Abstract
BACKGROUND:
There is a paucity of information regarding descriptive epidemiology of paediatric concussions over time, and few studies include both emergency department (ED) and physician office visits.
OBJECTIVE:
To describe trends in visits for paediatric concussions in both EDs and physician offices according to age and sex. A secondary objective was to describe the cause of concussion for children treated in EDs.
METHODS:
A retrospective, population-based study using linked health administrative data from all concussion-related visits to the ED or a physician office by school-age children and youth (three to 18 years of age) in Ontario between April 1, 2003 and March 3, 2011 was conducted.
RESULTS:
The number of children evaluated in both EDs and a physician offices increased between 2003 and 2010, and this linear trend was statistically significant (P=0.002 for ED visits and P=0.001 for office visits). The rate per 100,000 increased from 466.7 to 754.3 for boys and from 208.6 to 440.7 for girls during the study period. Falls accounted for approximately one-third of the paediatric concussions. Hockey/skating was the most common specific cause of paediatric sports-related concussions.
CONCLUSIONS:
The increasing use of health care services for concussions is likely related to changes in incidence over time and increased awareness of concussion as a health issue. Evidence-based prevention initiatives to help reduce the incidence of concussion are warranted, particularly in sports and recreation programs.
Keywords: Concussion, Concussion-related injury, Epidemiology, Paediatric
Abstract
HISTORIQUE :
On possède peu d’information sur l’épidémiologie descriptive des commotions cérébrales en pédiatrie au fil du temps, et rares sont celles qui portent à la fois sur les visites à l’urgence et au cabinet du médecin.
OBJECTIF :
Décrire les tendances des visites à l’urgence et au cabinet du médecin par une population d’âge pédiatrique en raison de commotions cérébrales, en fonction de l’âge et du sexe. Un objectif secondaire consistait à décrire la cause des commotions cérébrales chez les enfants traités à l’urgence.
MÉTHODOLOGIE :
Des chercheurs ont mené une étude rétrospective en population reliant les données administratives en matière de santé de toutes les visites d’enfants d’âge scolaire et d’adolescents (de trois à 18 ans) à l’urgence ou au cabinet du médecin en raison d’une commotion cérébrale en Ontario, entre le 1er avril 2003 et le 3 mars 2011.
RÉSULTATS :
Le nombre d’enfants évalués à l’urgence ou au cabinet du médecin a augmenté entre 2003 et 2010, et cette tendance linéaire était statistiquement significative (P=0,002 pour les visites à l’urgence et P=0,001 pour celles en cabinet). Pendant la période de l’étude, le taux sur 100 000 enfants est passé de 466,7 à 754,3 chez les garçons et de 208,6 à 440,7 chez les filles. Les chutes représentaient environ le tiers des commotions cérébrales en pédiatrie, tandis que le hockey ou le patin était la principale cause de commotions cérébrales liées au sport.
CONCLUSIONS :
L’utilisation croissante des services de santé en raison d’une commotion cérébrale est probablement liée à l’évolution de leur incidence et à une plus grande sensibilisation à leurs conséquences sur la santé. Il faudra entreprendre des initiatives de prévention fondées sur des données probantes pour contribuer à réduire l’incidence des commotions cérébrales, notamment dans le cadre des programmes sportifs et de loisirs.
Unintentional injuries are common among children and youth; among these injuries, traumatic brain injuries (TBIs) are a cause for concern. According to the 2009–2010 Canadian Community Health Survey, 23% of the adolescent population reported having sustained a head injury within the previous year (1). Mild TBIs (mTBIs), commonly referred to as concussions, may lead to impaired neurological functioning, including chronic headaches and memory deficits, making this an important public health problem (2).
Within the paediatric population, the association between age and concussion may vary, with one study reporting a peak at approximately 10 years of age and subsequent decline, while other studies reported that children >10 years of age were at increased risk for head injury (2–4). The reported causes of concussion vary according to age. Among them, falls are the most common cause of injury in younger children (3,5–8). Approximately 45% of the TBIs admitted to Canadian hospitals were fall-related. (6) Adolescents are more susceptible to sports-related injuries, which account for 30% of paediatric concussions (6,9–11). Sports-related concussions frequently occur in organized team sports such as hockey, basketball, soccer, football, baseball, etc (3,6,10–15). The rate of concussion in sports also varies according to sex. Boys are more likely to sustain a concussion while playing football or hockey, whereas girls are more likely to sustain a concussion while playing soccer (12,13). Snow sports, such as skiing, and combative sports, such as martial arts, have also been associated with an increased risk for concussion (3,10,16). Motor vehicle collisions are another major source of paediatric concussions (6,7). One study reported that 28% of paediatric concussions that were examined in an emergency department (ED) were caused by road traffic collisions (7).
Previous studies have mainly focused on children who were evaluated in an ED. To date, no studies have described the incidence of paediatric concussions treated in both EDs and physician offices. In addition, few studies have examined population-based trends in paediatric concussions over time – they have focused solely on sports-related concussions and have shown an increase in incidence (17,18).
The primary objective of the present study was to describe trends in paediatric concussions in both EDs and physician offices according to age and sex. A secondary objective was to examine the causes of concussion among children treated in the ED.
METHODS
Selection and description of participants
A retrospective analysis of all visits related to a diagnosis of concussion in an ED or a physician office by school-age children and youth (three to 18 years of age) in Ontario between April 1, 2003 and March 3, 2011 was conducted. ED visit records with an International Classification of Diseases, 10th Revision, Canada (ICD-10-CA) diagnosis of S060 (concussion) were reviewed, as well as office visit records with an Ontario Health Insurance Plan diagnosis code of 850 or 854 (concussion or head injury). Multiple visits for the same patient were included; however, only one billing per patient per day was included. Duplicated, overlapping and transferred ED visits were excluded. Records with a missing or invalid health card number, age or sex were also excluded.
Technical information
Unique anonymized encrypted identifiers were used to link multiple population-based health administrative databases routinely collected by the Institute for Clinical Evaluative Sciences (Toronto, Ontario), which contain information on all medically necessary services received by publicly insured residents of Ontario. These included the National Ambulatory Care Reporting System for ED visits, a database maintained by the Canadian Institute for Health Information (Toronto, Ontario); the Ontario Health Insurance Plan for physician billings including physician visits, diagnosis codes and procedures; and the Registered Persons Database for patient demographic information. For ED patients, the most common causes of injury were identified; however, this information was not available in the physician office data. The broad causes that were evaluated in the present study included falls, exposure to force, motor vehicle crashes and being struck by another person. The specific causes that were examined were identified based on availability of data and previous identification of common concussion risk factors. These were hockey/skating, motor vehicle occupant, football/rugby, snow sports, cycling, baseball, soccer, falls from playground equipment, inline skating or skateboarding, and pedestrian injury.
Statistics
The total number of ED and physician office visits for concussion according to sex and age group from the fiscal years 2003 to 2010 were identified. A χ2 test for trends was used to assess the change in the rates over the seven-year period.
All calculations were performed using SAS version 9.2 (SAS Corporation, USA). Rates were calculated using the number of visits as the numerator and the appropriate population, according to the Registered Persons Database, with age and sex as the denominator. Research Ethics Board approval was obtained from Sunnybrook Health Sciences Centre (Toronto, Ontario).
RESULTS
Between 2003 and 2010, a total of 88,688 paediatric concussions were treated in either an ED or a physician office, and there was a significant trend over time in both locations (P=0.002 and P=0.001, respectively). In 2003, there were 8736 concussions treated in either an ED or a physician office, compared with 14,886 in 2010 (Table 1). Figure 1 shows an increasing trend, with a growth in office-based visits in later years. In addition, the rate per 100,000 increased from 340.5 in 2003 to 601.3 in 2010 (Table 1).
TABLE 1.
Total annual number of visits for paediatric concussions to an emergency department and physician office in Ontario, 2003 to 2010
| Year | Emergency department | Physician office | Total number of visits | Rate per 100,000 |
|---|---|---|---|---|
| 2003 | 4180 | 4556 | 8736 | 340.5 |
| 2004 | 4791 | 4893 | 9684 | 378.5 |
| 2005 | 4701 | 4979 | 9680 | 379.8 |
| 2006 | 4847 | 4945 | 9792 | 386.1 |
| 2007 | 5252 | 5439 | 10,691 | 423.3 |
| 2008 | 5583 | 5968 | 11,551 | 460.0 |
| 2009 | 6443 | 7235 | 13,678 | 548.8 |
| 2010 | 6495 | 8391 | 14,886 | 601.3 |
| Total | 42,292 | 46,406 | 88,698 | – |
Figure 1).
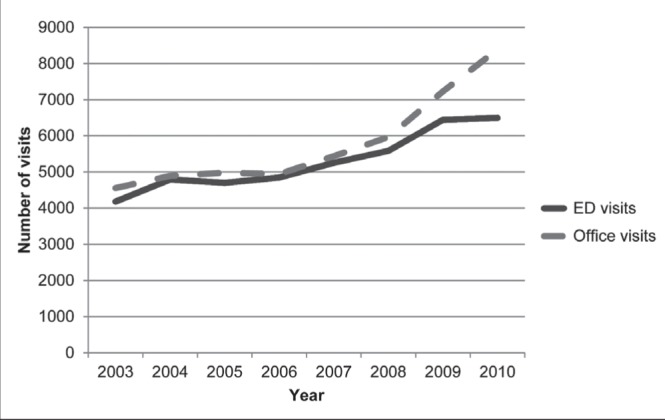
Total number of annual visits for paediatric concussion to an emergency department (ED) and physician office in Ontario, 2003 to 2010
Boys were more likely to be treated for concussions than girls, and this difference was consistent over the study period (Figure 1). For both boys and girls, the number of visits for concussion increased until 15 years of age, then decreased until 18 years of age (Figure 2). The rate per 100,000 increased from 466.7 to 754.3 for boys, and from 208.6 to 440.7 for girls between 2003 and 2010 (Table 2).
Figure 2).
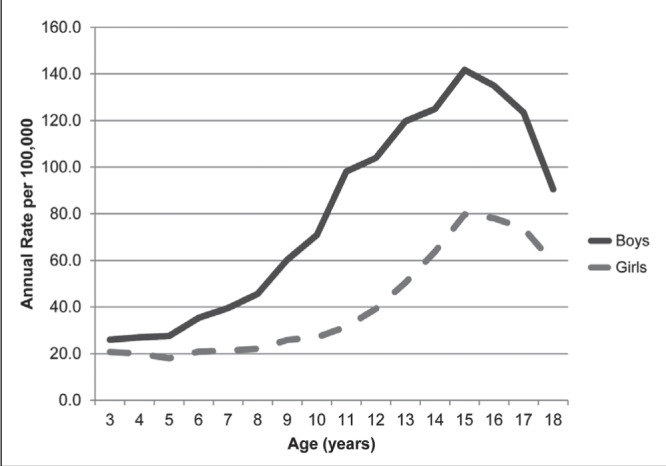
Paediatric emergency department and physician office visit annual concussion rate among boys and girls per 100,000 population according to age, 2003 to 2010
TABLE 2.
Total annual number of visits for paediatric concussions to an emergency department and physician office according to sex in Ontario, 2003 to 2010
| Year | All visits | Rate per 100,00 | ||
|---|---|---|---|---|
|
|
|
|||
| Boys | Girls | Boys | Girls | |
| 2003 | 6121 | 2615 | 466.7 | 208.6 |
| 2004 | 6817 | 2867 | 521.1 | 229.3 |
| 2005 | 6671 | 3009 | 511.8 | 241.7 |
| 2006 | 6604 | 3188 | 508.9 | 257.4 |
| 2007 | 7258 | 3433 | 561.4 | 278.4 |
| 2008 | 7659 | 3892 | 595.8 | 317.5 |
| 2009 | 8830 | 4838 | 692.0 | 397.8 |
| 2010 | 9563 | 5323 | 754.3 | 440.7 |
| Total | 59,523 | 29,165 | – | – |
When the broad causes of concussion were examined, falls were found to be the most common cause of concussion in an ED, representing 34% of all ED visits, followed closely by exposure to force (25.5%) and motor vehicle collisions (12.3%). When specific causes were examined in more detail, hockey/skating was the most common cause of concussions that were treated in an ED (Figure 3).
Figure 3).
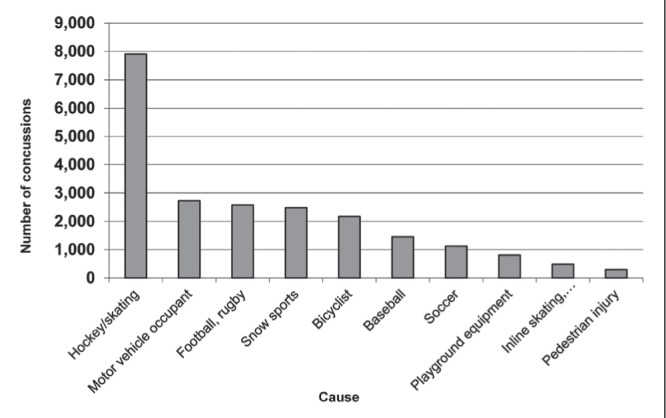
Emergency department visits for paediatric concussion according to selected causes in Ontario, 2003 to 2010
DISCUSSION
Our main finding was that the use of health services for concussion increased from 2003 to 2010 in Ontario, Canada’s largest province. Our study revealed an increase in office visits for concussions over this period of time. Given that the Zurich guidelines suggest that patients be diagnosed and subsequently cleared to return to activity by a physician, it is encouraging to observe more patients being evaluated for concussion in physician offices rather than EDs (19).
The variation in concussions according to age is not consistent in the literature, although most studies support our findings of increased concussions in adolescence (3,7–10). Only two studies reported that children <6 years of age were more likely to sustain a concussion than those >6 years of age (13,16).
The findings in our study are consistent with the majority of other studies reporting the major causes of paediatric concussions. Previous injury studies have reported the importance of falls as a cause of concussions in children (3,5–7,16). The Canadian Institute for Health Information analysis on national injury hospitalizations found falls to be one of the leading causes of injury hospitalizations in Canada (6). Previous studies of sports-related concussions involving children identified football and hockey as the sports that were associated with the highest number of concussions (3,10–12). Our findings reinforced that falls in general are the most common cause of paediatric concussions and, in terms of sports-specific causes, hockey/skating – a sport commonly played in North America – was associated with the greatest number of paediatric concussions.
Harris et al (17) conducted a population-based study of sport and recreation-related head injuries and reported that the rate of these injuries per 100,000 decreased from 99.4 in 1997/98 to 93.3 in 2007/2008. In contrast, Selassie et al (18) found that the rate of head injuries per 100,000 related to sports and recreation increased from 19.7 in 1998 to 45.6 in 2011. Our study showed that the rate of concussions per 100,000 for both sexes increased between 2003 and 2010; however, these rates are based on all causes and are not specific to sports.
Several interventions have been shown to reduce concussions. Sports-related concussions can be minimized by taking preventive action such as reducing body checking in hockey or wearing a helmet while cycling. Warsh et al (20) conducted a systematic review investigating the association between body checking and injury in youth ice hockey, and reported that the relative risk associated with body checking was between 0.63 and 39.79. The authors concluded that to decrease the burden of injury in hockey, body checking needs to be introduced at an older age. In addition, other prevention measures, such as wearing a helmet while cycling, have been shown to reduce the risk of head injury among youth. Macpherson and Spinks (21) conducted a systematic review of bicycle helmet legislation for the uptake of helmet use and prevention of head injuries. They reported that there is positive evidence to suggest that bicycle helmet legislation increases bicycle helmet use and decreases bicycle-related head injuries.
Strengths and limitations
The present study was the first to examine paediatric concussions evaluated in an ED and those evaluated in a physician office. By examining all of the paediatric concussions evaluated in multiple facilities, we were able to overcome the issue of under-reporting and obtain a more accurate number of concussions treated in Ontario. In addition, we collected data for a seven-year period; this enabled us to examine the changing trends over time.
The major limitation to our study was that not all concussions are treated in EDs or physician offices; therefore, we could not capture data regarding children who were evaluated by other medical professionals such as athletic therapists. In addition, the Institute for Clinical Evaluative Sciences only captures information for ED and physician visits in Ontario; therefore, our study may not be generalizable to other populations. We were also unable to discern whether the increase in visits for concussions were due to an increase in incidence, or an increase in awareness of concussion and the need for treatment. Finally, some children may have been seen in an ED initially and subsequently followed in a physician’s office, and may, therefore, be counted more than once in the present study.
CONCLUSION
The number of children and youth treated for concussions in both EDs and physician offices increased between 2003 and 2010 in Ontario, Canada. However, over the years, more children were being evaluated in physician offices than EDs. Falls were the greatest broad cause of paediatric concussions, alongside more specific causes such as hockey/skating. Evidence-based prevention programs, including helmet use, fall prevention and recent changes to limit body checking in hockey, may help to reduce the incidence of concussion. Ongoing epidemiological studies can attempt to differentiate between the true incidence of concussion and an increase in health service utilization associated with increased awareness of concussion and subsequent health consequences.
Footnotes
FUNDING SOURCE: The Institute for Clinical Evaluative Sciences.
FINANCIAL DISCLOSURES: Dr Guttmann and Dr Macpherson are both supported by a Canadian Institute for Health Research Applied Chair in Child Health Services Research. The study was performed at the Institute for Clinical Evaluative Sciences, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). Dr Macpherson also receives funding from the Donald Sanderson Memorial Foundation. The opinions, results and conclusions reported in this article are those of the authors and are independent from all funding sources. No endorsement by Institute for Clinical Evaluative Sciences or the Ontario MOHLTC is intended or should be inferred. Research Ethics Board approval was obtained from Sunnybrook Health Sciences Centre. None of these sources of support were involved in the study design, collection, analysis or interpretation of data, writing of the report or decision to submit the manuscript for publication. The authors have no conflicts of interest to declare.
REFERENCES
- 1.Billette JM, Janz T, Statistics Canada Injuries in Canada: Insights from the Canadian Community Health Survey. 2011.
- 2.Browne GJ, Lam LT. Concussive head injury in children and adolescents related to sports and other leisure physical activities. Br J Sports Med. 2006;40:163–8. doi: 10.1136/bjsm.2005.021220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Willer B. A population based investigation of head injuries and symptoms of concussion of children and adolescents in schools. Inj Prev. 2004;10:144–8. doi: 10.1136/ip.2003.005017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang J, Phillips G, Xiang H, Allareddy V, Heiden E, Peek-Asa C. Hospitalisations for sport-related concussions in US children aged 5 to 18 years during 2000–2004. Br J Sports Med. 2008;42:664–9. doi: 10.1136/bjsm.2007.040923. [DOI] [PubMed] [Google Scholar]
- 5.Andersson EE, Sejdhage R, Wage V, Centre C. Mild traumatic brain injuries in children between 0–16 years of age: A survey of activities and places when an accident occurs. Dev Neurorehabil. 2012;15:26–30. doi: 10.3109/17518423.2011.633570. [DOI] [PubMed] [Google Scholar]
- 6.Canadian Institute for Health Information. Head Injuries in Canada: A Decade of Change (1994 – 1995 to 2003 – 2004) 2006. < https://secure.cihi.ca/free_products/ntr_head_injuries_2006_e.pdf> (Accessed October 7, 2014)
- 7.Tabish A, Lone N, Afzal WM, Salam A. The incidence and severity of injury in children hospitalised for traumatic brain injury in Kashmir. Injury. 2006;37:410–5. doi: 10.1016/j.injury.2006.01.039. [DOI] [PubMed] [Google Scholar]
- 8.Faul M, Xu L, MD, Wald MM, Coronado VG. Brain Injury. Atlanta: Jan, 2010. Traumatic brain injury registries in the United States: An overview. < www.cdc.gov/traumaticbraininjury/pdf/blue_book.pdf> (Accessed October 7, 2014) [DOI] [PubMed] [Google Scholar]
- 9.Meehan WP, Mannix R. Pediatric concussions in United States emergency departments in the years 2002 to 2006. J Pediatr. 2010;157:889–93. doi: 10.1016/j.jpeds.2010.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakhos LL, Lockhart GR, Myers R, Linakis JG. Emergency department visits for concussion in young child athletes. Pediatrics. 2010;126:e550–6. doi: 10.1542/peds.2009-3101. [DOI] [PubMed] [Google Scholar]
- 11.Kimbler DE, Murphy M, Dhandapani KM. Concussion and the adolescent athlete. J Neurosci Nurs. 2011;43:286–90. doi: 10.1097/JNN.0b013e31823858a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halstead ME, Walter KD. Sport-related concussion in children and adolescents. Pediatrics. 2010;126:597–615. doi: 10.1542/peds.2010-2005. [DOI] [PubMed] [Google Scholar]
- 13.Schatz P, Moser RS. Current issues in pediatric sports concussion. Clin Neuropsychol. 2011;25:1042–57. doi: 10.1080/13854046.2011.556669. [DOI] [PubMed] [Google Scholar]
- 14.Johnson LSM. Concussion in youth ice hockey: It’s time to break the cycle. CMAJ. 2011;183:921–4. doi: 10.1503/cmaj.110282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giannotti M, Al-Sahab B, McFaull S, Tamim H. Epidemiology of acute head injuries in Canadian children and youth soccer players. Injury. 2010;41:907–12. doi: 10.1016/j.injury.2009.09.040. [DOI] [PubMed] [Google Scholar]
- 16.Knox CL, Comstock RD, McGeehan J, Smith G. Differences in the risk associated with head injury for pediatric ice skaters, roller skaters, and in-line skaters. Pediatrics. 2006;118:549–54. doi: 10.1542/peds.2005-2913. [DOI] [PubMed] [Google Scholar]
- 17.Harris AW, Jones CA, Rowe BH, Voaklander DC. A population-based study of sport and recreation-related head injuries treated in a Canadian health region. J Sci Med Sport. 2012;15:298–304. doi: 10.1016/j.jsams.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Selassie AW, Wilson D, Pickelsimer EE, Voronca DC, Williams NR, Edwards JC. Incidence of sport-related traumatic brain injury and risk factors of severity: A population-based epidemiologic study. Ann Epidemiol. 2013;23:750–6. doi: 10.1016/j.annepidem.2013.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: The 4th International Conference on Concussion in Sport held in Zurich, November 2012. Br J Sports Med. 2013;47:250–8. doi: 10.1136/bjsports-2013-092313. [DOI] [PubMed] [Google Scholar]
- 20.Warsh JM, Constantin S, Howard A, Macpherson A. A systematic review of the association between body checking and injury in youth ice hockey. Clin J Sport Med. 2009;19:134–44. doi: 10.1097/JSM.0b013e3181987783. [DOI] [PubMed] [Google Scholar]
- 21.Macpherson A, Spinks A. Bicycle helmet legislation for the uptake of helmet use and prevention of head injuries. Cochrane Database Syst Rev. 2010;(3):CD005401. doi: 10.1002/14651858.CD005401.pub2. [DOI] [PubMed] [Google Scholar]


