Abstract
Objective: To determine the effects of electroacupuncture (EA) preconditioning on the blood glucose level in jugular vein and water content in brain tissues in rats undergoing cerebral ischemia reperfusion that induced injury. Methods: 90 healthy male Wister rats were randomly assigned to 3 groups: sham-operation (SH) group, cerebral ischemia reperfusion (IR) group and electroacupuncture (EA) preconditioning plus IR group. EA group was pretreated with EA delivered to acupoints of “Baihui” (Du 20) and “Shuigou” (Du 26) 30 min before cerebral ischemia. Results: No marked difference was observed in brain water content 2 h after procedure in IR group, SH group and EA group. Compared with SH group, the brain water contents in IR group and EA group were significantly higher 6 h after reperfusion and peaked at 48 h (P < 0.01). The blood glucose levels in EA and IR groups were significantly higher than that of SH group 2 h after reperfusion, which peaked at 6 h and tended to decline up to 24 h after reperfusion (P < 0.01). 2 h, 6 h, and 24 h after reperfusion, EA group had significantly lower blood glucose levels than IR group (P < 0.01). Conclusion: Electroacupuncture preconditioning can significantly inhibit the augmentation of the blood glucose level and attenuate cerebral edema induced by reperfusion, which leads to alleviation of injury caused by ischemia reperfusion.
Keywords: Electroacupuncture preconditioning, ischemia reperfusion, blood glucose, cerebral oEdem
Introduction
Ischemia reperfusion (IR) can worsen the damaged ischemic cells or even cause them to die. Studies have demonstrated that electroacupuncture (EA) induces protection against cerebral ischemia reperfusion and therapy with EA has satisfactory effect [1,2]. EA preconditioning can elevate injury caused by reperfusion and protect tissues and organs. More studies relevant to EA are ongoing to refine our understanding. But only limited evidence studied the potential of EA as an effective preconditioning method [3]. In this study, we conducted a rat model of global cerebral ischemia and first proposed to study the effects of EA conditioning administered to “Baihui” (Du 20) and “Shuigou” (Du 26) on the blood glucose level in the jugular vein and the water content in brain tissues in rats. Our preliminary results suggested that EA preconditioning exhibited cerebral protection.
Materials and methods
Experimental animals and assignment to groups
90 healthy male Wister rats, weighing 250 to 300 g, were provided by the laboratory animal center of the Harbin Medical University-affiliated Second Hospital and housed at an ambient temperature of 23±1°C with standard light-dark cycle (light circle from 6:00 a.m. to 6:00 p.m.) and free access to food and water. After an adaptive period of 5 days, animals were randomly assigned to 3 groups (n=30 for each), including the SH group, the IR group and the EA preconditioning plus IR group. Each group was divided into three sub-groups (n=10 for each) based on the time points (2 h, 6 h, 24) of ischemia reperfusion. All animal procedures were approved by the Animal Ethics Committee of the Harbin Medical University.
Establishment of animal model
The model of global cerebral ischemia, with some modifications to those described in previous studies [4,5], was established by performing occlusion of both common carotid arteries combined with lowering the whole body blood pressure. The animals were anesthetized with intraperitoneal administration of 10% chloral hydrate (350 mg/kg) after 12-h fasting. For each animal, a catheter was advanced through the mouth and into the trachea. After that, the animals were fixed at spine position, connected with a ventilator. The scheduled blood gas analysis was conducted to adjust the respiratory rate and tidal volume to maintain the PetCO2 and the pH of artery blood within physiological range. The fur on the neck region was shaved and disinfected with 70%-alcohol wipe. After an incision was made in the midline of the neck, both common carotid arteries were separated and a segment of suture easy to retrieve was inserted. The femoral arteries were separated after an incision was made on both groins. The indwelling tube placed in the left femoral artery was used for collection of blood and monitoring of blood pressure, while the right one was used for blood releasing and transfusion. The SH group was only subjected to exposed both common carotid arteries and indwelling of catheter in femoral artery under the same anesthesia and procedures except for occlusion of the common carotid arteries and blood transfusion used in the IR group. In the other groups, blood was collected via the right femoral artery with a heparinized syringe. When the MAP was lowered to 35-40 mmHg (1 mmHg=0.133 kPa), both common carotid arteries were occluded with non-invasive aneurysm clips to induce cerebral ischemia. During cerebral ischemia, the MAP was controlled under 35 to 40 mmHg by withdrawing blood from the femoral artery. Also, electroencephalogram (EEG) was performed by placing electrodes into bilateral temporal region to scan and record the brain waves. Equal potential was observed in the EEG 10 to 15 s after the onset of ischemia, so the model of cerebral ischemia was successfully established. 15 min after the onset of ischemia, the clips were removed. And reperfusion was performed by blood transfusion. During the procedure, the temperature of rectum was maintained at 37 to 38°C using thermostatic electric blanket.
EA preconditioning
The EA group was subjected to EA stimulation prior to the onset of cerebral ischemia. The EA was delivered to acupoints of “Baihui” (Du 20) and “Shuigou” (Du 26) based on the method described in a national teaching material called Experimental Acupuncture. A stainless-steel Hwato needle (25 mm length with 0.40 mm in diameter,) was obliquely inserted at a depth of 2 mm in the midline of parietal bone to approach Du 20. The depth of needle on Du 26 was 1 mm vertically to the skin in the center of the upper lip, a point at a distance of 1 mm from nose. When tightness was felt around the needle, the needle was connected with G6805 EA apparatus (made in Shanghai) using dilatational waves at an intensity of 1 mA and a frequency of 2/15 Hz. The stimulation lasted for 30 min at an intensity which might mildly shake the heads of rats.
Determination of the water content in brain tissues
The animals in each group were sacrificed at stated time points. The brain tissues were removed. The moisture on the surface was dried with a filter paper. The brain tissues were covered with tinfoil which was previously weighed and labeled. First, the wet weight of brain tissues was determined by using an electronic balance. After that, the brain tissues covered with tinfoil were placed in a thermostatic oven and dried at 95°C for 24 h to a constant weight. After drying, the brain tissues were removed and allowed to recover to room temperature, and the dry weight was determined. The water content of brain tissues was calculated based on the following formula: [(Wet weight-dry weight)/wet weight ×100%].
Determination of the blood glucose level in jugular vein
The blood glucose level was determined using a blood glucose tester from Roche in Germany. One drop of jugular venous blood at each time point was used for determination of the blood glucose level.
Statistical analysis
All data was subjected to statistical analysis using SPSS13.0 software. The measurement data was presented as means±SD (x̅±s). The differences in three groups were compared with ANOVA, which were considered as significant if the P value was < 0.05.
Results
Comparison of data between groups
No significant differences were observed in some parameters such as weight, blood gas values, HR, MAP, baseline blood glucose in the SH group, IR group and EA group, as provided in Table 1.
Table 1.
Measurement of parameters such as weight, blood gas values, HR, MAP and blood glucose in each group (n=30, x̅±s)
| Parameters | SH group | IR group | E group |
|---|---|---|---|
| Weight (g) | 281±15 | 276±12 | 377±13 |
| pH | 7.41±0.05 | 7.41±0.02 | 7.42±0.16 |
| PaCO2 (mmHg) | 40.6±3.2 | 40.1±2.9 | 39.8±3.1 |
| PaO2 (mmHg) | 482±17 | 483±23 | 487±25 |
| HCO3ˉ (mmol/L) | 24.2±1.4 | 24.2±1.1 | 23.5±1.6 |
| HR (/min) | 350±20 | 353±17 | 346±18 |
| MAP (mmHg) | 123±3 | 121±11 | 125±10 |
| Blood glucose (mmol/L) | 4.3±0.66 | 4.46±0.61 | 4.41±0.58 |
Changes in EEG in rats with ischemia
The changes in EEG were observed in all animals subjected to ischemia. The equal potential (B)-different from that in EEG (A) taken before ischemia- was observed in EEG 10 to 15 s after the onset of ischemia, so the model of cerebral ischemia was successfully established, as shown in Figure 1.
Figure 1.
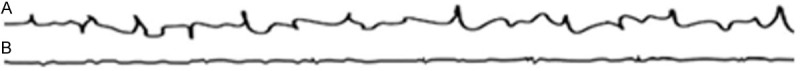
Electroencephalogram of rat before and after cerebral ischemia. A. EEG before cerebral ischemia; B. EEG after cerebral ischemia.
Changes of water content in brain tissues
2 h after procedure, no marked difference was observed in the water content in the IR group, SH group and EA group. Compared with the SH group, the brain water contents in the IR group and EA group were significantly higher 6 h after reperfusion and peaked at 48 h (P < 0.01). 6 h, and 24 h after reperfusion, the EA group had significantly lower blood glucose levels than the IR group (P < 0.01), as shown in Table 2.
Table 2.
Comparison of blood glucose and brain water content in 3 groups at different time points (n=30, x̅±s)
| Blood glucose level (mol/L) | Water content in brain tissues (%) | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Group | 2 h | 6 h | 24 h | 2 h | 6 h | 24 h |
| SH | 4.56±0.55 | 4.54±0.57 | 4.20±0.52 | 77.38±0.20 | 77.42±0.19 | 77.37±0.24 |
| IR | 7.17±0.57* | 8.73±0.47* | 7.23±0.45* | 77.33±0.26 | 79.36±0.27* | 81.20±0.46* |
| EA | 6.27±0.56*,∆ | 7.53±0.36*,∆ | 6.27±0.54*,∆ | 77.29±0.16 | 78.31±0.16*,∆ | 79.23±0.33*,∆ |
Compared with the SH group, P < 0.01;
Compared with the SH group, P < 0.01.
Changes in the blood glucose level in jugular vein
The blood glucose levels in the EA and IR groups were significantly higher than that of the SH group 2 h after reperfusion, which peaked at 6 h and tended to decline until 24 h after reperfusion (P < 0.01). 2 h, 6 h, and 24 h after reperfusion, the EA group had significantly lower blood glucose levels than the IR group (P < 0.01), as shown in Table 2.
Discussion
The principle of treatment of cerebral ischemia-induced injury is to recover blood reperfusion as soon as possible. In some cases, however, reperfusion after ischemia may result in tissue damage and functional disorders, known as ischemia/reperfusion-induced injury. The high blood glucose and cerebral edema are common factors that cause worsening or even death in patients with ischemia/reperfusion-induced injury. Evidence [6] reported that patients with acute craniocerebral injury developed hyperglycemia at different severity, and the prognosis was associated with the high blood glucose level. More and more importance has been attached to the prevention of high blood glucose level and cerebral edema after ischemia reperfusion.
The mechanism for the elevated blood glucose level after ischemia and its change pattern remain unknown, which may be associated with stress and the changes of hormone level [7,8]. In this study, the blood glucose level significantly elevated 2 h after ischemia reperfusion, peaked at 6 h and tended to decline until 24 after reperfusion, but still at a higher level. This might be associated with increased stress hormone secretion and reduced insulin secretion under stress after ischemia reperfusion, which reduced the uptake of glucose. The damaged brain cells also had reduced metabolism and less uptake and utilization of glucose. Eventually, the blood glucose level increased.
We also found that the blood glucose level in the EA group was significantly lower than the IR group, although the level increased too. This suggested that EA preconditioning regulated the blood glucose level after ischemia reperfusion-induced injury, and effectively improved the metabolism of damaged brain cells, and increased the uptake and utilization of glucose in brain cells, which enhanced the recovery of energy metabolism in brain tissues and help recovery of ischemic cerebral injury.
In previous studies relevant to EA, the animals were often administered with acupuncture or EA at awake, which impacted the results because the animals were under stress in addition to treatment. To exclude stress response caused by EA intervention, we anesthetized the animals to avoid the interference of EA on the blood glucose level.
Cerebral edema is basic pathological change after cerebral ischemia reperfusion. It is a complex process involving many factors. In this study, no significant change was observed in the water content 2 h after ischemia reperfusion. But it significantly increased 6 h after reperfusion and peaked at 24 h, demonstrating that the cerebral edema after reperfusion worsened gradually. Aquaporin-4 (AQP4) is one member of the aquaporin family and highly permeable to H2O molecules. It is an important aquaporin to regulate transport of H2O molecules in the brain [9,10]. The development of cerebral edema after reperfusion is closely associated with the expression of AQP4 and its distribution surrounding the blood vessels [11]. Some studies [11,12] showed that the expression of AQP4 and its density surrounding the blood vessels increased at the early stage of (6 h) ischemia reperfusion. But the density substantially declined 24 h after reperfusion while the expression of total proteins remained increased. This directly impacted the elimination of edema and worsened cerebral edema after cerebral ischemia. The hypothesis was demonstrated by our study results related to the changes of water content in the brain 6 h and 24 h after ischemia reperfusion. But the specific mechanism remains to be further studied.
A study [12] demonstrated that the density of AQP4 surrounding the blood vessels decreased 6 h after reperfusion while the density of AQP4 surrounding the blood vessels was significantly higher in the EA group 24 h after reperfusion, indicating that EA intervention slowed the development of early cellular edema to facilitate the elimination of edema in the late stage. In this study, we found that EA markedly lowered the water content and alleviated cerebral edema-although not completely resolved, demonstrating that EA preconditioning significantly reduced the water content and attenuated the cerebral edema after ischemia reperfusion, thereby protecting the brain tissues. Whether EA preconditioning impacts the distribution of AQP4 and what role the AQP4 plays in the protection against ischemia reperfusion-induced injury remain to be further studied.
Some researchers [6] reported that cerebral edema was correlated with increased blood glucose level. In the study, the blood glucose level increased 2 h after reperfusion and the water content in the brain tissue increased 6 h after reperfusion. The augmentation of blood glucose level occurred earlier than the cerebral edema, suggesting that the high blood glucose level promoted the occurrence of cerebral edema, and that the peak cerebral edema at the late stage might also induce increased blood glucose level.
The study showed that EA preconditioning significantly lowered the high blood glucose level and water content in brain tissue in rats after cerebral ischemia to alleviate ischemia reperfusion-induced injury, thereby exhibiting neuroprotection. The preliminary results from the study may thus provide evidence for clinical use of EA therapy. But the mechanism remains to be further studied.
Disclosure of conflict of interest
None.
References
- 1.Zhou F, Guo J, Cheng J, Wu G, Xia Y. Electroacupuncture increased cerebral blood flow and reduced ischemic brain injury: dependence on stimulation intensity and frequency. J Appl Physiol (1985) 2011;111:1877–1887. doi: 10.1152/japplphysiol.00313.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang F, Wu Y, Jia J. Electro-acupuncture can alleviate the cerebral edema of rat after ischemia. Brain Inj. 2011;25:895–900. doi: 10.3109/02699052.2011.581639. [DOI] [PubMed] [Google Scholar]
- 3.Xiong L, Lu Z, Hou L, Zheng H, Zhu Z, Wang Q, Chen S. Pretreatment with repeated electroacupuncture attenuates transient focal cerebral ischemic injury in rats. Chin Med J (Engl) 2003;116:108–111. [PubMed] [Google Scholar]
- 4.Brambrink AM, Koerner IP, Diehl K, Strobel G, Noppens R, Kempski O. The antibiotic erythromycin induces tolerance against transient global cerebral ischemia in rats (pharmacologic preconditioning) Anesthesiology. 2006;104:1208–1215. doi: 10.1097/00000542-200606000-00016. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Q, Cao B, Niu L, Cui X, Yu H, Liu J, Li H, Li W. Effects of permissive hypercapnia on transient global cerebral ischemia-reperfusion injury in rats. Anesthesiology. 2010;112:288–297. doi: 10.1097/ALN.0b013e3181ca8257. [DOI] [PubMed] [Google Scholar]
- 6.Lam AM, Winn HR, Cullen BF, Sundling N. Hyperglycemia and neurological outcome in patients with head injury. J Neurosurg. 1991;75:545–551. doi: 10.3171/jns.1991.75.4.0545. [DOI] [PubMed] [Google Scholar]
- 7.Hamill RW, Woolf PD, McDonald JV, Lee LA, Kelly M. Catecholamines predict outcome in traumatic brain injury. Ann Neurol. 1987;21:438–443. doi: 10.1002/ana.410210504. [DOI] [PubMed] [Google Scholar]
- 8.Pentelenyi T, Kammerer L. Alterations of the serum cortisol and blood glucose in brain-injured patients. Injury. 1984;15:397–402. doi: 10.1016/0020-1383(84)90205-5. [DOI] [PubMed] [Google Scholar]
- 9.Zelenina M, Zelenin S, Aperia A. Water channels (aquaporins) and their role for postnatal adaptation. Pediatr Res. 2005;57:47r–53r. doi: 10.1203/01.PDR.0000159572.79074.0B. [DOI] [PubMed] [Google Scholar]
- 10.Manley GT, Binder DK, Papadopoulos MC, Verkman AS. New insights into water transport and edema in the central nervous system from phenotype analysis of aquaporin-4 null mice. Neuroscience. 2004;129:983–991. doi: 10.1016/j.neuroscience.2004.06.088. [DOI] [PubMed] [Google Scholar]
- 11.Ribeiro Mde C, Hirt L, Bogousslavsky J, Regli L, Badaut J. Time course of aquaporin expression after transient focal cerebral ischemia in mice. J Neurosci Res. 2006;83:1231–1240. doi: 10.1002/jnr.20819. [DOI] [PubMed] [Google Scholar]
- 12.Ren QX, Yang F, Peng YJ, Guo JC. Electroacupuncture modulates the expression and perivascular distribution of aquaporin 4 (AQP4) in rats during cerebral ischemia/reperfusion. Fudan Uni J (Med Sci) 2012;39:594–599. [Google Scholar]


