Abstract
Gastrocolic fistula (GCF) is associated with a variety of diseases, but in recent years it has most frequently been observed with gastric or colonic malignancy. The management of primary tumor lesions and optimal surgical treatment strategies remain controversial. In this study, we explore the clinical diagnosis and treatment of GCF by retrospectively analyzing the records of GCF patients treated between August 2008 and February 2014. Three female patients and one male patient with an average age of 61 years were diagnosed with GCF caused by malignancy during this period. The predominant symptoms were diarrhea, vomiting, weight loss, and abdominal pain. Gastrointestinal contrast series combined with fiber endoscopy was the most accurate method of diagnosing the GCF, while CT and MRI were helpful in identifying the extent of tumor invasion and evaluating the possibility of en-bloc resection. Pathological and immunohistochemical tests, including staining for CK-20, CK-7, and CDX-2, suggested that three cases originated in the colon and one case in the stomach. All four cases underwent single-stage en-bloc fistula resection; two severely malnourished patients received concurrent colostomies. One patient died of postoperative anastomotic leakage and cardiopulmonary failure, but the remaining three patients were discharged in improved condition. En-bloc resection followed by adjuvant chemotherapy can result in long term survival. Gastrointestinal contrast series combined with fiber endoscopy showed high sensitivity in the diagnosis of GCF. Immunohistochemical staining can be conducted for tumors with an unclear source. Single-stage radical en-bloc fistula resection is the recommended surgical treatment, and concurrent colostomy should be considered in severely malnourished patients.
Keywords: Diagnosis, management, malignant, gastrocolic fistula
Introduction
Gastrocolic fistula (GCF) is a rare complication of both benign and malignant diseases of the gastrointestinal tract [1]. In the past 20 years, with the extensive use of proton pump inhibitors, GCFs are less frequently encountered as a complication of benign gastric ulcers [2,3], and the most common etiology of GCF is now malignant gastrointestinal disease, particularly locally invasive colonic and gastric carcinoma [4]. The mechanism of GCF formation is the infiltration of a tumor from the serosa of one viscus into the wall of another viscus, followed by lumen-to-lumen necrosis [5]. This results in the movement of some stomach contents directly into the colon, avoiding the normal digestive pathway and disrupting the normal digestive process. The fistula can also result in the reflux of fecal material from the colon into the stomach. This communication in the alimentary tract produces a devastating effect on the patient.
Gastrocolic fistula caused by malignant colonic and gastric disease is rare, and only 30% of patients present with the typical symptoms [6]: diarrhea, belching with fecal odor or fecal vomiting (some patients may vomit feces containing undigested food), and weight loss. Laboratory testing and physical examination show electrolyte imbalances and severe malnutrition, with some patients even appearing cachexia. The diagnosis is most reliably and frequently made by barium enema, fiber gastroscopy, and colonoscopy [4]. For patients in whom the source of the tumor cannot be identified, immunohistochemical staining can be performed, providing a basis for more effective postoperative treatment. Radical surgery remains the best treatment for GCF. The previous approach consisted of surgery in two or three phases, including colostomy, to improve the patient’s nutritional status and minimize mortality [7-10]. However, with the development of enteral and parenteral nutritional support and intensive care medicine, single-stage procedures can be used and have become the favored approach in minimizing mortality [11,12].
Despite radical en-bloc surgery to correct GCFs caused by malignant tumors, these patients usually have a poor prognosis [5]. Long-term survival has rarely been reported in this patient population [5], and diagnostic methods and surgical treatment strategies require further discussion in order to improve outcomes.
Materials and methods
In this study, we retrospectively analyzed the records of patients diagnosed with GCF from August 2008 to February 2014. All patients were diagnosed as having GCFs caused by malignant diseases. We identified three female patients and one male patient with an average age of 61 years (range, 35-73 years). All patients underwent operations in the general surgery department of Beijing Friendship Hospital, Capital Medical University, and received postoperative follow-up from the hospital’s general surgery doctors. Presenting symptoms, diagnostic studies, and surgical treatment strategies were reviewed using the case records.
Results
Case 1
A 35-year-old woman with a more than 30-year history of chronic viral hepatitis B was admitted to the hospital with a two-month history of upper abdominal pain and a change in her bowel habits to diarrhea, accompanied by vomiting and six months of weight loss (20 kg in total). Her body weight was 60.0 kg and her body mass index (BMI) was 21.3 kg/m2. Her father, uncle, and elder aunt had died of colon cancer, and her younger aunt was suffering from gastric cancer. Physical examination revealed vague left hypochondrium fullness with mild tenderness. On admission, laboratory tests showed anemia with a hemoglobin of 4.2 g/dL and hypoalbuminemia with a serum albumin of 22.3 g/L. The patient was transfused with ten units of red blood cells three times, which improved the hemoglobin to 8.2 g/dL. The CA125 level was 85.40 U/mL.
Gastroscopy revealed fecal matter in the stomach. A large ulcerated tumor was identified in the body of the stomach, which appeared likely to form a fistula or perforation. The scope was able to pass through the tumor into the pylorus and the duodenum without difficulty. Computed tomography (CT) showed a structural abnormality in the upper left abdominal cavity, including soft tissue structures containing gas and showing heterogeneous enhancement with contrast. The gastric body appeared to be connected with the transverse colon and descending colon (Figure 1A). Upper gastrointestinal contrast showed irregularity of the greater curvature of the gastric body and presence of the contrast agent in the transverse colon, considering gastrocolic fistula formation (Figure 1B).
Figure 1.
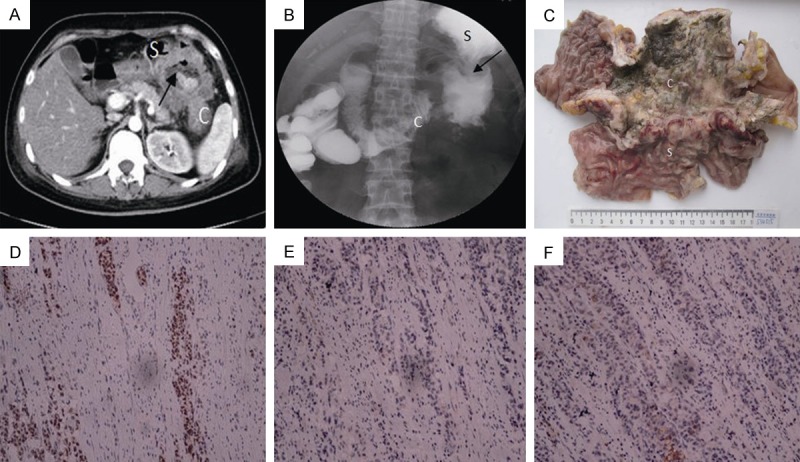
Case 1 clinical characteristics. A. Abdominal computed tomography showed a structural abnormality in the upper left abdominal cavity, including soft tissue structures containing gas and showing heterogeneous enhancement. A trickle of contrast is present in the gastrocolic fistula (arrow) between the stomach (S) and the colon (C). B. Upper gastrointestinal contrast showed contrast agent in the transverse colon (C), which was consistent with gastrocolic fistula formation (arrow). C. The resected specimen had a cutting edge distance of 5 cm on the colonic side and 6 cm on the other side (C). A giant, ulcerated tumor is visible; the tumor involved the greater curvature of the stomach (S). The fistula created a communication between the bowel and the stomach cavity. D-F. Immunohistochemical staining in turn: CDX2 (+), CK7 (-), CK20 (+) (× 400 magnification).
The preoperative diagnosis was gastric cancer and GCF formation. The patient underwent surgical exploration with palliative distal gastrectomy, partial resection of the jejunum (the proximal part), partial resection of the transverse colon (proximal stoma, remotely closed), gastrojejunostomy (Roux-Y), and jejunal side-to-side anastomosis with the duodenum. Postoperative pathology confirmed the diagnosis of GCF (Figure 1C), but the primary tumor was found to be colon cancer by immunohistochemical staining that involved the stomach, forming the GCF (Figure 1D-F). At 8 months after surgery, the patient has recovered well and has received standard XELOX scheme chemotherapy.
Case 2
A 65-year-old woman presented to the surgical clinic with epigastric pain, feculent vomiting, and post-prandial diarrhea of two years’ duration. She denied any past medical history but had been losing weight (23 kg in total) for one year. On presentation, her body weight was 30 kg and her BMI was 12.0 kg/m2. Physical examination revealed a palpable left upper quadrant mass with a diameter of approximately 10 cm accompanied by a fixed and light tenderness. Laboratory tests obtained on admission showed anemia with a hemoglobin of 6.8 g/dL and hypoalbuminemia with a serum albumin of 17.2 g/L. The CA125 level was 81.20 U/mL.
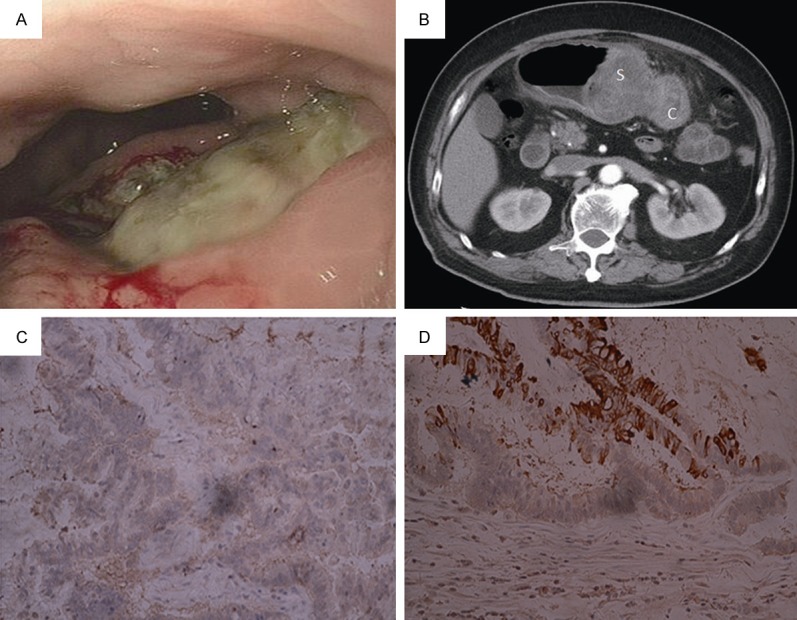
Gastroscopy revealed large ulcers of 4 cm along the greater curvature of the gastric body and a surface coating of filthy moss; a fistula with a diameter of approximately 0.3 cm was identified at the bottom of the ulcer, considered to represent GCF formation (Figure 2A). Computed tomography showed uniform thickening of the stomach and a portion of the colon wall, along with thickening of the left front abdominal soft tissues. Upper gastrointestinal contrast showed an irregularly protruding lesion at the junction of the greater curvature of the gastric body and the antrum, which was visible beneath the shadow of the contrast agent, as well as an intestinal mucosa-like structure (Figure 2B). The preoperative diagnosis was gastric cancer and GCF formation. The patient underwent surgical exploration and palliative distal gastrectomy, partial resection of the transverse colon (proximal stoma, remotely closed), and gastrojejunostomy (Roux-Y). Postoperative pathology confirmed the diagnosis of GCF, but the primary tumor was identified as colon cancer by immunohistochemical staining (Figure 2C), which involved the stomach and had created the GCF. At present, 26 months after the surgery, the patient has recovered well and is in good condition; she received standard chemotherapy with oral Xeloda monotherapy.
Figure 2.

Case 2 clinical characteristics. A. Gastroscopy showed a fistula in the bottom of the ulcer (arrow) in the greater curvature of the gastric body. B. Upper gastrointestinal contrast showed contrast agent in the transverse colon (C), consistent with gastrocolic fistula formation (arrow). C. Immunohistochemical staining: CDX2 (++) (× 400 magnification).
Case 3
A 73-year-old man was admitted to the hospital with a three-month history of upper abdominal pain after eating, which had been accompanied by vomiting and weight loss (20 kg in total) for three months. He had undergone coronary stenting because of coronary artery disease 10 years previously. His body weight was 51 kg and his BMI was 17.3 kg/m2. Physical examination revealed a palpable left upper quadrant mass with a diameter of about 5 cm, obscure boundaries, and associated fixed and light tenderness. On admission, laboratory tests showed anemia with a hemoglobin of 7.4 g/dL and hypoalbuminemia with a serum albumin of 21.6 g/L. The CA125 level was 66.70 U/mL, and the CA199 level was 1022.58 U/mL.
Gastroscopy revealed a 4 × 3 cm ulcer with irregular margins in the gastric body; yellow liquid was observed entering the stomach through the mucosal ulceration, which was consistent with a GCF (Figure 3A). Computed tomography showed lesions of the gastric body and transverse colon, establishing the possibility of a malignant tumor, although the primary source of the lesions was uncertain (Figure 3B). The preoperative diagnosis was gastric cancer with GCF formation. The patient underwent surgical exploration, radical distal gastrectomy (R0, D2, Billroth I), and radical resection of the transverse colon. Postoperative pathology confirmed the diagnosis of gastric cancer and GCF by immunohistochemical staining (Figure 3C, 3D). This patient received standard chemotherapy with oral Xeloda monotherapy; at present, 34 months after surgery, the patient is in good general condition, but peritoneal recurrence was identified 3 months ago.
Figure 3.
Case 3 clinical characteristics. A. Gastroscopy showed a 4 × 3 cm ulcer with irregular margins in the greater curvature of the gastric body; yellow liquid was observed. B. Abdominal computed tomography showed soft tissu lesions in the gastric body (S) and the transverse colon (C). C, D. Immunohistochemical staining in turn: CDX2 (-), CK20 (+) (× 400 magnification).
Case 4
A 72-year-old woman presented with a 3-year history of an abdominal mass and a 1-month history of post-prandial diarrhea. She had a 20-year history of coronary artery disease and a 10-year history of hypertension. On presentation, her body weight was 55 kg and her BMI was 22.9 kg/m2. Physical examination revealed a palpable, fixed left upper quadrant mass with a diameter of approximately 5 × 4 cm and a firm texture. On admission, laboratory tests showed anemia with a hemoglobin of 7.1 g/dL and hypoalbuminemia with a serum albumin of 24.2 g/L. The CA125 level was 264.80 U/mL, and the CA199 level was 66.02 U/mL.
Gastroscopy revealed a 6 × 5 cm ulcer with irregular margins in the posterior wall of the gastric body, and fecal liquid was observed to enter through the lesion, consistent with a GCF (Figure 4A). Lower gastrointestinal contrast showed irregular stenosis of the middle transverse colon, colonic wall stiffness, and the formation of a fistulous cavity connected with the stomach that was consistent with a GCF (Figure 4B). A MRI curved-planar reconstructed image showed an infiltrative colonic mass involving the stomach, GCF was present between the stomach and the colon (Figure 4C). Enhanced MRI showed an 8 × 6 cm irregular lesion with abnormal signal in the middle of the transverse colon, partial colonic stenosis, and apparent enhancement of the lesion, consistent with a transverse colon carcinoma (Figure 4D).
Figure 4.
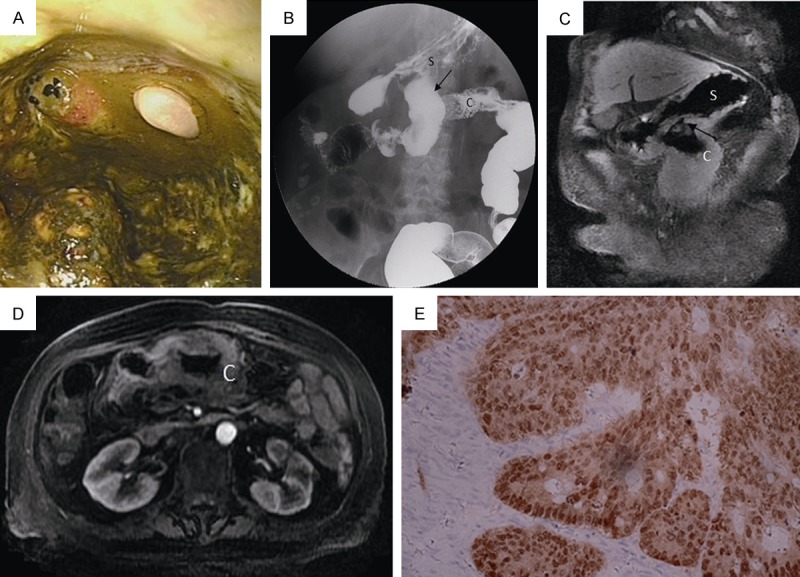
Case 4 clinical characteristics. A. Gastroscopy showed a 6 × 5 cm ulcer with irregular margins in the posterior wall of the gastric body; fecal liquid was observed. B. Lower gastrointestinal angiography showed a fistula cavity (arrow) that communicated with the stomach (S) in the middle of the transverse colon (C), consistent with gastrocolic fistula formation. C. A MRI curved-planar reconstructed image showed an infiltrative colonic mass involving the stomach. There is a gastrocolic fistula (arrow) between the stomach (S) and the colon (C). D. MRI showed an irregular 8 × 6 cm lesion with abnormal signal in the middle of the transverse colon (C), which was considered to be a transverse colon carcinoma. E. Immunohistochemical staining: CDX2 (++) (× 400 magnification).
The preoperative diagnosis was transverse colon cancer and GCF formation. The patient underwent surgical exploration with radical transverse colonic resection and partial gastrectomy. Postoperative pathology confirmed the diagnosis of transverse colon cancer and GCF (Figure 4E). The patient died of anastomotic leakage and cardiopulmonary failure 2 months postoperatively.
Discussion
There is still a scarcity of literature regarding GCFs, and the available reports are mostly case studies. Over the last 20 years, the most common cause of GCFs has been benign gastric ulcers because of the widespread use of nonsteroidal anti-inflammatory drugs. In recent years, GCFs have been identified as a severe complication of gastric or colonic carcinoma.
Adenocarcinoma of the transverse colon is more common in the Western world [13-15], whereas adenocarcinoma of the stomach is a more frequent occurrence in Japan [16]. In this study, the etiology of the observed GCFs was comparable to the case distribution in the Western world, as only one of the GCFs in our series originated from the stomach. Diarrhea, fecal vomiting, and weight loss make up the characteristic triad of clinical manifestations associated with GCF. With a longer course, there may be other clinical symptoms such as malnutrition, weight loss, anemia, and hypoproteinemia, which may be accompanied by leukocytosis and electrolyte imbalances.
Preoperative diagnostic tests contribute to the diagnosis of GCF and to the determination of the proper surgical treatment. The most accurate test for diagnosing a GCF is the barium enema, which correctly confirms the diagnosis in 95-100% of cases [17,18]. Although this modality allows for clear identification of the gastrocolic shunt and rough determination of the fistula site, its ability to determine the primary site of causative malignant disease is quite low. Meanwhile, the sensitivity of an upper gastrointestinal barium series is only 27-37%. A barium enema is able to create a certain pressure in the lumen of the colon, which is necessary for moving the barium through the fistula into the stomach; in contrast, upper gastrointestinal contrast is not able to create this pressure difference.
The second technique used for GCF identification is fiber gastroscopy and/or fiber colonoscopy, which enables direct visualization of the fistula and biopsy of the area to further clarify the nature of the pathological communication. A fiber gastroscope or colonoscope is able to directly enter the small intestine or stomach, thereby establishing the existence of a fistula. In a patient with distal colonic obstruction (i.e., case 1), it may be difficult for a fiber colonoscope or barium enema to pass through the narrow part of the colon, while gastroscopy or upper gastrointestinal angiography may be able to help confirm the fistula. In patients with an abdominal mass, CT scan or MRI can be helpful in identifying the extent of tumor invasion and the possibility of en-bloc resection.
Immunohistochemical staining is necessary to identify the primary lesion underlying a tumor-associated GCF; this information is useful in formulating the postoperative chemotherapy scheme. Immunohistochemistry, including staining for CDX-2, CK-7, and CK-20, was performed in the four GCF cases described here. When combined with the gross morphology of the pathological specimens, the results suggested that three of the cases originated in the stomach and one case originated in the colon.
Radical resection is still the best strategy for treating malignant GCFs [19]; it includes en-bloc resection of the involved gastrocolic region and suturing of the other sides of the fistula. Reconstructive procedures or a temporary diverting colostomy may be performed based on individual situations. In the past, because of the high mortality rate associated with single-stage procedures, two- or three-stage operations, potentially involving a preliminary diversion colostomy, were recommended by many surgeons to enable correction of the patient’s nutritional status and electrolyte imbalances with the goal of decreasing postoperative mortality. In the classic two-stage surgery, ileosigmoidostomy was performed first, followed by complete en-bloc fistula resection, radical colon resection, radical gastrectomy or other surgical procedures [18].
Today, with the rapid developments in parenteral and enteral support and intensive care medicine, experts and scholars are more likely to recommend a single-stage radical en-bloc fistula resection. However, this approach may not provide enough time to correct the patient’s preoperative nutritional status in cases of malignant GCF. Accordingly, the surgical procedure is individually planned for each patient. For severely malnourished patients, such as cases 1 and 2, performing single-stage en-bloc resection and concurrent colostomy may be the most suitable. In contrast, one of the patients (case 4) who underwent single-stage radical en-bloc resection died of anastomotic leakage 2 months postoperatively. Consequently, for malignant GCF cases accompanied by severe malnutrition, including patients with a low BMI, severe anemia, or hypoalbuminemia, it may be more suitable to perform colostomy at the same time as fistula resection.
In conclusion, GCF associated gastrointestinal malignancy should be suspected in patients who present with diarrhea or fecal vomiting. Barium enema is thought to be the most accurate test for diagnosing a GCF, while immunohistochemical staining can help to identify the primary lesion in malignancy-associated GCF. Single-stage procedures, with or without concurrent colostomy, are preferred by most scholars if the general condition of the patient is suitable.
Acknowledgements
This study was supported by grants from Capital clinical characteristic application study in Science and Technology Commission of Beijing (No. Z131107002213046), Capital health research and development of special (No. 2011100203).
Disclosure of conflict of interest
None.
References
- 1.Cody JH, DiVincenti FC, Cowick DR, Mahanes JR. Gastrocolic and gastrojejunocolic fistulae: report of twelve cases and review of the literature. Ann Surg. 1975;181:376–380. doi: 10.1097/00000658-197503000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Levine MS, Kelly MR, Laufer I, Rubesin SE, Herlinger H. Gastrocolic fistulas: the increasing role of aspirin. Radiology. 1993;187:359–361. doi: 10.1148/radiology.187.2.8475272. [DOI] [PubMed] [Google Scholar]
- 3.Schneider A, Holtmann G, Rünzi M, Drochner K, Oldhafer KJ, Gerken G. Gastrocolic fistula - a rare cause of cachexia and polyneuropathy. Z Gastroenterol. 2002;40:521–524. doi: 10.1055/s-2002-32800. [DOI] [PubMed] [Google Scholar]
- 4.Tavenor T, Smith S, Sullivan S. Gastrocolic fistula. A review of 15 cases and an update of the literature. J Clin Gastroenterol. 1993;16:189–191. [PubMed] [Google Scholar]
- 5.Martinez LO, Manheimer LH, Casal GL, Lubin J. Malignant fistulae of the gastrointestinal tract. Am J Roentgenol. 1978;131:215–218. doi: 10.2214/ajr.131.2.215. [DOI] [PubMed] [Google Scholar]
- 6.Chung DP, Li RS, Leong HT. Diagnosis and current management of gastrojejunocolic fistula. Hong Kong Med J. 2001;7:439–441. [PubMed] [Google Scholar]
- 7.Lowdon AG. Gastrojejunocolic fistula. Br J Surg. 1953;41:113–128. doi: 10.1002/bjs.18004116602. [DOI] [PubMed] [Google Scholar]
- 8.Thoeny RH, Hodgson JR, Scudamore HH. The roentgenologic diagnosis of gastrocolic and gastrojejunocolic fistulas. Am J Roentgenol Radium Ther Nucl Med. 1960;83:876–881. [PubMed] [Google Scholar]
- 9.Mathewson C. Preliminary colostomy in the management of gastrocolic and gastrojejunocolic fistula. Ann Surg. 1941;114:1004–1010. doi: 10.1097/00000658-194112000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pfeiffer DB. The surgical treatment of gastrojejunocolic fistula. Surg Gynecol Obstet. 1941;72:282–289. [Google Scholar]
- 11.Subramaniasivam N, Ananthakrishnan N, Kate V, Smile SR, Jagdish S, Srinivasan K. Gastrojejunocolic fistula following surgery for peptic ulcer. Trop Gastroenterol. 1997;18:183–187. [PubMed] [Google Scholar]
- 12.Alhan E, Calik A, Cinel A, Kucuktulu U. Complicated marginal ulcers after surgery for duodenal ulcer. Acta Chir Hung. 1995-1996;35:77–85. [PubMed] [Google Scholar]
- 13.Schweitzer RJ, Osborne MP. Gastrocolic fistula complicating carcinoma; report of case due to carcinoma of colon, with successful resection. Am J Surg. 1953;85:775–779. doi: 10.1016/0002-9610(53)90567-4. [DOI] [PubMed] [Google Scholar]
- 14.Marshall SF, Knud HJ. Gastrojejunocolic and gastrocolic fistulas. Ann Surg. 1957;145:770–782. doi: 10.1097/00000658-195705000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Amlicke JA, Ponka JL. Gastrocolic and gastrojejunocolic fistulas. A report of sixteen cases. Am J Surg. 1964;107:744–750. doi: 10.1016/0002-9610(64)90304-6. [DOI] [PubMed] [Google Scholar]
- 16.Matsuo S, Eto T, Ohara O, Miyazaki J, Tsunoda T, Kanematsu T. Gastrocolic fistula originating from transverse colon cancer: report of a case and review of the Japanese literature. Surg Today. 1994;24:1085–1089. doi: 10.1007/BF01367461. [DOI] [PubMed] [Google Scholar]
- 17.Ohta M, Konno H, Tanaka T, Baba M, Kamiya K, Mitsuoka H, Unno N, Sugimura H, Nakamura S. Gastrojejunocolic fistula after gastrectomy with Billroth II reconstruction: report of a case. Surg Today. 2002;32:367–370. doi: 10.1007/s005950200054. [DOI] [PubMed] [Google Scholar]
- 18.Christiansen S, Ram MD, Sachatello C, Griffen WO Jr. Management of gastrocolic fistrla. Am Surg. 1981;47:63–66. [PubMed] [Google Scholar]
- 19.Khanna MP, Gordon PH. Gastrocolic fistulization in Crohn’s disease: a case report and a review of the literature. Can J Surg. 2000;43:53–56. [PMC free article] [PubMed] [Google Scholar]


