Abstract
Broad associations between trauma exposure (TE) and Axis I psychopathology have been noted in the literature. However, it is not clear if TE is directly associated with Axis I disorders or if the relationship is better accounted for by familial factors (i.e., early environment and/or genetic factors). The current investigation used the co-twin control method in a large sample of adult twin pairs from the Norwegian Twin Registry (N = 2,776), including 449 twin pairs discordant for DSM-IV Criterion A TE. History of TE and Axis I psychopathology was assessed using DSM-IV based clinical interview. Results suggested that TE was significantly associated with greater likelihood of meeting criteria for major depression, dysthymia, anxiety, substance abuse, eating disorders, and somatization disorder in the general population (odds ratios [OR] ranging from 1.33 to 2.21). Among twins discordant for TE, results suggested that TE may exert a direct influence on major depression, dysthymia, anxiety, substance abuse, eating disorders, and somatization disorder. Shared familial effects may also account for at least some of the relationship between TE and major depression. TE may play an important role in the development of a wide range of Axis I psychopathology above and beyond familial factors. Research and clinical implications are discussed.
Keywords: lifetime trauma exposure, co-twin control design, psychopathology, psychiatric genetics
Estimates indicate that 39-82.5% of adults have a lifetime history of trauma exposure (TE; e.g., physical/sexual assault, accidental injury, sudden death of a loved one, combat exposure, etc.) in Western European countries (Darves-Bornoz et al., 2008) and the United States (Breslau, Davis, Andreski, & Peterson, 1991; Breslau, Wilcox, Storr, Lucia, & Anthony, 2004; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Although many individuals are resilient to such events, a significant proportion of those with TE develop posttraumatic stress disorder (PTSD) and other Axis I psychopathology such as panic disorder, major depressive disorder, anxiety disorders, and SUD across diverse populations (Amstadter et al., 2009; Archambeau et al., 2010; Kaltman, Green, Mete, Shara, & Miranda, 2010; Kilpatrick et al., 2003; Pietrzak, Goldstein, Southwick, & Grant, 2011), leading to speculation of a causal relationship between TE and Axis I psychopathology (Heim & Nemeroff, 2001). However, limited empirical tests of an underlying causal model have been conducted.
Three lines of research have led to the commonly accepted causal assumption of the relationship between TE and Axis I psychopathology. First, studies consistently find associations between rates of TE and Axis I psychopathology. For example, epidemiological studies have found higher rates of Axis I psychopathology, including major depression, dysthymia, generalized anxiety disorders, panic disorder with and without agoraphobia, social phobia, specific phobia, and SUD, in individuals with vs. without lifetime TE, (Amstadter, Aggen, Knudsen, Reichborn-Kjennerud, & Kendler, 2013; Kilpatrick et al., 2003; Pietrzak et al., 2011), as well as high rates of TE in clinical samples of individuals with Axis I psychopathology, including somatoform disorders (van Dijke et al., 2012). Retrospective studies on the long-term effects of childhood abuse have found significant relationships with Axis 1 disorders lasting into adulthood, including mood, anxiety, substance use, and eating disorders (Brewerton, 2007 Hovens et al., 2012; Kendall-Tackett, 2002; Neumann, Houskamp, Pollack, & Briere, 1996). Second, prospective studies have found onset of Axis I disorders frequently occurred after TE, providing evidence for temporal precedence (McFarlane & Van Hooff, 2009). Third, studies have found that higher magnitude of trauma, as indicated by directly-experienced TE (Amstadter et al., 2009; Pietrzak et al., 2011), assaultive TE (Breslau et al., 1991), life-threat or injury (Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993), or history of multiple traumas (Breslau, Chilcoat, Kessler, & Davis, 1999), is associated with greater incidence of PTSD and comorbid Axis I disorders, suggesting a potential dose-response relationship between TE and psychiatric outcomes. Unfortunately, these studies are not able to discern the effects of TE from the potentially confounding factors of genetic or shared environmental influences (e.g., economic disadvantage, familial discord) that may increase risk for both TE and psychopathology. Thus more research is needed to examine the relationship more closely to determine if the association between TE and Axis I psychopathology is better accounted for by confounding variables.
Indeed, research has suggested that familial factors may account for the observed relationship between TE and Axis 1 psychopathology. Data from twin studies have reported moderate heritability of some types of traumatic events in non-civilian and civilian populations (Lyons et al., 1993; Stein, Jang, Taylor, Vernon, & Livesley, 2002). A recent report from the dataset utilized in the current investigation suggests that familial factors play an important role in liability for both TE and subsequent PTSD symptoms, with a modest transmission between the TE and PTSD symptoms (Amstadter, Aggen, Knudsen, Reichborn-Kjennerud, & Kendler, 2012). There is also evidence for a shared genetic influence on exposure to stressful life events and major depressive disorder (MDD) and SUD (Kendler, Karkowski, & Prescott, 1999; Kendler & Prescott, 2006). Finally, there appears to be a common genetic influence on exposure to some forms of TE (i.e., rape, childhood abuse, and physical assault), PTSD, and MDD (Sartor et al., 2012). Additional research specifically targeting the relationship between TE and a range of Axis I disorders is needed to clarify whether TE itself or common genetic/environmental vulnerability is responsible for increased odds of developing such conditions (Kremen, Koenen, Afari, & Lyons, 2012).
Analysis of samples consisting of twins who are discordant for TE may provide some insight into the potentially causal role of TE in the development of Axis I pathology, by statistically accounting for both genetic and environmental factors (e.g., economic adversity, family discord) shared by the twins (Kendler & Campbell, 2009). Studies employing the discordant twin methodology provide preliminary evidence that specific forms of TE, such as childhood sexual abuse (Dinwiddie et al., 2000; Kendler et al., 2000; Nelson et al., 2002) and combat exposure (Koenen et al., 2003), may play a causal role in the development of Axis I disorders. However, more genetically informed research is needed to examine the relationship between a broader range of traumatic events and Axis I psychopathology in population-based studies of twins.
Aims of the Study
The current study used a co-twin control method to determine the extent to which the relationships between TE and Axis I diagnoses is best explained by a TE-causal model, or if familial factors account for some or all of the relationship between TE and Axis I psychopathology in a large population-based sample of adult Norwegian twins obtained from the Norwegian Twin Registry (NTR). The first aim of the current study was to detect and quantify an association between TE and Axis I diagnostic status (e.g., present, subthreshold, absent). The second aim of the study was to attempt to clarify the source of any significant associations between TE and Axis I psychopathology. Specifically, we aimed to determine whether the TE-Axis I relationship is: (a) entirely accounted for by TE, (b) partly accounted for by TE and partly due to familial factors, or (c) accounted for entirely by familial factors. Given the preponderance of evidence from other methodologies demonstrating both familial and direct TE effects on a range of psychopathologies, we hypothesized that the effect of TE would be partially mediated by shared familial factors.
Method
Participants
The Norwegian National Medical Birth Registry, established on January 1, 1967, receives mandatory notification of all live births. The current investigation utilized the twin group included in the NTR who completed questionnaire studies in 1992 (including twins born between 1967-1974) and again in 1998 (including twins born between 1967-1979). A complete description of recruitment and assessment procedures can be found in Tambs et al. (2009). Approval was received from The Norwegian Data Inspectorate and the Regional Ethical Committee, and all participants provided written informed consent. The current investigation included all participants who completed the interview study and had complete data on Axis I disorders and TE (N = 2,776), as well as a subset of the general sample (n = 898) comprised of the twin pairs (449 pairs, 45% monozygotic [MZ]) that were discordant for DSM-IV Criterion A TE. Participants in the general sample (63.5% women) had a mean age of 28.2 (SD = 3.9) at the time of the interview and reported having approximately 14.9 years of education (SD = 2.6).
Assessment
Axis I psychopathology
Lifetime Axis I disorders were assessed using a Norwegian computerized version of the Munich-Composite International Diagnostic Interview (M-CIDI; Wittchen & Pfister, 1997). The CIDI is a comprehensive structured diagnostic interview assessing DSM-IV Axis I disorders (American Psychiatric Association, 1994), and has been shown to have good test-retest and inter-rater reliability (Wittchen, 1994; Wittchen, Lachner, Wunderlich, & Pfister, 1998). Interviews were conducted by clinical psychology students at the end of their 6-year training course (with least 6 months of clinical practice), and psychiatric nurses with years of clinical experience. They received a standardized training program by professionals certified by the World Health Organization with extensive previous experience with the instruments. Most interviews were conducted face-to-face during the period from June of 1999 to May of 2004. For practical reasons, 231 interviews (8.3%) were conducted by phone. Each twin in a pair was interviewed by a different interviewer.
Eleven of the assessed Axis I disorders were included in this study: major depressive disorder, dysthymia, panic disorder, agoraphobia, specific phobia, social phobia, generalized anxiety disorder, eating disorders, somatoform disorder, alcohol abuse or dependence, and illicit drug abuse or dependence. Although it would be desirable to analyze each disorder separately, anxiety disorders were combined into one category, and SUD were collapsed into one category due to insufficient power to conduct separate tests. This approach is consistent with past twin studies, indicating that there is common genetic and environmental liability within anxiety disorders (Hettema, Prescott, Myers, Neale, & Kendler, 2005), and SUD (Kendler et al., 2001; Kendler, Prescott, Myers, & Neale, 2003). Furthermore, previous research has demonstrated non-specific effects of life adversity on the development of anxiety disorders in general, rather than on the development of specific anxiety disorders (Hettema et al., 2005; Safren, Gershuny, Marzol, Otto, & Pollack, 2002), thus there is theoretical and empirical justification for the combination of these disorders into diagnostic classes.
Diagnoses were classified as: 0 = no diagnosis, 1 = sub-threshold, 2 = diagnosis. For the aggregate variables, participants were assigned a diagnostic value based on the most severe rating within that category (e.g. a diagnosis of any disorder in that category was assigned a score of 2). Due to the use of stem questions for major depressive disorder, sub-threshold data were not available, and the disorder was coded dichotomously (0 = no diagnosis, 1 = diagnosis). With regard to TE, participants were asked in the PTSD module of the M-CIDI if they had personally experienced any of the following DSM-IV A1 traumatic events: (a) a terrible experience at war, (b) serious physical threat (with a weapon), (c) rape, (d) sexual abuse as a child, (e) a natural catastrophe, (f) a serious accident, (g) being imprisoned, taken hostage, or kidnapped, or (h) another event. They were also asked if they witnessed any of the listed events happening to another person. Participants were coded as either 0=not TE or 1= TE if they endorsed both DSM-IV A1 and A2 (i.e., peritraumatic fear, helplessness, or horror) criteria, which form Criterion A for a diagnosis of PTSD. Twenty-seven percent (n = 736) of the total sample endorsed a traumatic event that met DSM-IV Criterion A for PTSD. As reported in Amstadter et al. (2012), among individuals meeting criteria for TE, 26.3% reported their worst trauma as being physical threat to oneself, 16.8% an accident, 16.6% an “other” traumatic event, 14.2% childhood sexual assault, 11.7% a rape, 10.6% witnessing a traumatic event, 1.3% a combat-related incident, 1.3% being held hostage, and 1.1% a natural disaster.
Data Analysis Plan
The relationship between TE and Axis I pathology was examined using a co-twin control method utilizing logistic regression in: (a) the total twin sample, and (b) a sample of twins discordant for TE. MZ and dizygotic (DZ) twins were combined due to low power1. Combining the twin pairs allows for a test of a model in which the relationships between TE and Axis I disorders are accounted for entirely by TE compared to a familial model of TE and Axis I disorders but does not allow for discriminating between genetic and shared environmental effects accounting for overarching familial effects. The co-twin control method uses conditional logistic regression in which the non-exposed twin serves as a matched control for the TE-twin, and thus controls for all factors that are shared by each twin pair that would otherwise be impossible to measure and control. This includes genetic (100% shared for MZ, and approximately 50% for DZ), and shared environmental variables (e.g., socio-cultural factors, child rearing environment, parenting practices). Thus, observed differences between discordant twins are assumed to be due to non-shared effects, such as TE.
First, the broad association between TE and Axis I psychopathology in the total twin sample was examined using a series of logistic regressions2 using SPSS version 19 with diagnostic status (MDD, dysthymia, anxiety disorders, SUD, eating disorders, and somatization disorder) entered as the predictor variable in separate regression models, and TE (coded 0 = no trauma history, 1 = trauma history) entered as the criterion variable. The use of TE as the outcome variable in the logistic regression identifies which variables are associated with case (TE) versus control status to determine which psychiatric disorders are associated with TE, controlling for measured and unmeasured shared variables. Age at the time of interview, sex, and years of education were included as covariates due to their zero-order relationship with predictor and outcome variables (see Table 1). Second, conditional logistic regressions were conducted among the discordant twin pairs, which allows for matching the trauma-exposed twin with their non-exposed co-twin. The odds ratios (ORs) for each sample (i.e., total sample and discordant twin sub-sample) were compared for each of the Axis I diagnostic categories.
Table 1.
Descriptive Statistics and Zero-Order Correlations
| Variablea | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Mean (SD) or % |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex (% female) | 63.5% | |||||||||
| 2. Age (years) | -.02 | 28.2 (3.9) | ||||||||
| 3. Education (years) | -.04* | .08** | 14.9 (2.6) | |||||||
| 4. Trauma Exposure | -.09** | .02 | -.04* | 26.5% | ||||||
| 5. MDD | .07** | .04 | -.03 | .13** | 14.1% | |||||
| 6. Dysthymia | .04* | -.02 | -.14** | .06** | .16** | 2.4% = 1, 1.7% = 2 |
||||
| 7. Anxiety Disorders | .22** | -.01 | -.15** | .12** | .27** | .17** | 28.1% = 1, 24.1% = 2 |
|||
| 8. SUD | -.20** | -.18** | -.06** | .10** | .10** | .06** | .11** | 20.8% = 1, 10.3% = 2 |
||
| 9. Eating Disorder | .20** | .02 | -.03 | .09** | .13** | .08** | .19** | .06** | 12.4% = 1, 3.6% = 2 |
|
| 10. Somatoform Disorder | .20** | -.01 | -.14** | .13** | .17** | .19** | .27** | .03 | .19** | 13.8% = 1, 7.5% = 2 |
Note:
p < .05,
p < .01;
Sex coded 1 = male, 2 = female; Trauma Exposure coded 0 = no history of Criterion A trauma, 1 = history of Criterion A trauma endorsed; MDD (major depressive disorder) coded dichotomously (0 = no diagnosis, 1 = diagnosis); Remaining diagnoses classified as 0 = not present, 1 = sub-threshold, 2 = threshold. SUD=substance use disorders
Comparisons of the strength of association between the nonshared factor (TE) and psychiatric variables in the total sample and discordant twin sample provides some evidence about whether a TE-effects, shared effects, or familial effects model is supported (Kendler et al., 1993). If TE exerts a direct influence on Axis 1 psychopathology, the risk of psychopathology will be the same in the total sample as in the discordant twins. That is, accounting for shared familial factors does not reduce the association between TE and psychopathology. If the relationship between Axis I pathology is partially mediated by shared familial factors (either genetic or environmental) the magnitude of the relationship between TE and Axis I pathology should be greater in the total sample compared to the discordant twin pairs, but the ORs in both groups would be significantly greater than one. In this case, the association between TE and Axis I psychopathology is reduced, yet still significant, when accounting for shared familial factors. If shared familial (i.e., genetic and/or shared environmental) factors entirely account for the association between TE and Axis I disorders (i.e., the shared familial factor predisposes the individual to both TE and Axis I pathology), the association between TE and Axis I pathology in the discordant twin sample would no longer be apparent. This would suggest that when accounting for familial effects, TE would no longer be associated with psychopathology.
Results
Descriptive Statistics and Zero-Order Correlations (General Sample)
Table 1 displays descriptive statistics and zero-order correlations for demographic and key study variables. Sex was significantly related to years of education and TE, with men being more likely to report more years of education and endorsement of a Criterion A event. Women were more likely to endorse symptoms of all disorders, with the exception of SUD, which were more frequently endorsed among men. Age was significantly associated with substance use symptom endorsement, with younger individuals reporting greater symptom levels. Fewer years of education was related to greater symptom endorsement for all disorders except for major depressive disorder and eating disorders. TE was significantly yet modestly related to greater symptom endorsement for all disorders (rs range: .06-.13, p’s < .01).
TE and Axis I Psychopathology
See Table 2 for ORs and 95% confidence intervals (CI) for the total and discordant twin samples. In the total sample, a history of TE was significantly related to greater likelihood of meeting clinical levels of MDD, given the covariates of age, sex, and years of education (OR = 2.21, p<.01; CI = 1.76 – 2.77). To examine the potential source of these associations, we compared the observed ORs within the total sample to those obtained among twin pairs discordant for TE (see Figure 1). For MDD, the OR for discordant twins dropped to 1.95 (CI = 1.12 – 3.39). The pattern of findings for MDD, although not statistically discernible due to large confidence intervals, appear to suggest that shared familial factors account for some of the observed difference between TE and MDD, given that the point estimate between TE and MDD in the discordant twin sample is lower than that observed in the total sample, with the CIs in the twin sample excluding unity.
Table 2.
Trauma Exposure Predicting Axis I Disorders: Odds Ratios and 95% Confidence Intervals by Sample
| Total Sample | Discordant Twins | |
|---|---|---|
| Major Depressiona | 2.21** (1.76 – 2.77) | 1.95* (1.12 – 3.39) |
| Dysthymia | 1.51* (1.17 – 1.96) | 1.52 (.86 – 2.67) |
| Anxiety Disorders | 1.47** (1.32 – 1.64) | 1.46** (1.13– 1.88) |
| Substance Use Disorders | 1.33** (1.18 – 1.51) | 1.30 (.95 – 1.77) |
| Eating Disorder | 1.61** (1.36 – 1.91) | 1.65* (1.07– 2.56) |
| Somatization Disorder | 1.67** (1.47 – 1.94) | 1.56** (1.14 – 2.13) |
Note:
p < .05,
p < .01;
Major Depression coded dichotomously (0, 1), Remaining diagnoses classified as 0 = not present, 1 = sub-threshold, 2 = threshold; Anxiety Disorders include Generalized Anxiety Disorder, Panic Disorder, Agoraphobia, Specific Phobia, and Social Phobia; Substance Use Disorders include Alcohol and Drug Use Disorders.
Figure 1.
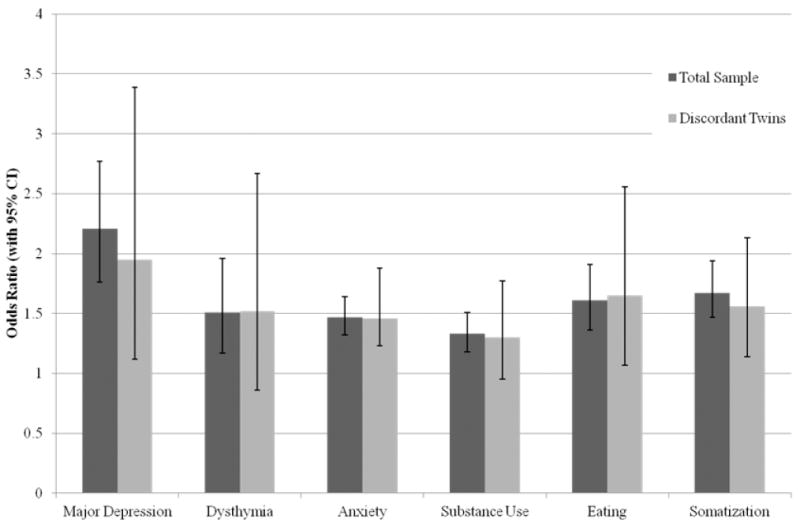
Trauma exposure (TE) and Axis I psychopathology in the total sample and discordant twin sample.
In the general population sample, TE was related to increased likelihood of meeting subclinical or clinical levels of dysthymia, anxiety disorders, SUD, eating disorders, and somatization disorder, above and beyond the covariates, with all ORs significantly greater than 1 (see Table 2). When examining the potential source of these associations (see Figure 1), the findings are consistent with a direct influence model of TE, with ORs and associated 95% CIs being consistent between the general population and twin samples. Comparison of the extreme points of the confidence interval ranges for anxiety, eating disorders, and somatization in the two samples suggests that in the current population, even if familial factors do account for some portion of the relationship between TE and anxiety disorders, it is likely quite small (i.e., at the very least, there is support for a partly meditated model). For dysthymia and SUD in discordant twins, the lower bound of the CI included 1; therefore, alternative shared-familial models cannot be ruled out for these disorders.
Discussion
The current study, to our knowledge, is the first co-twin epidemiologic investigation of the association between lifetime TE and Axis I psychopathology in a population-based sample of twins. The first aim of this investigation was to document the relationship between TE and Axis I disorders in a large population-based sample. As expected, we found that TE was associated with elevated odds of meeting subclinical or full diagnostic criteria for all forms of Axis I psychopathology. The strongest relationship between TE and psychopathology was found for MDD. The relationship between TE and SUD was the weakest relationship. These results are broadly consistent with previous research demonstrating associations between TE and many Axis I disorders, such as MDD, anxiety disorders, SUD, eating disorders (Brewerton, 2007; Brown, Schrag, & Trimble, 2005; Kilpatrick et al., 2003; Pietrzak et al., 2011).
The second, and we believe more interesting, aim of this paper was to examined the specific relationship between TE and psychopathology using the co-twin control design to determine if the variance accounted for by TE might be better explained by confounding genetic or familial factors that influence both TE and Axis I pathology. With the exception of MDD, discussed below, point estimates and their associated confidence intervals for dysthymia, anxiety disorders, SUD, eating disorder, and somatization disorder overlapped with the general sample. This pattern of results allows for a tentative interpretation that the observed relationship between TE and these Axis I disorders is likely due to a direct influence of TE as opposed to confounding genetic or early environmental factors. Our study, which examined lifetime TE broadly, provides an extension of previous co-twin studies that have found support for the direct influence of TE for childhood sexual abuse (Dinwiddie et al., 2000; Nelson et al., 2002) and combat exposure (Gilbertson et al., 2010; Koenen et al., 2003) on Axis I psychopathology.
These results do not suggest that genetic and familial factors are not significant factors in the development of Axis I psychopathology. There is ample evidence that genetic and environmental factors do indeed confer risk for the development of psychopathology (Hettema, Neale, & Kendler, 2001; Hettema et al., 2005; Kendler et al., 2000; Kendler et al., 2003; Safren et al., 2002). Undoubtedly, the etiology of these psychiatric conditions is complex. Results of the current study suggest that TE is one such unique environmental factor that confers significant risk for the development of these conditions.
One notable exception to the over-arching pattern of findings of a direct influence of TE and the other Axis I disorders was MDD. As previously noted, the strongest association in the general population was seen between TE and major depressive disorder. When accounting for familial factors, the relationship between TE and MDD was slightly reduced, suggesting that a small portion of the relationship between TE and MDD may be due to the overlap in familial factors that predispose individuals to both TE and MDD. Cross-sectional studies on TE and MDD are plentiful (Kilpatrick et al., 2003; Pietrzak et al., 2011) and these findings suggest that part of this relationship is likely due to factors that are unmeasured in most of these studies (i.e., familial factors). Indeed previous research has found that although stressful life events are associated with subsequent onset of MDD (Sartor et al., 2012), individuals with MDD also tend to self-select stressful environments (Kendler et al., 1999). It must be stressed that alternative models of directionality cannot be ruled out due to the large, over-lapping confidence intervals between the two samples.
Limitations and Future Directions
The results of this study should be considered in light of the following limitations. The co-twin control method is not without its limitations. The use of discordant twins controls for all variables shared by the twins to examine the effect of non-shared variables - ostensibly TE in this case. Although TE is a systematic difference between the twins, we cannot rule out the potential for an unmeasured non-shared confound that contributes to both TE and psychopathology that could bias the results (Frisell, Öberg, Kuja-Halkola, & Sjölander, 2012). However, the inability to control for unmeasured variables is a limitation in all research, and we believe the co-twin control method represents a powerful method by controlling for those unmeasured variables that are shared by twins.
Alternative models exist for examining the genetic, shared environmental, and unique environmental influences (De Moor, Boomsma, Stubbe, Willemsen, & de Geus, 2008; Neale & Cardon, 1992). However, these methods are often best suited for continuous outcome data, and our outcome data, TE, was dichotomous (i.e., exposed vs non-exposed). Furthermore, due to low power we had to combine MZ and DZ twins in our analyses. As a result we were unable to examine additive genetic effects or determine the extent to which familial effects were due to genetic or shared environment. Following, we were unable to conclude if shared genes or shared environment were likely accounting for the portion of the TE-depression relationship best explained by familial factors. These alternative covariance models, such as Cholesky decomposition and common/independent pathways models, are random-effects models which aim to partition variance into genetic, shared, and unique components. These models are computationally demanding and we were not sufficiently powered for these models. The co-twin control method, on the other hand, is a fixed-effects case-control model that aims to control for, rather than estimate, the effects of familial factors. With this method, discordant twins are identified and the case-control variable (i.e., TE) is used as the outcome in a conditional logistic regression that examines the variance within twin pairs to discriminate between direct and indirect effects of TE (Kendler et al, 1993). There is clearly a need for more nuanced TE assessment in large genetically informed epidemiological samples to provide sufficient power to examine the convergence of evidence from multiple methodologies, including co-twin and covariance models.
The use of binary (e.g., trauma exposed vs. non-exposed) and broad categorical data (e.g., diagnostic categories) increases the risk of measurement error, which can lead to biased results in the co-twin design (Frisell et al., 2012), as is true for any statistical procedure. TE was measured with a checklist in which participants indicated whether or not they had experienced each trauma class. We did not have data on the severity or number of occurrences of each class of trauma (e.g., accident, domestic violence, sexual assault). Thus, we were not able to create a meaningful continuous TE variable. In order to be classified as TE, participants must meet the DSM-IV A2 criteria of peritraumatic fear, helplessness, or horror. One possibility is preexisting nonshared factors may influence the perception of, or response to, the traumatic event that influenced whether the TE twin experienced and/or reported these peritraumatic emotions when the co-twin did not. Although the predictive utility of A2 has been heavily debated (Bedard-Gilligan & Zoellner, 2008; Brewin, Andrews, & Rose, 2000; Kubany, Ralston, & Hill, 2010), little research has been conducted exploring factors that predict endorsement of A2 criteria in response to a traumatic event, and this represents an area of needed research. The use of structured interviews with trained clinicians in the current study helps to reduce concern of measurement error, however future research should consider the use of continuous psychiatric data such as symptom count, severity scores, or research domain criteria (Insel et al., 2010).
In light of the relatively low base rates of the individual disorders in the discordant twin pairs, we combined several disorders into diagnostic categories rather than examining each disorder separately. Despite these attempts to increase the cell sizes and improve power, we still had large confidence intervals, making it difficult to make conclusive statements about the nature of the relationship between TE and the disorders examined. Future studies will be needed that include large sample sizes of individuals with targeted disorders.
The assessments were based on retrospective self-reports and are affected by recall and reporting biases. However, research has suggested that recall of potentially traumatic events are less biased than non-traumatic events (Lalande & Bonanno, 2011). Furthermore, the temporal ordering of TE and psychopathology onset was not assessed, thus we cannot be certain that psychopathology onset occurred after TE. However, our findings are consistent with previous research, including co-twin control designs, that has also found support for a direct relationship between retrospective reports of child maltreatment and Axis I psychopathology (Dinwiddie et al., 2000; Kendall-Tackett, 2002; Kendler, Kuhn, & Prescott, 2004; Nelson et al., 2002). However, prospective cohort studies are needed to examine the temporal effects of childhood trauma, Axis I psychopathology, and familial factors.
Given the relatively low base rate of TE in the sample we were unable to examine specific trauma types in association with the phenotypes. Lastly, the extent to which this sample generalizes to other countries may also be limited. The age and ethnic composition of the sample were homogenous, and may have limited generalizability. Previous co-twin studies have found similar results in Australian twin samples (Dinwiddie et al., 2000; Nelson et al., 2002), suggesting that findings maybe robust to other populations. Replication with large epidemiological samples from other countries, particularly non-Western samples, is needed to examine the extent to which macro-system level influences exist. Nonetheless, this study served as a broad overview of the relationship between TE and Axis I pathology.
Given the potential for a direct association between TE and Axis I psychopathology, more research is needed to elucidate the mechanism by which TE confers risk, as well as to examine aspects of the TE that may confer increased risk. Trauma type and severity are examples of trauma-related characteristics that previous research as shown to be related to risk for Axis I psychopathology, with particular risk being associated with interpersonal assault, rape, and childhood sexual abuse (Breslau, Peterson, Poisson, Schultz, & Lucia, 2004; Kendall-Tackett, 2002; Kilpatrick et al., 2003; Nelson et al., 2002). Furthermore, research suggests that once trauma-exposed, individuals are at greater risk for additional traumatic events, and that risk for PTSD and other psychopathology increases with multiple traumas (Breslau et al., 1999; Copeland, Keeler, Angold, & Costello, 2007; Kendler et al., 1999; McCutcheon et al., 2009).
In addition to enhancing our understanding of the mechanisms through which specific types, severity, or timing of trauma confer risk for psychopathology, such knowledge can help identify those who are at most risk for experiencing negative outcomes, determine which treatments are most effective (e.g., pharmacological, psychosocial, combination treatments (Nemeroff et al., 2003), or inform allocation of public resources toward trauma prevention and/or services. Finally, given the largely non-specific nature of the relationship between TE and Axis I disorders in the current study, future research addressing genetic and environmental factors that determine the nature of psychopathology post-TE are needed to better understand which individuals are at risk for which specific disorders or disorder classes. For example, although childhood abuse has been associated with adult onset Axis I disorders (Dinwiddie et al., 2000; Kendall-Tackett, 2002; Kendler et al., 2004; Nelson et al., 2002), a recent co-twin control analysis did not find support for a direct association between child abuse and adult borderline personality disorder (Bornovalova et al., in press).
Summary
Taking shared familial factors into account with the co-twin control analysis, the relationship between TE and Axis I pathology was largely robust. Indeed, dysthymia, anxiety disorders, SUD, eating disorders, and somatization disorder demonstrated apparently equivalent ORs in the general population and discordant twin samples, suggesting that TE may exert a causal influence on these disorders above and beyond shared familial influences. The etiology of Axis I disorders is quite complex and multi-determined. It is unlikely that the relationship between TE and these disorders is purely causal. However, the present findings suggest that TE may represent a contributory cause -- one of many pathways through which risk for Axis I pathology may increase. The findings of this study are preliminary and must be replicated; however, they suggest that the effects of TE extend beyond risk for PTSD. This has implications for research examining causal influences of environmental factors on the etiology of a range of Axis I pathology. From a clinical perspective, individuals who experience TE may need prevention or early intervention services to address a range of adjustment difficulties, including, but not limited to PTSD. Practitioners also may need to assess for history of TE for patients presenting with Axis I psychopathology and consider how TE might fit within the case conceptualization and treatment plan.
Footnotes
Results of analyses with MZ and DZ twins modeled separately are available upon request.
To account for clustering in the data resulting from twin-pairs, analyses were also run using generalized estimating equations in SPSS (v.19). Estimates and standard errors were not significantly different, thus the estimates and standard errors presented here can be considered robust. Results are available upon request.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, D.C: Author; 1994. [Google Scholar]
- Amstadter AB, Aggen SH, Knudsen GP, Reichborn-Kjennerud T, Kendler KS. A population-based study of familial and individual-specific environmental contributions to traumatic event exposure and posttraumatic stress disorder symptoms in a Norwegian twin sample. Twin Research and Human Genetics. 2012;15(5):656–662. doi: 10.1017/thg.2012.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Aggen SH, Knudsen GP, Reichborn-Kjennerud T, Kendler KS. Potentially traumatic event exposure, posttraumatic stress disorder, and Axis I and II comorbidity in a population-based study of Norwegian young adults. Social Psychiatry and Psychiatric Epidemiology. 2013;48(2):215–223. doi: 10.1007/s00127-012-0537-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amstadter AB, Acierno R, Richardson LK, Kilpatrick DG, Gros DF, Gaboury MT, Galea S. Posttyphoon prevalence of posttraumatic stress disorder, major depressive disorder, panic disorder, and generalized anxiety disorder in a Vietnamese sample. Journal of Traumatic Stress. 2009;22(3):180–188. doi: 10.1002/jts.20404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Archambeau OG, Frueh BC, Deliramich AN, Elhai JD, Grubaugh AL, Herman S, Kim BSK. Interpersonal violence and mental health outcomes among Asian American and Native Hawaiian/other Pacific Islander college students. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(4):273. doi: 10.1037/a0021262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedard-Gilligan M, Zoellner LA. The utility of the A1 and A2 criteria in the diagnosis of PTSD. Behaviour research and therapy. 2008;46(9):1062–1069. doi: 10.1016/j.brat.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Huibregtse BM, Hicks BM, Keyes M, McGue M, Iacono W. Tests of a direct effect of childhood abuse on adult Borderline Personality Disorder traits: A longitudinal discordant twin design. Journal of Abnormal Psychology. 2013;122(1):180–194. doi: 10.1037/a0028328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Archives of General Psychiatry. 1991;48:216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC. Estimating post-traumatic stress disorder in the community: Lifetime perspective and the impact of typical traumatic events. Psychological Medicine. 2004;34:1–10. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- Breslau N, Wilcox HC, Storr CL, Lucia VC, Anthony JC. Trauma exposure and posttraumatic stress disorder: A study of youths in urban America. Journal of Urban Health. 2004;81(4):530–544. doi: 10.1093/jurban/jth138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewerton TD. Eating disorders, trauma, and comorbidity: Focus on PTSD. Eating Disorders: The Journal of Treatment & Prevention. 2007;15(4):285–304. doi: 10.1080/10640260701454311. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Rose S. Fear, helplessness, and horror in posttraumatic stress disorder: Investigating DSM-IV criterion A2 in victims of violent crime. Journal of Traumatic Stress. 2000;13(3):499–509. doi: 10.1023/A:1007741526169. [DOI] [PubMed] [Google Scholar]
- Brown RJ, Schrag A, Trimble MR. Dissociation, childhood interpersonal trauma, and family functioning in patients with somatization disorder. The American Journal of Psychiatry. 2005;162(5):899–905. doi: 10.1176/appi.ajp.162.5.899. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Darves-Bornoz JM, Alonso J, de Girolamo G, de Graaf R, Haro JM, Kovess-Masfety V, Gasquet I. Main traumatic events in Europe: PTSD in the European Study of the Epidemiology of Mental Disorders Survey. Journal of Traumatic Stress. 2008;21(5):455–462. doi: 10.1002/jts.20357. [DOI] [PubMed] [Google Scholar]
- De Moor MHM, Boomsma DI, Stubbe JH, Willemsen G, de Geus EJC. Testing causality in the association between regular exercise and symptoms of anxiety and depression. Archives of General Psychiatry. 2008;65(8):897. doi: 10.1001/archpsyc.65.8.897. [DOI] [PubMed] [Google Scholar]
- Dinwiddie S, Heath AC, Dunne MP, Bucholz KK, Madden PAF, Slutske WS, Martin NG. Early sexual abuse and lifetime psychopathology: a co-twin-control study. Psychological Medicine. 2000;30(1):41–52. doi: 10.1017/s0033291799001373. [DOI] [PubMed] [Google Scholar]
- Frisell T, Öberg S, Kuja-Halkola R, Sjölander A. Sibling Comparison Designs: Bias From Non-Shared Confounders and Measurement Error. Epidemiology. 2012;23(5):713–720. doi: 10.1097/EDE.0b013e31825fa230. [DOI] [PubMed] [Google Scholar]
- Gilbertson MW, McFarlane AC, Weathers FW, Keane TM, Yehuda R, Shalev AY, Pitman RK. Is trauma a causal agent of psychopathologic symptoms in posttraumatic stress disorder? Findings from identical twins discordant for combat exposure. The Journal of clinical psychiatry. 2010;71(10):1324. doi: 10.4088/JCP.10m06121blu. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biological Psychiatry. 2001;49(12):1023–1039. doi: 10.1016/s0006-3223(01)01157-x. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. The American Journal of Psychiatry. 2001;158(10):1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Myers JM, Neale MC, Kendler KS. The structure of genetic and environmental risk factors for anxiety disorders in men and women. Archives of General Psychiatry. 2005;62:182–189. doi: 10.1001/archpsyc.62.2.182. [DOI] [PubMed] [Google Scholar]
- Hovens JGFM, Giltay EJ, Wiersma EJ, Spinhoven P, Penninx BWJH, Zitman FG. Impact of childhood life events and trauma on the course of depressive and anxiety disorders. Acta Psychiatrica Scandinavica. 2012;126(3):198–207. doi: 10.1111/j.1600-0447.2011.01828.x. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow CA, Wang PW. Research Domain Criteria (RDoC): Developing a valid diagnostic framework for research on mental disorders. American Journal of Psychiatry. 2010;167(7):748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- Kaltman S, Green BL, Mete M, Shara N, Miranda J. Trauma, depression, and comorbid PTSD/depression in a community sample of Latina immigrants. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(1):31. doi: 10.1037/a0018952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett K. The health effects of childhood abuse: four pathways by which abuse can influence health. Child Abuse & Neglect. 2002;26(6-7):715–729. doi: 10.1016/s0145-2134(02)00343-5. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Roysamb E, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for syndromal and subsyndromal common DSM-IV axis I and all axis II disorders. The American Journal of Psychiatry. 2001;168(1):29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Archives of General Psychiatry. 2000;57(10):953. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Campbell J. Interventionist causal models in psychiatry: Repositioning the mind-body problem. Psychological Medicine. 2009;39(6):881–887. doi: 10.1017/S0033291708004467. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. American Journal of Psychiatry. 2004;161(4):631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, MacLean CJ, Heath AC, Eaves LJ, Kessler RC. Smoking and major depression: A causal analysis. Archives of General Psychiatry. 1993;50:36–43. doi: 10.1001/archpsyc.1993.01820130038007. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA. Genes, Environment, and Psychopathology: Understanding the Causes of Pyschiatric and Substance Use Disorders. Guilford Press; New York: 2006. [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60(9):929. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology. 2003;71(4):692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Lyons MJ, Goldberg J, Simpson J, Williams WM, Toomey R, Tsaung MT. A co-twin control study of the relationship between combat exposure, combat-related posttraumatic stress disorder and other mental disorders. Journal of Traumatic Stress. 2003;16:433–438. doi: 10.1023/A:1025786925483. [DOI] [PubMed] [Google Scholar]
- Kremen WS, Koenen KC, Afari N, Lyons MJ. Twin studies of posttraumatic stress disorder: Differentiating vulnerability factors from sequelae. Neuropharmacology. 2012;62(2):647–653. doi: 10.1016/j.neuropharm.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubany ES, Ralston TC, Hill EE. Intense fear, helplessness, “and” horror? An empirical investigation of DSM-IV PTSD Criterion A2. Psychological Trauma: Theory, Research, Practice, and Policy. 2010;2(2):77. [Google Scholar]
- Lalande KM, Bonanno GA. Retrospective memory bias for the frequency of potentially traumatic events: A prospective study. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3(2):165. [Google Scholar]
- Lyons MJ, Goldberg J, Eisen SA, True W, Tsuang MT, Meyer JM. Do genes influence exposure to trauma? A twin study of combat. American Journal of Medical Genetics. 1993;48(1):22–27. doi: 10.1002/ajmg.1320480107. [DOI] [PubMed] [Google Scholar]
- McCutcheon VV, Heath AC, Nelson EC, Bucholz KK, Madden PAF, Martin NG. Accumulation of trauma over time and risk for depression in a twin sample. Psychological Medicine. 2009;39(3):431–441. doi: 10.1017/S0033291708003759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AC, Van Hooff M. Impact of childhood exposure to a natural disaster on adult mental health: 20-year longitudinal follow-up study. British Journal of Psychiatry. 2009;195(2):142–148. doi: 10.1192/bjp.bp.108.054270. [DOI] [PubMed] [Google Scholar]
- Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Dordrecht, The Netherlands: Kluwer; 1992. [Google Scholar]
- Nelson EC, Heath AC, Madden PAF, Cooper ML, Dinwiddie SH, Bucholz KK, Statham DJ. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Archives of General Psychiatry. 2002;59(2):139. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Heim CM, Thase ME, Klein DN, Rush AJ, Schatzberg AF, Dunner DL. Differential responses to psychotherapy versus pharmacotherapy in patients with chronic forms of major depression and childhood trauma. Proceedings of the National Academy of Sciences. 2003;100(24):14293. doi: 10.1073/pnas.2336126100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann DA, Houskamp BM, Pollack VE, Briere J. The long-term sequelae of childhood sexual abuse in women: A meta-analytic review. Child Maltreatment. 1996;1:6–16. [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders. 2011;25(3):456–465. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Safren SA, Gershuny BS, Marzol P, Otto MW, Pollack MH. History of childhood abuse in panic disorder, social phobia, and generalized anxiety disorder. Journal of Nervous and Mental Disease. 2002;190(7):453–456. doi: 10.1097/00005053-200207000-00005. [DOI] [PubMed] [Google Scholar]
- Sartor CE, Grant JD, Lynskey MT, McCutcheon VV, Waldron M, Statham DJ, Martin NG. Common Heritable Contributions to Low-Risk Trauma, High-Risk Trauma, Posttraumatic Stress Disorder, and Major Depression. Archives of General Psychiatry. 2012;69(3):293. doi: 10.1001/archgenpsychiatry.2011.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MB, Jang KJ, Taylor S, Vernon PA, Livesley WJ. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder: A twin study. American Journal of Psychiatry. 2002;159(10):1675–1681. doi: 10.1176/appi.ajp.159.10.1675. [DOI] [PubMed] [Google Scholar]
- Tambs K, Ronning T, Prescott CA, Kendler KS, Reichborn-Kjennerud T, Torgersen S, Harris JR. The Norwegian Institute of Public Health twin study of mental health: Examining recruitment and attrition bias. Twin Research and Human Genetics. 2009;12:158–168. doi: 10.1375/twin.12.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dijke A, Ford JD, van der Hart O, van Son M, van der Heijden P, Buhring M. Complex posttraumatic stress disorder in patients with borderline personality disorder and somatoform disorders. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(2):162. [Google Scholar]
- Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Lachner G, Wunderlich U, Pfister H. Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI) Social Psychiatry and Psychiatric Epidemiology. 1998;33(11):568–578. doi: 10.1007/s001270050095. [DOI] [PubMed] [Google Scholar]
- Wittchen HU, Pfister H. DIA-X-Interviews (M-CIDI): Manual fur Screening-Verfahren und Interview; Interviewheft Langsschnittuntersuchung (DIA-X-Lifetime); Erganzungsheft (DIA-X lifetime); Interviewheft Querschnittuntersuchung (DIA-X 12 Monate); Erganzungsheft (DIA-X 12 Monate); PC-Programm zur Durchfuhrung des Interviews (Langs-und Querschnittuntersuchung); Auswertungsprogramm. Frankfurt, Germany: Swets & Zeitlinger; 1997. [Google Scholar]


