Abstract
Primary malignant melanoma of the esophagus (PMME) is a rare disease, comprising 0.1-0.2% of all malignant esophageal neoplasms. The most common symptoms include progressive dysphagia, chest and back pain, choking feeling and weight loss. PMME cannot be definitely diagnosed from clinical symptoms or CT examination, but can be confirmed by histological examination or a pathological examination. Immunohistochemical examination with positive results of S-100 protein and human melanoma black 45 (HMB45) makes a definitive diagnosis. Esophagectomy is the standard treatment for localized PMME. But the prognosis is poor. Inoperableness, metastases and insensitiveness of radiotherapy and chemotherapy in advanced tumors have led to poor prognosis. Here, we report a case of a 61-year-old male with progressive dysphagia for 1 month. After barium X-ray test, chest and abdomen computed tomography examination, upper gastrointestinal endoscopy and biopsy, the patient accepted esophagectomy, then the pathologic and immunohistochemical examination conformed the diagnosis of PMME.
Keywords: Esophageal cancer, esophageal surgery, esophagus, surgery, outcomes
Introduction
Primary malignant melanoma of the esophagus is a highly aggressive disease representing 0.1% to 0.2% of all primary esophageal cancers [1]. Most patients are in their sixth and seventh decades, with a 2.02:1 male-to-female ratio. PMME has a poor prognosis. The mean survival time after operation is 10-14 months. Until now, what we have known about PMME is based primarily on single case reports.
Case presentation
A 61-year-old man with progressive dysphagia and loss of 2 kg of body weight in 1 month came to our institute. He had never undergone surgery due to malignancy previously. He was treated as gastritis without any symptomatic improvement at a private clinic. He denied retrosternal or epigastric pain or habitual consumption of cigarettes, alcohol. Physical examination and blood test results showed no abnormalities. Repeat physical examination found no abnormal pigmentations of the skin or mucosa. Fiberoptic esophagoscopy showed a pitchy rigid esophageal lesion located 30-35 cm from the incisors, which appeared as a protrusion of the esophagus wall (Figure 1). The pathology report of the biopsy specimen was malignant melanoma. Subsequent immunohistology revealed that tumor cells are strongly positive for the melanoma specific antigen HMB-45 and for S-100 protein (Figure 2). Chest computerized tomogram showed the mass to be 7.5 cm in length at the esophagus wall of the lower segment of esophagus with evidence of lymph node enlargement in the paraesophageal and carinal lymph (Figure 3). Pulmonary function tests, whole body bone scan with TC-99 m, and a computerized brain tomogram were all unremarkable, and therefore the pre-operative clinical stage was classified as III (cT4N1M0).
Figure 1.
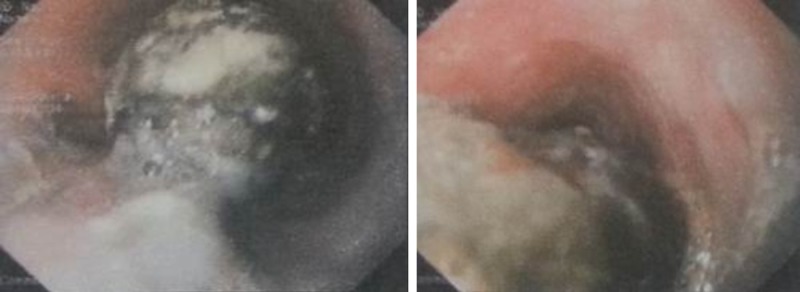
A polypoid mass covered by mucosa in the esophagus wall.
Figure 2.
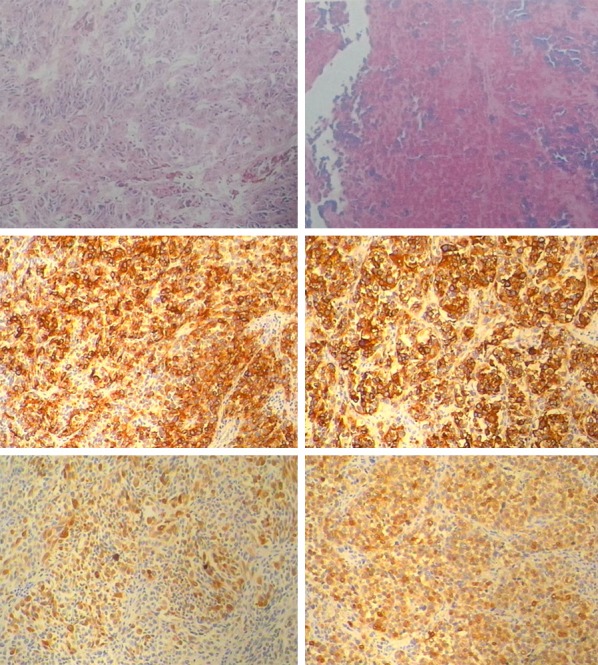
Tumor cells arranged in solid nests. Intracellular melanin granules were visible in the submucosa. HBM-45: The positive reaction (brown cytoplasmic reaction) supports the diagnosis of malignant melanoma. S-100: The tumor cells are immunoreactive with S-100 protein.
Figure 3.
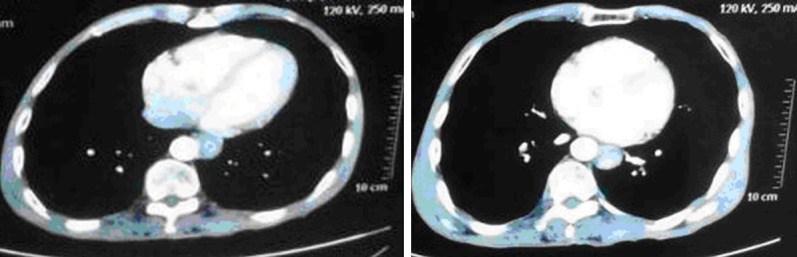
CT showed the thickness of the lower esophagus wall.
The patient underwent a subtotal esophagectomy and cervical esophagogastric anastomosis via a left thoracotomy, laparotomy and cervical incision. Reconstruction was performed by pulling the gastric tube up through a retro-sternal route. The cervical esophagogastric anastomosis was performed by a standard hand-sewn technique. There was no evidence of mediastinal lymph node enlargement and the post-operative course was uneventful. The tumor was 3.0 cm×2.5 cm×2.0 cm in size, polypoid and pigmented from the distal esophagus. Immunohistochemically, the tumor was positive for S-100 protein and HMB45. So a definitive diagnosis of PMME was made.The tumor cells invaded the submucosa. One of 15 lymph nodes at the mediastinal lymph was infiltrated by tumor cells. The final diagnosis was primary malignant melanoma of the esophagus, stage III: T2N1M0, according to the TMN classification of AJCC. The patient is still alive without disease progression 6 months after surgery.
Comment
Skin is the most common site for primary melanoma. However, melanoma can appear in many sites of human body, such as oronasal mucosa and anorectal junction where melanin cell reside [2]. The common symptoms of primary malignant melanoma of the esophagus (PMME) are dysphagia, heartburn, retrosternal pain, weight loss, and regurgitation, without specific feature compared with the clinical symptoms of esophageal carcinoma. Immunohistochemical examination with positive results for HMB-45 and S100 protein makes definite diagnosis of malignant melanoma. Multidisciplinary treatment such as radical surgery with chemotherapy, chemoradiotherapy, endocrinotherapy, immunotherapy, is in clinic use, whereas cases of long-term survival have seldom been reported. For the early cases, radical surgery is the optimum choice.
Allen and Spitz [3] originally defined the diagnostic criteria for primary melanoma, which includes: (1) a typical histological pattern of melanoma, with melanin granules inside the tumor cells, and (2) origin in an area of junctional activity in the squamous epithelium. Melanocytosis [4], which also presents as a black or gray appearance in the endoscopic view, is indicative of the lesion being the primary lesion rather than a secondary in cases of esophagus melanoma. In the Wang study [5], melanocytosis was detected in all cases, justifying the view that they were all primary lesions.
Sanchez et al [6] found that primary malignant melanoma of the esophagus occurred mostly (>90%) in the mid and lower third of esophagus. The locations of the tumor tend to be at the middle to lower thoracic esophagus.
The incidence of metastasis to the regional lymph nodes is high at 40-80% at the initial diagnosis. To diagnose metastatic regions, computed tomography (CT) is currently widely used. From the study [7] of the 38 patients with lymph node metastases from melanoma, FDG-PET detected 100% of metastatic sites when the size of the tumor was larger than 10 mm, 83% when 6-10 mm and 23% when less than 5 mm.
If endoscopic ultrasound had been used routinely in each patient, the accuracy may have been further improved. Meta-analyses [8] performed to examine the utility of sonography, CT, and positron emission tomography/CT for the staging and surveillance of patients with melanoma based on 10,528 patients between 1990 and 2009 found that positron emission tomography/CT was the most accurate modality for detection of metastases, with both a sensitivity and specificity of 95%. So the superior modality for staging and detecting distant metastases was PET-CT.
Subtotal esophagectomy is the optimum choice for the early cases. Despite multimodal therapy, such as radical surgery with chemotherapy, chemoradiotherapy, endocrinotherapy, immunotherapy or other adjuvant therapy was performed, cases of long-term survival have seldom been reported.
Tumor size and location, metastases, age and comorbidities of the patient affect the treatment modality. The only therapy option that influences survival is surgical treatment, whereas other therapies are palliative. The predominant death cause of PMME was the metastasis [2]. Shaohua Wang [5] showed that lymph node metastasis was the independent predictive factor for postoperative survival.
We have reported an extremely rare case of PMME by positive results for HMB-45 and S100 protein. Six months after surgery, the patient is alive without tumor recurrence. We hope the standard of diagnosis and treatment will be established in the future.
Disclosure of conflict of interest
None.
References
- 1.Volpin E, Sauvanet A, Couvelard A, Belghiti J. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus. 2002;15:244–249. doi: 10.1046/j.1442-2050.2002.00237.x. [DOI] [PubMed] [Google Scholar]
- 2.Li B, Lei W, Shao K, Zhang C, Chen Z, Shi S, He J. Characteristics and prognosis of primary Malignant melanoma of the esophagus. Melanoma Res. 2007;17:239–242. doi: 10.1097/CMR.0b013e3281c4a079. [DOI] [PubMed] [Google Scholar]
- 3.Allen AC, Spitz S. Malignant melanoma; a clinicopathological analysis of the criteria for diagnosis and prognosis. Cancer. 1953;6:1–45. doi: 10.1002/1097-0142(195301)6:1<1::aid-cncr2820060102>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki H, Nakanishi Y, Taniguchi H, Shimoda T, Yamaguchi H, Igaki H, Tachimori Y, Kato H. Two cases of early-stage esophageal malignant melanoma with long-term survival. Pathol Int. 2008;58:432–5. doi: 10.1111/j.1440-1827.2008.02249.x. [DOI] [PubMed] [Google Scholar]
- 5.Wang S, Tachimori Y, Hokamura N, Igaki H, Kishino T, Kushima R. Diagnosis and surgical outcomes for primary malignant melanoma of the esophagus: a single-center experience. Ann Thorac Surg. 2013;96:1002–7. doi: 10.1016/j.athoracsur.2013.04.072. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez AA, Wu TT, Prieto VG, Rashid A, Hamilton SR, Wang H. Comparison of primary and metastatic malignant melanoma of the esophagus: clinicopathologic review of 10 cases. Arch Pathol Lab Med. 2008;132:1623–1629. doi: 10.5858/2008-132-1623-COPAMM. [DOI] [PubMed] [Google Scholar]
- 7.Crippa F, Leutner M, Belli F, Gallino F, Greco M, Pilotti S, Cascinelli N, Bombardieri E. Which kinds of lymph node metastases can FDG PET detect? A clinical study in melanoma. J Nucl Med. 2000;41:1491–4. [PubMed] [Google Scholar]
- 8.Xing Y, Bronstein Y, Ross MI, Askew RL, Lee JE, Gershenwald JE, Royal R, Cormier JN. Contemporary diagnostic imaging modalities for the staging and surveillance of melanoma patients: a meta-analysis. J Natl Cancer Inst. 2011;103:129–42. doi: 10.1093/jnci/djq455. [DOI] [PMC free article] [PubMed] [Google Scholar]


