mania and cycle acceleration: a controversy revisited. Am J Psychiatry. 1995 152:1130–1138. [DOI] [PubMed] [Google Scholar]
- Henry C, Sorbara F, and Lacoste J. et al. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001 62:249–255. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Whiteside JE. The association between substance abuse and antidepressant-induced mania in bipolar disorder: a preliminary study [CME] J Clin Psychiatry. 2002;63:791–795. doi: 10.4088/jcp.v63n0907. [DOI] [PubMed] [Google Scholar]
- Wehr TA, Goodwin FK. Do antidepressants cause mania? Psychopharmacol Bull. 1987;23:61–65. [PubMed] [Google Scholar]
- Coryell W, Solomon D, and Turvey C. et al. The long-term course of rapid-cycling bipolar disorder. Arch Gen Psychiatry. 2003 60:914–920. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RMA, Bowden CL, and Perlis RH. et al. Practice Guideline for the Treatment of Patients With Bipolar Disorder [Revision]. Am J Psychiatry. 2002 159:1–50. [PubMed] [Google Scholar]
- Swann AC, Bowden CL, and Calabrese JR. et al. Differential effect of number of previous episodes of affective disorder on response to lithium or divalproex in acute mania. Am J Psychiatry. 1999 156:1264–1266. [DOI] [PubMed] [Google Scholar]
- Tondo L, Baldessarini RJ. Reduced suicide risk during lithium maintenance treatment. J Clin Psychiatry. 2000 61suppl 9. 97–104. [PubMed] [Google Scholar]
- Geller B, Cooper TB, and Sun K. et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry. 1998 37:171–178. [DOI] [PubMed] [Google Scholar]
- Coryell W, Endicott J, and Maser JD. et al. Long-term stability of polarity distinctions in the affective disorders. Am J Psychiatry. 1995 152:385–390. [DOI] [PubMed] [Google Scholar]
- Kassirer JP. Doctor discontent. N Engl J Med. 1998;339:1543–1545. doi: 10.1056/NEJM199811193392109. [DOI] [PubMed] [Google Scholar]
- Strober M, Carlson G. Bipolar illness in adolescents with major depression: clinical, genetic, and psychopharmacologic predictors in a three- to four-year prospective follow-up investigation. Arch Gen Psychiatry. 1982;39:549–555. doi: 10.1001/archpsyc.1982.04290050029007. [DOI] [PubMed] [Google Scholar]
- Winokur G, Coryell W, and Endicott J. et al. Further distinctions between manic-depressive illness (bipolar disorder) and primary depressive disorder (unipolar depression). Am J Psychiatry. 1993 150:1176–1181. [DOI] [PubMed] [Google Scholar]
- Benazzi F. Sensitivity and specificity of clinical markers for the diagnosis of bipolar II disorder. Compr Psychiatry. 2001;42:461–465. doi: 10.1053/comp.2001.27901. [DOI] [PubMed] [Google Scholar]
- Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158:1265–1270. doi: 10.1176/appi.ajp.158.8.1265. [DOI] [PubMed] [Google Scholar]
- Mitchell PB, Wilhelm K, and Parker G. et al. The clinical features of bipolar depression: a comparison with matched major depressive disorder patients. J Clin Psychiatry. 2001 62:212–216. [PubMed] [Google Scholar]
- Akiskal HS, Walker P, and Puzantian VR. et al. Bipolar outcome in the course of depressive illness: phenomenologic, familial, and pharmacologic predictors. J Affect Disord. 1983 5:115–128. [DOI] [PubMed] [Google Scholar]
- Kuhs H, Reschke D. Psychomotor activity in unipolar and bipolar depressive patients. Psychopathology. 1992;25:109–116. doi: 10.1159/000284760. [DOI] [PubMed] [Google Scholar]
- Simpson SG, Folstein SE, and Meyers DA. et al. Bipolar II: the most common bipolar phenotype? Am J Psychiatry. 1993 150:901–903. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, and Mendelson M. et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961 4:561–571. [DOI] [PubMed] [Google Scholar]
- Lam DH, Watkins ER, and Hayward P. et al. A randomized controlled study of cognitive therapy for relapse prevention for bipolar affective disorder: outcome of the first year. Arch Gen Psychiatry. 2003 60:145–152. [DOI] [PubMed] [Google Scholar]
- Otto MW, Reilly-Harrington NA. Cognitive-behavioural therapy for the management of bipolar disorder. In: Hofmann SG, Tompson MC, eds. Treating Chronic and Severe Mental Disorders: A Handbook of Empirically Supported Interventions. 1st ed. New York, NY: The Guilford Press. 2002 [DOI] [PubMed] [Google Scholar]
- Colom F, Vieta E, and Martinez-Aran A. et al. A randomized trial on the efficacy of group psychoeducation in the prophylaxis of recurrences in bipolar patients whose disease is in remission. Arch Gen Psychiatry. 2003 60:402–407. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Simoneau TL, and George EL. et al. Family-focused treatment of bipolar disorder: 1-year effects of a psychoeducational program in conjunction with pharmacotherapy. Biol Psychiatry. 2000 48:582–592. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Goldstein MJ, and Nuechterlein KH. et al. Family factors and the course of bipolar affective disorder. Arch Gen Psychiatry. 1988 45:225–231. [DOI] [PubMed] [Google Scholar]
- Fasmer OB. The prevalence of migraine in patients with bipolar and unipolar affective disorders. Cephalalgia. 2001;21:894–899. doi: 10.1046/j.1468-2982.2001.00279.x. [DOI] [PubMed] [Google Scholar]
- Fasmer OB, Oedegaard KJ. Clinical characteristics of patients with major affective disorders and comorbid migraine. World J Biol Psychiatry. 2001;2:149–155. doi: 10.3109/15622970109026801. [DOI] [PubMed] [Google Scholar]
- McElroy SL, Frye MA, and Suppes T. et al. Correlates of overweight and obesity in 644 patients with bipolar disorder. J Clin Psychiatry. 2002 63:207–213. [DOI] [PubMed] [Google Scholar]
- Fagiolini A, Frank E, and Houck PR. et al. Prevalence of obesity and weight change during treatment in patients with bipolar I disorder. J Clin Psychiatry. 2002 63:528–533. [DOI] [PubMed] [Google Scholar]
- Cassidy F, Ahearn E, Carroll BJ. Elevated frequency of diabetes mellitus in hospitalized manic-depressive patients. Am J Psychiatry. 1999;156:1417–1420. doi: 10.1176/ajp.156.9.1417. [DOI] [PubMed] [Google Scholar]
- Lilliker SL. Prevalence of diabetes in a manic-depressive population. Compr Psychiatry. 1980;21:270–275. doi: 10.1016/0010-440x(80)90030-9. [DOI] [PubMed] [Google Scholar]
- Markowitz GS, Radhakrishnan J, and Kambham N. et al. Lithium nephrotoxicity: a progressive combined glomerular and tubulointerstitial nephropathy. J Am Soc Nephrol. 2000 11:1439–1448. [DOI] [PubMed] [Google Scholar]
- Isojarvi JI, Laatikainen TJ, and Pakarinen AJ. et al. Polycystic ovaries and hyperandrogenism in women taking valproate for epilepsy. N Engl J Med. 1993 329:1383–1388. [DOI] [PubMed] [Google Scholar]
- US Dept Health and Human Services and National Institute of Mental Health. Epidemiologic Catchment Area (ECA) Survey of Mental Disorders, Wave I (household), 1980–1985: [United States]. Ann Arbor, Mich: Inter-university Consortium for Political and Social Research. 1991 [Google Scholar]
- Chen YW, Dilsaver SC. Comorbidity of panic disorder in bipolar illness: evidence from the Epidemiologic Catchment Area Survey. Am J Psychiatry. 1995;152:280–282. doi: 10.1176/ajp.152.2.280. [DOI] [PubMed] [Google Scholar]
- Vieta E, Colom F, and Corbella B. et al. Clinical correlates of psychiatric comorbidity in bipolar I patients. Bipolar Disord. 2001 3:253–258. [PubMed] [Google Scholar]
- Cassidy F, Ahearn EP, Carroll BJ. Substance abuse in bipolar disorder. Bipolar Disord. 2001;3:181–188. [PubMed] [Google Scholar]
- Eskalith (lithium carbonate). Physicians' Desk Reference. Montvale, NJ: Medical Economics, Inc. 2003 1515–1516. [Google Scholar]
- Glick ID, Suppes T, and DeBattista C. et al. Psychopharmacologic treatment strategies for depression, bipolar disorder, and schizophrenia. Ann Intern Med. 2001 134:47–60. [DOI] [PubMed] [Google Scholar]


