Abstract
Background
Despite intensive efforts over many years, the U.S. has made limited progress in improving rates of survival from out-of-hospital cardiac arrest (OHCA). Recently, national organizations, such as the American Heart Association, have focused on promoting bystander cardiopulmonary resuscitation (CPR), use of automated external defibrillators (AEDs), and other performance improvement efforts.
Methods and Results
Using the Cardiac Arrest Registry to Enhance Survival (CARES), a prospective clinical registry, we identified 70,027 U.S. patients who experienced an OHCA between October 2005 and December 2012. Using multilevel Poisson regression, we examined temporal trends in risk-adjusted survival. After adjusting for patient and cardiac arrest characteristics, risk-adjusted rates of OHCA survival increased from 5.7% in the reference period of 2005-2006 to 7.2% in 2008 (adjusted risk ratio, 1.27; 95% CI, 1.12-1.43; P<0.001). Survival improved more modestly to 8.3% in 2012 (adjusted risk ratio, 1.47; 95% CI, 1.26-1.70; P<0.001). This improvement in survival occurred in both shockable and non-shockable arrest rhythms (P for interaction=0.22) and was also accompanied by better neurological outcomes among survivors (P for trend=0.01). Improved survival was due to both higher rates of pre-hospital survival, where risk-adjusted rates increased from 14.3% in 2005-2006 to 20.8% in 2012 (P for trend<0.001), and in-hospital survival (P for trend=0.015). Rates of bystander CPR and AED use modestly increased during the study period and partly accounted for pre-hospital survival trends.
Conclusions
Data drawn from a large subset of U.S communities suggest that rates of survival from OHCA have improved among sites participating in a performance improvement registry.
Keywords: cardiac arrest, survival, trends
INTRODUCTION
Despite intensive efforts over 3 decades, the U.S. has made little progress in improving the overall rate of survival from out-of-hospital cardiac arrest, with survival rates remaining relatively unchanged at 7.6%.1 However, in recent years, advances in resuscitation science have generated promising findings. In randomized clinical trials, early use of therapeutic hypothermia2, 3 and automated external defibrillators (AEDs)4, 5 were found to improve survival and neurological outcomes in selected populations. National efforts have focused on delivery of higher-quality cardiopulmonary resuscitation.
While there is ample reason to believe that adoption of these practices and other performance improvement activities should lead to higher rates of out-of-hospital cardiac arrest survival in the U.S., this has not been consistently demonstrated. If quality improvement efforts are making a difference, it should be possible to document improved survival at the community level. Isolated studies in the U.S. have generated encouraging findings6, 7 but these may not be generalizable to the nation at large.
Accordingly, we analyzed contemporary trends in rates of survival to hospital discharge for out-of-hospital cardiac arrest from 2005-2012 in a large and geographically diverse set of U.S. communities—those that participate in the “Cardiac Arrest Registry to Enhance Survival” (CARES), which was established to improve pre-hospital care at the local level.8, 9 To determine which phase of resuscitation care may be influencing outcomes, we examined temporal trends in survival to hospital admission and, among those who survived to hospital admission, their likelihood of surviving to hospital discharge. Finally, to determine if any survival trends are due to improving rates of bystander CPR or AED use, we evaluated trends in both and their aggregate effect on out-of-hospital cardiac arrest survival.
METHODS
Data Source and Study Population
CARES is a large, prospective clinical registry of patients with out-of-hospital cardiac arrest in the U.S. Since the system was established in 2005, it has grown, by 2012, to collect data from 248 EMS systems across 23 states, representing a catchment area of more than 64 million people. Established by the Centers for Disease Control and Emory University for public health surveillance and continuous quality improvement, the design of the registry has been previously described in detail.8, 9 Briefly, all patients with a confirmed out-of-hospital cardiac arrest (defined as apneic and unresponsive) of presumed cardiac etiology and for whom resuscitation is attempted are identified and followed, including those with termination of resuscitation prior to hospital arrival. Data are collected from three sources that together define the continuum of emergency cardiac care: 911 dispatch centers, EMS agencies, and receiving hospitals. Standardized international Utstein definitions for defining clinical variables and outcomes are used to ensure uniformity.10 A CARES analyst reviews every record for completeness and accuracy.9
Our analysis is based on 73,390 cases submitted to the CARES registry between October 1, 2005 and December 31, 2012 (Figure 1). We excluded 8 patients with obvious signs of death and 315 patients with a valid do-not-attempt resuscitation order, as well as 2544 events occurring in a facility with an on-site healthcare professional (e.g., hospital, medical clinic), because these cases have response and treatment times that are different from other out-of-hospital cardiac arrests. We also excluded 496 events (0.7%) in which information on patient survival to hospital admission (n=409 [0.6%]) or discharge (n=87 [0.1%]) was missing. The final sample comprised 70,027 patients treated by 248 EMS agencies.
Figure 1.
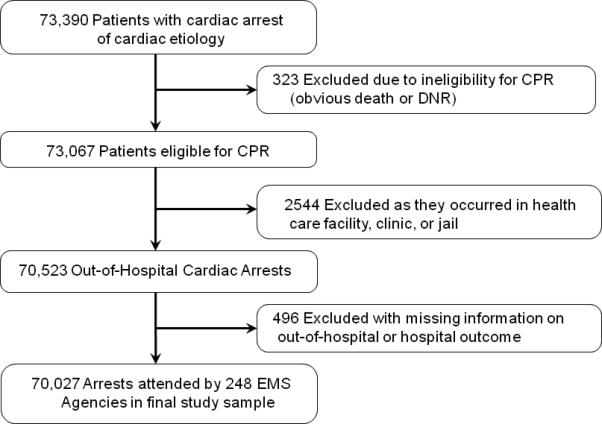
Definition of Study Cohort
Independent Variable and Study Outcome
The independent variable was calendar year, which was evaluated as a continuous variable. The primary outcome of interest was survival to hospital discharge. As the probability of survival from ventricular fibrillation or pulseless ventricular tachycardia is generally better than from asystole or pulseless electrical activity, we analyzed temporal survival trends in the overall cohort and separately by these two rhythm groups. As secondary outcomes, we analyzed temporal trends in the rate of survival to hospital admission to an inpatient unit (pre-hospital survival) and, among those who survived to be admitted, the likelihood of survival to hospital discharge (in-hospital survival). To determine if any recent changes in out-of-hospital cardiac arrest survival could be attributed to rising rates of bystander CPR or AED use, we examined the effect of both interventions on overall survival trends and for pre-hospital and in-hospital survival.
In addition to documenting survival to hospital discharge, CARES documents the degree of neurological disability from the inpatient record among survivors at discharge, measured by the cerebral performance category (CPC) score.11 A CPC score of 1 denotes a patient with mild or no neurological disability, 2 reflects moderate neurological disability, 3 indicates severe neurological disability, and 4 is assigned to patients in a persistent coma or vegetative state. For this study, we evaluated temporal trends in discharge neurological status as an ordinal variable.
Statistical Analyses
To evaluate changes in baseline characteristics by calendar year, we used the Mantel-Haenszel test of trend for categorical variables and linear regression for continuous variables. To assess whether survival to discharge has improved over time, three-level multilevel Poisson regression models were constructed for the overall cohort and by rhythm type, in which patients were nested within EMS agencies and EMS agencies were nested with U.S. states. In these models, random intercepts were estimated for each EMS agency and U.S. state.12 Since survival rates for out-of-hospital cardiac arrest have been noted to differ markedly among EMS agencies,13 the use of multilevel models ensures that our analyses reflect survival trends within EMS agency sites. Moreover, multilevel models account for the fact that different EMS agencies joined CARES at different time points. In these models, in order to obtain more interpretable estimates of effect, we directly estimated rate-ratios instead of odds ratios by specifying a Poisson distribution and including a robust variance estimate in our models.14, 15
Our independent variable, calendar year, was included in the model as a continuous variable with polynomial (quadratic and cubic) terms for year, as appropriate. We defined years 2005-2006 as the reference period, since CARES did not begin enrollment until October 1, 2005. We multiplied the adjusted rate-ratios for each subsequent year (2007 through 2012) with the observed survival rate for the reference period (2005-2006) to obtain yearly risk-adjusted survival rates for the study period. These rates represent what the survival would be for each year if the patient case-mix was identical to the reference period within each EMS agency. Our models adjusted for age, sex, race/ethnicity (coded by the EMS provider as white, black, Latino, other, or unknown), initial cardiac arrest rhythm (ventricular fibrillation, pulseless ventricular tachycardia, asystole, pulseless electrical activity), location of arrest (private residence, public area with likely AED availability [e.g., sporting facility, airport], other public areas, and other), and whether the arrest was witnessed. To examine the robustness of our survival trend findings (since any improvement in survival trends may have been due to later enrolling sites with higher survival rates), we repeated the models and included only those EMS agencies that have been enrolling patients within CARES since 2005-06 with an average annual case volume average of >20 out-of-hospital cardiac arrests.
We conducted several additional analyses. To evaluate whether there were geographical variations in any temporal survival trends, we constructed two-level models (patients nested within EMS agencies) and evaluated for an interaction between U.S. census region (Northeast, Midwest, South, and West) and time. We also assessed temporal trends in neurological disability among those surviving to hospital discharge. In these analyses, we constructed multinomial three-level models to evaluate discharge CPC score as an ordinal variable, with time assessed as a continuous variable with polynomial terms (as described for the primary analysis).
Finally, to discern potential reasons for any improvement over time, we constructed similar three-level logistic regression models to examine whether survival trends were due to increased rates of survival to hospital admission, in-hospital survival, or both. Since bystander CPR and/or AED use are potential mediators of any observed survival trends, we further examined whether increasing rates of bystander CPR and/or AED use were associated with survival trends by adding these two variables to the multilevel models described above and evaluated whether their inclusion attenuated year-over-year risk ratio estimates.
Besides race, data were missing in only 0.3% of cases, and the average number of missing data fields per patient was 0.003. There were no differences in baseline characteristics between those with missing data and those with complete data (results not shown). We used multiple imputation methods to impute missing values on the basis of all other observed data. Imputations were performed with Markov Chain Monte Carlo methods as implemented in SAS PROC MI. Five imputed data sets were generated; analyses were replicated across data sets and pooled to obtain final estimates. Patients with missing information on race were categorized as ‘unknown’ as a separate dummy variable in our models. Results with and without imputation were very similar; only the former are presented. All statistical analyses were conducted using SAS Version 9.1.3 (SAS Institute, Cary, NC) and R Version 2.6.0 (Free Software Foundation, Boston, MA). All hypothesis tests were 2-sided with a significance level of 0.05. Because this study used only de-identified data, it was considered exempt research by the Mid America Heart Institute's Institutional Review Board.
RESULTS
Patient and cardiac arrest characteristics of the study cohort are summarized in Table 1. The mean age of the study population was 64.1 years (standard deviation of 18.2 years), and 61% were men. Approximately five of six cardiac arrests occurred in a private residence, and <2% of all cardiac arrests occurred in a public area with likely access to an AED. Fewer than half of events were witnessed. More than three-quarters of patients were found in asystole or pulseless electrical activity, whereas 23.6% had cardiac arrest rhythms amenable to defibrillation treatment. During the study period, there were no temporal differences in patients’ sex or presenting rhythm. There were, however, modest changes in the age and racial composition of the study cohort, with an increasingly older and white population in the later years. There were also small changes in the proportion of patients whose cardiac arrest occurred at home or were witnessed.
Table 1. Trends in Baseline Characteristics.
For illustrative purposes, trends in baseline characteristics are presented as 3 time periods.
| Year Group | ||||
|---|---|---|---|---|
| 2005 to 2007 N = 4630 | 2008 to 2010 N = 26,058 | 2011 to 2012 N = 39,339 | P for trend* | |
| Age group | 0.02 | |||
| <50 | 923 (20.1%) | 4810 (18.5%) | 7148 (18.2%) | |
| 50-59 | 901 (19.6%) | 4964 (19.1%) | 7434 (18.9%) | |
| 60-69 | 910 (19.8%) | 5433 (20.9%) | 8509 (21.7%) | |
| 70-79 | 854 (18.6%) | 4944 (19.0%) | 7385 (18.8%) | |
| ≥80 | 1010 (22.0%) | 5872 (22.6%) | 8786 (22.4%) | |
| Missing | 32 | 35 | 77 | |
| Sex | 0.22 | |||
| Female | 1846 (39.9%) | 10,066 (38.6%) | 15,176 (38.6%) | |
| Male | 2783 (60.1%) | 15,980 (61.4%) | 24,155 (61.4%) | |
| Missing | 1 | 12 | 8 | |
| Race | 0.005 | |||
| White | 1794 (38.7%) | 10,037 (38.5%) | 16,513 (42.0%) | |
| Black | 1236 (26.7%) | 6986 (26.8%) | 8433 (21.4%) | |
| Latino | 238 (5.1%) | 1400 (5.4%) | 2314 (5.9%) | |
| Other | 88 (1.9%) | 697 (2.7%) | 1036 (2.6%) | |
| Unknown | 1274 (27.5%) | 6938 (26.6%) | 11,043 (28.1%) | |
| Location of Arrest | < 0.001 | |||
| Private residence | 3859 (83.3%) | 21,809 (83.7%) | 33,232 (84.5%) | |
| Public area with likely AED | 80 (1.7%) | 459 (1.8%) | 684 (1.7%) | |
| Other public areas | 575 (12.4%) | 3064 (11.8%) | 4916 (12.5%) | |
| Other | 116 (2.5%) | 726 (2.8%) | 507 (1.3%) | |
| First documented rhythm | 0.24 | |||
| Asystole and PEA | 3536 (76.4%) | 19,965 (76.7) | 30,283 (77.0) | |
| VF and pulseless VT | 1092 (23.6%) | 6081 (23.3%) | 9056 (23.0%) | |
| Missing | 2 | 12 | ||
| Witnessed Arrest | 2208 (47.7%) | 12,052 (46.3%) | 18,815 (47.8%) | 0.01 |
Temporal changes in patient characteristics were assessed, with calendar year evaluated as a continuous variable, and expressed as a P for trend.
Abbreviations: AED, automated external defibrillator; BLS, basic life support; CPR, cardiopulmonary resuscitation; EMS, emergency medical services; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia.
Survival to Discharge
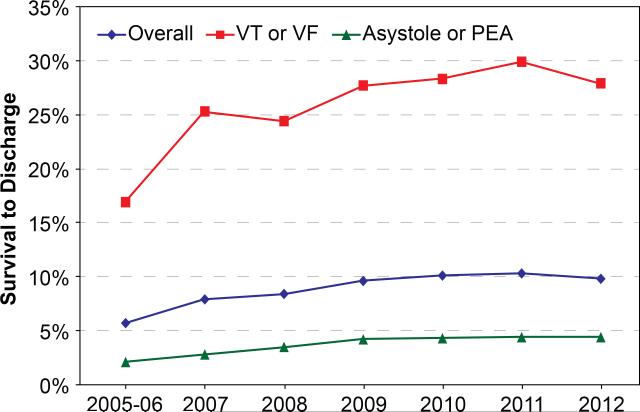
During the study interval, unadjusted rates of survival to hospital discharge increased from 5.7% in 2005-2006 to 9.8% in 2012 (Figure 2). For cardiac arrests due to ventricular fibrillation or pulseless ventricular tachycardia, the unadjusted rate of survival increased from 16.1% to 27.9%, whereas for cardiac arrests due to asystole or pulseless electrical activity, the unadjusted rate of survival increased from 2.1% to 4.4%.
Figure 2. Unadjusted Rates of Survival to Hospital Discharge by Calendar Year.
Observed rates for survival to discharge are displayed for the overall cohort and separately for shockable (ventricular fibrillation [VF] and pulseless ventricular tachycardia [VT]) and non-shockable (asystole and pulseless electrical activity [PEA]) cardiac arrest rhythms.
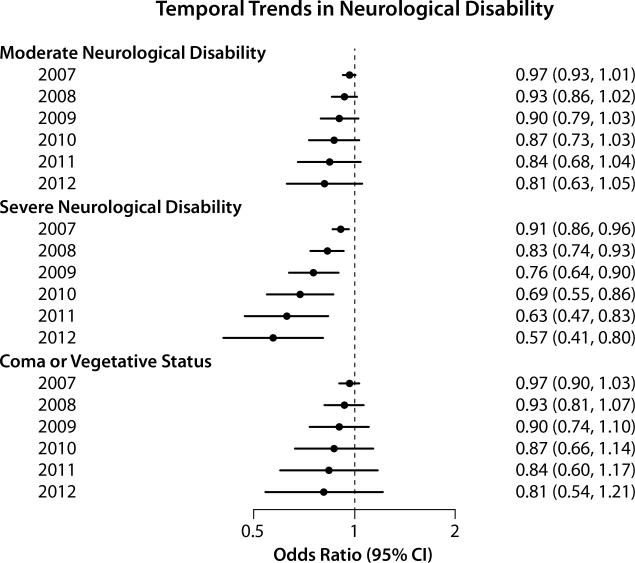
After adjusting for temporal trends in patient and cardiac arrest characteristics, risk-adjusted rates of survival improved markedly over the study period (P for trend <0.001). For instance, compared to the 5.7% survival rate in 2005-2006, the risk-adjusted survival rate in 2008 increased to 7.2% (adjusted risk ratio, 1.27; 95% CI, 1.12-1.43) and continued to increase more modestly thereafter (e.g., 8.3% in 2012; adjusted risk ratio, 1.47; 95% CI, 1.26-1.70) (Table 2; full model in Supplementary Appendix eTable 1). These gains were observed for both types of arrest rhythms (P for interaction between calendar year and rhythm type = 0.22), and yearly risk-adjusted survival rates by rhythm type are summarized in Supplementary Appendix eTable 2. The improved survival trends persisted (P for trend <0.001) when our analyses were restricted to only those EMS agencies which participated in CARES throughout the entire study period (Supplementary Appendix eTable 3 and eFigure 1). Importantly, this improvement in overall rates of survival to hospital discharge was also accompanied by lower rates of neurological disability in survivors over time (P value of 0.01 for yearly trend, compared to discharge CPC of 1; Figure 3). Finally, there were geographical differences in overall survival trends (P for interaction of 0.04), with the greatest improvement in out-of-hospital cardiac arrest survival in the Northeast and little to no improvement in the Midwest (Supplementary Appendix eTable 4).
Table 2. Overall Survival.
* Model-adjusted rates of survival to discharge were compared against the reference period, 2005-2006.
| Year | Unadjusted Rate | Adjusted Rate | Adjusted Rate Ratio (95% CI) | P value for trend |
|---|---|---|---|---|
| 2005-2006 | 5.7% | Reference | Reference | <0.001 |
| 2007 | 7.9% | 6.5% | 1.14 (1.06-1.22) | |
| 2008 | 8.4% | 7.2% | 1.27 (1.12-1.43) | |
| 2009 | 9.6% | 7.8% | 1.37 (1.18-1.59) | |
| 2010 | 10.0% | 8.2% | 1.44 (1.22-1.69) | |
| 2011 | 10.3% | 8.4% | 1.47 (1.25-1.73) | |
| 2012 | 9.8% | 8.3% | 1.47 (1.26-1.70) |
Rates are adjusted for EMS agency and temporal changes in age, sex, race/ethnicity initial cardiac arrest rhythm, location of arrest, and whether the arrest was witnessed.
Figure 3. Trends in Neurological Outcomes.
Compared to a discharge CPC score of 1 (little to no neurological disability), there was a significant trend (P for trend of 0.01) for lower rates of neurological disability over time.
Secondary Outcomes
Because gains in survival to hospital discharge might be attributable to better pre-hospital or inhospital care, we examined temporal trends in these 2 phases of resuscitation care. Unadjusted rates of pre-hospital survival improved from 14.3% in 2005-2006 to 26.4% in 2012 (Table 3). After multivariable adjustment, pre-hospital survival improved by 45% from 2005 to 2012 (P for trend <0.001). There was also a significant, though less substantial, temporal trend for improved in-hospital survival for patients who survived to hospital admission (P for trend of 0.015).
Table 3. Pre-Hospital and In-Hospital Survival.
* Model-adjusted rates of survival to hospital admission and in-hospital survival (among those surviving to hospital admission) are compared against the reference period, 2005-2006.
| Year | Unadjusted Rate | Adjusted Rate | Adjusted Rate Ratio (95% CI) | P value for trend |
|---|---|---|---|---|
| Pre-Hospital Survival | 0.001 | |||
| 2005-2006 | 14.3% | Reference | Reference | |
| 2007 | 22.2% | 17.9% | 1.25 (1.14-1.37) | |
| 2008 | 26.1% | 20.0% | 1.40 (1.23-1.59) | |
| 2009 | 27.0% | 20.8% | 1.45 (1.27-1.65) | |
| 2010 | 27.1% | 20.7% | 1.45 (1.28-1.64) | |
| 2011 | 26.2% | 20.5% | 1.43 (1.27-1.61) | |
| 2012 | 26.4% | 20.8% | 1.45 (1.28-1.65) | |
| In-Hospital Survival | 0.015 | |||
| 2005-2006 | 34.6% | Reference | Reference | |
| 2007 | 35.6% | 35.9% | 1.02 (1.00-1.04) | |
| 2008 | 32.1% | 35.6% | 1.04 (1.01-1.07) | |
| 2009 | 35.5% | 37.2% | 1.06 (1.02-1.11) | |
| 2010 | 36.9% | 39.3% | 1.08 (1.01-1.15) | |
| 2011 | 39.4% | 40.7% | 1.10 (1.02-1.20) | |
| 2012 | 37.2% | 39.5% | 1.12 (1.02-1.24) | |
Rates are adjusted for EMS agency and temporal changes in age, sex, race/ethnicity initial cardiac arrest rhythm, location of arrest, and whether the arrest was witnessed.
To discern potential reasons for the improvement in pre-hospital survival, we considered several potential explanations (Table 4). Bystander CPR increased from 28.2% of cases in 2005-2006 to 36.3% of cases in 2012 (P for trend <0.001). In addition, there was a modest increase in rates of bystander AED use over the study period (P for trend <0.001 for all arrests and 0.048 for witnessed arrests). Further adjustment for these 2 factors in our models showed modest attenuation of the adjusted rate ratios for pre-hospital survival, while estimates for overall and in-hospital survival were not affected (Supplementary Appendix eTable 5).
Table 4. Trends in Bystander CPR and AED Use.
Rates of both bystander CPR and lay person deployment of AEDs increased during the study period.
| 2005-2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | P for trend | |
|---|---|---|---|---|---|---|---|---|
| Person performing CPR | <0.001 | |||||||
| Bystander | 28.2% | 33.1% | 33.8% | 31.6% | 31.8% | 36.7% | 36.3% | |
| First responder | 35.1% | 32.1% | 35.0% | 36.4% | 38.1% | 26.5% | 29.3% | |
| EMS personnel | 36.7% | 34.8% | 31.2% | 32.0% | 30.1% | 36.8% | 34.4% | |
| Bystander AED use* | ||||||||
| All Arrests | 1.9% (18/946) | 2.3% (49/2173) | 3.7% (138/3686) | 3.5% (210/6021) | 3.6% (298/8270) | 4.5% (493/10,853) | 4.2% (692/16,614) | <0.001 |
| Witnessed arrests | 6.5% (14/217) | 5.6% (27/481) | 9.2% (78/847) | 9.1% (122/1340) | 10.3% (183/1784) | 9.5% (259/2719) | 9.4% (398/4224) | 0.048 |
Abbreviation: AED, automated external defibrillator; CPR, cardiopulmonary resuscitation; EMS, emergency medical services
By convention, for calculations of bystander AED use, we excluded from consideration patients with a witnessed arrest for whom CPR was initiated by a first responder (police, firemen) or EMS personnel, as bystanders would not be expected to deploy an AED in these circumstances
DISCUSSION
Based on data collected from a large, prospectively collected registry of cardiac arrest cases in communities across the U.S., we found that overall rates of survival from out-of-hospital cardiac arrest improved dramatically between 2005 and 2012, with accompanying improved trends in both pre-hospital and in-hospital survival. This finding stands in stark contrast to the lack of progress in out-of-hospital cardiac arrest survival over the preceding 30 years in the U.S.1 Improved rates of survival were noted in both shockable and non-shockable cardiac arrest rhythms and were also accompanied by lower rates of neurological disability over time. Finally, bystander CPR and use of AEDs modestly increased during the study period and appeared to, in part, account for some of the observed improved trends in pre-hospital survival.
We are not the first to report encouraging survival trends for out-of-hospital cardiac arrest. Recent studies involving single communities or much smaller populations have also reported improved rates of survival,6, 7 but the generalizability of these findings was unknown. Non-U.S. groups have also documented favorable survival trends.16-18 However, these studies did not account for the potentially confounding role of EMS agency, and findings in other countries may not pertain to the U.S, given differences in the organization and delivery of emergency care. Our study—by far the largest conducted to date in the U.S.—includes data from a much larger and more diverse set of U.S. communities than prior studies and takes local characteristics into account.
Several aspects of our study warrant comment. Our use of multilevel models allowed us to control for clustering of patients within sites to estimate overall survival trends across EMS agencies. In addition, we confirmed a similar survival trend when we restricted our analyses to only those sites which began participation in CARES from its inception. These analyses ensured that our findings were not simply due to recruitment of higher-performing EMS systems during the later years. Moreover, we found that the improvement in survival was not at the expense of higher rates of neurological disability among survivors; in fact, we found that rates of neurological disability actually decreased over time. We also examined temporal trends in survival from out-of-hospital cardiac arrests caused by ventricular fibrillation or pulseless ventricular tachycardia – cardiac arrest rhythms less likely to be confounded by differences in patient characteristics over time – and found the same pattern of improved survival. Lastly, we observed that the improvement in out-of-hospital cardiac arrest survival was due to both gains in pre-hospital resuscitation and inhospital survival, although the improvement in pre-hospital survival appeared larger.
What might explain the recent improvements in rates of out-of-hospital cardiac arrest survival? In contrast to a recent study from Denmark,18 we found that the higher rates of bystander CPR and AED use did not appear to be the principal contributors to overall improvements in survival, perhaps owing to the fact that overall rates of bystander CPR and AED use in the U.S. increased only modestly during the study interval and remained relatively low. However, higher rates of bystander CPR and AED use did attenuate the adjusted rate ratios for pre-hospital survival trends, suggesting that these factors may have mediated, in part, some of the pre-hospital survival improvement. Other factors which were not measured within CARES but may have contributed to the survival trends we observed include a renewed focus on the delivery of high quality CPR (e.g., appropriate depth and rate of chest compressions), avoidance of interruptions in compressions, and elimination of “stacked defibrillations” and frequent pulse checks following defibrillation, but these require confirmation in future studies.
Our findings indicate that the pace of improvement in study communities slowed in recent years, but it has not stopped. It is possible that additional progress can be achieved. For example, clinical trials have reported that compression-only (i.e., “hands only”) CPR is as effective as conventional CPR, and is considerably easier to perform and retain.19 If national efforts to disseminate an easier to perform and retain method of CPR lead to marked improvements in rates of bystander CPR, which parenthetically was initiated in only one-third of our study cohort, additional gains in survival may be realized.19, 20 Likewise, more consistent provision of advanced cardiac life support, including techniques that emphasize uninterrupted delivery of chest compressions and post-cardiac arrest care, may produce better outcomes.21
Our study is limited in certain respects. CARES was designed as a public health surveillance system to make it less burdensome for communities to participate. For that reason, it only collects essential data elements.8 Therefore, we do not have access to detailed clinical information to assess other factors (e.g., comorbidities or EMS response times) that may influence survival. However, because the average age of patients with an out-of-hospital cardiac arrest increased over the study interval, it is unlikely that the survival gains we observed were due to lower severity of illness. Second, although we had information on rates of bystander CPR and AED use, CARES does not collect information on every aspect of resuscitation care, including the quality of CPR. Third, before 2011, information on therapeutic hypothermia was not systematically collected in CARES. Consequently, we were unable to assess trends in hypothermia use. Fourth, because CARES does not specify the catchment area of individual EMS agencies, we cannot compare local differences in cardiac arrest incidence. Fifth, although many studies have documented neurological outcomes based on the broad categories encompassed in a CPC score, interpretation of a particular neurological outcome as a CPC score of 1 or 2 may vary somewhat among sites. Therefore, this secondary outcome should be interpreted with some caution. Sixth, CARES collected information on only cardiac arrests due to a presumed cardiac etiology during the study period. As non-cardiac arrests (e.g., drowning, trauma, progressive respiratory failure, overdoses, asphyxia, primary respiratory arrests) may be associated with different outcomes, our findings of improved trends could reflect, in part, differences in classification of cardiac arrests as cardiac vs. non-cardiac over time. Because CARES did not collect information on non-cardiac arrests, we could not exclude this possibility although there were no changes in the registry's definition of cardiac arrest during the study period. Finally, although this study encompassed communities representing nearly 25% of the U.S. population, our findings may not apply to communities that do not participate in CARES.
In conclusion, in a large prospective, quality improvement registry, we found that rates of survival from out-of-hospital cardiac arrest in the U.S. have substantially improved since 2005. This improvement was attributed to both improved pre-hospital and in-hospital survival and was accompanied by lower rates of neurological disability over time among survivors. These findings indicate that the dismal rates of out-of-hospital cardiac arrest survival that have persisted for so long are not immutable.
Supplementary Material
Acknowledgments
Funding/Support:
Dr. Chan is supported by a Career Development Grant Award (K23HL102224) from the National Heart Lung and Blood Institute.
Dr. Kellermann was supported by the Paul-O'Neill-Alcoa Chair at the RAND Corporation during the initial writing of this manuscript. He is now an employee of the U.S. government.
Footnotes
Authorship: Dr. Chan had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
- Dr. Chan has received funding support from the American Heart Association, which currently helps to fund the CARES registry.
- CARES was funded by the Centers for Disease Control and Prevention from 2004-2012. The program is now supported through private funding from the American Red Cross, the Medtronic Foundation Heart Rescue Program, the American Heart Association, Zoll Corporation, and in-kind support from Emory University.
- Dr. McNally is supported by grant funding from CARES and serves as Executive Director of the program.
None of these funding partners had a role in the study design, data analysis or manuscript preparation and revision.
Disclaimer for Dr. Kellermann: The views expressed do not necessarily represent those of the Uniformed Services University of the Health Sciences or the U.S. Department of Defense.
REFERENCES
- 1.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 2.Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- 3.Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- 4.Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 5.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–1209. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 6.Rea TD, Crouthamel M, Eisenberg MS, Becker LJ, Lima AR. Temporal patterns in long-term survival after resuscitation from out-of-hospital cardiac arrest. Circulation. 2003;108:1196–1201. doi: 10.1161/01.CIR.0000087403.24467.A4. [DOI] [PubMed] [Google Scholar]
- 7.Hinchey PR, Myers JB, Lewis R, De Maio VJ, Reyer E, Licatese D, Zalkin J, Snyder G. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia: the Wake County experience. Ann Emerg Med. 2010;56:348–357. doi: 10.1016/j.annemergmed.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 8.McNally B, Stokes A, Crouch A, Kellermann AL. CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2009;54:674–683. e672. doi: 10.1016/j.annemergmed.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 9.McNally B, Robb R, Mehta M, Vellano K, Valderrama AL, Yoon PW, Sasson C, Crouch A, Perez AB, Merritt R, Kellermann A. Out-of-hospital cardiac arrest surveillance --- Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005--December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 10.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D'Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–3397. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 11.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein H. Multilevel Statistical Models. 3rd Edition. Free 2nd Edition. London: http://www.ats.ucla.edu/stat/examples/msm_goldstein/goldstein.pdf: Arnold Publishers; 2003. [Google Scholar]
- 13.Eisenberg M, White RD. The unacceptable disparity in cardiac arrest survival among American communities. Ann Emerg Med. 2009;54:258–260. doi: 10.1016/j.annemergmed.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 15.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 16.Kitamura T, Iwami T, Kawamura T, Nitta M, Nagao K, Nonogi H, Yonemoto N, Kimura T. Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation. 2012;126:2834–2843. doi: 10.1161/CIRCULATIONAHA.112.109496. [DOI] [PubMed] [Google Scholar]
- 17.Hollenberg J, Herlitz J, Lindqvist J, Riva G, Bohm K, Rosenqvist M, Svensson L. Improved survival after out-of-hospital cardiac arrest is associated with an increase in proportion of emergency crew--witnessed cases and bystander cardiopulmonary resuscitation. Circulation. 2008;118:389–396. doi: 10.1161/CIRCULATIONAHA.107.734137. [DOI] [PubMed] [Google Scholar]
- 18.Wissenberg M, Lippert FK, Folke F, Weeke P, Hansen CM, Christensen EF, Jans H, Hansen PA, Lang-Jensen T, Olesen JB, Lindhardsen J, Fosbol EL, Nielsen SL, Gislason GH, Kober L, Torp-Pedersen C. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 19.Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, Bloomingdale M, Subido C, Romines S, Eisenberg MS. CPR with chest compression alone or with rescue breathing. N Engl J Med. 2010;363:423–433. doi: 10.1056/NEJMoa0908993. [DOI] [PubMed] [Google Scholar]
- 20.Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, Berg MD, Chameides L, O'Connor RE, Swor RA. Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S676–684. doi: 10.1161/CIRCULATIONAHA.110.970913. [DOI] [PubMed] [Google Scholar]
- 21.Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S768–786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.