Abstract
Background
Although survival after in-hospital cardiac arrest is likely to vary among hospitals caring for children, validated methods to risk-standardize pediatric survival rates across sites do not currently exist.
Methods and Results
Within the American Heart Association’s Get With the Guidelines-Resuscitation registry for in-hospital cardiac arrest, we identified 1,551 cardiac arrests in children (<18 years) from 2006 to 2010. Using multivariable hierarchical logistic regression, we developed and validated a model to predict survival to hospital discharge and calculated risk-standardized rates of cardiac arrest survival for hospitals with a minimum of 10 pediatric cardiac arrest cases. A total of 13 patient-level predictors were identified: age, sex, cardiac arrest rhythm, location of arrest, mechanical ventilation, acute non-stroke neurologic event, major trauma, hypotension, metabolic or electrolyte abnormalities, renal insufficiency, sepsis, illness category, and need for intravenous vasoactive agents prior to the arrest. The model had good discrimination (C-statistic of 0.71), confirmed by bootstrap validation (validation C-statistic of 0.69). Among 30 hospitals with at least 10 cardiac arrests, unadjusted hospital survival rates varied considerably (median, 37%; inter-quartile range [IQR]: 24%–42%; range: 0%–61%). After risk-standardization, the range of hospital survival rates narrowed (median, 37%; IQR: 33%–38%; range: 29%– 48%), but variation in survival persisted.
Conclusion
Using a national registry, we developed and validated a model to predict survival after in-hospital cardiac arrest in children. After risk-standardization, significant variation in survival rates across hospitals remained. Leveraging these models, future studies can identify best practices at high-performing hospitals to improve survival outcomes for pediatric cardiac arrest.
Keywords: pediatrics, heart arrest, cardiopulmonary resuscitation, risk model
Although in-hospital cardiac arrest in children is associated with poor survival, the extent to which survival rates differ across hospitals is unknown.1 Understanding this inter-hospital variation is important, as the presence of substantial variability would suggest an opportunity to improve pediatric outcomes after cardiac arrest. Toward that end, The Joint Commission and other national organizations, such as the American Heart Association, are developing performance measures to benchmark outcomes for in-hospital cardiac arrest and resuscitation.
Until recently, the ability to examine variation in pediatric outcomes for in-hospital cardiac arrest has been limited due to the lack of a central registry. Moreover, while standard methods have emerged to perform risk-standardization for other conditions, these have not been applied to survival after cardiac arrest in children.2 Therefore, current efforts to compare hospital resuscitation outcomes for children may be premature until validated models are developed.
The emergence of the American Heart Association’s Get With the Guidelines (GWTG)-Resuscitation registry—a national registry of in-hospital cardiac arrest—over the past decade provides a unique opportunity to address these current gaps in knowledge. Accordingly, we developed and validated a hierarchical regression model for survival in pediatric patients with inhospital cardiac arrest. We then applied this model to calculate risk-standardized survival rates for pediatric in-hospital cardiac arrest at each hospital and evaluated the extent of site-level variation in survival outcomes. The findings in this study will offer a methodological framework for future hospital comparisons of survival outcomes for pediatric in-hospital cardiac arrest.
Methods
Study Population
Formerly known as the National Registry of Cardiopulmonary Resuscitation, GWTG-Resuscitation is a large, prospective, national registry of in-hospital cardiac arrest sponsored by the American Heart Association. Its design has been described in detail previously.3 In brief, trained hospital personnel enroll all patients without do-not-resuscitate orders with a cardiac arrest (defined as pulselessness requiring chest compressions and/or defibrillation and eliciting a hospital-wide or unit-based emergency response). Cases are identified by multiple methods, including centralized collection of cardiac arrest flow sheets, reviews of hospital paging system logs, and routine checks of code carts, pharmacy tracer drug records, and hospital billing charges for resuscitation medications.3 Standardized “Utstein-style” definitions are used for all patient variables and outcomes to facilitate uniform reporting across hospitals.4, 5 In addition, data accuracy is ensured by rigorous certification of hospital staff and use of standardized software with data checks for completeness and accuracy.3 Currently, the Registry incorporates data from approximately 8% of all U.S. hospitals.
From January 2000 through August 2010, data from 2,883 pediatric patients under 18 years of age with an in-hospital cardiac arrest were submitted to GWTG-Resuscitation. Since pediatric in-hospital survival rates have improved over time6, we restricted our study sample to the 1,640 patients enrolled between January 2006 and August 2010 to ensure that our risk models were based on a contemporary cohort of patients. Additionally, we excluded 89 resuscitations performed in the delivery room, as cardiac arrests in the delivery room differ physiologically and mechanistically from cardiac arrests in other hospital settings. Our final study cohort comprised 1,551 patients from 164 hospitals.
Study Outcome and Variables
The primary outcome of interest was survival to hospital discharge. A number of baseline characteristics were screened as candidate predictors for the study outcome. Variables that were considered for model inclusion were those clinical and demographic characteristics that were known to be associated with survival. These included age at the time of cardiac arrest (categorized as neonates [≤30 days], infants [31 days to ≤1 year], young children [1–8 years], and older children [>8 years of age]), sex, location of arrest (categorized as procedure areas, intensive care, monitored unit, non-monitored unit, emergency department, and other), time of arrest (day vs. night [11pm to 6:59am])7, initial cardiac arrest rhythm (ventricular fibrillation, pulseless ventricular tachycardia, asystole, pulseless electrical activity), and illness category (medical-cardiac, medical-noncardiac, surgical-cardiac, surgical-noncardiac).
In addition, the following co-morbidities or medical conditions coded as present prior to cardiac arrest were evaluated for the model: heart failure; renal, hepatic, or respiratory insufficiency; baseline evidence of motor, cognitive, or functional neurologic deficits (CNS depression); acute stroke; acute non-stroke neurologic event; pneumonia; hypotension; arrhythmia; sepsis; major trauma; metabolic or electrolyte abnormality; and metastatic or hematologic malignancy. Finally, we considered for model inclusion several critical care interventions (requirement for mechanical ventilation, intravenous vasoactive medications or intravenous antiarrhythmics) already in place at the time of cardiac arrest. Race was not considered for model inclusion, as prior studies have found that racial differences in survival after in-hospital cardiac arrest are partly mediated by differences in hospital care quality for blacks and whites.8, 9
Model Development and Validation
Multivariable logistic regression models were constructed to identify significant predictors of inhospital survival. Because our primary objective was to derive risk-standardized survival rates for each hospital, which would require us to account for clustering of observations within hospitals, we used hierarchical logistic regression models for our analyses.10 By using hierarchical models to estimate the log-odds of in-hospital survival as a function of demographic and clinical variables (both fixed effects) and a random effect for each hospital, we were able to assess for hospital variation in risk-standardized survival rates after accounting for patient case-mix.
We considered for model inclusion the candidate variables described in the previous section. Age group, sex, initial cardiac arrest rhythm, and arrest location were included in the model regardless of statistical significance. Multicollinearity between covariates was assessed for each variable prior to model inclusion.11 Model discrimination was assessed with the C-statistic, which quantifies the receiver operating characteristic curve (ROC) of the model.12 To validate the model, we examined observed vs. predicted plots and performed 1000 bootstrap samples to derive a validation C-statistic that would correct for potential model over-fitting.13
Hospital Risk-Standardized Survival Rates
Using the hospital-specific estimates (i.e., random intercepts) from the hierarchical models, we then calculated risk-standardized survival rates for the 30 study hospitals with a minimum of 10 cardiac arrest cases by multiplying the registry’s unadjusted survival rate by the ratio of a hospital’s predicted to expected survival rate. We used the ratio of predicted to expected outcomes (described below) instead of the ratio of observed to expected outcomes to overcome analytical issues that have been described for the latter approach.14–16 Specifically, our approach ensured that all hospitals, including those with smaller case volumes, would have appropriate risk-standardization and confidence intervals for their cardiac arrest survival rates.
For these calculations, the expected hospital number of cardiac arrest survivors is the number of cardiac arrest survivors expected at the hospital if the hospital’s patients were treated at a “reference” hospital (i.e. the average hospital-level intercept from all hospitals in GWTG-Resuscitation). This was determined by regressing patients’ risk factors and characteristics on inhospital survival with all hospitals in the sample, and then applying the subsequent estimated regression coefficients to the patient characteristics observed at a given hospital, and then summing the expected number of deaths. In effect, the expected rate is a form of indirect standardization. In contrast, the predicted hospital outcome is the number of survivors at a specific hospital. It is determined in the same way that the expected number of deaths is calculated, except that the hospital’s individual random effect intercept is used. The risk-standardized survival rate was then calculated by the ratio of predicted to expected survival rate, multiplied by the unadjusted rate for the entire study sample.17 The effects of risk-standardization on unadjusted hospital rates of survival were then illustrated with descriptive plots and statistics.
All study analyses were performed with SAS 9.2 (SAS Institute, Cary, NC) and R version 2.10.0.18 The hierarchical models were fitted with the use of the GLIMMIX macro in SAS. Dr. Chan had full access to the data and takes responsibility for its integrity. All authors have read and agree to the manuscript as written. The American Heart Association’s GWTG-Resuscitation Committee approved the final manuscript draft.
Results
Of 1,551 patients with in-hospital cardiac arrest, 481 (31.0%) were neonates, 358 (23.1%) infants, 358 (23.1%) younger children, and 354 (22.8%) older children. Fifty-eight percent of the study population was male and 21.5% were black. The vast majority (n=1361, 87.7%) had a non-shockable cardiac arrest rhythm; 53.8% had a first documented rhythm of pulseless electrical activity and 33.9% with asystole. Sixty-seven percent of the arrests occurred in an intensive care unit and 21.4% in a procedure area or in the emergency department, with less than 10% occurring on a general pediatric ward. Hypotension was documented in 38.3% prior to the cardiac arrest, and respiratory insufficiency in 60.1%.
Predictors of Survival
Overall, 543 (35.0%) pediatric patients with an in-hospital cardiac arrest survived to hospital discharge. Tables 1 and 2 compare baseline demographics of the study cohort among those patients who survived and did not survive to hospital discharge. Children over 8 years of age were less likely to survive an in-hospital cardiac arrest than younger patients. In univariate analyses, the presence of hypotension, renal insufficiency, hepatic insufficiency, metabolic or electrolyte abnormalities, acute CNS non-stroke event, sepsis, major trauma, and metastatic or hematologic malignancy were also associated with a lower likelihood of survival. Finally, patients treated with mechanical ventilation and intravenous vasoactive medications at the time of cardiac arrest were less likely to survive, whereas patients treated with antiarrhythmics at the time of cardiac arrest were more likely to survive to discharge.
Table 1.
Baseline Characteristics of Patients Surviving and Not Surviving to Hospital Discharge
| No. (%)(N =1551) | Survivors (n=543) | Non-Survivors (n= 1008) | P value | |
|---|---|---|---|---|
| Demographics | ||||
| Age groups | <0.001 | |||
| Neonates (0–1 month) | 481 (31.0) | 165 (30.4) | 316 (31.3) | |
| Infants (1–12 months) | 358 (23.1) | 167 (30.8) | 191 (18.9) | |
| Young Children (1–8 years) | 358 (23.1) | 120 (22.1) | 238 (23.6) | |
| Older Children (8–18 years) | 354 (22.8) | 91 (16.8) | 263 (26.1) | |
| Male Sex | 900 (58.0) | 301(55.4) | 599(59.4) | 0.13 |
| Race | 0.01 | |||
| White | 853 (55.0) | 318 (58.6) | 535 (53.1) | |
| Black | 333 (21.5) | 103 (19.0) | 230 (22.8) | |
| Other | 199 (12.8) | 78 (14.4) | 121 (12.0) | |
| Unknown | 166 (10.7) | 44 (8.1) | 122 (12.1) | |
| Event Characteristics | ||||
| Initial Rhythm | 0.03 | |||
| Asystole | 526 (33.9) | 166 (30.6) | 360 (35.7) | |
| PEA | 835 (53.8) | 295 (54.3) | 540 (53.6) | |
| VF | 102 (6.6) | 42 (7.7) | 60 (6.0) | |
| Pulseless VT | 88 (5.7) | 40 (7.4) | 48 (4.8) | |
| Night* (11pm to 6:59am) | 429 (27.9) | 140 (26.0) | 289 (28.9) | 0.23 |
| Weekend (11pm Fri to 6:59am Mon) | 457 (29.5) | 137 (25.2) | 320 (31.7) | 0.007 |
| Location | <0.001 | |||
| ICU | 1042 (67.2) | 368 (67.8) | 674 (66.9) | |
| Procedure areas | 117 (7.5) | 61 (11.2) | 56 (5.6) | |
| ED | 215 (13.9) | 45 (8.3) | 170 (16.9) | |
| Monitored | 39 (2.5) | 12 (2.2) | 27 (2.7) | |
| Unmonitored | 86 (5.5) | 36 (6.6) | 50 (5.0) | |
| Other | 52 (3.4) | 21(3.9) | 31 (3.1) | |
| Illness Category | <0.001 | |||
| Med-Cardiac | 221 (14.2) | 86 (15.8) | 135 (13.4) | |
| Med-Noncardiac | 540 (34.8) | 164 (30.2) | 376 (37.3) | |
| Surg-Cardiac | 332 (21.4) | 156 (28.7) | 176 (17.5) | |
| Surg-Noncardiac | 125 (8.1) | 54 (9.9) | 71 (7.0) | |
| Other | 333 (21.5) | 83 (15.3) | 250 (24.8) | |
| Pre-Existing Conditions | ||||
| Heart failure this admission | 108 (7.0) | 41 (7.6) | 67 (6.6) | 0.51 |
| Heart failure prior to admission | 82 (5.3) | 27 (5.0) | 55 (5.5) | 0.69 |
| Arrhythmia | 332 (21.4) | 123 (22.7) | 209 (20.7) | 0.38 |
| Hypotension | 594 (38.3) | 175 (32.2) | 419 (41.6) | <0.001 |
| Respiratory insufficiency | 932 (60.1) | 323 (59.5) | 609 (60.4) | 0.72 |
| Renal insufficiency | 150 (9.7) | 28 (5.2) | 122 (12.1) | <0.001 |
| Hepatic insufficiency | 59 (3.8) | 11 (2.0) | 48 (4.8) | 0.007 |
| Metabolic or electrolyte abnormality | 290 (18.7) | 78 (14.4) | 212 (21.0) | 0.001 |
| Baseline depression in CNS function | 216 (13.9) | 65 (12.0) | 151 (15.0) | 0.10 |
| Acute CNS non-stroke event | 116 (7.5) | 23 (4.2) | 93 (9.2) | <0.001 |
| Pneumonia | 106 (6.8) | 41(7.6) | 65 (6.4) | 0.41 |
| Sepsis | 220 (14.2) | 55 (10.1) | 165 (16.4) | <0.001 |
| Major trauma | 164 (10.6) | 24 (4.4) | 140 (13.9) | <0.001 |
| Metastatic or hematologic malignancy | 73 (4.7) | 7 (1.3) | 66 (6.5) | <0.001 |
| Interventions in Place | ||||
| Assisted/mechanical ventilation | 1004 (64.7) | 329 (60.6) | 675 (67.0) | 0.01 |
| Intravenous antiarrhythmics | 69 (4.4) | 35(6.4) | 34 (3.4) | 0.005 |
| Intravenous vasopressors | 628 (40.5) | 175 (32.2) | 453 (44.9) | <0.001 |
Abbreviations: PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia; ICU, intensive care unit; ED, emergency department; CNS, central nervous system; Mon, Monday; Fri, Friday
13 patients (5 survivors, 8 non-survivors) with missing data for time of cardiac arrest
Table 2.
Event Characteristics of Patients Surviving to Hospital Discharge
| No. (%)(N =1551) | Survivors (n=543) | Non-Survivors (n= 1008) | P value | |
|---|---|---|---|---|
| Year | 0.69 | |||
| 2006 | 305 (19.7) | 101 (18.6) | 204 (20.2) | |
| 2007 | 315 (20.3) | 104 (19.2) | 211 (20.9) | |
| 2008 | 407 (26.2) | 143 (26.3) | 264 (26.2) | |
| 2009 | 372 (24.0) | 137 (25.2) | 235 (23.3) | |
| 2010* | 152 (9.8) | 58 (10.7) | 94 (9.3) | |
| Code Blue activated | 408 (26.3) | 130 (23.9) | 278 (27.6) | 0.12 |
| Teaching Status† | <0.001 | |||
| Major teaching‡ | 1169 (77.5) | 443 (84.7) | 726 (73.7) | |
| Minor teaching§ | 231 (15.3) | 52 (9.9) | 179 (18.2) | |
| Non-teaching | 108 (7.2) | 28 (5.4) | 80 (8.1) | |
| Ownership | 0.02 | |||
| Private | 59 (3.8) | 11 (2.0) | 48 (4.8) | |
| Government | 233 (15.0) | 82 (15.1) | 151 (15.0) | |
| Non-profit | 1216 (78.4) | 430 (79.2) | 786 (78.0) | |
| Unknown | 43 (2.8) | 20 (3.7) | 23 (2.3) | |
| Region | 0.04 | |||
| North Mid-Atlantic | 145 (9.3) | 49 (9.0) | 96 (9.5) | |
| South Atlantic | 334 (21.5) | 96 (17.7) | 238 (23.6) | |
| North Central | 290 (18.7) | 116 (21.4) | 174 (17.3) | |
| South Central | 481 (31.0) | 169 (31.1) | 312 (31.0) | |
| Mountain/Pacific | 258 (16.6) | 93 (17.1) | 165 (16.4) | |
| Unknown | 43 (2.8) | 20 (3.7) | 23 (2.3) | |
| Location | 0.14 | |||
| Urban | 1466 (94.5) | 512 (94.3) | 954 (94.6) | |
| Rural | 42 (2.7) | 11 (2.0) | 31 (3.1) | |
| Unknown | 43 (2.8) | 20 (3.7) | 23 (2.3) | |
| Bed size† | 0.07 | |||
| <250 beds | 110 (7.3) | 28 (5.4) | 82 (8.3) | |
| 250–499 beds | 743 (49.3) | 255 (48.8) | 488 (49.5) | |
| >499 beds | 655(43.4) | 240 (45.9) | 415 (42.1) |
Data available only from January 1 to August 30
43 patients (20 survivors and 23 non-survivors) with missing data for teaching status and bed size
Includes institutions with residents and fellows
Includes institutions with residents
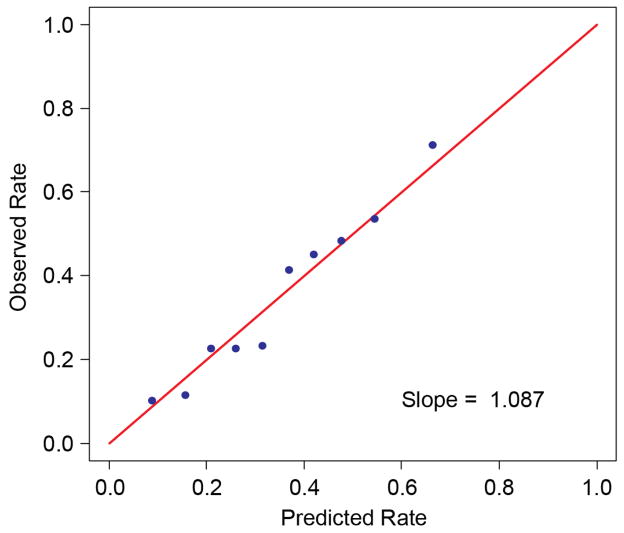
After multivariable adjustment, 13 variables were identified as critical factors for risk-standardization (Table 3). These included age, sex, illness category, cardiac arrest rhythm, location of arrest, mechanical ventilation, acute non-stroke neurologic event, major trauma, hypotension, metabolic or electrolyte abnormalities, renal insufficiency, sepsis, and requirement for intravenous vasoactive medications at the time of arrest. The model had good discrimination (C-statistic of 0.71). Model calibration was confirmed with observed vs. predicted plots (Figure 1). For model validation, we performed a series of 1000 bootstrap samples and found that model discrimination was similar (bootstrap-corrected validation C-statistic of 0.69).
Table 3.
Model Predictors for Survival to Discharge
| Predictor | Odds Ratio (95% CI) |
|---|---|
| Age | |
| Older Children (8 to 18 years) | Reference |
| Neonates(0 to 1 month) | 0.95 (0.65, 1.39) |
| Infants (1 month to <1 year) | 1.67 (1.17, 2.40) |
| Young children(1 to 8 years) | 1.21 (0.84, 1.73) |
| Male sex | 0.86 (0.69, 1.08) |
| Illness Category | |
| Medical-Cardiac | Reference |
| Medical-Noncardiac | 0.88 (0.61, 1.27) |
| Surgical-Cardiac | 1.86 (1.23, 2.81) |
| Surgical-Noncardiac | 1.23 (0.74, 2.03) |
| Other | 0.93 (0.57, 1.50) |
| Hypotension | 0.85 (0.64, 1.13) |
| Renal Insufficiency | 0.50 (0.32, 0.79) |
| Metabolic or electrolyte abnormality | 0.79 (0.57, 1.09) |
| Acute non-stroke CNS event | 0.61 (0.37, 1.02) |
| Septicemia | 0.65 (0.46, 0.94) |
| Major Trauma | 0.39 (0.21, 0.71) |
| Mechanical Ventilation | 0.79 (0.59, 1.06) |
| Intravenous Vasoactive Agents | 0.49 (0.36, 0.65) |
| Location of Arrest | |
| Unmonitored Unit | Reference |
| ICU | 1.23 (0.74, 2.06) |
| Procedure Areas | 2.10 (1.12, 3.96) |
| ED | 0.49 (0.27, 0.86) |
| Monitored Unit | 0.42 (0.18, 0.99) |
| Other | 1.14 (0.53, 2.47) |
| Cardiac Arrest Rhythm | |
| Asystole | Reference |
| PEA | 1.18 (0.90, 1.54) |
| VF | 1.23 (0.75, 2.00) |
| PVT | 1.95 (1.18, 3.22) |
Abbreviations: CI, confidence interval; CNS, central nervous system; ICU, intensive care unit; ED, emergency department; PEA, pulseless electrical activity; VF, ventricular fibrillation; PVT, pulseless ventricular tachycardia
Figure 1. Calibration of the Final Model in the Derivation Cohort.
The model showed excellent calibration, with slope of 1.1 (slope of 1.0 for perfect calibration).
Hospital Variation in Risk-Standardized Survival Rates
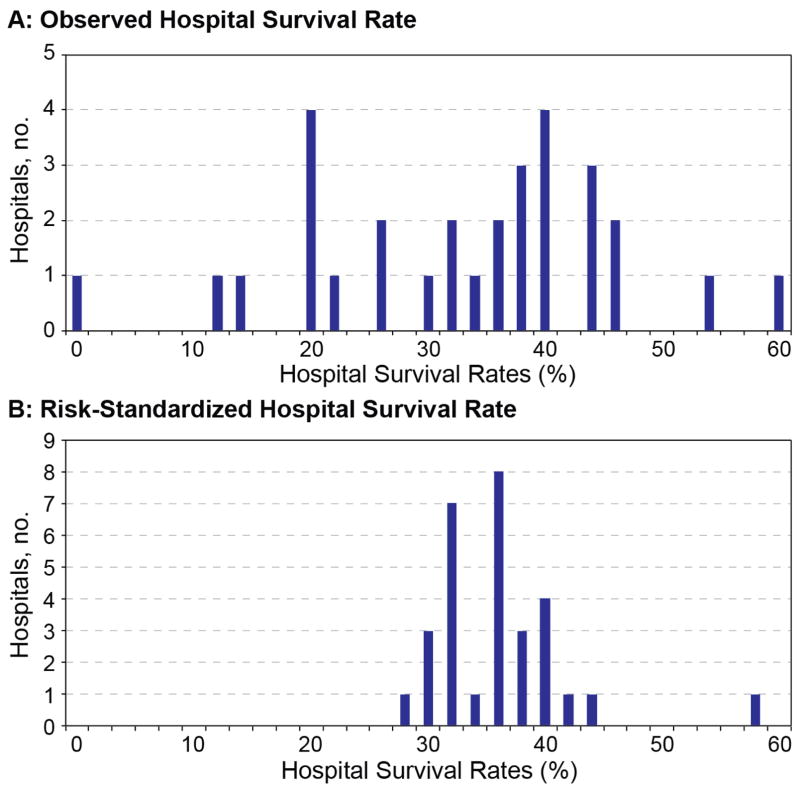
Prior to adjustment for case-mix, survival rates for the 30 hospitals with at least 10 cardiac arrest cases varied considerably, with a median hospital rate of 37%, an inter-quartile range (IQR) of 24% to 42%, and a total range of 0% to 61% (Figure 2a). After risk-standardization, the distribution of hospital rates of survival narrowed considerably. However, some variation in hospital rates of survival persisted, with a median hospital risk-standardized rate of 37%, IQR of 33% to 38%, and a total range of 29% to 48% (Figure 2b).
Figure 2.
Unadjusted (Fig. 2a) and Risk-Standardized (Fig. 2b) Hospital Survival Rates for In-Hospital Cardiac Arrest
Discussion
Using a large national registry, we developed and validated a risk-standardized model for survival in pediatric patients with in-hospital cardiac arrest. Among a wide range of variables, our model identified 13 unique patient predictors of survival to discharge. These variables were defined using standardized definitions and are easily obtainable from medical records. Without adjustment for patient factors, the range of survival rates across hospitals was 0% to 61%. After adjustment for patient case-mix, the range of risk-standardized hospital rates of cardiac arrest survival narrowed substantially (range= 29 to 48%), but hospital variation in survival remained. The presence of variability in risk-standardized survival rates among hospitals suggests an opportunity to save lives if hospitals in the lower range were able to achieve survival rates of higher-performing hospitals.
Most prior studies on pediatric in-hospital cardiac arrest have focused on identifying patient predictors of survival. For instance, children whose cardiac arrest is caused by an underlying cardiac etiology have been shown to have lower survival than those with a respiratory etiology.19 Likewise, those with an arrest surrounding surgery for repair or palliation of congenital heart disease are more likely to survive than those with a medical-cardiac or non-cardiac diagnosis.20 Others have found that certain cardiac arrest rhythms, such as ventricular fibrillation and pulseless ventricular tachycardia, are associated with improved survival.21 Despite identifying certain patient characteristics associated with survival in prior studies, there has not been, to date, a validated method to risk standardize hospital rates of survival for pediatric in-hospital cardiac arrest– a critical foundation for quality improvement. In this study, we have created and validated such a model to facilitate comparisons of pediatric outcomes for this condition between hospitals. Such a model will be of great value to benchmark hospital performance on in-hospital cardiac arrest and to guide future quality improvement efforts. Our model adhered to recommended standards for models of publicly reported outcomes, including high-quality and timely data as well as clinical coherence of the model variables.2 Importantly, we utilized a hierarchical random-effects model, which accounts for variation in sample size between hospitals to generate ‘shrinkage estimates’ for sites with lower case volumes.
In this study, we found that the inter-quartile range prior to risk-adjustment was 18% and narrowed to 5% following risk adjustment. This suggests that risk-standardization is critical for future benchmarking efforts, as the inter-quartile range narrowed by over 70%. It also highlights that, despite a reduction in variation of survival rates across hospitals, there remained significant variability in hospital survival rates that was not attributable to differences in patient characteristics reported in the registry. This suggests that the remaining hospital variation in pediatric cardiac arrest survival may be due to hospital-specific factors including quality of care before, during, and after resuscitation. Such factors may include resuscitation response times (e.g., time to defibrillation), chest compression depth, frequency of interruptions in chest compressions, duration of cardiopulmonary resuscitation, and post-resuscitation care (e.g., hospital differences in intensive care expertise).1, 22–26 Future studies are needed to identify “best practices” associated with higher survival rates at top-performing hospitals and whether such practices can be readily disseminated and effectively implemented to all hospitals.
The impact of having access to a risk-standardized model for survival in pediatric patients with in-hospital cardiac arrest may be profound for quality improvement initiatives. Hospitals need to be able to benchmark the effect of their improvement programs over time, and with other organizations. Similar to other conditions that are the focus of broad quality programs such as acute myocardial infarction27, the field of pediatric resuscitation will greatly benefit from having validated methods to risk-standardize survival outcomes for in-hospital cardiac arrest.
Our study has certain limitations. GWTG-Resuscitation is a quality improvement registry, and hospital participation is voluntary. Given the fact that a minority of children’s hospitals in the U.S. participate in the registry, and hospitals in a quality improvement registry are more likely to direct substantial resources to improving CPR outcomes, our findings may not be generalizable to non-registry hospitals. Second, although our model adjusted for a number of patient characteristics and had good discrimination, we did not have information on certain patient factors. For instance, we did not have information on cyanotic and acyanotic congenital heart disease in most patients, which may have improved model discrimination. Moreover, we did not have information on hospital factors, such as staffing ratios, presence of around-the-clock intensivists in critical care units, a site’s annual cardiac surgery volume, and use of mock codes and other quality improvement initiatives. Additionally, our examination of variation in risk-standardized survival rates was limited to 30 hospitals with at least 10 pediatric in-hospital cardiac arrest cases; future studies with a larger hospital sample may be needed to confirm these findings. Lastly, we did not assess survival with favorable neurological outcomes – another clinically important outcome to patients – as it was missing in 26% of pediatric survivors and was outside the scope of our present study on survival.
Conclusion
In a national registry of in-hospital cardiac arrest, we have developed and validated a model to risk-standardize hospital rates of survival for pediatric in-hospital cardiac arrest. After accounting for patient case-mix, we found that variation in hospital survival rates decreased but persisted. Our findings lay the methodological foundation for future efforts by national organizations to benchmark hospital survival for cardiac arrest in children and suggest the possibility that differences in hospital processes and quality of care, in part, account for the differences in survival rates across hospitals.
Acknowledgments
Funding/Support:
• Dr. Jayaram is supported by a T32 training grant (HL110837) from the National Heart Lung and Blood Institute.
• Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the National Heart Lung and Blood Institute.
Footnotes
- Dr. Chan has worked as a consultant with the American Heart Association
References
- 1.Matos RI, Watson RS, Nadkarni VM, Huang HH, Berg RA, Meaney PA, Carroll CL, Berens RJ, Praestgaard A, Weissfeld L, Spinella PC. Duration of cardiopulmonary resuscitation and illness category impact survival and neurologic outcomes for in-hospital pediatric cardiac arrests. Circulation. 2013;127:442–451. doi: 10.1161/CIRCULATIONAHA.112.125625. [DOI] [PubMed] [Google Scholar]
- 2.Krumholz HM, Brindis RG, Brush JE, Cohen DJ, Epstein AJ, Furie K, Howard G, Peterson ED, Rathore SS, Smith SC, Jr, Spertus JA, Wang Y, Normand SL. Standards for statistical models used for public reporting of health outcomes: An American Heart Association Scientific Statement from the Quality of Care and Outcomes Research Interdisciplinary Writing Group: Cosponsored by the Council on Epidemiology and Prevention and the Stroke Council. Endorsed by the American College of Cardiology Foundation. Circulation. 2006;113:456–462. doi: 10.1161/CIRCULATIONAHA.105.170769. [DOI] [PubMed] [Google Scholar]
- 3.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, Berg RA, Nichol G, Lane-Trultt T. Cardiopulmonary resuscitation of adults in the hospital: A report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 4.Cummins RO, Chamberlain D, Hazinski MF, Nadkarni V, Kloeck W, Kramer E, Becker L, Robertson C, Koster R, Zaritsky A, Bossaert L, Ornato JP, Callanan V, Allen M, Steen P, Connolly B, Sanders A, Idris A, Cobbe S. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: The in-hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 5.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update and simplification of the Utstein templates for resuscitation registries: A statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, Interamerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 6.Girotra S, Spertus JA, Li Y, Berg RA, Nadkarni VM, Chan PS. Survival trends in pediatric in-hospital cardiac arrests: An analysis from Get with the Guidelines-Resuscitation. Circulation Cardiovascular Quality and Outcomes. 2013;6:42–49. doi: 10.1161/CIRCOUTCOMES.112.967968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peberdy MA, Ornato JP, Larkin GL, Braithwaite RS, Kashner TM, Carey SM, Meaney PA, Cen L, Nadkarni VM, Praestgaard AH, Berg RA. Survival from in-hospital cardiac arrest during nights and weekends. JAMA: the Journal of the American Medical Association. 2008;299:785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 8.Chan PS, Nichol G, Krumholz HM, Spertus JA, Jones PG, Peterson ED, Rathore SS, Nallamothu BK. Racial differences in survival after in-hospital cardiac arrest. JAMA: the Journal of the American Medical Association. 2009;302:1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merchant RM, Becker LB, Yang F, Groeneveld PW. Hospital racial composition: A neglected factor in cardiac arrest survival disparities. American Heart Journal. 2011;161:705–711. doi: 10.1016/j.ahj.2011.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein H. Multilevel Statistical Models. 2. London: Edward Arnold; 1995. [Google Scholar]
- 11.Belsley DA, Kuh E, Welsch RE. Regression Diagnostics: Identifying influential data and sources of collinearity. New York: Wiley; 1980. [Google Scholar]
- 12.DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- 13.Harrell FE. Regression modeling strategies: With applications to linear models, logistic regression, and survival analysis. New York, NY: Springer-Verlag; 2001. [Google Scholar]
- 14.Shahian DM, Torchiana DF, Shemin RJ, Rawn JD, Normand SL. Massachusetts cardiac surgery report card: Implications of statistical methodology. The Annals of Thoracic Surgery. 2005;80:2106–2113. doi: 10.1016/j.athoracsur.2005.06.078. [DOI] [PubMed] [Google Scholar]
- 15.Christiansen CL, Morris CN. Improving the statistical approach to health care provider profiling. Annals of Internal Medicine. 1997;127:764–768. doi: 10.7326/0003-4819-127-8_part_2-199710151-00065. [DOI] [PubMed] [Google Scholar]
- 16.Normand SL, Glickman ME, Gatsonis CA. Statistical methods for profiling providers of medical care: Issues and applications. J Am Stat Assoc. 1997;92:803–814. [Google Scholar]
- 17.Normand SL, Shahian DM. Statistical and clinical aspects of hospital outcomes profiling. Statistical Science. 2007;22:206–226. [Google Scholar]
- 18.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2008. http://www.R-project.org. [Google Scholar]
- 19.Berens RJ, Cassidy LD, Matchey J, Campbell D, Colpaert KD, Welch T, Lawson M, Peterson C, O’Flynn J, Dearth M, Tieves KS. Probability of survival based on etiology of cardiopulmonary arrest in pediatric patients. Paediatric Anaesthesia. 2011;21:834–840. doi: 10.1111/j.1460-9592.2010.03479.x. [DOI] [PubMed] [Google Scholar]
- 20.Ortmann L, Prodhan P, Gossett J, Schexnayder S, Berg R, Nadkarni V, Bhutta A. Outcomes after in-hospital cardiac arrest in children with cardiac disease: A report from Get With the Guidelines--Resuscitation. Circulation. 2011;124:2329–2337. doi: 10.1161/CIRCULATIONAHA.110.013466. [DOI] [PubMed] [Google Scholar]
- 21.Nadkarni VM, Larkin GL, Peberdy MA, Carey SM, Kaye W, Mancini ME, Nichol G, Lane-Truitt T, Potts J, Ornato JP, Berg RA. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA: the Journal of the American Medical Association. 2006;295:50–57. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 22.Sutton RM, Niles D, Nysaether J, Abella BS, Arbogast KB, Nishisaki A, Maltese MR, Donoghue A, Bishnoi R, Helfaer MA, Myklebust H, Nadkarni V. Quantitative analysis of CPR quality during in-hospital resuscitation of older children and adolescents. Pediatrics. 2009;124:494–499. doi: 10.1542/peds.2008-1930. [DOI] [PubMed] [Google Scholar]
- 23.Hunt EA, Vera K, Diener-West M, Haggerty JA, Nelson KL, Shaffner DH, Pronovost PJ. Delays and errors in cardiopulmonary resuscitation and defibrillation by pediatric residents during simulated cardiopulmonary arrests. Resuscitation. 2009;80:819–825. doi: 10.1016/j.resuscitation.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 24.Sutton RM, French B, Nishisaki A, Niles DE, Maltese MR, Boyle L, Stavland M, Eilevstjonn J, Arbogast KB, Berg RA, Nadkarni VM. American Heart Association cardiopulmonary resuscitation quality targets are associated with improved arterial blood pressure during pediatric cardiac arrest. Resuscitation. 2012 doi: 10.1016/j.resuscitation.2012.08.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sutton RM, Niles D, Nysaether J, Arbogast KB, Nishisaki A, Maltese MR, Bishnoi R, Helfaer MA, Nadkarni V, Donoghue A. Pediatric CPR quality monitoring: Analysis of thoracic anthropometric data. Resuscitation. 2009;80:1137–1141. doi: 10.1016/j.resuscitation.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 26.Sutton RM, Maltese MR, Niles D, French B, Nishisaki A, Arbogast KB, Donoghue A, Berg RA, Helfaer MA, Nadkarni V. Quantitative analysis of chest compression interruptions during in-hospital resuscitation of older children and adolescents. Resuscitation. 2009;80:1259–1263. doi: 10.1016/j.resuscitation.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 27.Bradley EH, Curry LA, Spatz ES, Herrin J, Cherlin EJ, Curtis JP, Thompson JW, Ting HH, Wang Y, Krumholz HM. Hospital strategies for reducing risk-standardized mortality rates in acute myocardial infarction. Annals of Internal Medicine. 2012;156:618–626. doi: 10.1059/0003-4819-156-9-201205010-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]