Abstract
Male Breast Cancer (MBC) is a rare disease in the U.S., accounting for less than 1% of all breast cancers. Rates of MBC in Africa are more variable than in the U.S., therefore, understanding the risk factors involved in a population like Egypt can clarify the nature of MBC. The polyglutamine tract (QT) is a variable region of the androgen receptor (AR), a nuclear receptor which is important in modulating androgen actions and generally inhibits growth in breast tissue. It is hypothesized that a long QT results in weaker AR activity over the lifetime, resulting in less AR mediated control over cellular division and higher risk of MBC. As a corollary, we expect to see a distribution skewed toward longer QTs in MBC patients compared to controls and overall relatively longer QT’s in populations with higher rates of MBC. This study aimed to investigate for the first time the distribution of AR QT lengths among MBC patients in Egypt. Paraffin-embedded tumor tissues from 44 Egyptian MBC patients were analyzed for this polymorphism. Amplification followed by fragment length analysis revealed QT length. For the control series, blood from 43 Egyptian males without a family or personal history of breast or prostate cancers was collected and analyzed similarly. There was no significant difference between patients and controls with respect to mean QT length (P = 0.84; means were 19.5 ± 2.8 and 19.3 ± 4.2, for patients and controls, respectively). Though, short QT lengths were more prevalent among controls (14.0%), but almost absent in cases (2.3%). Although the mean lengths were not different in cases and controls, the near absence of short tracts in cases suggests a possible protective effect of very short QT lengths against MBC. In populations in which there is variable incidence of MBC by region, investigations of the distribution of AR QT lengths are warranted to further delineate its role as a risk factor in MBC.
Keywords: Androgen receptor, Male breast cancer, CAG repeat, Polymorphism, Developing countries, Egypt
Introduction
Male breast cancer is a relatively rare disease, accounting for approximately 1% of all breast cancers in the United States [1]. Of the 209,060 total cases of breast cancer expected in the U.S. in 2010, 1,970 (0.94%) will occur in men and 390 men are expected to die from the disease in 2010 [1].
There is a broad global variability in the rates and risk factors for MBC. In Africa, the proportion of male breast cancer relative to all breast cancer is estimated to be 1.42% in Egypt [2], 2.3% in Rabat, Morocco [3], 2.9% in Tanzania [4], and 8.9% in South Western Nigeria [5]. Incidence rates of MBC have also been observed to change over time. In Egypt, incidence rates were reported to be up to 12-times that of the United States [6], several decades ago, but the current incidence rate is only slightly higher than the U.S. rate [7]. While this shift in MBC proportion may be attributed in part to hospital-based data of earlier studies in Egypt [6, 8], others point to the recent significant decline in the Schistosoma parasitic infection and its associated liver fibrosis [9-14] as a major protective factor. Liver disease is believed to be a risk factor for MBC because of the associated high circulating level of estrogen, which stimulates breast tissue growth [15]. AR QT length may modulate the MBC risk further and variations in populations’ QT length distribution may help to explain the different international rates in MBC.
The molecular etiology of MBC is not well defined. A variety of studies offer conflicting results in part due to the rarity of the disease [16] and paucity of national population-based registries [17, 18]. Studies show that 10-20% of all MBC are familial [19-21] and that men with BRCA2 mutations have an 8.4% risk of MBC up to the age of 80 years [22]. Klinefelter’s Syndrome, or 47XXY syndrome, is also associated with MBC [16, 21]. Patients with this syndrome are up to 50 times more likely to develop male breast cancer than normal 46XY males [16, 23]. Other known risk factors for MBC include gynecomastia, diabetes, obesity, and orchitis/epididymitis [16, 21, 24]. A recent large epidemiologic investigation of the disease in a cohort of veteran administration men showed significant associations of MBC with diabetes (Relative Risk (RR) 1.30, 95% CI 1.05–1.60), obesity (RR 1.98, 1.55–2.54), and orchitis/epididymitis (1.84, 1.10–3.08), Klinefelter’s Syndrome (29.64, 12.26–71.68), and gynecomastia (5.86, 3.74–9.17). The study did not show an association with diabetes, liver cirrhosis, prostate disease, broken bones, thyroid diseases, or smoking-related conditions, which are hypothesized to have an association with MBC [16].
Hormonal factors are especially important in breast cancer development. Androgens, like dihydrotestosterone, restrain tissue growth in the breast thereby exerting antimitogenic effects [25]. The AR activity modulates breast tissue growth inhibition. The transactivational power of the AR is inversely related to its length [25-27]. In breast tissue then, a long AR will be weaker and worse at restraining tissue growth. Within the AR the highly polymorphic region of glutamine repeats called the polyglutamine tract (QT) is a prime candidate as a risk modulator. QT lengths are known to vary according to ethnicity [28, 29], and any individual’s QT length can vary from 6–39 glutamines, resulting in differing androgen receptor activity [28]. A longer QT results in a weaker AR. As such, we expect a population of MBC to have a longer average QT length when compared to a similar population without breast cancer.
Recent studies indicate that the incidence rates of male breast cancer are on the rise [21]. Over the past few decades, male breast cancer incidence rates have increased 26% in the United States [30]. Egypt presents a good setting to study male breast cancer. The decrease in liver disease rates experienced in this population along with a variety of environmental exposures such as xenoestrogens [31, 32] may be informative as to the risk the AR QT contributes to MBC. In this study, we investigated for the first time the distribution of QT lengths in male breast cancer patients and normal controls in Egypt and uncovered potentially important differences with regards to shorter QT lengths that are nearly absent in MBC cases.
Materials and methods
Study population
Patients in this study came from two sources, the National Cancer Institute of Cairo University (NCI-Cairo) and the Tanta Cancer Center (TCC) in the Nile delta region. NCI-Cairo is the largest cancer center in Egypt with referrals from all regions of the country [32]. TCC is located in Gharbiah Province in the center of the Nile delta region and is the home of the only population-based registry of Egypt that is funded by the National Cancer Institute of the U.S. [2].
Cases
Male breast cancer patient records were obtained for 140 patients at NCI-Cairo and 71 patients at TCC; these 211 subjects represented all male patients with breast cancer seen at the two institutions during the period of 1999–2006. Patients’ medical records were retrieved and the following information was abstracted from them: histopathologic and treatment characteristics, such as tumor grade, hormone receptor status, lymph node involvement, and laterality of disease. Of the 211 subjects, tissues were obtained from 47 patients, 33 from NCI-Cairo, and 14 from TCC; QT length was determined for 31 and 13, respectively. Tumor tissue paraffin blocks were available only for patients diagnosed in the 3–4 years preceding 2006 due to institutional limitations of paraffin blocks.
Controls
Forty-three blood samples were collected from blood donors at the TCC from March to October of 2010. Samples were from residual whole blood donations of men who did not have a personal history of breast or prostate cancer or a family history of male breast cancer. The study was approved by the Institutional Review Boards of the University of Michigan and the Gharbiah Cancer Society.
Methods
Tumor tissues were used for staining for BRCA2 status determination and QT length determination according to the following laboratory methods:
DNA extraction
Formalin-fixed paraffin-embedded (FFPE) tumor tissues were obtained from 47 Egyptian men with breast cancer. Hematoxylin and eosin staining and analysis by a pathologist allowed for differentiation of normal tissue from tumor tissue for 44 cases (31 from NCI-Cairo, 13 from TCC). Microdissection of normal tissue from the tumor blocks allowed for working samples to represent the true genome in MBC patients. DNA was isolated according to a protocol specialized for FFPE tissues provided by Qiagen (QIAamp DNA FFPE Tissue Kit; Qiagen, Valencia, CA). For the control series, PAXgene Blood DNA Tubes provided by Qiagen allowed for collection of samples in Egypt and subsequent DNA isolation in the U.S. with the PAX-gene Blood DNA Kit.
Q-tract size determination
On the molecular level, the glutamines that appear in the polyglutamine tract of the androgen receptor are encoded by a series of CAG repeats in the DNA of the AR gene. Each sequence of CAG base pairs in this region of the AR gene will result in one glutamine in the androgen receptor. The QT is located in the first exon of the AR gene on the X chromosome [33]. Non-Klinefelter’s males, then, will exhibit only one allele for this polymorphism. Amplification of only one allele in every case confirms this.
PCR was used to amplify the AR gene CAG repeat region. Primers F 5′-TGCGCGAAGTGATCCAGAACC-3′ and R 5′-CTCATCCAGGACCAGGTAGCC-3′ were chosen to amplify a region containing the repeat polymorphism of about 250 base pairs [34]. The forward primer was fluorescently labeled with 6-carboxy-fluorescine (FAM). 100 ng of DNA was amplified in a reaction mix containing 1 μl of each primer at 10 pmol, 15 μl of GeneAmp Fast PCR Mix from ABI (Applied Biosystems, Foster City, CA), and distilled water to bring to final volume to 30 μl. PCR was performed according to a standard protocol (modified from Young et al. [34]); starting with 95°C for 1 min; followed by 40 cycles of 95° denaturation for 15 s, 55° annealing for 15 s, and 72° extension for 30 s; ending with a final extension at 72° for 7 min. The PCR products were run on a 1% agarose gel to confirm amplification. As the AR gene is located on the X chromosome, men should have only one allele. However, amplification of trinucleotide repeat regions results in products of various sizes [33]. If the true size of a QT is 22 glutamines, then amplification will result in copied strands containing 22 glutamines, 21, 20, and so on. However, it has been shown that the true size of the CAG repeat region will be the most abundant strand in this mixture of amplified strands resulting from the PCR process [33].
The PCR products were examined by amplified fragment length polymorphism analysis to determine the length and frequency of amplified strands, thereby obtaining the size of the subjects’ AR QT allele (modified from Blanco et al. [33]). 1 μl of the FAM-labeled PCR products were diluted with 150 μl of water; 1 μl of this diluted mixture was transferred to a MicroAmp Optical 96-Well Reaction Plate with Barcode from ABI. To each sample, a mixture of 12 μl Hi-Di Formamide and 0.04 μl GeneScan-500LIZ size standard (orange) from ABI were added. Allele frequencies were determined using GeneMarker software by Soft Genetics LLC (State College, PA).
Non-FAM-labeled primers were used in a separate PCR to prepare the reactions for sequencing in order to confirm the CAG repeat polymorphism. Reactions were sequenced with both the reverse and non-FAM-labeled forward primer according to a standard sequencing protocol [33]. Sequencing verifies a successful amplification of the CAG repeat region.
Statistical analysis
The mean QT length of the male breast cancer population was compared to that of the control population. The student’s t-test was used to determine the significance of this difference. Frequency distributions of QT lengths were compared using Fisher’s exact χ2 analysis. The cut-off value for statistical significance was P value = 0.05. SAS version 9.1 (SAS Institute, Cary, NC) was used.
Results
Table 1 shows the histopathological features of the MBC patients. There was no significant difference with respect to mean QT length for any tumor feature. Tumor grade (II: 20.1 ± 3.8, III: 19.0 ± 2.4, P = 0.579), BRCA2 status (Present: 19.2 ± 2.4, Mutated: 20.3 ± 4.1, Absent: 19.0 ± 4.2, P = 0.557), the laterality of disease (Left: 19.8 ± 3.1, Right: 19.8 ± 2.8, P = 0.932), whether the lymph nodes were positive for disease (Negative: 19.7 ± 2.0, Positive: 19.9 ± 3.9, P = 0.814), ER hormone receptor status (Negative: 20.5 ± 0.7, Positive: 19.3 ± 2.2, P = 0.473), and PR hormone receptor status (Negative: 19.5 ± 0.7, Positive: 19.5 ± 2.3, P = 0.979) were found to have no statistically significant effect on mean QT lengths. Furthermore, there was no significant difference in mean QT length between patients from NCI-Cairo, a largely urban center, and TCC, a mixed rural and urban population (NCI-Cairo: 19.4 ± 3.0, TCC: 19.7 ± 2.2, P = 0.719).
Table 1.
Summary of histopathological characteristics and QT length analysis in male breast cancer patient group
| Characteristic | Number of patients |
QT length (mean ± SD) |
P value (t-test) |
|---|---|---|---|
| Hospital | |||
| NCI-Cairo | 31 | 19.4 ± 3.0 | 0.719 |
| TCC | 13 | 19.7 ± 2.2 | |
| Tumor grade | |||
| II | 15 | 20.1 ± 3.8 | 0.579 |
| III | 4 | 19.0 ± 2.4 | |
| BRCA2 status | |||
| Present | 32 | 19.2 ± 2.4 | 0.557a |
| Mutated | 9 | 20.3 ± 4.1 | |
| Absent | 2 | 19.0 ± 4.2 | |
| Laterality | |||
| Left breast | 16 | 19.8 ± 3.1 | 0.932 |
| Right breast | 13 | 19.8 ± 2.8 | |
| Lymph node status | |||
| Negative | 18 | 19.7 ± 2.0 | 0.814 |
| Positive | 13 | 19.9 ± 3.9 | |
| ER status | |||
| Negative | 2 | 20.5 ± 0.7 | 0.473 |
| Positive | 11 | 19.3 ± 2.2 | |
| PR status | |||
| Negative | 2 | 19.5 ± 0.7 | 0.979 |
| Positive | 11 | 19.5 ± 2.3 |
Fisher’s exact test
Table 2 shows the mean QT length among the breast cancer patients and controls. There was no significant difference in mean QT lengths for the MBC patients and controls (MBC patients: 19.5 ± 2.8, Controls: 19.3 ± 4.2, P = 0.843). There was no statistical difference in average ages between the two groups (MBC patients: 59.4 ± 15.6, Controls: 57.5 ± 7.5, P = 0.476).
Table 2.
Comparison of mean QT repeat length in normal Egyptian population and male breast cancer patient group
| MBC cases (n = 44) |
Controls (n = 43) |
P value (t-test) |
|
|---|---|---|---|
| QT length | |||
| Mean ± SD | 19.5 ± 2.8 | 19.3 ± 4.2 | 0.843 |
| Median | 20 | 20 | |
| Range | 14–27 | 7–28 | |
| Age | |||
| Mean ± SD | 59.4 ± 15.6 | 57.5 ± 7.5 | 0.476 |
Figure 1 illustrates the QT length distribution among the MBC patients and control groups. While there are no defined cutoff points for QT categories, previous studies have used allele lengths ranging from 21 to 28 as a definition of ‘‘long’’ QT lengths [35]. This study used allele lengths of ≥22 and ≤14 as ‘‘long’’ and ‘‘short’’ QT length cut-points because they represent the upper and lower 20th percentile of our control population. This can be intuited in Fig. 1, which shows the majority of QT lengths to be within these boundaries. The MBC patients and controls had approximately equal proportions of subjects with long QT’s (MBC patients: 22.7%, Controls: 25.6%, P = 0.806). However, controls were more likely to exhibit short QT lengths than MBC patients (MBC patients: 2.3%, Controls: 14.0%, P = 0.058).
Fig. 1.
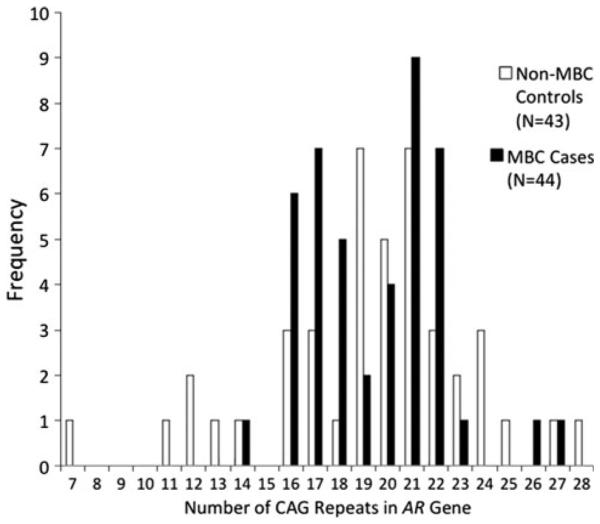
Distribution of QT lengths in normal Egyptian population and male breast cancer patient group
Discussion
This study revealed the following important findings: first, there was not a significant difference in the mean QT length between MBC patients and controls. Second, long QT lengths were not more common in patients than controls, but rather had similar frequencies. Third, there was no difference by clinical factors regarding QT lengths in the MBC patients. Fourth, there was a strong trend toward short lengths being more prevalent in cases than in controls.
Regarding the comparison of mean QT lengths in MBC patients and controls, four studies from Sweden [20], Scotland [34], Finland [36], and Australia [35] investigated the QT length relationship in MBC patients and controls in these countries. All four of the studies showed no significant difference in mean QT length between MBC patients and controls.
When considering the distribution of QT lengths, only the study from Australia showed longer QT lengths to be statistically more common in patients than controls [35]. The higher proportion of shorter QT lengths among controls that we observed in our study was also described in a study from Scotland that found only one male breast cancer patient but six controls with QT lengths of 18 or less. It has been postulated that there is a protective effect of a short QT on MBC [34]. This study’s observation of more short QT lengths among the control population supports this, and warrants further investigation.
Our finding of no significant difference in mean QT length between the different histopathological characteristics is consistent with the Australian study [35] that found no statistically significant difference in mean QT lengths between tumor grades, estrogen receptor status, progesterone receptor status, or lymph node involvement [35].
No studies have been published from Egypt on AR QT length and MBC. The only study on the androgen receptor QT length from Egypt investigated the relationship between QT length and infertility in Egyptian males [37]. Although no significant association was found between QT length and male infertility, a significant and positive association between QT length and serum testosterone concentration was observed [37]. It is notable that this study’s control population of 52 fertile men from a geographically representative sample of Egyptians had an average QT length of 18.18 ± 3.63 [37], consistent with that in our control group. Populations from different countries were also studied for QT length variations. Esteban et al. studied Berber populations in North Africa along the Mediterranean region. The study included three Berber populations from three Moroccan regions (High Atlas, Middle Atlas, and Northeast Atlas) and Siwa Berbers in Western Egypt. The Siwa Berbers had a mean QT length of 20.58 and exhibited a higher percentage of shorter QT lengths compared to the other Moroccan populations [29]. The authors further note that North African populations have the lowest degree of medium QT lengths (19–21) but an intermediate degree of short QT lengths (≥18) [29].
Our study is the first investigation of QT length in Egyptian men with breast cancer. The study has the strengths of including men from different geographical representative regions of the country. Furthermore, the availability of clinical and pathological data and BRCA2 status added to the strength of the study. The limitations of the study include the relatively small sample size, which precluded the conduct of more sophisticated statistical analysis. However, owing to the rarity of MBC, most studies of MBC have fewer or similar number of cases [20, 34-36].
To conclude, although this study highlights the lack of statistically significant difference between MBC patients and controls with respect to QT length, the strong trend toward higher proportion of short QT length in controls suggests the hypothesis that short QT length acts as a protective factor for MBC. Prospective and larger case–control studies across populations of different MBC incidence [24], with clinical and epidemiologic data will enable the more accurate delineation of the role of the QT length as a risk factor in MBC. This study was reported taking into consideration the REMARK guidelines [38].
Acknowledgments
This research, Samuel Gilbert, and Ashley Strahley, were supported by the Cancer Epidemiology Education in Special Populations Program of the University of Michigan, an R25 Cancer Education Grant from the National Cancer Institute (R25 CA112383). The work was also supported by the Breast Cancer Research Foundation, the Avon Foundation, the Debbie Strange-Brown Inflammatory Breast Cancer Foundation, and the Tempting Tables Organization. The authors of this study would like to thank Dr. Khaled Daboos of the Tanta Cancer Center for his generous assistance in collecting blood samples to use as controls and Dr. Leon Raskin at the University of Michigan for his valuable guidance in interpreting the allele fragment analyses.
Footnotes
Conflict of interest The authors do not have any to declare. This study was reported taking into consideration the REMARK guidelines.
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. 2010. doi:10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Freedman L, Edwards BK, Ries LAG, Al-Kayed S, Barchana M, Ibrahim AS, Komodiki C, Young JL. Overview and summary data. In: Freedman LS, Edwards BK, Ries LAG, Young JL, editors. Cancer incidence in four member countries (Cyprus, Egypt, Israel, and Jordan) of the Middle East Cancer Consortium (MECC) compared with US SEER. Bethesda, MD: 2006. pp. 1–27. NIH Pub. No. 06-5873. [Google Scholar]
- 3.Incidence Des Cancer a Rabat, 2005. Cancer du Sein; Rabat, Morocco: 2009. pp. 45–47. [Google Scholar]
- 4.Burson AM, Soliman AS, Ngoma TA, Mwaiselage J, Ogweyo P, Eissa MS, Dey S, Merajver SD. Clinical and epidemiologic profile of breast cancer in Tanzania. Breast Dis. 2010 doi: 10.3233/BD-2009-0296. doi: 10.3233/BD-2009-0296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oguntola AS, Aderonmu AO, Adeoti ML, Olatoke SA, Akanbi O, Agodirin SO. Male breast cancer in LAUTECH teaching hospital Osogbo, South Western Nigeria. Niger Postgrad Med J. 2009;16:166–170. [PubMed] [Google Scholar]
- 6.El-Gazayerli MM, Abdel-Aziz AS. On bilharziasis and male breast cancer in Egypt: a preliminary report and review of the literature. Br J Cancer. 1963;17:566–571. doi: 10.1038/bjc.1963.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rennert G. Breast cancer. In: Freedman LS, Edwards BK, Ries LAG, Young JL, editors. Cancer incidence in four member countries (Cyprus, Egypt, Israel, and Jordan) of the Middle East Cancer Consortium (MECC) compared with US SEER. Bethesda, MD: 2006. pp. 73–79. NIH Pub. No. 06-5873. [Google Scholar]
- 8.Soliman AS, Bondy ML, Raouf AA, Makram MA, Johnston DA, Levin B. Cancer mortality in Menofeia, Egypt: comparison with US mortality rates. Cancer Causes Control. 1999;10:349–354. doi: 10.1023/a:1008968701313. doi:10.1023/A:1008968701313. [DOI] [PubMed] [Google Scholar]
- 9.Barakat R, Farghaly A, El Masry AG, El-Sayed MK, Hussein MH. The epidemiology of Schistosomiasis in Egypt: patterns of Schistosoma mansoni infection and morbidity in Kafer el-Sheikh. Am J Trop Med Hyg. 2000;62:21–27. doi: 10.4269/ajtmh.2000.62.21. [DOI] [PubMed] [Google Scholar]
- 10.Michelson MK, Azziz FA, Gamil FM, Wahid AA, Richards FO, Juranek DD, Habib MA, Spencer HC. Recent trends in the prevalence and distribution of Schistosomiasis in the Nile delta region. Am J Trop Med Hyg. 1993;49:76–87. doi: 10.4269/ajtmh.1993.49.76. [DOI] [PubMed] [Google Scholar]
- 11.Anwar WA, Khaled HM, Amra HA, El-Nezami H, Loffredo CA. Changing pattern of hepatocellular carcinoma (HCC) and its risk factors in Egypt: possibilities for prevention. Mutat Res. 2008;659:176–184. doi: 10.1016/j.mrrev.2008.01.005. doi:10.1016/j.mrrev.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 12.El-Khoby T, Galal N, Fenwick A, Barakat R, El-Hawey A, Nooman Z, Habib M, Abdel-Wahab F, Gabr NS, Hammam HM, Hussein MH, Mikhail NN, Cline BL, Strickland GT. The epidemiology of Schistosomiasis in Egypt: summary findings in nine governorates. Am J Trop Med Hyg. 2000;62:88–99. doi: 10.4269/ajtmh.2000.62.88. [DOI] [PubMed] [Google Scholar]
- 13.Sherif M, Ibrahim AS, El-Aaser AA. Prostatic carcinoma in Egypt: epidemiology and etiology. Scand J Urol Nephrol. 1980;55:25–26. [PubMed] [Google Scholar]
- 14.Gouda I, Mokhtar N, Bilal D, El-Bolkainy T, El-Bolkainy NM. Bilharziasis and bladder cancer: a time trend analysis of 9843 patients. J Egypt Natl Cancer Inst. 2007;19:158–162. [PubMed] [Google Scholar]
- 15.Sorensen HT, Friis S, Olsen JH, Thulstrup AM, Mellemkjaer L, Linet M, Trichopoulos D, Vilstrup H, Olsen J. Risk of breast cancer in men with liver cirrhosis. Am J Gastroenterol. 1998;93:231–233. doi: 10.1111/j.1572-0241.1998.00231.x. doi:10.1111/j.1572-0241.1998.00231.x. [DOI] [PubMed] [Google Scholar]
- 16.Brinton LA, Carreon JD, Gierach GL, McGlynn KA, Gridley G. Etiologic factors for male breast cancer in the U.S. Veterans affairs medical care system database. Breast Cancer Res Treat. 2010;119:185–192. doi: 10.1007/s10549-009-0379-0. doi:10.1007/s10549-009-0379-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dey S, Zhang Z, Hablas A, Seifeldein IA, Ramadan M, El-Hamzawy H, Soliman AS. Geographic patterns of cancer in the population-based registry of Egypt: possible links to environmental exposures. Cancer Epidemiol. 2010 doi: 10.1016/j.canep.2010.09.010. doi:10.1016/j.canep.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 18.Khatib O, Aljurf M. Cancer prevention and control in the eastern Mediterranean region: the need for a public health approach. Hematol Oncol Stem Cell Ther. 2008;1:44–52. doi: 10.1016/s1658-3876(08)50060-4. [DOI] [PubMed] [Google Scholar]
- 19.Rosenblatt KA, Thomas DB, McTiernan A, Austin MA, Stalsberg H, Stemhagen A, Thompson WD, Curnen MG, Satariano W, Austin DF. Breast cancer in men: aspects of familial aggregation. J Natl Cancer Inst. 1991;83:849–854. doi: 10.1093/jnci/83.12.849. doi:10.1093/jnci/83.12.849. [DOI] [PubMed] [Google Scholar]
- 20.Haraldsson K, Loman N, Zhang QX, Johannsson O, Olsson H, Borg A. BRCA2 germ-line mutations are frequent in male breast cancer patients without a family history of the disease. Cancer Res. 1998;58:1367–1371. [PubMed] [Google Scholar]
- 21.Gomez-Raposo C, Zambrana Tevar F, Sereno Moyano M, Lopez Gomez M, Casado E. Male breast cancer. Cancer Treat Rev. 2010;36:451–457. doi: 10.1016/j.ctrv.2010.02.002. doi:10.1016/j.ctrv.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Evans DG, Susnerwala I, Dawson J, Woodward E, Maher ER, Lalloo F. Risk of breast cancer in male BRCA2 carriers. J Med Genet. 2010;47:710–711. doi: 10.1136/jmg.2009.075176. doi:10.1136/jmg.2009.075176. [DOI] [PubMed] [Google Scholar]
- 23.Brinton LA. Breast cancer risk among patients with Klinefelter syndrome. Acta Paediatr. 2011 doi: 10.1111/j.1651-2227.2010.02131.x. doi:10.1111/j.1651-2227.2010.02131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Onami S, Ozaki M, Mortimer JE, Pal SK. Male breast cancer: an update in diagnosis, treatment and molecular profiling. Maturitas. 2010;65:308–314. doi: 10.1016/j.maturitas.2010.01.012. doi:10.1016/j.maturitas.2010.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferro P, Catalano MG, Dell’Eva R, Fortunati N, Pfeffer U. The androgen receptor CAG repeat: a modifier of carcinogenesis? Mol Cell Endocrinol. 2002;193:109–120. doi: 10.1016/s0303-7207(02)00104-1. doi:10.1016/S0303-7207(02) 00104-1. [DOI] [PubMed] [Google Scholar]
- 26.Lindstrom S, Ma J, Altshuler D, Giovannucci E, Riboli E, Albanes D, Allen NE, Berndt SI, Boeing H, Bueno-de-Mesquita HB, Chanock SJ, Dunning AM, Feigelson HS, Gaziano JM, Haiman CA, Hayes RB, Henderson BE, Hunter DJ, Kaaks R, Kolonel LN, Le Marchand L, Martinez C, Overvad K, Siddiq A, Stampfer M, Stattin P, Stram DO, Thun MJ, Trichopoulos D, Tumino R, Virtamo J, Weinstein SJ, Yeager M, Kraft P, Freedman ML. A large study of androgen receptor germline variants and their relation to sex hormone levels and prostate cancer risk results from the national cancer institute breast and prostate cancer cohort consortium. J Clin Endocrinol Metab. 2010;95:E121–E127. doi: 10.1210/jc.2009-1911. doi:10.1210/jc.2009-1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamberlain NL, Driver ED, Miesfeld RL. The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function. Nucleic Acids Res. 1994;22:3181–3186. doi: 10.1093/nar/22.15.3181. doi:10.1093/nar/22.15.3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buchanan G, Yang M, Cheong A, Harris JM, Irvine RA, Lambert PF, Moore NL, Raynor M, Neufing PJ, Coetzee GA, Tilley WD. Structural and functional consequences of glutamine tract variation in the androgen receptor. Hum Mol Genet. 2004;13:1677–1692. doi: 10.1093/hmg/ddh181. doi:10.1093/hmg/ddh181. [DOI] [PubMed] [Google Scholar]
- 29.Esteban E, Rodon N, Via M, Gonzalez-Perez E, Santamaria J, Dugoujon JM, Chennawi FE, Melhaoui M, Cherkaoui M, Vona G, Harich N, Moral P. Androgen receptor CAG and GGC polymorphisms in Mediterraneans: repeat dynamics and population relationships. J Hum Genet. 2006;51:129–136. doi: 10.1007/s10038-005-0336-7. doi:10.1007/ s10038-005-0336-7. [DOI] [PubMed] [Google Scholar]
- 30.Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men: a population-based study. Cancer. 2004;101:51–57. doi: 10.1002/cncr.20312. doi:10.1002/cncr.20312. [DOI] [PubMed] [Google Scholar]
- 31.Dey S, Soliman AS, Hablas A, Seifeldin I, Ismail K, Ramadan M, El-Hamzawy H, Wilson ML, Banerjee M, Boffetta P, Harford J, Merajver SD. Urban rural differences in breast cancer incidence by hormone receptor status across 6 years in Egypt. Breast Cancer Res Treat. 2010;120:149–160. doi: 10.1007/s10549-009-0427-9. doi:10.1007/s10549-009-0427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Felix AS, Soliman AS, Khaled H, Zaghloul MS, Banerjee M, El-Baradie M, El-Kalawy M, Abd-Elsayed AA, Ismail K, Hablas A, Seifeldin IA, Ramadan M, Wilson ML. The changing patterns of bladder cancer in Egypt over the past 26 years. Cancer Causes Control. 2008;19:421–429. doi: 10.1007/s10552-007-9104-7. doi:10.1007/s10552-007-9104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blanco S, Suarez A, Gandia-Pla S, Gomez-Llorente C, Antunez A, Gomez-Capilla JA, Farez-Vidal ME. Use of capillary electrophoresis for accurate determination of CAG repeats causing Huntington disease. An oligonucleotide design avoiding shadow bands. Scand J Clin Lab Invest. 2008;9:1–8. doi: 10.1080/00365510801915171. doi:10.1080/00365510801915171. [DOI] [PubMed] [Google Scholar]
- 34.Young IE, Kurian KM, Mackenzie MA, Kunkler IH, Cohen BB, Hooper ML, Wyllie AH, Steel CM. The CAG repeat within the androgen receptor gene in male breast cancer patients. J Med Genet. 2000;37:139–140. doi: 10.1136/jmg.37.2.139. doi:10.1136/jmg.37.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacLean HE, Brown RW, Beilin J, Warne GL, Zajac JD. Increased frequency of long androgen receptor CAG repeats in male breast cancers. Breast Cancer Res Treat. 2004;88:239–246. doi: 10.1007/s10549-004-0781-6. doi:10.1007/s10549-004-0781-6. [DOI] [PubMed] [Google Scholar]
- 36.Syrjakoski K, Hyytinen ER, Kuukasjarvi T, Auvinen A, Kallioniemi OP, Kainu T, Koivisto PA. Androgen receptor gene alterations in Finnish male breast cancer. Breast Cancer Res Treat. 2003;77:167–170. doi: 10.1023/a:1021369508561. doi:10.1023/A:1021369508561. [DOI] [PubMed] [Google Scholar]
- 37.Badran WA, Fahmy I, Abdel-Megid WM, Elder K, Mansour R, Kent-First M. Length of androgen receptor-CAG repeats in fertile and infertile Egyptian men. J Androl. 2009;30:416–425. doi: 10.2164/jandrol.108.005843. doi:10.2164/jandrol.108.005843. [DOI] [PubMed] [Google Scholar]
- 38.McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM, Statistics Subcommittee G of NCI-EORTC Working group on Cancer Diagnostics Reporting recommendations for tumor marker prognostic studies (REMARK) Breast Cancer Res Treat. 2006;100:229–235. doi: 10.1007/s10549-006-9242-8. doi:10.1007/s10549-006-9242-8. [DOI] [PubMed] [Google Scholar]


